Abstract
Patient: Female, 24
Final Diagnosis: DRESS syndrome
Symptoms: Fever • rash • facial and body swelling • muscular pain • diarrhea
Medication: Ciprofloxacin
Clinical Procedure: —
Specialty: Internal Medicine • Hematology
Objective:
Unusual or unexpected effect of treatment
Background:
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) is a rare, potentially life-threatening drug reaction with a mean latency period of 3.9 weeks. It has been described in association with many medications; yet, Ciprofloxacin was reported once in literature to be the offending drug. We are presenting a rare case of Ciprofloxacin-induced DRESS syndrome with symptom onset 2 days after exposure.
Case Report:
A 24-year-old female presented with symptoms suggestive of UTI and was prescribed Ciprofloxacin. Two days later she started to complain of fever, diffuse rash, swelling of her face, arms and flanks, watery diarrhea and muscular pain. Five days after symptom onset she presented to our institution with WBC count 38,810 cells/μL and absolute Eosinophil count 17,080 cell/μL. Peripheral blood smear showed immature Eosinophilic myelocytes and metamyelocytes. Skin biopsy showed superficial perivascular lymphocytic infiltration with dermal edema. Further workup was negative for parasitic infestations, HIV and viral hepatitis, allergic diseases, hematologic and non-hematologic malignancies, vasculitides and autoimmune processes. Ciprofloxacin was discontinued upon admission and the patient started to improve quickly. Patient was followed in clinic after 3 weeks and was completely asymptomatic with WBC count 7,250 cell/μL and absolute Eosinophil count 2,900 cell/μL.
Conclusions:
DRESS syndrome is a possible complication of Ciprofloxacin treatment that clinicians should consider. Shorter latency period might be a unique feature of Fluoroquinolone-induced DRESS syndrome. According to RegiSCAR scoring system, our case is categorized as (probable) with a score of (4). In fact, the vast majority of reported cases are classified as (probable/definite).
Keywords: DRESS syndrome, eosinophilia, ciprofloxacin
Background
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) is a rare, potentially life-threatening adverse drug reaction that includes severe skin eruption, fever, hematologic abnormalities and multi-organ involvement. The estimated incidence of this syndrome ranges from 1 in 1000 to 1 in 10,000 drug exposures [1]. DRESS syndrome is usually characterized by long latency period between administration of the offending drug and symptom onset with a mean of 3.9 weeks (range 0.5–16 weeks) [2]. Bocquet et al. [3] in 1996 first proposed the use of the acronym (DRESS) to describe this entity and since that time DRESS syndrome has been well described in association with many medications. In a literature review conducted by Cacoub et al. [2]; 172 cases of DRESS syndrome were reported between 1997 and 2009 with a total of 44 culprit drugs, yet, Ciprofloxacin was described merely once in literature to be the offending drug [4]. Herein, we are presenting a rare case of Ciprofloxacin-induced DRESS syndrome with an onset of symptoms only 2 days after drug exposure.
Case Report
A 24-year-old Hispanic female without significant past medical history presented with symptoms suggestive of UTI and was prescribed Ciprofloxacin. Two days later she started to complain of fever (highest 38.8°C), pruritic skin rash involving the trunk and extremities, swelling of her face, arms and flanks, watery diarrhea with diffuse muscular pain and tenderness. Five days after symptom onset she presented to our institution with worsening symptoms. Her WBC count upon admission was 38,810 cell/μL with absolute Eosinophil count 17,080 cell/μL. Peripheral blood smear showed predominance of immature Eosinophilic myelocytes and metamyelocytes without atypical cells or blasts. Biopsy of one of the skin lesions showed mild superficial perivascular lymphocytic and mononuclear leukocytes infiltration with mild dermal edema (Figure 1). CT scan of the abdomen and pelvis done in the emergency room showed small bilateral pleural effusions with stranding suggestive of edema in the deep subcutaneous soft tissues anterior to the fascia of the abdominal muscles and posterior to the paraspinal muscles (Figure 2).
Figure 1.
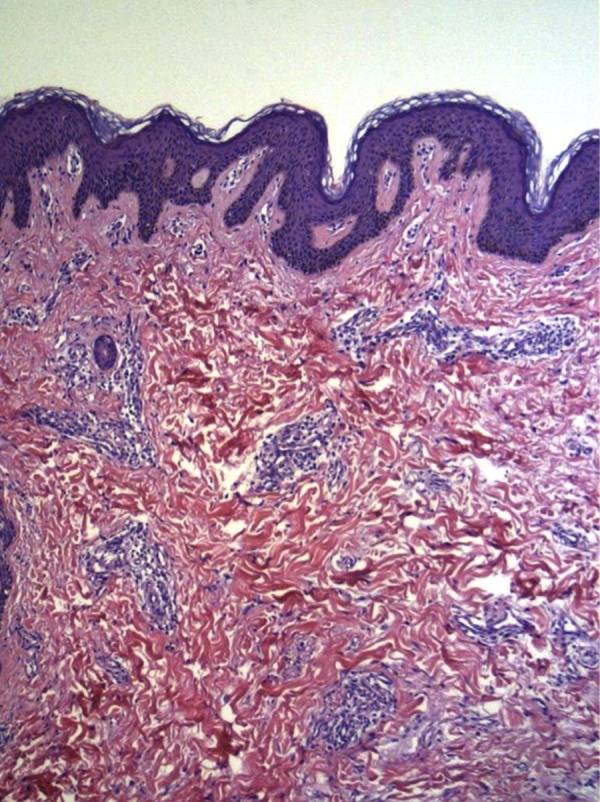
Skin biopsy showing mild superficial perivascular lymphocytic and mononuclear leukocytes infiltration with mild dermal edema.
Figure 2.
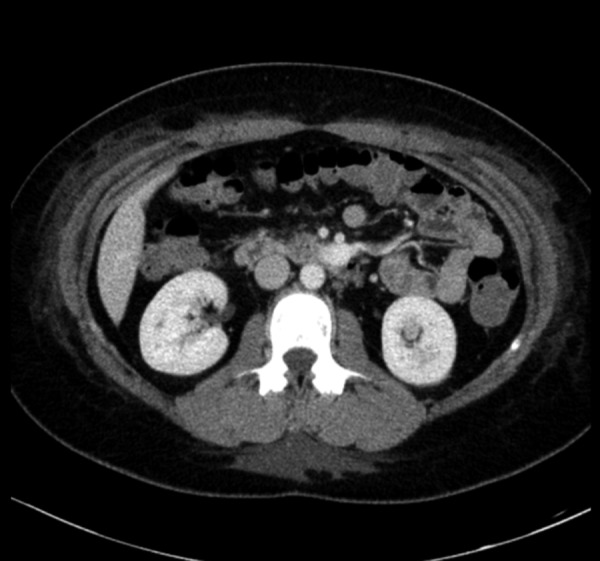
CT scan of the abdomen showing stranding suggestive of edema in the deep subcutaneous soft tissues anterior to the fascia of the abdominal muscles and posterior to the paraspinal muscles.
Work up for Eosinophilia showed normal levels of serum IgE, complement and tryptase. Stool studies failed to show any evidence of ova or parasites. Blood cultures along with serological studies for Strongyloidosis, Coccidioidomycosis, HIV and viral hepatitis infections were all negative. Furthermore, serological studies for Rheumatoid factor, ANA and ANCA were also negative. Flourescent in-situ hybridization (FISH) studies were negative for break point cluster region-abelson translocation and platelet derived growth factor (pdgfr) alpha and beta translocations. Polymerase chain reaction (PCR) study was performed for JAK-2 mutation and was also negative.
Ciprofloxacin was discontinued upon admission and the patient symptoms started to improve quickly with supportive care. Patient was discharged after 4 days of hospitalization. She was followed in clinic 3 weeks after discharge and was found to be completely asymptomatic with a normal WBC count (7,250 cell/μL) and dramatically improved absolute Eosinophil count (2,900 cell/μL).
Discussion
DRESS syndrome is a challenging entity with no current reliable standard to establish the diagnosis. Clinicians must first exclude other potentially serious conditions including infections, neoplastic processes, autoimmune disorders, connective tissue diseases and allergic conditions [5]. The proposed diagnostic criteria are based on clinical and laboratory findings. Clinical testing and biopsy can be helpful, but are not always specific [5].
The time relationship between administration of the drug and symptom onset in our case was short in comparison to other reported cases of DRESS syndrome which might be a unique feature of Ciprofloxacin-induced DRESS syndrome. The skin biopsy findings in our case are consistent with the histological description typically found in this syndrome, yet it’s not pathognomonic. The extensive workup that was done basically ruled out other possible causes of hyper-Eosinophilia including infections, autoimmune and connective tissue diseases and common Eosinophilic myeloproliferative disorders. The rapid resolution of symptoms in our patient after discontinuation of Ciprofloxacin makes the diagnosis of DRESS syndrome more likely.
The European Registry of Severe Cutaneous Adverse Reaction (RegiSCAR) study group expanded on the diagnostic criteria proposed by Bocquet et al and devised a scoring system to help establish the diagnosis of DRESS syndrome [6]. According to the RegiSCAR scoring system our case scored (4) which will place it in the (probable) category. In fact, the vast majority of reported cases are classified as (probable/definite) [2].
Conclusions
DRESS syndrome is a possible complication of Ciprofloxacin treatment that clinicians should keep in mind. Shorter latency period between the exposure to the drug and onset of symptoms might be a unique feature of Fluoroquinolone-induced DRESS syndrome.
References:
- 1.Fiszenson-Albala F, Auzerie V, Mahe E, et al. A 6-month prospective survey of cutaneous drug reactions in a hospital setting. Br J Dermatol. 2003;149:1018–22. doi: 10.1111/j.1365-2133.2003.05584.x. [DOI] [PubMed] [Google Scholar]
- 2.Cacoub P, Musette P, Descamps V, et al. The DRESS syndrome: a literature review. Am J Med. 2011;124(7):588–97. doi: 10.1016/j.amjmed.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 3.Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS) Semin Cutan Med Surg. 1996;15:250–57. doi: 10.1016/s1085-5629(96)80038-1. [DOI] [PubMed] [Google Scholar]
- 4.Artuković M, Kustelega J, Lugović-Mihić L. DRESS syndrome with mild manifestations as a diagnostic and therapeutic problem: case report. Acta Clin Croat. 2010;49(4):479–84. [PubMed] [Google Scholar]
- 5.Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: Part I. Clinical perspectives. J Am Acad Dermatol. 2013;68(5):693e1–14. doi: 10.1016/j.jaad.2013.01.033. quiz 706–8. [DOI] [PubMed] [Google Scholar]
- 6.Kardaun SH, Sidoroff A, Valeyrie-Allanore L, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007;156:609–11. doi: 10.1111/j.1365-2133.2006.07704.x. [DOI] [PubMed] [Google Scholar]


