Abstract
Aims
Reduced physical activity is associated with increased risk of heart failure (HF) in middle-aged individuals. We hypothesized that physical inactivity is also associated with greater HF risk in older individuals, and examined if the association was consistent for HF with preserved ejection fraction (HFPEF) vs. HF with a reduced ejection fraction (HFREF).
Methods and results
We evaluated 1142 elderly participants (mean age 76 years) from the Framingham Study without prior myocardial infarction and who attended a routine examination when daily physical activity was assessed systematically with a questionnaire. A composite score, the physical activity index (PAI), was calculated and modelled as tertiles, and related to incidence of HF, HFPEF, and HFREF on follow-up using proportional hazards regression models adjusting for age and sex, and then additionally for standard HF risk factors. Participants with HF and EF <45% vs. ≥45% were categorized as HFREF and HFPEF, respectively. On follow-up (mean 10 years), 250 participants developed HF (108 with HFPEF, 106 with HFREF, 36 with unavailable EF). In age- and sex-adjusted models, the middle and highest PAI tertiles were associated with a 15–56% lower risk of any HF, of HFREF, and of HFPEF, with a graded response across tertiles. In multivariable models, the association of higher PAI with lower risk of any HF and with HFPEF was maintained, whereas the association with HFREF was attenuated.
Conclusions
Our study of an older community-based sample extends to the elderly and to HFPEF previous findings of a protective effect of physical activity on HF risk.
Keywords: Physical activity, Heart failure, Elderly
Introduction
Heart failure (HF) is an important public health problem that is increasing in prevalence with the ageing of the world population.1,2 To prevent HF, it is important to identify modifiable risk factors. Healthy lifestyle factors have been associated with lower risk of HF, including a dietary pattern characterized by intake of fruits and vegetables, greater physical activity, and lesser adiposity.3 Data on physical activity and the risk of HF are limited and somewhat variable. For example, physical activity was associated with a lower risk of HF in men in the Physicians Health Study.4 In the NHANES 1 Follow-Up Study, physical activity was associated with a lower risk of HF in women but not in men.5 In the FINMONICA Study, higher physical activity was associated with lower risk of HF among both men and women.6 These previous studies4–6 evaluated the association of physical activity and HF in middle-aged samples and did not examine if the association was consistent for both HF with preserved ejection fraction (HFPEF) and HF with reduced ejection fraction (HFREF). Also, because HF is a disease of the elderly,2,7 it would be important to understand if the beneficial effects of physical activity are also experienced by older people. Recent data from the Cardiovascular Health Study suggest that older adults who are unable to perform activities of daily living have an increased risk of HF and mortality.8 However, that study did not specifically evaluate physical activity in the elderly and risk of HF.
Accordingly, we examined the association of physical activity and the incidence of HF in the elderly in a community-based sample and evaluated if the association was consistent for both HFPEF and HFREF. We tested the hypothesis that lower physical activity is associated with higher risk of HF in the elderly, and evaluated if any potential association was consistent for both HFPEF and HFREF.
Methods
Participants
In 1948, the Framingham Heart Study began as a prospective cohort study of a community-based sample.9 All participants in the original cohort have been under continuous surveillance including periodic examinations at the Heart Study clinic approximately every 2 years. For the present investigation, we evaluated participants attending the 20th biennial examination (1986–1990) who were free of previous myocardial infarction (MI) and HF and reported physical activity information. Thus, of 1401 attendees, we excluded 259 individuals [n = 68 for prevalent HF, n = 12 for renal dysfunction (serum creatinine >2 mg/dL), n = 87 for prior MI, and n = 92 for missing physical activity index (PAI)], leaving 1142 participants (mean age 76 years, range 67–97; 65% women) with regular follow-up eligible for the present investigation (Supplementary material, Figure S1). The endpoint for the present investigation was the first documented episode of symptomatic HF.
The study complied with the Declaration of Helsinki; written informed consent was obtained from all study participants, and the Institutional Review Board of the Boston University Medical Center approved the study protocol.
Assessment of physical activity
Physical activity was assessed using a standardized validated questionnaire.8 The questionnaire records the number of hours a day spent on different physical activities, including at the work place and during leisure time (Supplementary material, Table S1). A composite score, the PAI,10 was calculated by adding the products of the hours at each level of activity multiplied by a weight based on the oxygen consumption required for that activity, as detailed previously10 and shown in the footnote to Table S1 in the Supplementary material.
Assessment of covariates
Covariates were assessed at the baseline examination, and included age, sex, systolic blood pressure, hypertension treatment, diabetes mellitus, valvular heart disease, alcohol use, and LV hypertrophy (LVH). Valvular heart disease was defined as the presence of any diastolic murmur or a systolic murmur grade 3/6 or more on the baseline physical examination at the Heart Study.
Ascertainment of outcome
Heart failure was defined as meeting the previously published Framingham criteria (presence of two major, or of one major plus two minor criteria; Supplementary material, Table S2).11 Episodes of HF were identified by review of hospitalization records, medical records from outpatient visits, and from data gathered at routine biennial follow-up visits or annual telephonic health history updates. Records of HF events were reviewed and adjudicated by a physician panel consisting of three experienced investigators. We used the LVEF closest to the date of the HF event to categorize HF into HFPEF (EF >45%) or HFREF (EF ≤45%), or HF with unknown EF (when the EF was not available), as detailed elsewhere.12 We used EF values obtained at the onset of HF, during HF hospitalization, or within 1 year of HF onset in the absence of intervening MI.
Statistical analyses
Physical activity was modelled as sex-specific tertiles of PAI. We plotted cumulative incidence curves relating PAI tertiles to the incidence of HF.
We used Cox proportional hazards regression13 to relate physical activity to the incidence of HF after verifying that the assumption of proportionality of hazards was satisfied. We estimated the hazard ratio of HF in the second and third tertiles of PAI compared with the first tertile that served as the reference group. We constructed models adjusting for: age and sex; and age, sex, systolic blood pressure, hypertension treatment, diabetes and valve disease, alcohol use, and LVH. In additional analyses, we adjusted for body masss index (BMI), acknowledging that it may be along the causal pathway from physical inactivity to HF. We also evaluated for effect modification by BMI by incorporating corresponding interaction terms in the multivariable models and assessing statistical significance of the interaction terms at a P < 0.10 level. All analyses were repeated separately for incidence of HFPEF (censoring incident cases of HFREF at the time of that event) and HFREF (censoring incident cases of HFPEF at the time of that event).
We also evaluated the longitudinal relationship between changes in BMI and PAI as between the 19th (1985–1988) and 20th examinations on the incidence of HF using Cox proportional hazards regression; the sample size for these analyses was slightly smaller because participants were required to enter two successive examinations. In these secondary analyses, participants were grouped into four categories based on an increase vs. a decrease in PAI and/or BMI. Individuals in whom BMI decreased and PAI increased constituted the referent group with which the other groups were compared.
Data were analysed using SAS version 9.2, and a two-sided P-value of <0.05 was used to indicate statistical significance unless otherwise specified. All authors had full access to the data and take responsibility for the integrity of the data.
Results
Baseline characteristics
Table 1 displays the baseline characteristics of our study sample according to PAI tertiles. The sample consisted of 1142 elderly participants (Table 1). Approximately three-quarters of the participants had high blood pressure, and about half were on antihypertensive treatment. The distribution of PAI tertiles appears in the footnote to Table 1. Most individuals in the first tertile were sedentary. Those in the lowest PAI tertile were older, had higher BMI, and were more likely to have diabetes and valve disease.
Table 1.
Baseline characteristics of the study sample
| Characteristic | PAI tertile 1 (n = 376) | PAI tertile 2 (n = 376) | PAI tertile 3 (n = 390) | P-value |
|---|---|---|---|---|
| Age, years | 78 ± 7 | 76 ± 5 | 75 ± 5 | <0.01 |
| Women, % | 66 | 65 | 64 | 0.86 |
| Hypertension, % | 77 | 74 | 76 | 0.64 |
| Systolic BP, mmHg | 146 ± 23 | 146 ± 22 | 148 ± 22 | 0.60 |
| Diastolic BP, mmHg | 74 ± 12 | 76 ± 10 | 76 ± 11 | 0.02 |
| Pulse pressure, mmHg | 72 ± 20 | 70 ± 19 | 71 ± 18 | 0.53 |
| Total cholesterol, mg/dL | 211 ± 43 | 218 ± 49 | 216 ± 38 | 0.08 |
| HDL cholesterol, mg/dL | 47 ± 14 | 49 ± 16 | 51 ± 16 | 0.03 |
| Blood glucose, mg/dL | 105 ± 40 | 101 ± 31 | 102 ± 40 | 0.27 |
| Antihypertensive treatment, % | 53 | 52 | 47 | 0.27 |
| Diabetes, % | 14 | 10 | 8 | 0.01 |
| BMI, kg/m2 | 27.1 ± 5.2 | 26.4 ± 4.3 | 26.2 ± 4.3 | 0.03 |
| FEV1/FVC ratio | 70 ± 10 | 72 ± 8 | 72 ± 7 | 0.01 |
| Valve disease, % | 6 | 2 | 3 | 0.01 |
| Smoking, % | 10 | 12 | 9 | 0.35 |
BMI, body mass index; BP, blood pressure; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; PAI, physical activity index.
Tertile of PAI: T1, men, 24.9–30.0, women 24.2–29.8; T2, men, 30.1–34.3, women, 29.9–33.7; T3, men, 34.5–63.2, women, 33.8–57.6.
Physical activity and incidence of heart failure
On follow-up (mean 10 years; median 11.5 years, range 0.04–19.3 years), 250 participants developed HF, including 108 with HFPEF and 106 with HFREF (36 HF with unavailable EF). A total of 788 participants died during the follow-up period. Figure 1 shows the cumulative incidence of HF according to PAI tertile. With increasing level of physical activity, there was a decrease in the cumulative incidence of all HF. Table 2 shows the incidence rates of overall HF and of HFPEF and HFREF according to PAI tertile. Incidence rates of HF and its subtypes fell across PAI tertiles.
Figure 1.
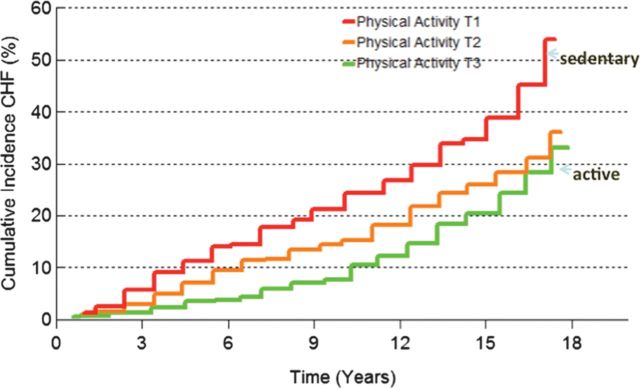
Cumulative incidence of incident heart failure according to physical activity tertile (unadjusted for competing events such as death).
Table 2.
Cumulative incidence rates of heart failure by tertile of physical activity
| Outcome | Physical activity level | HF events/ person-years of follow-up | Age- and-sex adjusted 10-year cumulative incidence (95% CI) |
|---|---|---|---|
| Overall HF | First tertile | 95/2594 | 0.20 (0.14–0.25) |
| Second tertile | 80/3082 | 0.16 (0.11– 0.21) | |
| Third tertile | 75/3417 | 0.10 (0.06–0.13) | |
| HFPEF | First tertile | 45/2594 | 0.10 (0.05–0.15) |
| Second tertile | 25/3082 | 0.06 (0.02, 0.09) | |
| Third tertile | 38/3417 | 0.04 (0.01–0.06) | |
| HFREF | First tertile | 38/2594 | 0.09 (0.04–0.13) |
| Second tertile | 38/3082 | 0.09 (0.05–0.13) | |
| Third tertile | 30/3417 | 0.05 (0.02, 0.08) |
CI, confidence interval; HF, heart failure; HFPEF, heart failure with preserved ejection fraction; HFREF, heart failure with reduced ejection fraction.
Table 3 shows the results of Cox models relating PAI tertiles to HF risk, and to the risk of HFPEF and HFREF. In age- and sex-adjusted models, the middle and highest PAI tertiles were associated with a 15–56% lower risk of any HF, of HFPEF, and of HFREF, with a statistically significant graded response across tertiles for any HF and HFREF (Table 3). In multivariable models, the significant association of PAI tertiles with any HF and with HFPEF was maintained, whereas the association with HFREF was attenuated (Table 3). As secondary analyses, multivariable models were additionally adjusted for the BMI. The association between PAI tertiles and HF remained significant with any HF (P = 0.01 for trend) and approached significance with HFPEF (P = 0.11 for trend). None of the interactions by BMI were statistically significant (all P > 0.10). Because adjustment for BMI attenuated the association between PAI and incident HF, we assessed the longitudinal relationship between changes in BMI and PAI on incident HF using data from participants who attended both the examination cycles 19 and 20. A decrease in PAI between these examinations (regardless of an increase or decrease in BMI) was significantly associated with an increased risk of HF (Table 4) .
Table 3.
Association of physical activity with all heart failure, heart failure with preserved ejection fraction, and heart failure with reduced ejection fraction
| Type of HF | No. of events/no. at risk | Model | Relative risk for HF (95% CI) associated with PAI tertiles |
P for trend across PAI tertiles | ||
|---|---|---|---|---|---|---|
| Tertile 1 | Tertile 2 | Tertile 3 | ||||
| Any HF | 250/1142 | Age- and sex-adjusted | Referent | 0.68 (0.50–0.92) | 0.57 (0.41–0.77) | <0.01 |
| Multivariable-adjusted | Referent | 0.74 (0.53–1.02) | 0.61 (0.44–0.85) | <0.01 | ||
| Multivariable-adjusted plus BMI | Referent | 0.84 (0.60–1.17) | 0.65 (0.46–0.91) | 0.01 | ||
| HFPEF | 108/1142 | Age- and sex-adjusted | Referent | 0.44 (0.27–0.72) | 0.59 (0.38–0.93) | 0.03 |
| Multivariable-adjusted | Referent | 0.45 (0.27–0.76) | 0.60 (0.38–0.97) | 0.04 | ||
| Multivariable- adjusted plus BMI | Referent | 0.54 (0.31–0.92) | 0.66 (0.41–1.07) | 0.11 | ||
| HFREF | 106/1142 | Age- and sex-adjusted | Referent | 0.85 (0.53–1.34) | 0.60 (0.37–0.99) | 0.04 |
| Multivariable-adjusted | Referent | 0.93 (0.57–1.51) | 0.68 (0.41–1.13) | 0.13 | ||
| Multivariable-adjusted plus BMI | Referent | 1.07 (0.64–1.79) | 0.69 (0.41–1.19) | 0.16 | ||
Multivariable models adjusted for age, sex, systolic blood pressure, hypertension treatment, diabetes, valve disease, alcohol use, and LV hypertrophy.
BMI, body mass index; CI, confidence interval; HF, heart failure; HFPEF, heart failure with preserved ejection fraction; HFREF, heart failure with reduced ejection fraction; PAI, physical activity index.
Table 4.
Predicting incident heart failure according to longitudinal changes in body mass index and physical activity index between examinations 19 and 20
| BMI/PAI categorya | No. of events/no. at risk | HRb (95% CI) | P-value |
|---|---|---|---|
| BMI decreased/PAI increased | 31/201 | Referent | Referent |
| BMI increased/PAI increased | 44/201 | 1.44 (0.89–2.31) | 0.14 |
| BMI Decreased/PAI decreased | 60/243 | 1.82 (1.15–2.87) | 0.01 |
| BMI increased/PAI decreased | 73/285 | 1.76 (1.13–2.76) | 0.01 |
BMI, body mass index; CI, confidence interval; HF, heart failure; HFPEF, heart failure with preserved ejection fraction; HFREF, heart failure with reduced ejection fraction; HR, hazard ratio; PAI, physical activity index.
aChange in BMI and PAI from cohort exam 19 to cohort exam 20.
bMultivariable models adjusted for age, sex, baseline BMI (exam 19), baseline PAI (exam 19), systolic blood pressure, hypertension treatment, diabetes, valve disease, alcohol use, and LV hypertrophy.
Discussion
Principal findings
In our longitudinal study of an elderly community-based sample we observed that lower physical activity is associated with higher incidence of HF. This association was consistent for both HFPEF and HFREF in age- and sex-adjusted analyses, but was attenuated for HFREF in multivariable analyses. Adjustment for BMI also attenuated the associations of PAI with HFPEF and HFREF. As noted above, we chose a sequential strategy for adjustment for standard risk factors because risk factors, including BMI, are very likely along the causal pathway from physical inactivity to HF. As such, including risk factors in the models (especially BMI) may represent an overadjustment. However, our results investigating the longitudinal association between serial changes in PAI and incident HF even when accounting for a change in BMI support the robustness of the relationship between PAI and incident HF. Overall, the temporality of the association, the presence of a dose response, the consistency of the association for both HFPEF and HFREF (in minimally adjusted models), an overall concordance of our results with the published literature, and the biological plausibility suggest that the observed association between physical inactivity and greater HF risk in older people may be a causal one. A less likely but alternative plausible explanation may be that individuals with pre-existing subclinical or undiagnosed cardiac dysfunction may reduce their activity level (reverse causality).
Comparison with the published literature
Data on the association of physical activity and HF are sparse. The Physicians' Health Study reported that vigorous physical activity is associated with a lower risk of HF in middle-aged male physicians.5 The NHANES I Epidemiologic Follow-up Study reported an association of low recreational physical activity with greater risk of HF in women but not in men.6 Neither study evaluated elderly individuals who are at the highest risk of HF or the association of physical activity with HFPEF and HFREF. The Physicians' Health Study did not assess less than vigorous physical activity, and the NHANES Study evaluated only recreational physical activity.5,6 The FINMONICA Study evaluated nearly 60 000 middle-aged participants using a mailed self-administered questionnaire to assess physical activity and reported an inverse association between physical activity (leisure time and occupational activity) and hospitalized HF identified via a hospital discharge registry.7
The present investigation extends the important observations made by these three previous reports to elderly individuals assessed with a comprehensive physical activity questionnaire that captured both work and leisure time physical activity of different grades. Additionally, our study broadens the protective effect of physical activity to HFPEF.
Mechanisms underlying the observed association
There are multiple mechanisms by which greater physical activity may lower the risk of HF, including beneficial effects on the risk factor profile, the heart, and the blood vessels.14 The favourable effects on cardiovascular risk factors include lower BMI, lower blood pressure, and better lipid and glycaemic profiles in individuals who exercise more.14 Beneficial effects of exercise on the heart include prevention of age-related cardiac remodelling, adaptive prohypertrophic effects, and the promotion of better cardiac systolic and diastolic function.14 The positive effects of exercise on the vasculature include improved endothelial function of conduit and resistance vessels and enhanced angiogenesis due to mobilization of endothelial progenitor cells.14
Strengths and limitations
The strengths of our study include the large older community-based sample (the segment of the population with higher HF risk), detailed assessment of physical activity (both work and recreational), and the evaluation of both HFPEF and HFREF incidence.
Limitations include the lack of more objective assessment of physical activity (e.g. with an accelerometer; questionnaire-based measurement of physical activity may be susceptible to recall bias), the missing information of EF in some participants who developed HF (which prevented their classification into HFPEF and HFREF), the relatively simplistic definition of HFPEF, lack of assessment of diastolic function using state-of-the-art echocardiographic measures, lower statistical power to evaluate relationships of PAI to HFREF vs. HFPEF (compared with all HF), a potential temporal bias, and the all-white ethnicity of our sample (that limits generalizability to other ethnic groups).
Conclusions
In our elderly community-based sample, greater physical activity was associated with lower risk of HFPEF. Our study extends previous findings of a protective effect of physical activity on HF risk to the elderly and to HFPEF.
Supplementary material
Supplementary material is available at European Journal of Heart Failure online.
Funding
The National Heart, Lung and Blood Institute (contract no. NO1-HC-25195).
Conflict of interest: none declared.
Supplementary Material
References
- 1.Owan TE, Redfield MM. Epidemiology of diastolic heart failure. Prog Cardiovasc Dis. 2005;47:320–332. doi: 10.1016/j.pcad.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 2.Mureddu GF, Agabiti N, Rizzello V, Forastiere F, Latini R, Cesaroni G, Masson S, Cacciatore G, Colivicchi F, Ugucciono M, Perucci CA, Boccanelli A on behalf of the PREDICTOR Study Group. Prevalence of preclinical and clinical heart failure in the elderly. A population-based study in Central Italy. Eur J Heart Fail. 2012;14:718–729. doi: 10.1093/eurjhf/hfs052. [DOI] [PubMed] [Google Scholar]
- 3.Djousse L, Driver JA, Gaziano JM. Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA. 2009;302:394–400. doi: 10.1001/jama.2009.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kenchaiah S, Sesso HD, Gaziano JM. Body mass index and vigorous physical activity and the risk of heart failure among men. Circulation. 2009;119:44–52. doi: 10.1161/CIRCULATIONAHA.108.807289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med. 2001;161:996–1002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- 6.Hu G, Jousilahti P, Antikainen R, Katzmarzyk PT, Tuomilehto J. Joint effects of physical activity, body mass index, waist circumference, and waist-to-hip ratio on the risk of heart failure. Circulation. 2010;121:237–244. doi: 10.1161/CIRCULATIONAHA.109.887893. [DOI] [PubMed] [Google Scholar]
- 7.McMurray JJ, Stewart S. Epidemiology, aetiology, and prognosis of heart failure. Heart. 2000;83:596–602. doi: 10.1136/heart.83.5.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bowling B, Fonarow GC, Patel K, Zhang Y, Feller MA, Sui X, Blair SN, Alagiakrishnan K, Aban IB, Love TE, Allman RM, Ahmed A. Impairment of activities of daily living and incident heart failure in community-dwelling older adults. Eur J Heart Fail. 2012;14:581–587. doi: 10.1093/eurjhf/hfs034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dawber TR, Meadors GF, Moore FE. Epidemiologic approaches to heart disease: the Framingham Study. Am J Public Health. 1951;41:279–286. doi: 10.2105/ajph.41.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kannel WB, Sorlie P. Some health benefits of physical activity. The Framingham Study. Arch Intern Med. 1979;139:857–861. [PubMed] [Google Scholar]
- 11.McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285:1441–1446. doi: 10.1056/NEJM197112232852601. [DOI] [PubMed] [Google Scholar]
- 12.Lee DS, Gona P, Vasan RS, Larson MG, Benjamin EJ, Wang TJ, Tu JV, Levy D. Relation of disease pathogenesis and risk factors to heart failure with preserved or reduced ejection fraction: insights from the framingham heart study of the national heart, lung, and blood institute. Circulation. 2009;119:3070–3077. doi: 10.1161/CIRCULATIONAHA.108.815944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cox DR, Oakes D. Analysis of Survival Data. London: Chapman and Hall; 1984. [Google Scholar]
- 14.Gielen S, Schuler G, Adams V. Cardiovascular effects of exercise training: molecular mechanisms. Circulation. 2010;122:1221–1238. doi: 10.1161/CIRCULATIONAHA.110.939959. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


