Abstract
Patient: Female, 78
Final Diagnosis: Cerebral hyperperfusion syndrome
Symptoms: —
Medication: —
Clinical Procedure: Endovascular embolectomy
Specialty: Neurology
Objective:
Unknown ethiology
Background:
Cerebral hyperperfusion syndrome (cHS) is a well known but rare complication after carotid endarterectomy, carotid angioplasty with stenting, and stenting of intracranial arterial stenosis.
The clinical presentation may vary from acute onset of focal oedema (stroke-like presentation) and intracerbral hemorrhage to delayed (>24h hours after the procedure) presentation with seizures, focal motor weakness, or late intracerebral hemorrhage. The incidence of cHS after carotid endarterectomy ranges from 0–3% and defined as an increase of the ipsilateral cerebral blood flow up to 40% over baseline in ultrasound.
Case Report:
We present a case of a 78-year-old woman with an acute ischemic stroke due to left side middle cerebral artery territory with right sided hemiparesis and aphasia (NIHSS 16). After systemic thrombolysis embolectomy using a retractable stent (Solitaire® device) was performed and resulted in complete and successful recanalization of MCA including its branches about 210 minutes after symptom onset but, partial dislocation of thrombotic material into the anterior cerebral artery (ACA).
Conclusions:
Cerebral hyperperfusion syndrome should be considered in patients with clinical deterioration after successful recanalisation and the early diagnosis and treatment may be important for neurological outcome after endovascular embolectomy
Keywords: embolectomy, hyperperfusion syndrome, ischemic stroke, middle cerebral artery occlusion
Background
Cerebral hyperperfusion syndrome (cHS) is a well known but rare complication after carotid endarterectomy, carotid angioplasty with stenting, and stenting of intracranial arterial stenosis [1,2]. The clinical presentation may vary from acute onset of focal oedema (stroke-like presentation) and intracerebral hemorrhage to delayed (>24h hours after the procedure) presentation with seizures, focal motor weakness, or late intracerebral hemorrhage. The incidence of cHS after carotid endarterectomy ranges from 0–3% and defined as an increase of the ipsilateral cerebral blood flow up to 40% over baseline in ultrasound [3,4]. Predisposing risk factors for developing cHS are thought to be exhausted cerebrovascular reserve and post-stenotic low flow. However, and to the best of our knowledge, despite the growing numbers of endovascular thrombectomy in cases of complete intracranial artery occlusion this complication has not been reported for this type of intervention. We demonstrate a case of hyperperfusion syndrome with distinct MRI patterns of neurovascular injury in a patient following embolectomy using the Solitaire® device.
Case Report
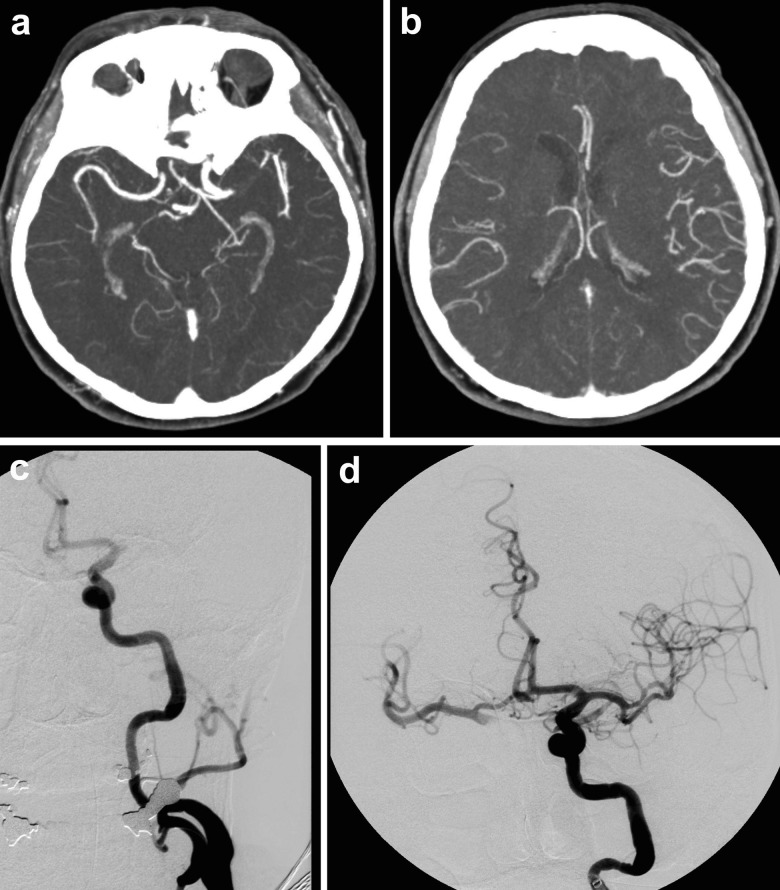
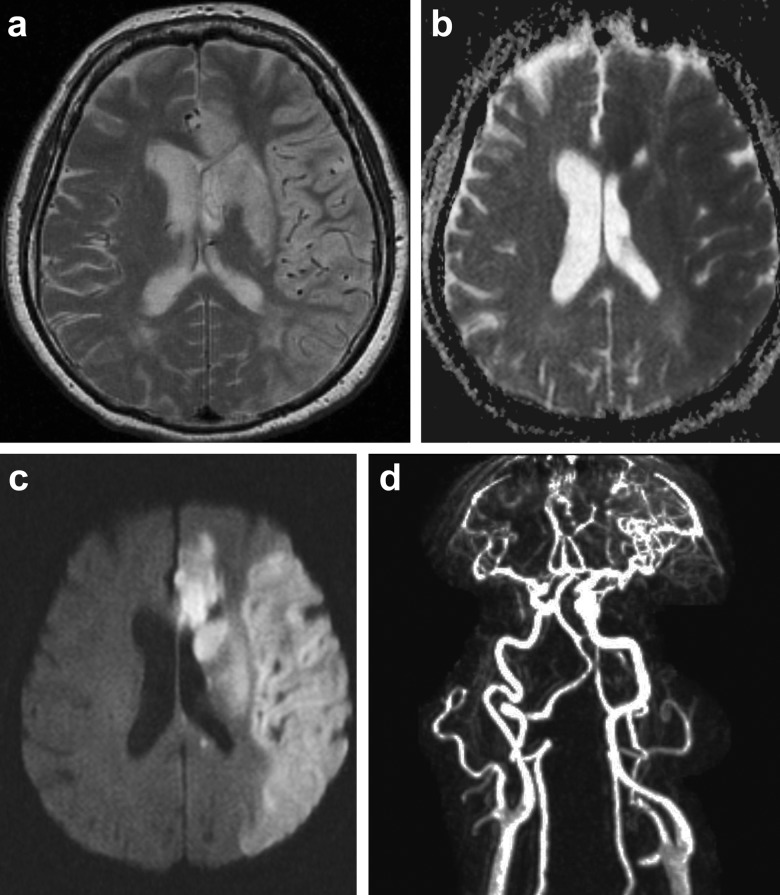
A 78-year-old woman with an acute ischemic stroke due to middle cerebral artery occlusion with right sided hemiparesis and aphasia (NIHSS 16), left middle cerebral artery occlusion was already diagnosed in the prehospital phase using portable transcranial color-coded sonography (TCCS), and was treated with standard systemic rtPA 130 minutes after symptom onset and after cerebral computed tomography (cCT) excluded intracerebral hemorrhage [5]. Furthermore, cCT showed absence of early stroke signs, a dense artery sign at the left MCA which confirmed as complete MCA occlusion of 10mm length by CT-angiography (CTA) with good collateralization into the Sylvian fissure on CTA (Figure 1). Decision to perform embolectomy was based on the length of MCA occlusion and good collateral score, and performed under general anesthesia [6,7]. Embolectomy using a retractable stent (Solitaire® EV3) resulted in complete and successful recanalization of the MCA and its branches about 210 minutes after symptom onset (Figure 1). However, partial dislocation of thrombotic material into the anterior cerebral artery (ACA) occurred, and treatment using the GpIIb/IIIa inhibitor tirofiban was initiated for 24 hours according to the PRISM plus protocol [8]. The following day TCCS revealed an increase of MCA peak systolic flow to 1.6m/sec compared to 1m/sec in the right MCA, and cCT confirmed small ACA infarction and mild left hemispheric oedema. After frustrated weaning from ventilation, magnetic resonance imaging (MRI) was performed 6 days later revealing cortical swelling of the complete left MCA territory however sparing the lateral insula, strong diffusion weighted lesions in the ACA and slightly attenuated diffusion abnormality in the left MCA territory, and dilated left internal carotid artery and MCA vessels. The T2-weighted sequences demonstrated dilated MCA branches indicative for compromised vasoreactivity (Figure 2). In absence of severe atherosclerosis and other risk factors, stroke was classified as cardioembolic due to intermittend atrial fibrillation which, however, was not detected during hospital stay. 7 days after onset, left sided MCA flow was still increased to 2 m/sec, tracheotomy was performed and the patient transferred to neurological rehabilitation with severe left hemispheric deficits.
Figure 1.
(A) Maximum intensity projection reconstruction of CT-angiography demonstrates left M1 occlusion 130 minutes after symptom onset. (B) Good contrast of left lateral insular branches indicates good collateral flow into the left MCA territory. (C) Initial digital subtraction angiography (DSA) at intervention demonstrates complete left MCA mainstem occlusion. (D) Post-embolectomy DSA shows complete perfusion recovery of left side MCA 210 minutes after symptom onset.
Figure 2.
(A) T2-weighted MRI 6 days later demonstrates partial left ACA ischemia and basal ganglia and a homogenous lesion of left MCA territory sparing the subcortical white matter. Note the pronounced vessel of the left MCA territorium. (B) Apparent diffusion maps maps showing partial anterior and complete MCA infarction. (C) Corresponding diffusion weighted imaging. Note the distinct lesion pattern in the partial ACA and basal ganglia infarct compared to the MCA territory. (D) Contrast-enhanced MR angiography demonstrates the pronounced hyperperfusion of the left MCA territory.
Discussion
Cerebral hyperperfusion syndrome is a rare but expected complication following rapid revascularization especially embolectomy in acute intracranial artery occlusion. However, as this may be the first case published cHS may be underestimate as patients are often sedated after the procedure and separation of the new lesion from the initial ischemic injury is difficult. The diagnosis of cHS in this case is based on the elevated MCA flow in MRA and TCCS, the distinct lesion pattern in T2 sparing the insula and the distinct pattern in dwi distinguishing partial ACA territory stroke and MCA cHS. Apart from acute revasularisation, potential risk factors for the development of cHS are similar to the predisposing for arteriosclerosis, and including diabetes, age ≥72 year, previous minor stroke and pre-existing hypertensive microangiopathy especially in patients high grade stenosis with poor collateral flow, increased peak flow velocity, a contralateral carotid occlusion, intraoperativ ischemia resulting in exhausted cerebrovascular reserve [1,2]. The ethology of cHS has not been fully understood, but impaired autoregulation i.e. by endothelial nitric oxygen production and rapid reflow into the cerebral vasculature add to vasodilatation and free radical cause further damage to the cerebral endothelium including the blood-brain barrier [9].
Conclusions
Cerebral hyperperfusion syndrome should be considered in patients with clinical deterioration after successful recanalisation and the early diagnosis and treatment may be important for neurological outcome after endovascular embolectomy. Especially in patients still under artificial ventilation the diagnosis of cHS is challenging and routine transcranial Doppler sonography may routinely be considered for early detection and initiation of rapid further diagnostics especially MRI. Therapy may consist in rapid normalization of blood pressure, treatment of cerebral oedema, free radical scavengers, and anti-convulsant therapy as potential basic concepts [10].
Acknowledgments
The authors thank all physician, therapists and nurses of Department of Neurology, University of Regensburg.
Footnotes
Statement
No potential conflict of interes relevant to this article were reported or known.
References:
- 1.Halliday A, Mansfield A, Marro J, et al. Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomised controlled trial. Lancet. 2004;363(9420):1491–502. doi: 10.1016/S0140-6736(04)16146-1. [DOI] [PubMed] [Google Scholar]
- 2.van Mook WN, Rennenberg RJ, Schurink GW, et al. Cerebral hyperperfusion syndrome. Lancet Neurol. 2005;4(12):877–88. doi: 10.1016/S1474-4422(05)70251-9. [DOI] [PubMed] [Google Scholar]
- 3.Jorgensen LG, Schroeder TV. Defective cerebrovascular autoregulation after carotid endarterectomy. Eur J Vasc Surg. 1993;7(4):370–79. doi: 10.1016/s0950-821x(05)80252-x. [DOI] [PubMed] [Google Scholar]
- 4.Lieb M, Shah U, Hines GL. Cerebral Hyperperfusion Syndrome following Carotid Intervention. A Review. Cardiol Rev. 2011 doi: 10.1097/CRD.0b013e318237eef8. Epub 2011/12/21. [DOI] [PubMed] [Google Scholar]
- 5.Schlachetzki F, Herzberg M, Holscher T, et al. Transcranial Ultrasound from Diagnosis to Early Stroke Treatment – Part 2: Prehospital Neurosonography in Patients with Acute Stroke – The Regensburg Stroke Mobile Project. Cerebrovasc Dis. 2012;33(3):262–71. doi: 10.1159/000334667. [DOI] [PubMed] [Google Scholar]
- 6.Riedel CH, Zimmermann P, Jensen-Kondering U, et al. The importance of size: successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length. Stroke. 2011;42(6):1775–77. doi: 10.1161/STROKEAHA.110.609693. [DOI] [PubMed] [Google Scholar]
- 7.Ribo M, Flores A, Rubiera M, et al. Extending the time window for endovascular procedures according to collateral pial circulation. Stroke. 2011;42(12):3465–69. doi: 10.1161/STROKEAHA.111.623827. [DOI] [PubMed] [Google Scholar]
- 8.Inhibition of the platelet glycoprotein IIb/IIIa receptor with tirofiban in unstable angina and non-Q-wave myocardial infarction. Platelet Receptor Inhibition in Ischemic Syndrome Management in Patients Limited by Unstable Signs and Symptoms (PRISM-PLUS) Study Investigators. N Engl J Med. 1998;338(21):1488–97. doi: 10.1056/NEJM199805213382102. [DOI] [PubMed] [Google Scholar]
- 9.Sbarigia E, Speziale F, Giannoni MF, et al. Post-carotid endarterectomy hyperperfusion syndrome: preliminary observations for identifying at risk patients by transcranial Doppler sonography and the acetazolamide test. Eur J Vasc Surg. 1993;7(3):252–56. doi: 10.1016/s0950-821x(05)80005-2. [DOI] [PubMed] [Google Scholar]
- 10.Ogasawara K, Konno H, Yukawa H, et al. Transcranial regional cerebral oxygen saturation monitoring during carotid endarterectomy as a predictor of postoperative hyperperfusion. Neurosurgery. 2003;53(2):309–14. doi: 10.1227/01.neu.0000073547.86747.f3. discussion 14–15. [DOI] [PubMed] [Google Scholar]