Abstract
Post-traumatic anterior open bite can occur as a result of broken balance among the masticatory muscles. The superior hyoid muscle group retracts the mandible downward and contributes to the anterior open bite. Denervation of the digastric muscle by injection of botulinum toxin type A (BTX-A) can reduce the power of the digastric muscle and help to resolve the post-traumatic anterior open bite. A patient with a bilateral angle fracture had an anterior open bite even after undergoing three operations under general anesthesia and rubber traction. Although the open bite showed some improvement by the repeated operation, the occlusion was still unstable six weeks after the initial treatment. To eliminate the residual anterior open bite, BTX-A was injected into the anterior belly of the digastric muscle. Following injection of BTX-A, the anterior open bite showed immediate improvement. Complication and relapse were not observed during follow-up. Long-standing post-traumatic open bite could be successfully corrected by injection of BTX-A into the anterior belly of the digastric muscle without complication.
Keywords: Open bite, Neck muscles, Botulinum toxins
I. Introduction
Bilateral mandibular angle fractures separate two posterior condyle-bearing segments from the anterior tooth-bearing segment1. Treatment of bilateral mandibular angle fractures is difficult because of the high morbidity rate2. After the reduction of the angle fractures, anterior open bite can occur because two posterior condyle-bearing fragments are drawn superomedially by the action of masseter, temporalis, and medial pterygoid muscles. On the contrary, the mandibular anterior fragment is depressed by muscles such as digastric, geniohyoid, and mylohyoid1.
The position of the mandible is mainly determined by attached muscles. The muscle group for closing the mouth is mainly attached to the ramus, and the muscle group for opening the mouth is attached to the body. In case of bilateral mandibular angle fractures, the mandibular body is disconnected to the ramus area. Though open reduction restores the connection between the ramus area and the body area, the masseter muscle loses most of its attachment to the ramus because of the muscle being stripped during open reduction. Therefore, the balance of power between the muscle groups for closing and opening should be tipped toward the opening muscle group. The opening muscles will then track the mandible posteroinferiorly. This mechanism can induce the anterior open bite1. Since it is important for opening the mouth, the digastric muscle can be a treatment target for restoring the balance.
Intramuscular injection of botulinum toxin type A (BTX-A) can denervate muscle by preventing the release of acetylcholine from the terminal of the motor nerve; this leads to the paralysis of muscle3,4. BTX-A can cause muscle atrophy, thereby reducing the volume of muscle5. In this study, the injection of BTX-A into the digastric muscle demonstrated the correction of post-operative anterior open bite. To the best of our knowledge, this is the first technical report using BTX-A for the correction of post-operative anterior open bite.
II. Case Report
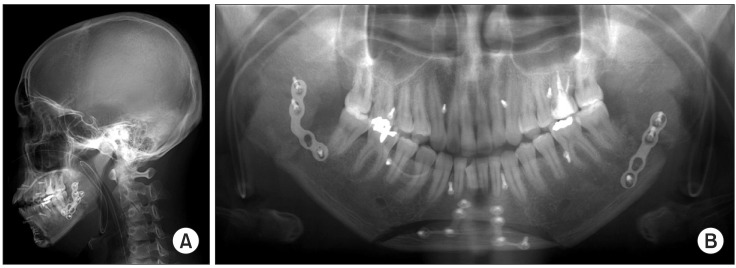
On October 12, 2011, a twenty-year-old man visited Gangneung-Wonju National University Hospital with malocclusion and wound dehiscence in the left retromolar area. He had swelling and local hotness in the left mandible angle area. He had previ ously undergone surgery twice at the department of plastic surgery of another hospital but had failed to achieve proper occlusion after both surgeries. After the surgery, the patient had received active rubber traction for 4 weeks to correct the anterior open bite. He also showed premature contact in the molar area. Three-dimensional cone beam computed tomography (CBCT) and panoramic radiography were taken for preoperative diagnosis. There were malunion of bony fragments and large bony gap in the left mandibular angle area.(Fig. 1)
Fig. 1.
The patient already received open reduction operation 2 times in another hospital. Pre-operative three-dimension computed tomography image of the left mandibular angle area. Anterior open-bite and a large bony gap (arrow) were shown.
Thus, hardware removal and reduction and fixation were planned intra-orally. After hardware removal, bony malunion areas were separated using chisel and mallet. After the separation of proximal and distal segments, proper occlusions were established by manipulation. Internal fixation was done using reconstruction plates and screws. Genioplasty was performed simultaneously for esthetic reasons. One day after operation, the anterior open bite was improved compared to the preoperative condition, although it remained.(Fig. 2. A) To resolve the residual anterior open bite, we applied additional rubber traction over a week. Rubber was located on the anterior tooth area and both premolar areas using 8 screws anchored on the alveolar bone.(Fig. 2. B) In spite of active rubber traction, there was no improvement in the anterior open bite. To eliminate residual anterior open bite, we decided to use BTX-A (Meditoxin; Medy-Tox, Seoul, Korea). Ten days after the third operation, 24-gauge intravenous catheters were inserted into the anterior belly of the digastric muscle at 4 sites.(Fig. 3) This muscle is attached to the digastric fossa as an internal aspect of the mandible and both sides of the midline. We could easily find the anterior belly of the digastric muscle using the digastric fossa. At each point, 5 units of BTX-A were injected into the muscle through the plastic catheter. A total of 20 units of BTX-A was used.
Fig. 2.
First day after the third operation. A. Lateral view. B. Panoramic view.
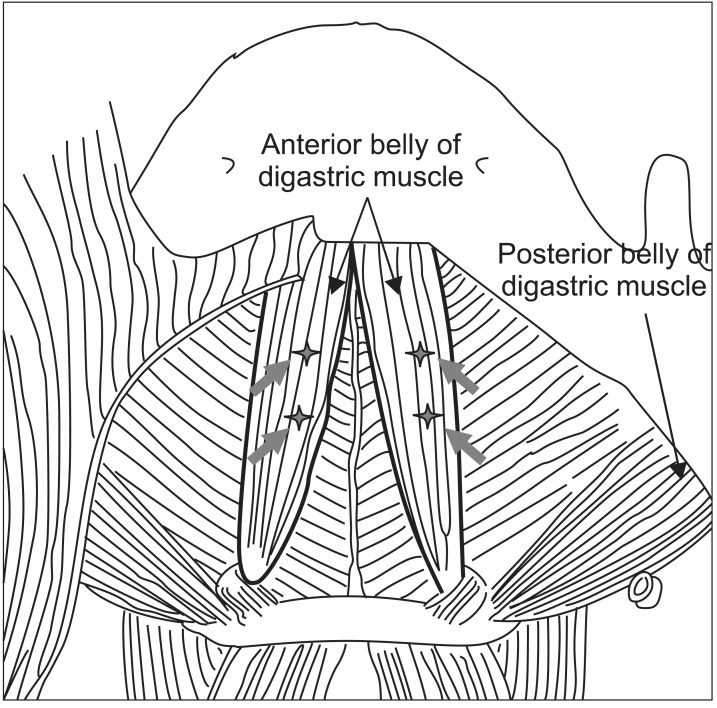
Fig. 3.
Injection sites of botulinum toxin type A in the anterior belly of digastric muscles (arrows).
There was no early complication after the injection of BTX-A. The anterior open bite completely disappeared 3 days after BTX-A injection.(Fig. 4) Elastic traction was not used after achieving stable occlusion, with only screws kept in preparation against any unexpected accident. CBCT was taken 4 weeks after BTX-A injection, showing the resolution of anterior open-bite and good occlusion.(Fig. 5) During the follow-up, no event occurred. Occlusion was stable until 6 months after BTX-A injection. Thus, repeated BTX-A injection was not considered.
Fig. 4.
Third day after botulinum toxin type A injection. A. Lateral view. B. Panoramic view.
Fig. 5.
Post-operative three-dimension computed tomography image of left mandibular angle area in 4 weeks after botulinum toxin type A injection. The gap between fragments was healed (arrow) and the occlusion was stable.
III. Discussion
Simple elastics traction can treat most cases of post-traumatic anterior open bite. The traction period may differ according to the trauma severity, but approximately 2-4 weeks has been reported to be adequate6-8. If the post-traumatic open bite does not improve in spite of extensive elastic traction, the patient must feel discomfort and complain. Though the open bite is corrected through 3 weeks of rubber traction, the patient will suffer from 3 weeks' treatment, and the overall expense will also increase. BTX-A injection is a relatively safe, non-invasive method for reducing muscle volume and power5. In the presented case, BTX-A injection showed rapid correction of post-traumatic open bite. Occlusal stability was maintained until 6 months' follow-up, and repeated injections were not required. Therefore, BTX-A injection into the anterior belly of the digastric muscle was an effective method for the correction of post-traumatic open bite.
BTX-A has been injected periodically for the correction of masseter muscle hypertrophy. Though BTX-A injection denervates the muscle, motor nerves regenerate and renervate again. Note, however, that BTX-A injection was done 1 time for the correction of post-traumatic open bite. Unlike masseter muscle hypertrophy, the post-traumatic open bite was due to the broken balance among muscles. The muscle group for closing the mouth was detached from the mandibular body in the bilateral angle fracture. Even after proper reduction, these muscles were still in a state of being stripped from the bone. After the correction of open bite, the reattachment of these muscles could occur. Though the power of the digastric muscle would be recovered 3-4 months later, the muscle group for closing the mouth also exerted power after reattachment. In this case, the balance among muscles would not be impaired. For similar reasons, once the closure of the anterior open bite is achieved by elastic intermaxillary traction, anterior open bite seldom recurs after the removal of the elastics.
In single mandibular angle fracture, only one plate is usually applied on the external oblique ridge, which is a tension zone of the mandible9. To secure proper stabilization, one more plate can be applied on the inferior border of the mandibular angle area10. Note, however, that we applied only metal plate on the mid-portion of the fracture line. Because of previous surgery, severe bone resorption was observed on the external oblique ridge and inferior border of the mandibular angle, so we could not fix the plate and screw on this area. Thus, we had to apply only one reconstruction plate on the mid-portion of the mandible angle fracture line. Wound dehiscence, swelling, and hotness were observed prior to surgery; thus, we tried to operate with minimal dissection and plate screwing.
In this study, the anterior belly of the digastric muscle was selected as target of BTX-A injection. The main role of the digastric muscle is to depress the mandible, so it is primarily related to opening the mouth11-13. The lateral pterygoid muscle is also related to opening the mouth. Note, however, that the lateral pterygoid muscle is seated deeply, and the complication after BTX injection will be higher. Suprahyoid myotomy can reduce muscle power14. Radiofrequency therapy to the digastric muscle has been considered an additional therapy for preventing open bite or correcting the reestablished open bite15. As an aggressive procedure, suprahyoid myotomy can cause severe morbidity. Radiofrequency therapy is a relatively less invasive method15 but requires an expensive device such as radiofrequency generator. In contrast, the BTX-A injection method is relatively cheap, requiring no special device.
BTX-A has been used for the treatment of dystonia. Previous studies showed that injection of BTX-A into the digastric muscle can treat jaw opening and oromandibular dystonia16. The suggested doses of BTX-A ranged from 3.8 to 30 units16. In this study, we used 20 units of BTX-A. We injected BTX-A into the muscle through plastic intravenous catheter instead of using metal needle injection syringe. Plastic intravenous catheter is a very useful drug delivery tool to the muscle. The diameter of the 24-gauge plastic intravenous catheter is very small, and the plastic catheter is not rigid. If BTX-A is injected into the blood vessel, there was no effect on the muscle, possibly causing rare but severe complication such as botulism accompanied by dysphagia, muscle weakness, and respiratory distress17. When the plastic catheter is placed in a vessel, the aspirated blood can be observed in the plastic catheter. Therefore, unwanted intravascular injection can be avoided.
We believe the presented technique can be applied to correct open bite in orthodontic practice or orthognathic surgery. Simple BTX-A injection may speed up overall treatment and minimize the post-treatment relapse. To provide evidence of this hypothesis, a large-scale, case control study will be required. In this stage, BTX-A injection may be applied to selective open bite patients who do not respond to extensive rubber traction.
In conclusion, long-standing post-traumatic open bite could be corrected successfully by BTX-A injection into the anterior belly of the digastric muscle without any complication.
References
- 1.Haskell R. Applied surgical anatomy. In: Williams JL, editor. Rowe and Williams' maxillofacial injuries. 2nd ed. Edinburgh: Churchill Livingstone; 1994. pp. 12–14. [Google Scholar]
- 2.Lamphier J, Ziccardi V, Ruvo A, Janel M. Complications of mandibular fractures in an urban teaching center. J Oral Maxillofac Surg. 2003;61:745–749. doi: 10.1016/s0278-2391(03)00147-2. [DOI] [PubMed] [Google Scholar]
- 3.Duchen LW. Changes in motor innervation and cholinesterase localization induced by botulinum toxin in skeletal muscle of the mouse: differences between fast and slow muscles. J Neurol Neurosurg Psychiatry. 1970;33:40–54. doi: 10.1136/jnnp.33.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Angaut-Petit D, Molgó J, Comella JX, Faille L, Tabti N. Terminal sprouting in mouse neuromuscular junctions poisoned with botulinum type A toxin: morphological and electrophysiological features. Neuroscience. 1990;37:799–808. doi: 10.1016/0306-4522(90)90109-h. [DOI] [PubMed] [Google Scholar]
- 5.Morbiato L, Carli L, Johnson EA, Montecucco C, Molgó J, Rossetto O. Neuromuscular paralysis and recovery in mice injected with botulinum neurotoxins A and C. Eur J Neurosci. 2007;25:2697–2704. doi: 10.1111/j.1460-9568.2007.05529.x. [DOI] [PubMed] [Google Scholar]
- 6.Landes CA, Lipphardt R. Prospective evaluation of a pragmatic treatment rationale: open reduction and internal fixation of displaced and dislocated condyle and condylar head fractures and closed reduction of non-displaced, non-dislocated fractures. Part I: condyle and subcondylar fractures. Int J Oral Maxillofac Surg. 2005;34:859–870. doi: 10.1016/j.ijom.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 7.Ferguson JW, Stewart IA, Whitley BD. Lateral displacement of the intact mandibular condyle. Review of literature and report of case with associated facial nerve palsy. J Craniomaxillofac Surg. 1989;17:125–127. doi: 10.1016/s1010-5182(89)80084-8. [DOI] [PubMed] [Google Scholar]
- 8.Satoh K, Suzuki H, Matsuzaki S. A type II lateral dislocation of bilateral intact mandibular condyles with a proposed new classification. Plast Reconstr Surg. 1994;93:598–602. [PubMed] [Google Scholar]
- 9.Ellis E, 3rd, Walker LR. Treatment of mandibular angle fractures using one noncompression miniplate. J Oral Maxillofac Surg. 1996;54:864–871. doi: 10.1016/s0278-2391(96)90538-8. [DOI] [PubMed] [Google Scholar]
- 10.Ellis Edward., III . Rigid versus nonrigid fixation. In: Miloro Michael., editor. Peterson's oral and maxillofacial surgery. 2nd ed. Hamilton: BC Decker Inc; 2004. pp. 371–373. [Google Scholar]
- 11.Bérzin F. Electromyographic analysis of the sternohyoid muscle and anterior belly of the digastric muscle in jaw movements. J Oral Rehabil. 1995;22:463–467. doi: 10.1111/j.1365-2842.1995.tb00802.x. [DOI] [PubMed] [Google Scholar]
- 12.Widmalm SE, Lillie JH, Ash MM., Jr Anatomical and electromyographic studies of the digastric muscle. J Oral Rehabil. 1988;15:3–21. doi: 10.1111/j.1365-2842.1988.tb00142.x. [DOI] [PubMed] [Google Scholar]
- 13.Celik H, Yilmaz E, Atasever A, Durgun B, Taner D. Bilateral anatomical anomaly of anterior bellies of digastric muscles. Kaibogaku Zasshi. 1992;67:650–651. [PubMed] [Google Scholar]
- 14.Carlson DS, Ellis E, 3rd, Dechow PC, Nemeth PA. Short-term stability and muscle adaptation after mandibular advancement surgery with and without suprahyoid myotomy in juvenile Macaca mulatta. Oral Surg Oral Med Oral Pathol. 1989;68:135–149. doi: 10.1016/0030-4220(89)90181-3. [DOI] [PubMed] [Google Scholar]
- 15.Choi SS, Rotaru H, Kim SG. Treatment of post-traumatic open bite by radiofrequency. Br J Oral Maxillofac Surg. 2007;45:311–313. doi: 10.1016/j.bjoms.2005.11.018. [DOI] [PubMed] [Google Scholar]
- 16.Tan EK. Oromandibular dystonia. In: Mitchell FB, editor. Dystonia: etiology, clinical features, and treatment. Philadenphia: Lippincott Williams & Wilkins; 2004. pp. 171–172. [Google Scholar]
- 17.Coban A, Matur Z, Hanagasi HA, Parman Y. Iatrogenic botulism after botulinum toxin type A injections. Clin Neuropharmacol. 2010;33:158–160. doi: 10.1097/WNF.0b013e3181d479e0. [DOI] [PubMed] [Google Scholar]