Abstract
Objectives
Infererior alveolar nerve (IAN) damage may be one of the distressing complications occurring during implant placement. Because of nature of closed injury, a large proportion is approached non-invasively. The purpose of this study was to analyze the outcomes of conservative management of the injured nerve during dental implant procedure.
Materials and Methods
Sixty-four patients of implant related IAN injury, who were managed by medication or observation from January 1997 to March 2007 at the Department of Oral and Maxillofacial Surgery, Seoul National University Dental Hospital, were retrospectively investigated. The objective tests and subjective evaluations were performed to evaluate the degree of damage and duration of sensory disturbance recovery. Tests were performed on the day of the first visit and every two months afterward. Patient's initial symptoms, proximity of the implant to the IAN, time interval between implant surgery and the first visit to our clinic, and treatment after implant surgery were analyzed to determine whether these factors affected the final outcomes.
Results
Among the 64 patients, 23 had a chief complaint of sensory disturbance and others with dysesthesia. The mean time until first visit to our hospital after the injury was 10.9 months.One year after nerve injury, the sensation was improved in 9 patients, whereas not improved in 38 patients, even 4 patients experienced deterioration. Better prognosis was observed in the group of patients with early visits and with implants placed or managed not too close to the IAN.
Conclusion
Nearly 70% of patients with IAN injury during implant placement showed no improvement in sensation or dysesthesia with the conservative management. Earlier decision for active treatment needs to be considered because of possibility of deterioration of symptoms and unsatisfactory recovery.
Keywords: IAN injury, Trigeminal nerve, Conservative therapy
I. Introduction
One of the distressing complications of implant placement is damage to the inferior alveolar nerve (IAN).Various degrees of prevalence of altered sensation after the placement of mandibular implants have been published. Kiyak et al.1 reported 43.5% cases of paresthesia two weeks after mandibular implant placement; Bartling et al.2 stated that 8.5% of patients had altered sensation. Ellies and Hawker3, in a retrospective questionnaire addressing sensory changes, observed 37% of patients with altered sensation one month after implant placement1-4. Due to the difficulty in defining the extent of injury and poor accessibility to the IAN (closed wound), imme diate surgical repair of a damaged IAN is uncommon. Therefore, the first line of treatment is medication and physio therapy to enhance nerve regeneration. Although the conservative management of implant-induced IAN injury is generally accepted to produce improved results, the effect on the functional recovery of the IAN is inconsistent and is too variable.
This study sought to evaluate the outcomes of conservative treatment of an injured IAN after implant placement and to attempt to identify predictors of better recovery.
II. Materials and Methods
This study targeted patients with altered sensations of the IAN as a result of dental implant surgery and who were managed with a conservative approach at the Department of Oral and Maxillofacial Surgery, Seoul National University Dental Hospital (SNUDH). The period of data collection was from January 1, 1997 to March 30, 2007. A total of 64 patients (35 women, 29 men) were selected based on inclusion criteria of (1) neurosensory alteration after the placement of implants in the posterior mandible and (2) no history of neurologic discomfort.
Patient records were examined, and information pertaining to the date of implant placement, location of implant placement, chief complaint at the initial visit, patients' subjective evaluation, and objective evaluation were recorded. Depending on the time interval between the implant surgery and the first visit to our hospital, the patients were divided into two groups. Group I included patients who visited our clinic within 9 months of nerve injury, whereas group II included patients who visited our clinic 9 months after nerve injury. In addition, the previous treatments before visiting our clinic were recorded, and the patients were grouped accordingly. Group III included patients whose implants were surgically decompressed (removed or partially unscrewed or removed and re-implanted with shorter fixtures), whereas group IV patients had not undergone any treatment or medication. The radiographic proximity of the implant fixture to the IAN canal was examined, and the distance from the bottom of the implant to the roof of the inferior alveolar canal was measured on the panoramic radiograph.
The patients' subjective evaluation included the self-assessment of the neurosensory function in terms of reduced function (hypoesthesia, anesthesia) and neurogenic discomfort (paresthesia, dysesthesia, etc.). Associated discomfort and malfunction were recorded. We compared the current neurological status with the previous state of each patient. In addition, the patients were told to classify their overall altering state of sensory function to an improved state, stationary state, aggravated state, or change of symptom. Patients followed-up every two months after the initial visit to our clinic.
Every objective evaluation was performed at each visit. These included contact detection threshold, direction perception, two-point discrimination, pin prick, and thermal discrimination (cold).
After visiting our clinics, conservative treatment was performed on the patients before deciding on surgery which was usually conducted at 3 or 9 months from injury. Our treatment protocol is given in Table 1, with the protocol usually consisting of medication and physical treatment.
Table 1.
Protocols of conservative management
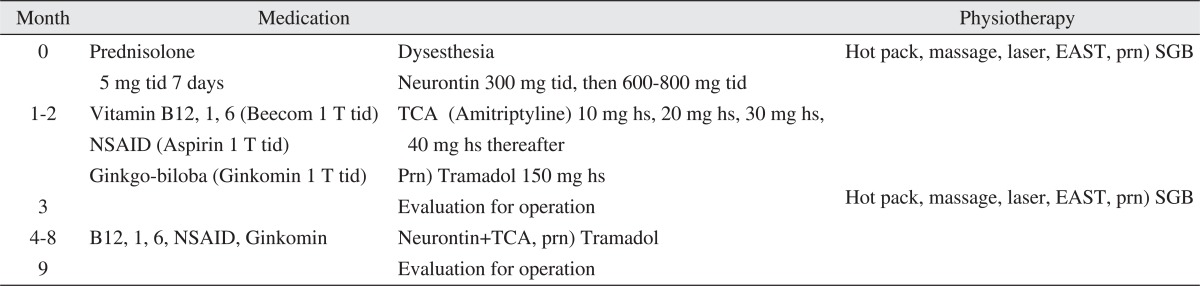
(tid: three times a day, NSAID: nonsteroidal anti-inflammatory drugs, T: tablet, TCA: tricyclic antidepressant, hs: hora somni, at bedtime, prn: pro re nata, as required, EAST: electrical acupuncture stimulation therapy, SGB: stellate ganglion block)
Statistical analysis was performed using SPSS version 17.0 (SPSS, Chicago, IL, USA). Correlation between the duration after nerve damage and patient's subjective prognosis, between the duration after nerve damage and patient's type of altered sensation, between the treatment of damaged nerve and patient's prognosis, and between the distance from implant to IAN and patient's prognosis was analyzed using the chi-square test. A significant difference was assumed when P value was <0.05.
III. Results
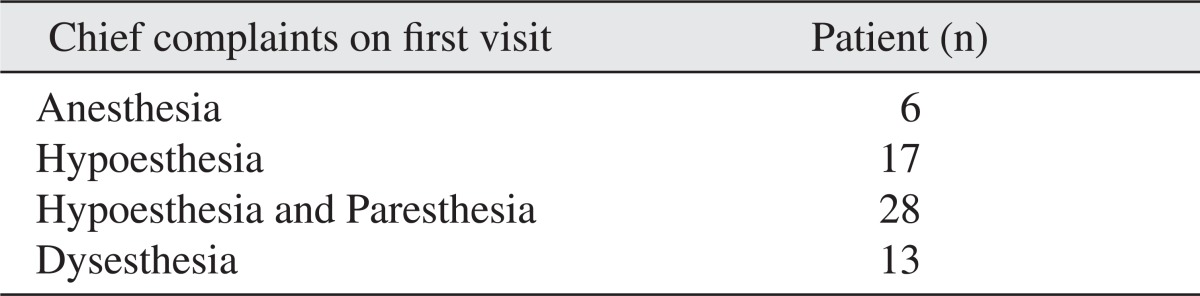
A total of 64 patients underwent conservative treatment. The mean follow-up period was 30.18 months (from 2 months to 7 years and 7 months). The affected sites consisted of 35 cases on the right side, 25 cases on the left side, and 4 cases of bilateral involvement. The chief complaints of the patients on their first visit were interpreted into medical terms (anesthesia, hypoesthesia, paresthesia, and dysesthesia) and are shown in Table 2.
Table 2.
Chief complaints of patients on first visit (total=64)
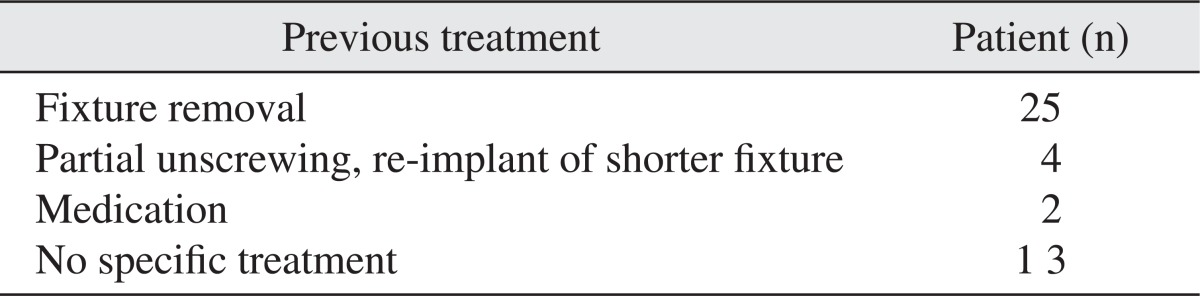
The mean interval between injury and first visit to SNUDH was 10.91 months (from 1 week to 5 years). The number of patients who visited our clinic before 9 months post-injury was 36, whereas the number of patients who visited our clinic after 9 months was 28. The previous treatments before the visit and the number of patients are given in Table 3.
Table 3.
Previous treatment before the visit to our clinic (total=44)
1. Patient subjective evaluation
1) Functional deficit
The most commonly impaired activities as a result of altered sensation were chewing and speech problem. The functional deficits at the most recent follow-up are shown in Table 4. The vast majority of the affected population group (38 patients) did not exhibit any difficulty.
Table 4.
Functional deficit at most recent follow-up (total=64)
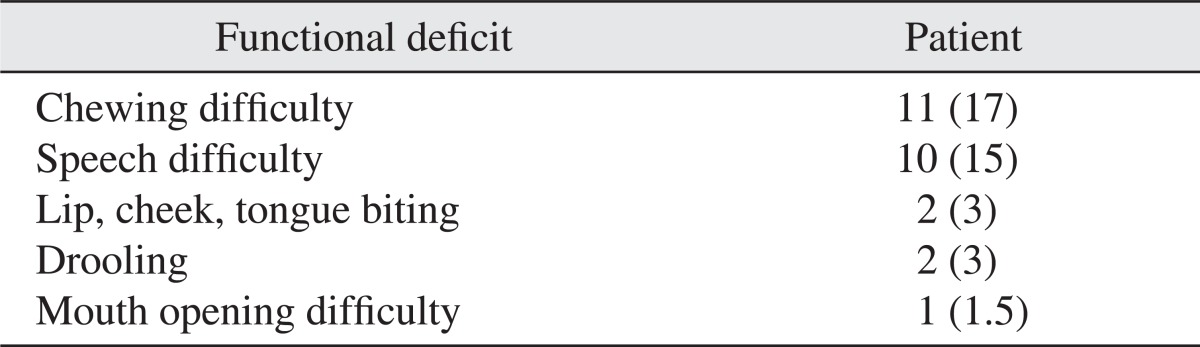
Values are presented as number (%).
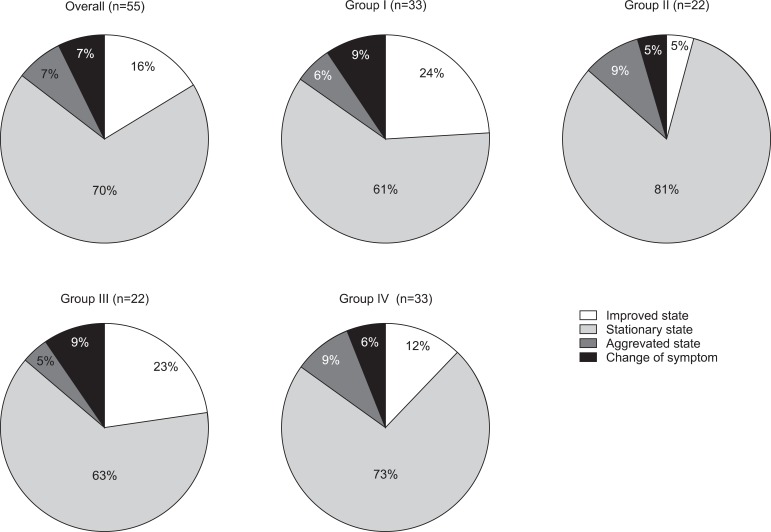
2) Change of symptom
All 55 patients were investigated, and the results are shown in Fig. 1. In 38 patients, there were no changes in symptoms, whereas 4 patients experienced worsening symptoms and 9 patients had improved tactile sensation. The patients who complained of worsened symptoms were those with feeling of hypoesthesia was exaggerated or those with dysesthesia with aggravated pain. Groups I and III exhibited greater improvement in symptoms than groups II and IV, but the difference was not statistically significant.(Table 5)
Fig. 1.
Change of symptom (total=55).
(Group I: first visit time to our department after nerve damage <9 months, group II: first visit time to our department after nerve damage >9 months, group III: implant removal or decompression, group IV: no treatment or medication)
Table 5.
Type of altered sensation inthe groups (total=55)
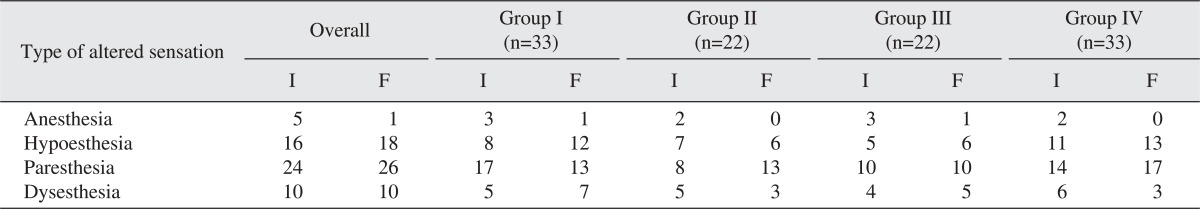
(Group I: time of first visit to our department after nerve damage <9 months, group II: time of first visit to our department after nerve damage >9 months, group III: implant removal or decompression, group IV: no treatment or medication, I: initial, F: final)
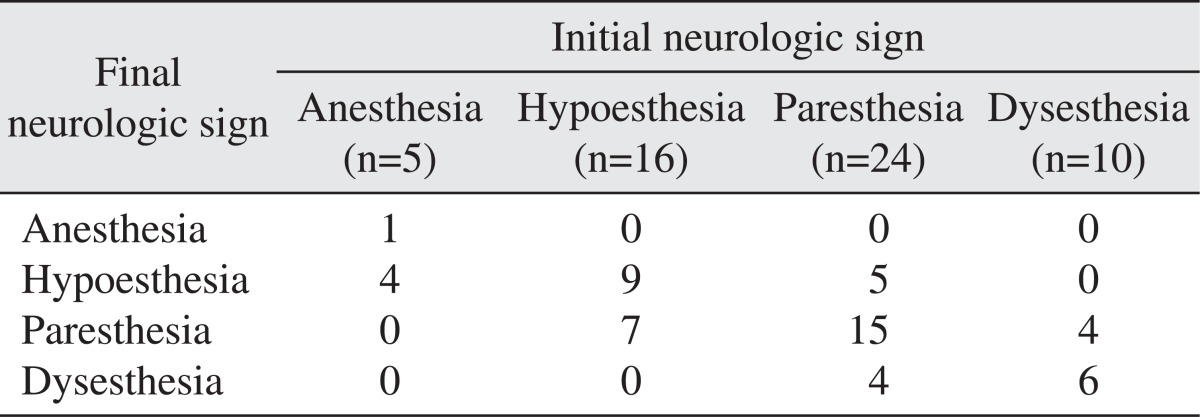
Initial neurologic signs after nerve damage and their recovery consequences are shown in Table 6. Five patients had initial symptoms of anesthesia. Four of the 5 patients, anesthesia improved slightly (hypoesthesia).
Table 6.
Initial neurologic signs after nerve damage and symptom consequence (total=55)
3) Objective evaluation-sensory test result
Among the 64 patients, 57 were included in this study. The implants were removed in 25 patients before the first visit to our hospital, 30 patients received no treatment, and 2 patients were treated with medication only. Three groups were analyzed according to the recovery rate and time, and the results are shown in Table 7. A determination of improvement was archived when all of the following four criteria were met:
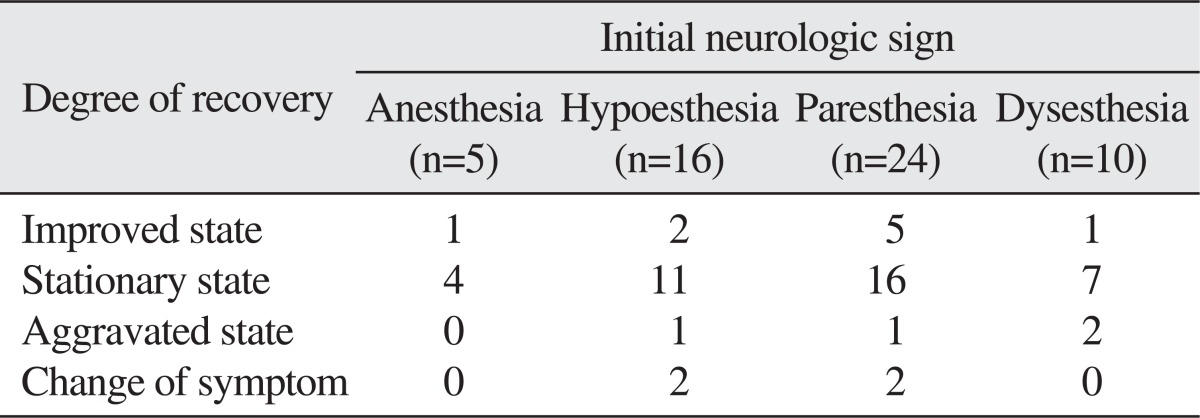
Table 7.
Degree of recovery classified on the initial neurologic signs after nerve damage (total=55)
(1) Contact detection threshold of less than 2.83 g
(2) Two-point discrimination threshold of less than 1.5 cm
(3) Tactile direction discrimination of more than 75%
(4) Normal ability to detect cold5,6
Fifty-eight percent of the patients had not recovered objectively. Approximately 21% of the improved patients showed improvement within 9 months.
4) Subjective symptom and objective evaluation
We compared the sensory test results of the patients with their subjective symptoms.(Table 8) The subjective symptoms of the patients can be divided into two categories: decreased sensation and unpleasant sensation. The severity of the symptoms was recorded for each category, and the results are shown in Table 9. While complete recovery seemed to have occurred based on the sensory test results, only 40% of those patients exhibited mild to moderate improvement of decreased sensation.
Table 8.
Comparison between the sensory test results and the patients' subjective symptoms (total=52)
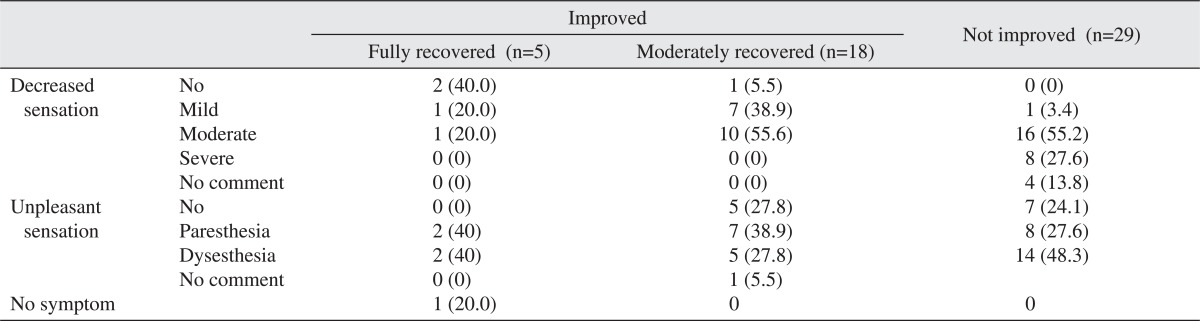
Values are presened as number (%).
Table 9.
Previous treatment and rate of recovery (total=57)
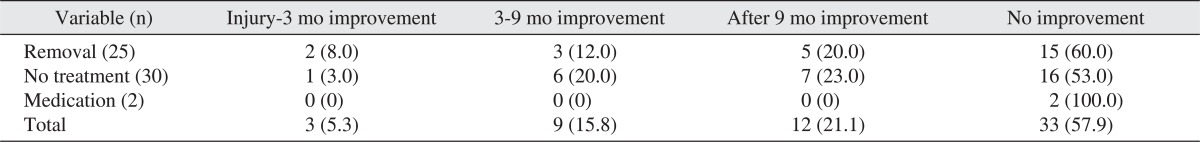
Values are presened as number (%).
5) Radiographic proximity of the implant fixture to the inferior alveolar canal and its consequences
The distance between the implant and inferior alveolar canal was examined using a panoramic radiograph. We divided the cases into three groups depending on the distances: one group included cases wherein the distance between the implant and IAN was greater than 2 mm; another group had cases wherein the distance between the inferior alveolar canal and implant fixture was within 2 mm, and; the third group included cases wherein the implant fixture penetrated the canal. The final subjective symptoms and objective signs of the patients are shown in Table 10. These symptoms improved in most cases if the distance was greater than 2 mm. There was no improvement if the distance was less than 2 mm or if nerve damage occurred. Note, however, that there were no statistically significant differences between the distance and the prognosis.
Table 10.
Signs and symptoms according to the distance from the IANto the fixture (total=36)
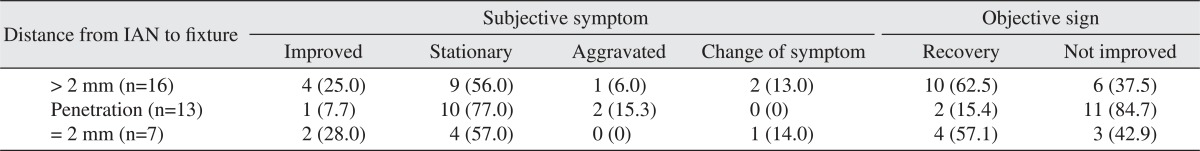
(IAN: inferior alveolar nerve)
Values are presened as number (%).
IV. Discussion
This study was primarily designed to examine the recovery rate of IAN damage after implant placement and to examine the factors that influence the outcomes. Based on our results, only 16% of patients exhibited improved sensation, whereas 70% of patients remained in stationary sensation. Based on the sensory test results, only 42.1% of patients recovered their senses. For half of the patients, the duration of altered sensation was within 9 months, whereas the other half experienced altered sensation which lasted more than 9 months. The period of postoperative altered sensation is diverse and has not been frequently reported. Vazquez et al.4 reported that temporary paresthesia occurred in 0.1% of patients and lasted approximately 3-6 weeks. Similarly, Bartling et al.2 claimed that 50% of the patients were back to normal after three weeks of non-steroidal anti-inflammatory medication. Frei et al.7 found that, for 2.6% of patients who had an implant placed, paresthesia of the lower lip area lasted 4 weeks. According to Ellies and Hawker2, of the 23% of patients experiencing short-term changes, 90% reported that their symptoms had disappeared within 6 months4. Our results showed relatively high rates of permanent damage. These differing results may be explained by the types of patients seen at SNUDH. Most patients who visited SNUDH were referred by local clinics. Most of them had to spend several months waiting for the damaged nerve to recover before visiting SNUDH. Among the patients with nerve damage, those who had not improved considerably visited our hospital. For this reason, our results showed a higher percentage of patients with relatively poor prognosis than other studies.
Altered sensation in the lower lip area can be caused by several factors8. One factor may be nerve compression through edema as a result of the operation or by hematoma and scarring9. In most cases, however, these types of disturbance are usually reversible. If implants are inserted closely to the IAN without directly damaging it, patients may experience periodic changes of sensation, such as when the area is exposed to a stimulating temperature during a meal. Nerve injury also occurred if unintended direct damage to the IAN occurred during implant insertion. In this case, damage may lead to permanent neurosensory damage or variable sensation of pain10.
Hillerup11 investigated the iatrogenic damage of the trigeminal nerve. The magnitude of neurosensory impairment and amount of neurologic malfunction (paresthesia, dysesthesia, etc.) were so troublesome that some patients suffered severe deterioration of the overall quality of life. At least 17% of patients suffered from chewing difficulty, whereas 15% had speech difficulty. Reduction or loss of sensation and painful triggers in the damaged nerve dermatome would result in unilateral chewing behavior, leading to concomitant temporomandibular dysfunction issues such as pain upon chewing11. Pronunciation disability was also a frequently encountered problem that may follow the loss of sensory input from the IAN11. These patients require more concentration for word pronunciation, which was considered a stress factor.
Majority of patients experienced trigeminal nerve injuries as a result of minor oral surgery of the head and neck. Patients who had dental implants placed or experienced trauma in the oral and maxillofacial region were known to recover spontaneously from paresthesia (defined as an abnormal sensation) and dysesthesia (defined as an abnormal painful sensation)8. Nonetheless, the damaged neurosensory function experienced by some patients and which lasted for a long time was permanent. Several studies have described various types of neurosensory impairment and altered sensations that resulted in patient annoyance and disability. Post-injury subjective symptoms consisted of paresthesia and dysesthesia. Dysesthesia includes several pathologic conditions such as neuroma pain, allodynia, hyperalgesia, hyperpathia, sympathetic mediated pain, central trigeminal pathoses, anesthesia dolorosa, and psychogenic pain12.
According to Seo et al.12, there are two types of paresthesia: spontaneous and elicited paresthesia. Mechanical touch sensations conduct afferent stimuli through Aβ-fibers, and their elevation may imply a dysfunction of the fibers12. These phenomena are usually thought to be associated with the spontaneous paresthesia observed in neuromas12.
Nerve damage affecting limited parts of the fibers could cause demyelination of axons, resulting in hyper-excitability to physical stimuli. These damages also trigger the hyper-excitability of dorsal horn cells owing to the prolonged existence of discharges from the damaged nerve12. Therefore, peripheral injuries of the IAN elicit hyper-excitation at both the distal injury site and the cells of the trigeminal nucleus. These phenomena could explain the pathologic discomfort experienced by our patients.
Sometimes, elicited paresthesia does not accompany apparent sensory dysfunction. This also shows several transient symptoms followed by spontaneous paresthesia during the post-injury period, suggesting some possible changes in the peripheral site and/or central neurons. In addition to an increase of current perception threshold (CPT), elicited paresthesia exhibited higher CPT values than spontaneous paresthesia, indicating C-fiber dysfunction12. Since non-myelinated afferent fibers release neuropeptides and glutamates from their central afferent terminals, their injury could promote long-term excitation in dorsal horn neurons12,13. This is the reason elicited paresthesia is longer-lasting than spontaneous paresthesia.
Regarding the altered sensation type, the number of patients with anesthesia decreased, and the number of patients with hypoesthesia and paresthesia increased. These phenomena could be explained by neuromas or scar formation that occurred during the recovery from sensory nerve damage.
In our study, until the latest follow-up, patient's symptoms remained stationary in 70% of patients. Only 16% of patients experienced an improvement in symptoms. Patients recovering from nerve damage were divided into two groups, and patients who visited the hospital within 9 months exhibited greater improvement in their symptoms than those visiting after 9 months. These results suggest that early treatment is important in cases of nerve damage. We need to be aware of the situation in the early stages to respond quickly when nerve damage occurs especially 9 months before.
Comparing patients who underwent the removal of implants or decompression with no treatment or those who took medication, the former's patient subjective symptoms improved slightly. The former also showed greater improvement in their sensory test result. This result was similar to that of the study of Khawaja and Renton14, suggesting that the early removal of implants - especially within 36 hours' post-injury - could minimize IAN neuropathy.
Our last study was the evaluation between the distance from implant fixture to the inferior alveolar canal and their outcome. Patients' subjective symptoms and sensory test results showed greater improvement for the group of patients with sufficient distance from the canal. Therefore, accurate diagnosis and careful surgery are necessary to recognize the anatomical location of the inferior nerve canal to avoid iatrogenic nerve damage.
V. Conclusion
Nearly 70% of patients with IAN injury following implant installation showed no improvement in sensation or dysesthesia with the conservative management. The factors that influence the final results are the distance from the fixture to the IAN canal and the surgeon's immediate management such as implant removal, decompression, or medication. Our retrospective study showed somewhat better results with patient's who started appropriate treatment earlier. Accurate analysis about the location of the IAN in radiographs should be required. Earlier decision for active treatment needs to be considered because of possibility of deterioration of symptoms and unsatisfactory recovery.
Footnotes
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry of Health, Welfare & Family Affairs, Republic of Korea (A101578).
References
- 1.Kiyak HA, Beach BH, Worthington P, Taylor T, Bolender C, Evans J. Psychological impact of osseointegrated dental implants. Int J Oral Maxillofac Implants. 1990;5:61–69. [PubMed] [Google Scholar]
- 2.Bartling R, Freeman K, Kraut RA. The incidence of altered sensation of the mental nerve after mandibular implant placement. J Oral Maxillofac Surg. 1999;57:1408–1412. doi: 10.1016/s0278-2391(99)90720-6. [DOI] [PubMed] [Google Scholar]
- 3.Ellies LG, Hawker PB. The prevalence of altered sensation associated with implant surgery. Int J Oral Maxillofac Implants. 1993;8:674–679. [PubMed] [Google Scholar]
- 4.Vazquez L, Saulacic N, Belser U, Bernard JP. Efficacy of panoramic radiographs in the preoperative planning of posterior mandibular implants: a prospective clinical study of 1527 consecutively treated patients. Clin Oral Implants Res. 2008;19:81–85. doi: 10.1111/j.1600-0501.2007.01402.x. [DOI] [PubMed] [Google Scholar]
- 5.Htut M, Misra P, Anand P, Birch R, Carlstedt T. Pain phenomena and sensory recovery following brachial plexus avulsion injury and surgical repairs. J Hand Surg Br. 2006;31:596–605. doi: 10.1016/j.jhsb.2006.04.027. [DOI] [PubMed] [Google Scholar]
- 6.Pogrel MA. The results of microneurosurgery of the inferior alveolar and lingual nerve. J Oral Maxillofac Surg. 2002;60:485–489. doi: 10.1053/joms.2002.31841. [DOI] [PubMed] [Google Scholar]
- 7.Frei C, Buser D, Dula K. Study on the necessity for cross-section imaging of the posterior mandible for treatment planning of standard cases in implant dentistry. Clin Oral Implants Res. 2004;15:490–497. doi: 10.1111/j.1600-0501.2004.01032.x. [DOI] [PubMed] [Google Scholar]
- 8.Strauss ER, Ziccardi VB, Janal MN. Outcome assessment of inferior alveolar nerve microsurgery: a retrospective review. J Oral Maxillofac Surg. 2006;64:1767–1770. doi: 10.1016/j.joms.2005.11.111. [DOI] [PubMed] [Google Scholar]
- 9.Renzi G, Carboni A, Perugini M, Giovannetti F, Becelli R. Posttraumatic trigeminal nerve impairment: a prospective analysis of recovery patterns in a series of 103 consecutive facial fractures. J Oral Maxillofac Surg. 2004;62:1341–1346. doi: 10.1016/j.joms.2004.05.212. [DOI] [PubMed] [Google Scholar]
- 10.Wismeijer D, van Waas MA, Vermeeren JI, Kalk W. Patients' perception of sensory disturbances of the mental nerve before and after implant surgery: a prospective study of 110 patients. Br J Oral Maxillofac Surg. 1997;35:254–259. doi: 10.1016/s0266-4356(97)90043-7. [DOI] [PubMed] [Google Scholar]
- 11.Hillerup S. Iatrogenic injury to oral branches of the trigeminal nerve: records of 449 cases. Clin Oral Investig. 2007;11:133–142. doi: 10.1007/s00784-006-0089-5. [DOI] [PubMed] [Google Scholar]
- 12.Seo K, Tanaka Y, Terumitsu M, Someya G. Characterization of different paresthesias following orthognathic surgery of the mandible. J Oral Maxillofac Surg. 2005;63:298–303. doi: 10.1016/j.joms.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 13.Gilron I, Watson CP, Cahill CM, Moulin DE. Neuropathic pain: a practical guide for the clinician. CMAJ. 2006;175:265–275. doi: 10.1503/cmaj.060146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khawaja N, Renton T. Case studies on implant removal influencing the resolution of inferior alveolar nerve injury. Br Dent J. 2009;206:365–370. doi: 10.1038/sj.bdj.2009.258. [DOI] [PubMed] [Google Scholar]