Abstract
Valid and reliable psychosocial measures for parents are lacking in the children’s sun protection literature. We examined the construct validity and reliability of measures of parents’ self-efficacy and perceived barriers specific to four sun protection behaviors in children: sunscreen, clothing, shade and limiting time outdoors. Melanoma survivors (N = 205) with children aged 12 years and younger completed an interview. Confirmatory factor analyses supported a four-factor structure of self-efficacy in which each factor was specific to one of the sun protection behaviors. This structure, consistent with Bandura’s conceptualization, suggests using behavior-specific scores. A bifactor model best fit the perceived barriers data. Each item loaded on both a general barriers factor and one of four behavior-specific factors. Based on the magnitude of general factor loadings relative to behavior-specific factor loadings, use of subscale scores or a total score is recommended. Correlations between self-efficacy measures (0.30–0.46) and between perceived barriers measures (0.22–0.42) suggested convergent validity. Correlations between self-efficacy and perceived barriers were strongest within behavior (–0.34 to −0.63), suggesting discriminant validity. Almost all measures were most strongly associated with corresponding behaviors, supporting construct validity. Reliabilities ranged from 0.72 to 0.90. Measures are valid and reliable for use in children’s sun protection studies.
Introduction
Excessive childhood sun exposure increases skin cancer risk [1, 2]. Parents directly provide and reinforce children’s sun protection [3, 4]. Parents’ attitudes and beliefs have been associated with sun protection in younger [5] and older [6] children. The specific sun protection behaviors that are recommended are applying and reapplying sunscreen; dressing in wide-brimmed hats and other protective clothing; staying in the shade and limiting time outdoors [3, 7]. These four distinct sun protection behaviors require different skills and steps. A systematic review conducted by the Task Force on Community Preventive Services (the Task Force) showed that many studies tested sun protection interventions for their effects on a composite behavioral outcome, which is a combination of specific sun protection behaviors [3]. Instead, the Task Force recommends that researchers examine intervention effects on each of the four specific sun protection behaviors [3]. Parental psychosocial determinants of children’s sun protection may be behavior specific. Furthermore, parents’ psychosocial constructs relevant to individual sun protection behaviors in children may mediate intervention effects. This research depends on valid and reliable measures of parents’ psychosocial constructs.
In this literature, validated psychosocial measures for parents are generally lacking (M. Tripp et al., in preparation). We examined the construct validity and reliability of new measures of two of the most frequently assessed sun protection psychosocial constructs in parents, self-efficacy and perceived barriers. Parents’ self-efficacy is positively associated with children’s sun protection [5, 8, 9] and mediates the association between parents’ perceived barriers and children’s sun protection [5]. Bandura conceptualized self-efficacy as behavior specific [10]. In Social Cognitive Theory (SCT), self-efficacy, or the belief that one can exercise control over behavior and produce desired changes by one’s actions, affects behavior both directly and indirectly through other determinants including outcome expectations, impediments and goals [10–12]. Parents’ perceived barriers is negatively associated with children’s sun protection [5, 8]. Perceived barriers originally was conceptualized in the Health Belief Model as influencing the likelihood of taking behavioral action [13]. Perceived barriers refers to potential negative aspects of a particular behavior that may act as impediments to undertaking the behavior [13]. This conceptualization suggests that perceived barriers may be behavior specific. Perceived barriers are distinct from objective social, environmental and economic barriers [14].
Measure validity is of primary importance and refers to the accuracy of a measure in assessing a construct [15]. Reliability is of secondary importance as a condition of validity [16]. Content validity, or how well a measure represents the construct, usually is determined through literature review and expert judgment [15]. Because sun protection psychosocial constructs cannot be observed directly, a suitable gold standard is lacking, limiting assessment of criterion validity [17]. Construct validity is of paramount importance as the degree to which empirical associations between measures of constructs are consistent with theory based or hypothesized associations between constructs [15, 16]. This includes the extent to which measures of the same construct are associated (convergent validity) and measures of different constructs are not associated (discriminant validity) [15]. Furthermore, factorial validity is the degree to which a hypothesized model of a measure’s underlying factor structure fits the data. Factor analytic findings also provide valuable information about measure dimensionality to guide scoring, a practical concern for researchers.
Current study
Theory-based associations between self-efficacy and perceived barriers measures, and between these measures and behavior, informed construct validity. Additionally, alternative, plausible measurement models based on theory and empirical findings were tested and compared to assess factorial validity and measure dimensionality. Reliability also was determined.
It is a widespread practice in the children’s sun protection literature to treat psychosocial measures as unidimensional (as if they assess a single construct), even when measures contain multiple items assessing different sun protection behaviors (M. Tripp et al., in preparation). Based on this empirical literature, we conducted analyses to determine whether our self-efficacy and perceived barriers measures were unidimensional, which would support the use of a total score.
Alternatively, the theoretical bases of self-efficacy and perceived barriers suggest that it is reasonable to conceptualize their measures as multidimensional and behavior specific. Thus, we tested models that hypothesized a behavior-specific factor structure underlying measures. If this multidimensional model adequately fits the data, then behavior-specific scores, not a total score, would be warranted.
It may be expected that behavior-specific factors would be highly correlated given that they are measures of the same construct (e.g. self-efficacy). We tested a hierarchical model that allows for multidimensionality while suggesting that a higher-level construct explains why behavior-specific factors are correlated. Adequate fit of this empirically based model suggests the use of total and behavior-specific subscale scores.
It is not possible in the hierarchical model, however, to clearly determine the utility of subscales (behavior-specific factors) because they are modeled on a different conceptual level (i.e. first order) than the higher-level construct (i.e. second order). Whether a subscale is plausible, and subscale scores are warranted, depends on the extent of information provided by the subscale that is not already provided by the general construct or factor (e.g. self-efficacy). Controlling for the general factor, do items associated with behavior-specific factors provide enough information to justify subscale scores? To answer this, we tested a bifactor model, which is uncommon in the health behavior literature but has been reported in other empirical literatures (e.g. quality of life and psychopathology) to determine measure dimensionality and subscale plausibility [18–23].
Community-based studies and national surveys of sun protection have collected data from parents whose children vary widely in age [24–26], as in this study. This practice underscores the need for psychosocial measures that are valid and reliable for use in these parents. Notably, we examined measures in melanoma survivors. Their children are at increased melanoma risk due to family history [27]. Despite the increased risk of these children, there have not been any studies of the validity and reliability of psychosocial measures in parents who are melanoma survivors.
Materials and methods
Data source
We identified 795 individuals diagnosed between April 1999 and April 2005 with in situ, localized or microscopic stage III melanoma from a hospital-based cancer registry. We mailed an informed consent/authorization statement and a letter describing an interview study. This interview study aimed to describe the prevalence and correlates of sun protection in children of melanoma survivors (M. Tripp et al., in preparation). Data from this interview study were analysed for this study.
Eligibility screening and informed consent for the interview study were conducted by telephone. Melanoma survivors were eligible if they had a child aged 12 years or younger; were at least 18 years old; and were able to speak, read and write English. All survivors meeting eligibility requirements were recruited regardless of race, ethnicity or gender. Of the 795 survivors, 456 (57%) completed eligibility screening. Remaining survivors (n = 339) were not interested (n = 48) or study personnel were not able to reach them (n = 291). Of the 456 survivors screened, 232 (51%) were eligible. Ineligible survivors (n = 224) did not have a child in the eligible age range. Of the 232 eligible survivors, 230 (99%) agreed to participate and 205 of these (89%) completed the interview.
Telephone interviews were conducted from July 2005 to March 2006. If the survivor had more than one child in the eligible age range, one child was randomly selected as the referent for the interview. All questions were directed to the survivor; the child did not answer any questions. Self-efficacy and perceived barriers measures were included within the interview that assessed several sets of variables relevant to children’s sun protection. Most interviews took 50–60 min to complete. Respondents received a $20 gift card for participating. The study was approved by the study institution’s Institutional Review Board.
Measures
New measures assessed parents’ self-efficacy and perceived barriers specific to four distinct sun protection behaviors for children (Table I). Measures were developed based on our survey research in preschool parents [9] and qualitative research in melanoma survivors (M. Tripp et al., in preparation). Measures did not assess constructs in the context of melanoma risk or diagnosis, making them appropriate for parents with or without a melanoma diagnosis.
Table I.
Descriptive statistics for sun protection self-efficacy and perceived barriers items
| Item label | Itema | M (SD) | Skewness | Kurtosis |
|---|---|---|---|---|
| Self-efficacy for protecting child with sunscreen (sunscreen self-efficacy) | ||||
| 30 min | You can consistently put sunscreen on your child 30 minutes before he/she goes outdoors. | 3.65 (1.12) | −0.35* | −0.78* |
| Reapply sunscreen | You can consistently reapply sunscreen to your child after he/she has been outdoors two hours or less. | 3.88 (1.12) | −0.63*** | −0.57 |
| Exposed areas | You can consistently put sunscreen on all exposed areas on your child not covered by clothing. | 4.33 (0.94) | −1.38*** | 1.28*** |
| Don’t have time | You can put sunscreen on your child if you don’t have much time. | 4.07 (0.98) | −0.84*** | −0.03 |
| Self-efficacy for protecting child with hats and clothing (clothing self-efficacy) | ||||
| Wear hat | You can ensure that your child wears a wide-brimmed hat while he/she is outdoors. | 2.17 (1.27) | 0.81*** | −0.49 |
| Wear clothing | You can ensure that your child wears clothing that covers most of his/her skin while he/she is outdoors. | 3.28 (1.22) | −0.30 | −0.91** |
| Hot outside | When it’s hot outside, you can ensure that your child is dressed so that most of his/her skin is covered. | 2.78 (1.23) | 0.13 | −0.88** |
| Self-efficacy for protecting child with shade (shade self-efficacy) | ||||
| Stay in shade | You can convince your child to stay in shaded areas when he/she is outside. | 3.12 (1.18) | −0.19 | −0.74* |
| Find shade | You can create or find outdoor shaded areas for your child. | 3.91 (1.05) | −0.80*** | −0.11 |
| Self-efficacy for limiting child’s time outdoors (limiting time self-efficacy) | ||||
| Limit time | You can limit the amount of time your child spends outdoors during the hours of 10:00 a.m. to 4:00 p.m. | 4.02 (1.00) | −0.65*** | −0.72* |
| Child stay out | You can limit the amount of time your child spends outdoors during the hours of 10:00 a.m. to 4:00 p.m. even if your child wants to stay out longer. | 4.03 (0.95) | −0.65*** | −0.42 |
| Others stay out | You can limit the amount of time your child spends outdoors during the hours of 10:00 a.m. to 4:00 p.m. if others whom you are with are letting their children stay out longer. | 3.60 (1.10) | −0.31 | −0.72* |
| Perceived barriers to protecting child with sunscreen (sunscreen perceived barriers) | ||||
| Too much time | It takes too much time to apply sunscreen to all areas on my child not covered by clothing. | 1.46 (0.84) | 1.91*** | 3.03*** |
| Forget to take | I forget to take sunscreen on outdoor trips with my child. | 1.50 (0.77) | 1.71*** | 3.05*** |
| Too expensive | Sunscreen is too expensive to use routinely. | 1.22 (0.65) | 3.35*** | 11.74*** |
| Perceived barriers to protecting child with hats and clothing (clothing perceived barriers) | ||||
| Too hot | It is too hot in the summer for my child to wear clothing that covers most of his/her skin. | 3.48 (1.29) | −0.51** | −0.87* |
| Clothing not fashionable | My child does not think it is fashionable to wear clothing that covers most of his/her skin. | 2.49 (1.51) | 0.51** | −1.23*** |
| Hats mess hair | Hats mess up my child’s hair. | 1.63 (1.11) | 1.81*** | 2.28*** |
| Hassle | It is a hassle to make sure that my child wears a wide-brimmed hat that shades the face, ears and neck. | 2.95 (1.48) | 0.03 | −1.39*** |
| Does not like hats | My child does not like to wear wide-brimmed hats that shade the face, ears and neck. | 3.74 (1.38) | −0.65*** | −0.97** |
| Hats not fashionable | My child does not think it is fashionable to wear wide-brimmed hats that shade the face, ears and neck. | 3.15 (1.63) | −0.13 | −1.61*** |
| Perceived barriers to protecting child with shade (shade perceived barriers) | ||||
| Stay shade | It's difficult to convince my child to stay in the shade. | 2.87 (1.21) | 0.07 | −0.85* |
| Trouble | It's too much trouble to create shaded areas outdoors for my child using umbrellas and other coverings. | 1.97 (1.04) | 0.91*** | 0.09 |
| Hard to find | It's hard to find shaded outdoor play areas for my child. | 2.56 (1.28) | 0.33 | −1.04** |
| Does not like shade | My child does not like to stay in the shade unless it is really hot outside. | 2.76 (1.28) | 0.14 | −1.09** |
| Forget to create | I forget to bring canopies or umbrellas to create shaded areas when I go outside with my child. | 2.46 (1.24) | 0.50** | −0.62 |
| Perceived barriers to limiting child’s time outdoors (limiting time perceived barriers) | ||||
| Interrupt fun | If I limit the time my child spends outside during the hours of 10:00 a.m. to 4:00 p.m., I will interrupt my child’s fun. | 2.42 (1.35) | 0.46** | −1.03** |
| Hard to schedule | It's hard to schedule outdoor activities for my child for the morning or late afternoon. | 2.33 (1.24) | 0.49** | −0.95** |
| Likes outside | My child likes to be outside for long periods of time in the middle of the day. | 2.67 (1.30) | 0.33 | −1.02** |
aEach item was scored on a scale of 1–5. For self-efficacy items, higher scores reflected higher levels of self-efficacy. For perceived barriers items, higher scores reflected higher levels of perceived barriers. *P < 0.05. **P < 0.01. ***P < 0.001.
Measures assessed parents’ self-efficacy for using sunscreen on children (four items), dressing children in hats and clothing that cover most of the body (three items), protecting children with shade (two items) and limiting children’s time outdoors midday (three items). Self-efficacy items had 5-point response scales ranging from not confident at all (1) to extremely confident (5). Items assessed parents’ perceived barriers to using sunscreen on children (three items), dressing children in hats and clothing that cover most of the body (six items), protecting children with shade (five items) and limiting children’s time outdoors midday (three items). Perceived barriers items had 5-point response scales ranging from strongly disagree (1) to strongly agree (5).
Behavioral measures of sunscreen (two items), clothing (four items) and shade (one item) had 5-point response scales ranging from always (1) to never (5). Sunscreen items assessed how often sunscreen with an SPF of at least 15 is put on the child 30 min before going outdoors and reapplied within 2 h. Clothing items assessed how often the child wears a hat with a wide brim of 4 inches or more to shade the face, ears and neck; a long-sleeved shirt; shorts to the knees or longer or pants to the mid-calf; and long pants to the shoe. The shade item asked how often the child is in the shade. Item scores were reverse-coded so that higher scores reflected more frequent behavior. For the sunscreen and clothing measures, item scores were averaged to form a behavior-specific index. Time outdoors was measured by parental report of the number of hours the child spent outdoors between 10:00 a.m. and 4:00 p.m. on a typical weekend day.
Statistical analyses
Factorial validity
We conducted confirmatory factor analyses (CFA) to test and compare alternative measurement models of self-efficacy and perceived barriers. The behavior-specific nature of these constructs and the common empirical uses of their measures support testing the same hypothesized factor structures for both sets of measures. First, we hypothesized a unidimensional, or one-factor model, in which all items loaded on one factor (Fig. 1). This model suggests that one common factor explains the covariation between items and the use of a total score is justified. Second, we hypothesized a correlated, four-factor model in which each factor was specific to one of the four distinct sun protection behaviors. This model of separate but correlated dimensions suggests the use of behavior-specific scores. Third, we hypothesized a second-order model in which each of the four behavior-specific measures was a first-order factor and a second-order factor accounted for the correlations between the four, first-order factors. Adequate fit of this hierarchical model suggests the use of total and subscale scores. Finally, we hypothesized a bifactor model in which each item loaded on both a general factor and one of four behavior-specific factors. Factors are uncorrelated to enable us to determine whether a behavior-specific factor contributes variance to the item above and beyond the variance contributed by a general factor that accounts for the covariation between all items. Findings suggest the plausibility of subscales and whether the measure may be scored as unidimensional [22].
Fig. 1.
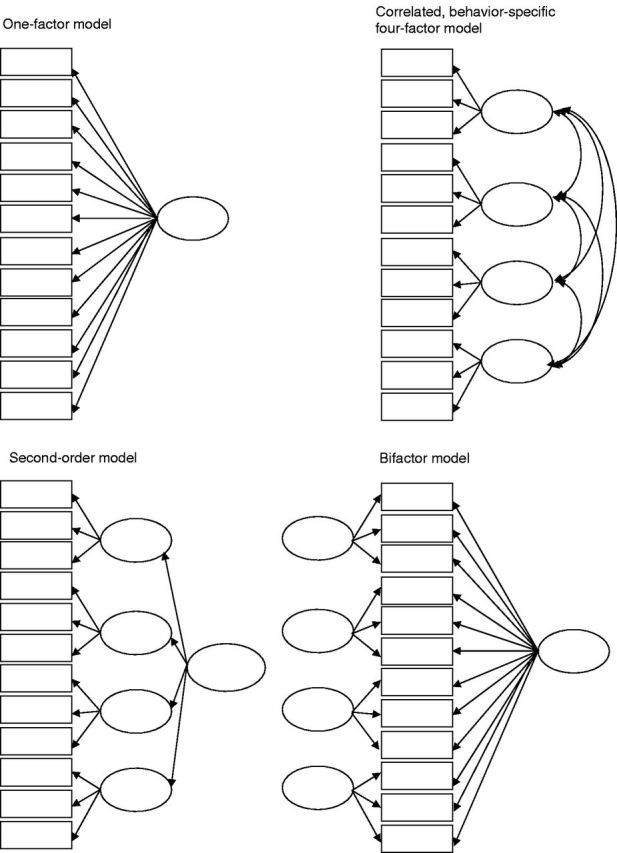
Graphical representations of hypothesized models. Rectangles represent observed variables (items) and ovals represent factors (latent variables). Errors, disturbances and item labels have been omitted for clarity.
We analysed CFA models in Mplus version 4.1 [28] and fixed the variance of each latent variable to one to scale the factors. Most univariate skewness and about half of univariate kurtosis values were less than |1.0| (Table I). Because items exhibited multivariate non-normality based on a significant two-sided multivariate kurtosis test of fit and most items displayed floor or ceiling effects, we treated items as ordered, categorical. We ran models using the Weighted Least Squares with Mean and Variance Adjustment (WLSMV) estimator which is recommended for CFA procedures with ordered, categorical data [28, 29]. Less than 1% of the data were missing and data from all respondents were included in analyses.
The chi-square goodness-of-fit test is a test of overall model fit [30]. We also examined multiple indices of model fit: the comparative fit index (CFI) (values of at least 0.90 are considered to indicate good model fit and higher values indicate better fit) [31, 32]; the Tucker−Lewis index (TLI) (higher values up to 1.0 indicate good fit) [30, 33]; the weighted root mean square residual (WRMR) (values ≤ 1.0 may indicate good model fit, with smaller values indicating better model fit) [34]; and the root mean square error of approximation (RMSEA) [35]. RMSEA values less than 0.08 indicate adequate fit and values less than 0.05 indicate good fit [36]. More stringent cutoff values for maximum likelihood-based indices have been suggested (e.g. CFI and TLI close to 0.95 and RMSEA close to 0.06) [37]. It is challenging to decide upon cutoff criteria because values of fit indices may depend on the type of model under investigation [38] and sample size [39]. We compared nested, competing measurement models using chi-square difference tests. For models estimated by WLSMV in Mplus, only the P value is interpreted [28]. A non-significant P value indicates that there is not a significant difference in the overall fit of the models.
Convergent and discriminant validity
We computed scale scores for the self-efficacy and perceived barriers measures and calculated Pearson correlations between these measures. Convergent validity was examined by assessing the extent to which measures of the same construct were associated. It was expected that the four self-efficacy measures would be positively associated with each other and the four perceived barriers measures would be positively associated with each other. A measure has discriminant validity if it is not associated with measures of different constructs. Self-efficacy and perceived barriers are different constructs but it was expected based on SCT that self-efficacy and perceived barriers measures would be negatively associated [12]. Thus, weaker associations between different constructs, compared with the same constructs, would provide evidence of discriminant validity. Because psychosocial measures were behavior specific, it was expected that negative associations between self-efficacy and perceived barriers measures would be strongest within each sun protection behavior.
Construct validity would be further suggested if behavior-specific psychosocial measures (e.g. sunscreen self-efficacy) were associated with measures of the corresponding sun protection behavior (e.g. sunscreen) and, to a lesser degree, with measures of other sun protection behaviors (e.g. clothing, shade and time outdoors). Self-efficacy would be positively associated with sunscreen, clothing and shade behaviors and negatively associated with time outdoors [10]. Perceived barriers would be negatively associated with sunscreen, clothing and shade behaviors and positively associated with time outdoors [13].
Reliability
We calculated Cronbach’s coefficient alpha [40], a commonly reported estimate of internal consistency. Alphas of 0.70 are reasonable for short measures [16]. Coefficient alpha has limitations such as not allowing for correlated errors of measurement [41] and representing the lower bound of the reliability estimate by assuming equal factor loadings [42]. Thus, we also estimated reliability using indicator loadings and error variances from the measure’s single-factor CFA model [43]. Reliability estimates above 0.60 are recommended [44].
Results
Characteristics of melanoma survivors and their children
Most (70%) of the respondents (melanoma survivors) were female. The mean age was 39 years. Almost all (99%) identified themselves as White. Relatively few (6%) self-reported their ethnicity as Hispanic or Latino. Most survivors were graduates of college or graduate school (78%), were married (93%), had been diagnosed with one melanoma (90%), were diagnosed with early-stage melanoma (87%) and did not have a melanoma family history in a first-degree relative (87%). The mean time since diagnosis was 3.3 years. About half (47%) of the children were female. Children ranged in age from infant to 12 years. The mean age was 7 years. Almost all survivors (98%) self-reported their children’s race as White and 7% reported their children’s ethnicity as Hispanic or Latino. Survivors had moderate to high levels of self-efficacy for protecting children with sunscreen and shade and limiting their time outdoors. Survivors had less self-efficacy for dressing children in protective clothing. Survivors perceived low (sunscreen) to moderate (clothing) levels of barriers to children’s sun protection.
Factorial validity
Self-efficacy measurement models
The one-factor model provided a poor fit to the data according to the chi-square test and fit indices (Table II). Chi-square tests of the four-factor and second-order models also were significant but these models provided an adequate or good fit according to fit indices. The bifactor model did not fit the data according to the chi-square test. This model’s CFI, TLI and WRMR values suggested good fit but the RMSEA was higher than recommended.
Table II.
Goodness-of-fit of confirmatory factor analytic models of sun protection self-efficacy and perceived barriers items
| Model | χ2 | df a | P | CFI | TLI | RMSEA | WRMR |
|---|---|---|---|---|---|---|---|
| Self-efficacy | |||||||
| One-factor | 286.37 | 22 | 0.0000 | 0.802 | 0.847 | 0.242 | 1.979 |
| Four-factor | 35.79 | 21 | 0.0231 | 0.989 | 0.991 | 0.059 | 0.617 |
| Second-order | 43.14 | 22 | 0.0045 | 0.984 | 0.988 | 0.068 | 0.697 |
| Bifactor | 48.55 | 20 | 0.0004 | 0.979 | 0.982 | 0.083 | 0.663 |
| Perceived barriers | |||||||
| One-factor | 307.99 | 44 | 0.0000 | 0.716 | 0.800 | 0.171 | 1.658 |
| Four-factor | 111.58 | 48 | 0.0000 | 0.932 | 0.956 | 0.080 | 0.895 |
| Second-order | 107.35 | 46 | 0.0000 | 0.934 | 0.956 | 0.081 | 0.926 |
| Bifactor | 88.02 | 42 | 0.0000 | 0.950 | 0.963 | 0.073 | 0.787 |
By the chi-square difference test, the four-factor model provided a significantly better fit to the data than did the one-factor model (P = 0.0000) or second-order model (P = 0.0142). The bifactor model fit significantly better than did the one-factor model (P = 0.0000). The bifactor model was not significantly different from the second-order model (P = 0.6561). The bifactor and four-factor models could not be compared using the chi-square difference test because they were not nested. Indices such as Akaike’s Information Criterion [45], recommended to compare non-nested models, are not available for WLSMV estimation [28]. However, the chi-square test’s P value and values of fit indices were more favorable for the four-factor model, suggesting that this model provided the best fit.
Overall, findings suggest that a behavior-specific factor structure underlies the self-efficacy measures. All indicators in the four-factor model were significantly associated (P < 0.001) with their hypothesized factors and all but one had substantial loadings, ranging from 0.67 to 0.94 (Fig. 2). ‘Wear hat’ had a relatively low loading (0.56), suggesting that it was the weakest indicator of the clothing-specific factor. Correlations between self-efficacy factors were significant (P < 0.001) and moderate, ranging from 0.43 to 0.61.
Fig. 2.
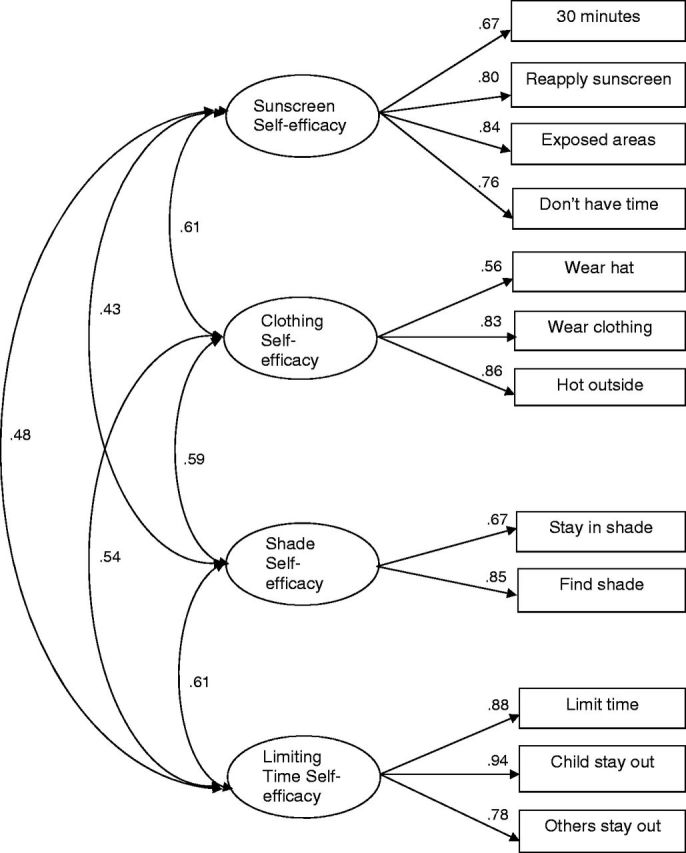
Factor loadings and correlations in the correlated, behavior-specific four-factor model of self-efficacy measures. All indicators in the four-factor model were significantly associated (P < 0.001) with their hypothesized factors. Correlations between the self-efficacy factors were significant (P < 0.001).
Perceived barriers measurement models
The one-factor model was a poor fit (Table II). The chi-square tests of the four-factor and second-order models were significant but these models provided an adequate or good fit to the data according to CFI and TLI values. The RMSEA of the four-factor model was at the recommended maximum for adequate fit (0.080). The RMSEA of the second-order model was a little higher (0.081). The bifactor model did not fit well according to the significant chi-square test but CFI, TLI and WRMR values suggested good fit while the RMSEA suggested adequate fit.
The four-factor model provided a significantly better fit to the data than did the one-factor model (P = 0.0000). The four-factor and second-order models were not significantly different in terms of overall fit (P = 0.0890). The bifactor model fit significantly better than did the one-factor (P = 0.0000) and second-order model (P = 0.0003). The bifactor and four-factor models were not nested so could not be compared statistically. However, the bifactor model had more favorable fit indices, suggesting that it provided better fit. Overall, findings suggested that the bifactor model provided the best fit to the data.
In the bifactor model, loadings for the general perceived barriers factor were significant (P < 0.001) and ranged from 0.33 to 0.67 (Fig. 3). Except for ‘too hot,’ all behavior-specific factor loadings also were significant (P < 0.05, 0.01 or 0.001), ranging from 0.25 to 0.87. The non-significant loading of ‘too hot’ on the clothing factor suggests that this factor did not contribute any variance to this item beyond that contributed by the general perceived barriers factor. Items that loaded more strongly on their behavior-specific factors than the general factor may assess constructs that are highly distinct from the general factor. Less than half of the items were more strongly associated with the behavior-specific factor.
Fig. 3.
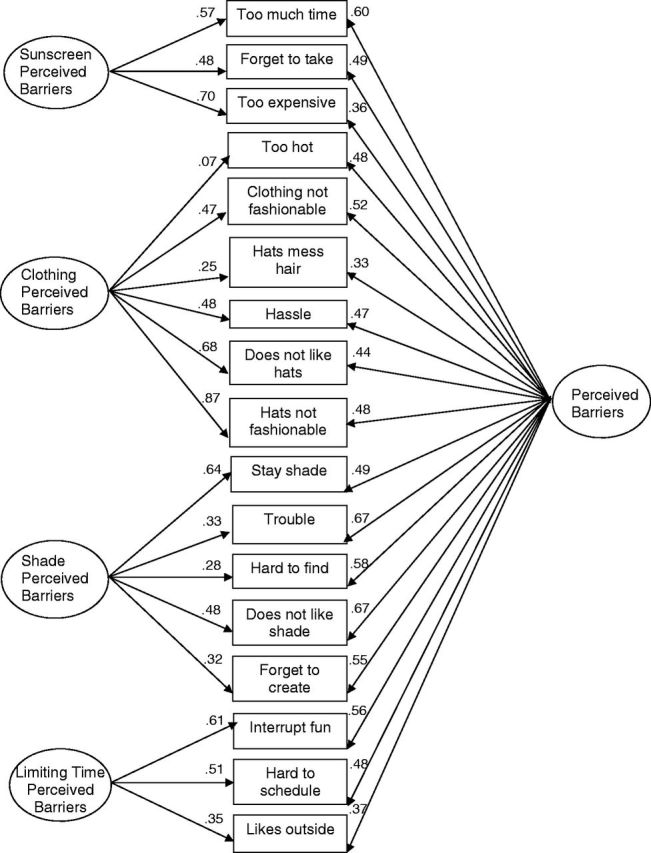
Factor loadings for the perceived barriers items in the bifactor model. All loadings for the general barriers factor were significant (P < 0.001). Except for ‘too hot,’ all behavior-specific factor loadings were significant (P < 0.05, 0.01 or 0.001).
Convergent and discriminant validity
Positive correlations between self-efficacy measures and positive correlations between perceived barriers measures were significant and moderate, suggesting convergent validity (Table III). Negative associations between self-efficacy and perceived barriers measures were strongest within behavior, suggesting discriminant validity. Seven of the measures were most strongly associated with corresponding behavior measures, providing additional evidence of construct validity (Table IV). Self-efficacy and perceived barriers measures either had no association with measures of different behaviors, or were associated to a lesser degree, with the exception of limiting time self-efficacy which had a slightly stronger association with shade behavior than with the number of hours spent outdoors midday. As expected, self-efficacy measures were positively associated with measures of sunscreen, clothing and shade behaviors and negatively associated with time outdoors. Perceived barriers measures were negatively associated with sunscreen, clothing and shade measures, and positively associated with time outdoors.
Table III.
Descriptive statistics and intercorrelations between self-efficacy and perceived barriers scales
| Scalea | M (SD) | α | Reliabilityb | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sunscreen self-efficacy | 3.98 (0.81) | 0.78 | 0.85 | |||||||
| 2. Clothing self-efficacy | 2.74 (0.99) | 0.71 | 0.79 | 0.46** | ||||||
| 3. Shade self-efficacy | 3.51 (0.96) | 0.67 | 0.72 | 0.30** | 0.43** | |||||
| 4. Limiting time self-efficacy | 3.88 (0.89) | 0.85 | 0.90 | 0.36** | 0.42** | 0.43** | ||||
| 5. Sunscreen perceived barriers | 1.40 (0.57) | 0.63 | 0.80 | −0.34** | −0.14* | −0.18** | −0.24** | |||
| 6. Clothing perceived barriers | 2.90 (0.95) | 0.76 | 0.83 | −0.22** | −0.59** | −0.27** | −0.37** | 0.28** | ||
| 7. Shade perceived barriers | 2.53 (0.90) | 0.80 | 0.85 | −0.27** | −0.32** | −0.63** | −0.37** | 0.40** | 0.42** | |
| 8. Limiting time perceived barriers | 2.48 (1.00) | 0.66 | 0.73 | −0.24** | −0.24** | −0.30** | −0.45** | 0.22** | 0.39** | 0.40** |
α, Cronbach’s coefficient alpha. aPsychosocial items were scored on a scale of 1–5. Higher scores reflected higher levels of self-efficacy and higher levels of perceived barriers. bReliability was calculated based on indicator loadings and error variances from the single-factor CFA model for the measure. *P < 0.05. **P < 0.01.
Table IV.
Associations between self-efficacy and perceived barriers scales and sun protection behavior
| Behavior |
||||
|---|---|---|---|---|
| Scalea | Sunscreen | Clothing | Shade | Time outdoors |
| Sunscreen self-efficacy | 0.30** | 0.17* | 0.17* | −0.06 |
| Clothing self-efficacy | 0.16* | 0.47** | 0.30** | −0.16* |
| Shade self-efficacy | 0.25** | 0.14* | 0.40** | −0.10 |
| Limiting time self-efficacy | 0.20** | 0.12 | 0.25** | −0.24** |
| Sunscreen perceived barriers | −0.35** | 0.01 | −0.13 | 0.07 |
| Clothing perceived barriers | −0.21** | −0.32** | −0.28** | 0.19** |
| Shade perceived barriers | −0.28** | −0.14* | −0.47** | 0.12 |
| Limiting time perceived barriers | −0.08 | −0.08 | −0.21** | 0.35** |
aPsychosocial items were scored on a scale of 1–5. Higher scores reflected higher levels of self-efficacy and higher levels of perceived barriers. Sunscreen, clothing and shade behavior items also were scored on a scale of 1–5; higher scores reflected more frequent behavior. Time outdoors measured the number of hours outdoors between the hours of 10:00 a.m. and 4:00 p.m. *P < 0.05. **P < 0.01.
Reliability
All coefficient alphas exceeded 0.60; at least half were >0.70 (Table III). CFA-based reliability estimates ranged from 0.72 to 0.90, suggesting that measures were adequately reliable and coefficient alpha underestimated reliability.
Discussion
CFA results suggested that these measures of parents’ self-efficacy and perceived barriers are valid and reliable. There was support for a four-factor, behavior-specific structure underlying the self-efficacy measures, consistent with Bandura’s conceptualization of self-efficacy. Thus, behavior-specific scores would be warranted. A bifactor model provided the best fit to the perceived barriers data. In this model, more than half of the perceived barriers items were more strongly associated with the general factor, which would support the use of a total scale score. However, for a few of these items, the general factor loadings were only slightly larger in magnitude than the behavior-specific factor loadings. Thus, we recommend computing behavior-specific subscale scores or a total scale score. Subscale scores may be more helpful when tailoring interventions to increase specific sun protection behaviors while a total scale score may be advised when examining perceived barriers as a determinant of a composite measure of sun protection behavior. The pattern and magnitude of associations between the behavior-specific self-efficacy and perceived barriers measures, and between these measures and children’s sun protection behaviors, further provided strong evidence of the construct validity of these theory-based measures for parents.
Some items assessed self-efficacy at different levels of challenge or barriers to performance, as recommended by Bandura [10]. Writing all items in this way may more adequately assess self-efficacy. For example, clothing self-efficacy items could be written to include barriers such as comfort and convenience. Future research is needed to determine whether it is informative to assess perceived barriers separately when they are captured within self-efficacy measures.
Limiting time self-efficacy was significantly associated with the number of hours outdoors (the measure of limiting time behavior), as expected, but this self-efficacy measure had a slightly stronger association with shade behavior. Because self-efficacy items had behavior-specific wording, a stronger association between limiting time self-efficacy and the corresponding behavior may be achieved by assessing limiting time behavior explicitly (e.g. ‘How often do you limit your child’s time outdoors?’). The limiting time self-efficacy measure may be enhanced by adding items to assess self-efficacy regarding scheduling.
The perceived barriers measures may be multidimensional due to item content. This is reasonable considering the potentially different barriers to specific sun protection behaviors. In the perceived barriers bifactor model, behavior-specific factors contributed substantial independent variance, beyond that accounted for by the general factor, to less than half of the items. Items that had higher loadings on their behavior-specific factors may provide a starting point for further development of behavior-specific measures. ‘Too hot’ was the only item with a non-significant loading on the behavior-specific factor. The content of this item is relevant, so removal is not advised. Unlike other items, ‘too hot’ referred to summer. Removing that reference would eliminate distinctive wording and focus content on heat as a barrier. Adding items to assess perceived clothing barriers related to other practical considerations (e.g., comfort, convenience and outdoor activity) may enhance this measure. In structural equation models, general and behavior-specific factors, each controlling for the variance due to the other, may make independent contributions to external variables such as children’s sun protection.
There may be plausible models that were not examined. However, the adequately fitting models appear to reasonably describe the data given fit indices and model justification. The chi-square test of exact model fit was significant for each model tested. Given the relatively small sample size, this significance cannot be dismissed. Models based on behavioral science theory typically provide an approximate explanation of associations between variables. Measure refinement and examination of additional models may further inform factor structures underlying these measures. Future research to replicate findings is warranted, particularly for the bifactor model which is understudied.
This study was conducted in a unique population, melanoma survivors, and results may not generalize to a population of parents who have not had melanoma. Because of their experiences with melanoma, or their awareness of their children’s increased risk, parents who have had melanoma may be more likely to respond in a socially desirable way. Furthermore, they may have more positive responses given their potential for more experience with sun protection. Further study is needed to determine whether measures may be enhanced by including items grounded in survivors’ melanoma experiences. Additionally, these measures should be examined in parents who have not had melanoma, to determine whether factor structures in this study adequately fit the data in these parents.
Melanoma incidence is highest in Whites as reflected by the hospital-based registry sample. Most respondents had high levels of education, which is consistent with studies that have shown that socioeconomic characteristics, particularly higher levels of education, are associated with increased melanoma incidence [46]. We were unable to compare respondents with non-respondents on demographic or disease-related variables. The patient registry did not maintain records on whether patients had children in the eligible age range. Because of the relatively small sample size, it was not possible to examine factorial invariance pertaining to demographic, disease-related or other variables that may affect item interpretation. Future studies in diverse samples would present an opportunity to determine whether measurement models are invariant across racial and ethnic groups and education levels.
This study makes a significant contribution to the skin cancer prevention literature, which contains few detailed assessments of the validity and reliability of psychosocial measures. We present evidence of the construct validity and reliability of measures of parents’ self-efficacy and perceived barriers regarding children’s sun protection. Our study of behavior-specific psychosocial measures, particularly in an understudied population of melanoma survivors, is novel. Study findings have implications for the conceptualization and assessment of parents’ self-efficacy and perceived barriers.
Acknowledgements
Data management services were provided by the Patient-Reported Outcomes, Survey & Population Research shared resource, a part of the University of Texas MD Anderson Cancer Center’s CORE grant funded by the National Cancer Institute at the National Institutes of Health [CA016672].
Funding
American Cancer Society [RSGPB 04-010-01-CPPB to E.R.G.].
Conflict of interest statement
None declared.
References
- 1.Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. Eur J Cancer. 2005;41:45–60. doi: 10.1016/j.ejca.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 2.Corona R, Dogliotti E, D'Errico M, et al. Risk factors for basal cell carcinoma in a Mediterranean population: role of recreational sun exposure early in life. Arch Dermatol. 2001;137:1162–8. doi: 10.1001/archderm.137.9.1162. [DOI] [PubMed] [Google Scholar]
- 3.Saraiya M, Glanz K, Briss PA, et al. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiation: a systematic review. Am J Prev Med. 2004;27:422–66. doi: 10.1016/j.amepre.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 4.Hill D, Dixon H. Promoting sun protection in children: rationale and challenges. Health Educ Behav. 1999;26:409–17. doi: 10.1177/109019819902600310. [DOI] [PubMed] [Google Scholar]
- 5.Turner LR, Mermelstein RJ. Psychosocial characteristics associated with sun protection practices among parents of young children. J Behav Med. 2005;28:77–90. doi: 10.1007/s10865-005-2565-9. [DOI] [PubMed] [Google Scholar]
- 6.O'Riordan DL, Geller AC, Brooks DR, et al. Sunburn reduction through parental role modeling and sunscreen vigilance. J Pediatr. 2003;142:67–72. doi: 10.1067/mpd.2003.mpd039. [DOI] [PubMed] [Google Scholar]
- 7.American Cancer Society. Cancer Facts & Figures 2012. Atlanta, GA: American Cancer Society; 2012. [Google Scholar]
- 8.Lescano CM, Rodrigue JR. Skin cancer prevention behaviors among parents of young children. Child Health Care. 1997;26:107–14. [Google Scholar]
- 9.Tripp MK, Carvajal SC, McCormick LK, et al. Validity and reliability of the parental sun protection scales. Health Educ Res. 2003;18:58–73. doi: 10.1093/her/18.1.58. [DOI] [PubMed] [Google Scholar]
- 10.Bandura A. Self-Efficacy: The Exercise of Control. New York: W. H. Freeman and Company; 1997. [Google Scholar]
- 11.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall, Inc.; 1986. [Google Scholar]
- 12.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 13.Becker MH. The Health Belief Model and Personal Health Behavior. Thorofare, NJ: Slack; 1974. [Google Scholar]
- 14.Glasgow RE. Perceived barriers to self-management and preventive behaviors. Health behavior constructs: theory, measurement & research. 2012 Available at: http://dccps.cancer.gov/brp/constructs/index.html. Accessed: 16 April 2012. [Google Scholar]
- 15.Aday LA. Designing and Conducting Health Surveys: A Comprehensive Guide. 2nd edn. San Francisco, CA: Jossey-Bass Publishers; 1996. [Google Scholar]
- 16.Nunnally JC, Bernstein IH. Psychometric Theory. 3rd ed. New York: McGraw-Hill, Inc.; 1994. [Google Scholar]
- 17.Carmines EG, Zeller RA. Reliability and Validity Assessment. Beverly Hills, CA: Sage; 1979. [Google Scholar]
- 18.Reise SP, Ventura J, Keefe RS, et al. Bifactor and item response theory analyses of interviewer report scales of cognitive impairment in schizophrenia. Psychol Assess. 2011;23:245–61. doi: 10.1037/a0021501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen FF, West SG, Sousa KH. A comparison of bifactor and second-order models of quality of life. Multivariate Behav Res. 2006;41:189–225. doi: 10.1207/s15327906mbr4102_5. [DOI] [PubMed] [Google Scholar]
- 20.Patrick CJ, Hicks BM, Nichol PE, et al. A bifactor approach to modeling the structure of the psychopathy checklist-revised. J Pers Disord. 2007;21:118–41. doi: 10.1521/pedi.2007.21.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holzinger KJ, Swineford R. The bifactor method. Psychometrika. 1937;2:41–54. [Google Scholar]
- 22.Reise SP, Moore TM, Haviland MG. Bifactor models and rotations: exploring the extent to which multidimensional data yield univocal scale scores. J Pers Assess. 2010;92:544–59. doi: 10.1080/00223891.2010.496477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reise SP, Morizot J, Hays RD. The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Qual Life Res. 2007;16(Suppl 1):19–31. doi: 10.1007/s11136-007-9183-7. [DOI] [PubMed] [Google Scholar]
- 24.Miller DR, Geller AC, Wood MC, et al. The Falmouth safe skin project: evaluation of a community program to promote sun protection in youth. Health Educ Behav. 1999;26:369–84. doi: 10.1177/109019819902600307. [DOI] [PubMed] [Google Scholar]
- 25.Smith BJ, Ferguson C, McKenzie J, et al. Impacts from repeated mass media campaigns to promote sun protection in Australia. Health Promot Int. 2002;17:51–60. doi: 10.1093/heapro/17.1.51. [DOI] [PubMed] [Google Scholar]
- 26.Robinson JK, Rigel DS, Amonette RA. Summertime sun protection used by adults for their children. J Am Acad Dermatol. 2000;42:746–53. doi: 10.1067/mjd.2000.103984. [DOI] [PubMed] [Google Scholar]
- 27.Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: III. Family history, actinic damage and phenotypic factors. Eur J Cancer. 2005;41:2040–59. doi: 10.1016/j.ejca.2005.03.034. [DOI] [PubMed] [Google Scholar]
- 28.Muthén LK, Muthén BO. Mplus User's Guide. 4th edn. Los Angeles, CA: Muthén & Muthén, 1998–2006. [Google Scholar]
- 29.Flora DB, Curran PJ. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychol Methods. 2004;9:466–91. doi: 10.1037/1082-989X.9.4.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu L, Bentler PM. Evaluating model fit. In: Hoyle RH, editor. Structural Equation Modeling: Concepts, Issues and Applications. Thousand Oaks, CA: Sage; 1995. pp. 76–99. [Google Scholar]
- 31.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–46. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 32.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88:588–606. [Google Scholar]
- 33.Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- 34.Yu C-Y. Evaluating Cut-Off Criteria of Model Fit Indices for Latent Variable Models with Binary and Continuous Outcomes. Los Angeles, CA: University of California; 2002. [Google Scholar]
- 35.Steiger JH. Structural model evaluation and modification: an interval estimation approach. Multivariate Behav Res. 1990;25:173–80. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- 36.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Newbury Park, CA: Sage; 1993. pp. 136–62. [Google Scholar]
- 37.Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 38.Fan X, Sivo SA. Sensitivity of fit indices to model misspecification and model types. Multivariate Behav Res. 2007;42:509–29. [Google Scholar]
- 39.Yuan K-H. Fit indices versus test statistics. Multivariate Behav Res. 2005;40:115–48. doi: 10.1207/s15327906mbr4001_5. [DOI] [PubMed] [Google Scholar]
- 40.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 41.Bollen KA. Structural Equations with Latent Variables. New York: John Wiley & Sons; 1989. [Google Scholar]
- 42.McDonald RP. Test Theory: A Unified Treatment. Mahwah, NJ: Lawrence Erlbaum Associates; 1999. [Google Scholar]
- 43.Raykov T. Estimation of congeneric scale reliability using covariance structure analysis with nonlinear constraints. Br J Math Stat Psychol. 2001;54:315–23. doi: 10.1348/000711001159582. [DOI] [PubMed] [Google Scholar]
- 44.Bagozzi RP, Yi Y. On the evaluation of structural equation models. J Acad Mark Sci. 1988;16:74–94. [Google Scholar]
- 45.Akaike H. Factor analysis and the AIC. Psychometrika. 1987;52:317–32. [Google Scholar]
- 46.Harrison RA, Haque AU, Roseman JM, et al. Socioeconomic characteristics and melanoma incidence. Ann Epidemiol. 1998;8:327–33. doi: 10.1016/s1047-2797(97)00231-7. [DOI] [PubMed] [Google Scholar]


