Abstract
Damage to adjacent teeth is one of the various complications that may occur during implant placement and is often the result of improper direction during fixture placement or excessive depth of placement. In general, if detrimental symptoms, such as reaction to percussion in damaged teeth, mobility, and pulp necrosis, are not present, osseointegration should be observed at follow-up. In three cases, the possibility of root damage due to an implant fixture placed too close to each adjacent tooth was perceived on radiographs. However, in all of these cases, there were no clinical symptoms or radiographic changes present in the tooth, and the implants did not exhibit decreased stability or peri-implantitis. Therefore, we can carefully predict that the implant fixture close to the adjacent tooth did not invade the cementum of the root, and therefore did not produce the suspected pulpal damage or periradicular symptoms. In this study, we considered both the implant status as well as the adjacent tooth.
Keywords: Complication, Dental implants
I. Introduction
For partially or totally edentulous patients in Korea and worldwide, dental implants have been widely used as restorative treatment for the loss of mastication ability, esthetics, and phonetic function. Studies on the osseointegration of implants with bone, biodynamics, and other diverse areas have been actively conducted. Nevertheless, the success rate of implants placed in the oral cavity using developed techniques is generally 93%1, although it varies among studies. Causes of implant failure are osseointegration failure, implant placement at the wrong site, lesion around implants, biodynamic failure, etc.1,2
Damage to natural teeth adjacent to implants during implant placement may wield adverse effects on adjacent teeth and may facilitate implant failure; thus emphasizing the importance of its treatments and prevention. Its primary causes include: implant placement in erroneous sites and at an improper placement angle; errors in determining the distance to the adjacent teeth, and; use of excessively wide-type fixtures due to the insufficient height of the residual alveolar bone. Nonetheless, depending on the distance of the fixture to the adjacent teeth, symptoms may be present or absent, and opinions regarding these differences are not consistent between investigators.
Therefore, in these case reports, we discuss the overall causes, symptoms, treatments, and strategies for the prevention of damage to adjacent teeth, which may occur during implant placement.
II. Cases Report
1. Case 1
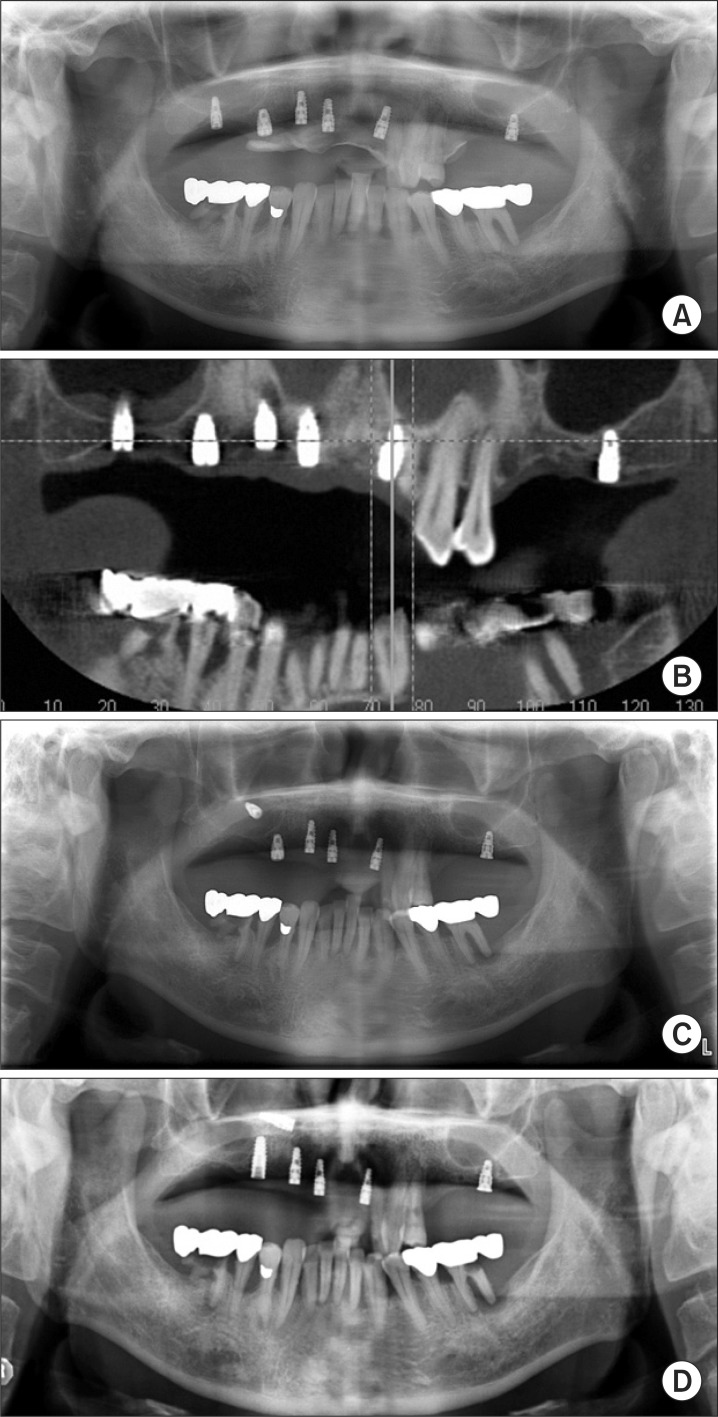
A 63-year-old male patient visited our hospital with chief complaint of uncomfortable current maxillary removable partial denture. There were no special findings in his medical history. Including the immediate implant placement after the extraction of tooth #13, implants were placed in 6 areas (#17, #14, #13, #11, #21, and #27). On the postsurgical panoramic radiographs and computed tomography images, the implant (DAS, 3.8×10 mm; DAS Tech, Gwangju, Korea) placed in #21 was observed to be tilted to the distal side and positioned closely to the adjacent #22.(Figs. 1. A, 1. B) The fixture did not affect the adjacent periodontal ligament space, however. The implant stability quotient (ISQ) using Osstell Mentor (Integration Diagnostics AB, Göteborg, Sweden) was 67. #22 did not show specific clinical and radiological findings.
Fig. 1.
Radiographic findings. A, B. Immediately after installation. C. After 6 months. D. After 18 months.
The follow-up radiographs taken 6 and 18 months after surgery showed no extraordinary findings in the periradicular area of the natural adjacent tooth.(Figs. 1. C, 1. D)
2. Case 2
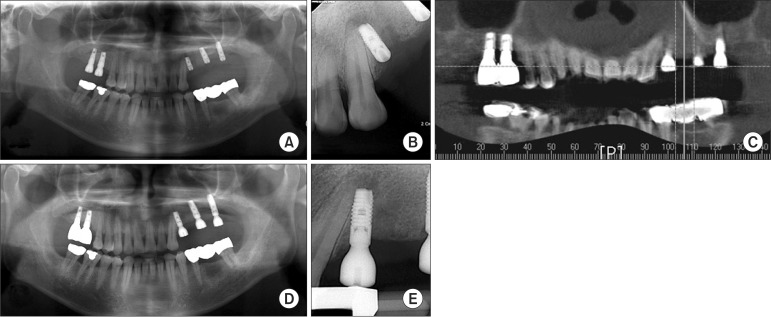
A 55-year-old male patient visited our hospital primarily requiring repair of the implant placed in the missing maxillary molar area. According to his medical history, he had diabetes, which was controlled with medication. Clinical and radiological tests revealed the loss of several maxillary molars (#16, 17, 25, 26, and 27). The left maxillary first premolar (#24) showed a residual root with periradicular inflammation. On the day of the visit, the root was extracted. Because of the patient's personal situation, 18 months passed before an implant was placed in the corresponding area (Astra, 3.5×9.0 mm; OsseoSpeed TX, Astra Tech AB, Mölndal, Sweden), and allogenic bone graft (Allomatrix; Wright Medical Technology Inc., Arlington, TN, USA) was performed simultaneously. ISQ using Osstell Mentor was 72. Nonetheless, the fixture was observed to be located very close to the adjacent tooth (#23).(Figs. 2. A-2. C) In addition, radiolucency was noted in the periradicular area of the fixture. The radiographs taken 14 months later showed that its size was not changed.(Figs. 2. D, 2. E) There were no specific clinical findings in the adjacent natural teeth. After 1 year, the Periotest value (PTV) using PerioTest C (Medizintechnik Gulden, Hessen, Germany) was -4.
Fig. 2.
Radiographic findings. A, B, C. Immediately after installation. D, E. After 14 months.
3. Case 3
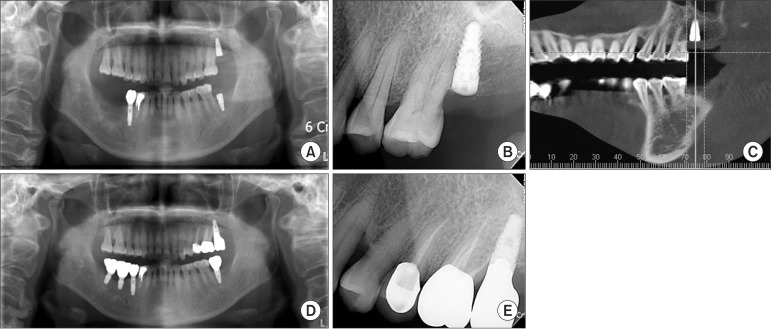
An implant was placed in a 62-year-old female patient due to the loss of the left maxillary second molar (#27) (Biohorizon, 4.6×10.5 mm; Biohorizons Implant Systems Inc., Bir mingham, AL, USA). PTV was 7, which was slightly low. In addition, the postsurgical radiographs showed that, due to the dilaceration of the adjacent natural tooth, the fixture was located near the left maxillary first molar.(Figs. 3. A-3. C) A second surgery was performed after 9 months. PTV was -6 (PerioTest C), and ISQ was 84, which were good levels. One year after surgery, endodontic treatments were performed to resolve hypersensitivity symptoms caused by the fall-out of the prosthesis in the mesial area of the adjacent natural tooth (#26) but were not associated with a fixture placed nearby. The follow-up radiographs did not show special findings.(Figs. 3. D, 3. E)
Fig. 3.
Radiographic findings. A, B, C. Immediately after installation. D, E. After 2 years.
III. Discussion
As the placement of implant prostheses becomes more common in partially edentulous patients, damage to the adjacent teeth due to placement in wide areas must be considered a serious potential side effect.
Causes of such damage include errors in determining the distance to the adjacent teeth by radiological tests, erroneous placement and angle3, direct damage due to the use of excessively wide fixtures owing to the insufficient height of the residual alveolar bone, and indirect damage caused by the generation of excessive heat during osteotomy4. Consequently, due to the invasion of the periodontal ligament space, blood supply is impaired, resulting in the loss of viability of the endodontium5; hence the higher incidence rate of periapical lesions. In addition, the mobility of the tooth may increase6. The damaged natural tooth may require endodontic treatments or apicoectomy; if the symptoms persist, tooth extraction may be necessary7. Additionally, if the integration of implants and the alveolar bone are decreased due to apical inflammation, the bone defect areas may be restored, and the position stability of the fixture may be raised with guided bone regeneration using a flap8,9. If the prognosis is poor, and the symptoms persist, however, the removal of the fixture may ultimately be necessary due to a reduction in the initial stability of implants10. Moreover, this problem may occur not only with simple implants but also with the placement of orthodontic mini-screws.
To prevent the injury of the natural tooth by implants, the slope of the adjacent teeth should be measured accurately using radiographs prior to surgery, and the appropriate placement angle should be determined. This angle is pertinent to the postsurgical direction of mastication, and it is an important factor for the success of the prosthesis. In addition, the presence or absence of dilaceration of the root should be determined4. Finally, the thickness of the alveolar bone surrounding the fixture should be at least 1.0 mm1. This value can reach 1.5 mm depending on the study3. If an implant fixture is located closer than this range, depending on the biological width or stress, the resorption of the bone between the adjacent tooth and implants may be induced11. Errors in detecting this phenomenon can be prevented with the use of the parallel technique when taking intraoral standard images. In panoramic images, a distortion of approximately 25% is present, increasing the possibility of errors; thus, presurgical computed tomography may help ensure accurate diagnosis12,13. In addition, establishing a placement guide is helpful by preparing a surgical stent using a preliminary impression14. During surgery, the equilibrium must be assessed by inserting a guide pin after osteotomy. In placement, to prevent the generation of excessive heat, implants wherein the temperature does not rise above 33.8℃ during a maximum of 5 seconds of drilling should be ensured.
In our 3 cases, the possibility of root injury was increased by the erroneous position and angle during implant placement and movement toward the natural tooth. Nonetheless, specific symptoms of the corresponding implant and the adjacent natural teeth were not observed during the follow-up period. According to other documents, injury of the teeth adjacent to implants may result in poor implant success rate and difficulty in maintaining the viability of the endodontium of the natural tooth. Not all cases with injured natural tooth have increase mobility, loss of viability of the endodontium, or periapical lesions, but these manifestations can be prevented by accurate diagnosis using presurgical radiographs, appropriate placement angle, reduction of generation of heat during implant placement, and appropriate postsurgical treatments through continuous follow-ups.
References
- 1.Chee W, Jivraj S. Failures in implant dentistry. Br Dent J. 2007;202:123–129. doi: 10.1038/bdj.2007.74. [DOI] [PubMed] [Google Scholar]
- 2.Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90:121–132. doi: 10.1016/S0022-3913(03)00212-9. [DOI] [PubMed] [Google Scholar]
- 3.Misch K, Wang HL. Implant surgery complications: etiology and treatment. Implant Dent. 2008;17:159–168. doi: 10.1097/ID.0b013e3181752f61. [DOI] [PubMed] [Google Scholar]
- 4.Sussman HI. Tooth devitalization via implant placement: a case report. Periodontal Clin Investig. 1998;20:22–24. [PubMed] [Google Scholar]
- 5.Sussman HI. Periapical implant pathology. J Oral Implantol. 1998;24:133–138. doi: 10.1563/1548-1336(1998)024<0133:PIP>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Shabahang S, Bohsali K, Boyne PJ, Caplanis N, Lozada J, Torabinejad M. Effect of teeth with periradicular lesions on adjacent dental implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:321–326. doi: 10.1016/s1079-2104(03)00367-6. [DOI] [PubMed] [Google Scholar]
- 7.Kim SG. Implant-related damage to an adjacent tooth: a case report. Implant Dent. 2000;9:278–280. doi: 10.1097/00008505-200009030-00016. [DOI] [PubMed] [Google Scholar]
- 8.von Arx T. Failed root canals: the case for apicoectomy (periradicular surgery) J Oral Maxillofac Surg. 2005;63:832–837. doi: 10.1016/j.joms.2005.02.019. [DOI] [PubMed] [Google Scholar]
- 9.Skoglund A, Persson G. A follow-up study of apicoectomized teeth with total loss of the buccal bone plate. Oral Surg Oral Med Oral Pathol. 1985;59:78–81. doi: 10.1016/0030-4220(85)90120-3. [DOI] [PubMed] [Google Scholar]
- 10.Lindhe J, Berglundh T, Ericsson I, Liljenberg B, Marinello C. Experimental breakdown of peri-implant and periodontal tissues. A study in the beagle dog. Clin Oral Implants Res. 1992;3:9–16. doi: 10.1034/j.1600-0501.1992.030102.x. [DOI] [PubMed] [Google Scholar]
- 11.Tarnow DP, Eskow RN. Preservation of implant esthetics: soft tissue and restorative considerations. J Esthet Dent. 1996;8:12–19. doi: 10.1111/j.1708-8240.1996.tb00904.x. [DOI] [PubMed] [Google Scholar]
- 12.Napier ID. Reference doses for dental radiography. Br Dent J. 1999;186:392–396. doi: 10.1038/sj.bdj.4800121. [DOI] [PubMed] [Google Scholar]
- 13.Tronje G, Eliasson S, Julin P, Welander U. Image distortion in rotational panoramic radiography. II. Vertical distances. Acta Radiol Diagn (Stockh) 1981;22:449–455. doi: 10.1177/028418518102200409. [DOI] [PubMed] [Google Scholar]
- 14.Salama H, Salama MA, Li TF, Garber DA, Adar P. Treatment planning 2000: an esthetically oriented revision of the original implant protocol. J Esthet Dent. 1997;9:55–67. doi: 10.1111/j.1708-8240.1997.tb00919.x. [DOI] [PubMed] [Google Scholar]