Abstract
Adolf Meyer (1866–1950) did not see schizophrenia as a discrete disorder with a specific etiology but, rather, as a reaction to a wide variety of biopsychosocial factors. He may have been right. Today, we have evidence that gene mutations, brain injury, drug use (cocaine, amphetamine, marijuana, phencyclidine, and steroids), prenatal infection and malnutrition, social isolation and marginalization, can all result in the signs and symptoms of schizophrenia. This clinical picture is generally associated with supersensitivity to dopamine, and activates dopamine neurotransmission that is usually alleviated or blocked by drugs that block dopamine D2 receptors. While the dopamine neural pathway may be a final common route to many of the clinical symptoms, the components of this pathway, such as dopamine release and number of D2 receptors, are approximately normal in schizophrenia patients who are in remission. Postmortem findings, however, reveal more dimers of D1D2 and D2D2 receptors in both human schizophrenia brains and in animal models of schizophrenia. Another finding in animal models is an elevation of high-affinity state D2High receptors, but no radioactive ligand is yet available to selectively label D2High receptors in humans.
It is suggested that synaptic dopamine supersensitivity in schizophrenia is an attempt at compensation for the original damage by heightening dopamine neurotransmission pathways (preparing the organism for fight or fiight). The dopamine overactivity is experienced subjectively as overstimulation, which accounts for some of the clinical symptoms, with attempts at dampening down the stimulation leading to still other symptoms. Reaction and counter-reaction may explain the symptoms of schizophrenia.
Keywords: D1D2 receptor dimer, D2 receptor, D2D2 receptor dimer, Dopamine release, Mutation, Psychosis, Psychotogens
1. Introduction
Most investigators acknowledge that there are many risk factors that contribute to schizophrenia. These include various gene mutations (both new and inherited), prenatal malnutrition or infection, birth anoxia/injury, brain trauma, drug abuse (cocaine, amphetamine, marijuana, phencyclidine, and steroids), social isolation and marginalization. Nevertheless, despite the impact of many different factors, the brain can react to them all similarly to produce the signs and symptoms of schizophrenia, the specific experiential and behavioral expression of which can, and does, vary from patient to patient.
This common general reaction is associated with supersensitivity to dopamine (Lieberman et al., 1987; Seeman, 2011), and overactivity of dopamine neurotransmission, which is usually alleviated or blocked by drugs that block dopamine D2 receptors (Madras, 2013).
At present, there is no diagnostic test or unique biological marker for schizophrenia, either associated with or extraneous to the dopamine system. For example, while all antipsychotics target the dopamine D2 receptor, the number of these receptors has been found to be approximately normal in the cerebral cortex of patients, as long as they have not been medicated with antipsychotics (Seeman, 2013a, in press). Numbers may differ, however, in specific parts of the brain, such as an apparent reduction in presynaptic D2 receptors in the thalamus (reviewed by Seeman, in press).
The psychopathology and molecular mechanisms that trigger overactivity at the D2 receptor, either by presynaptic or postsynaptic events, offer a potential pathway that might unravel the vulnerable elements that underlie schizophrenia. For over half a century, a door into the psychotic brain has been opened via the strategy of searching for the mechanism of antipsychotic drug action and working backwards to identify the brain networks involved in psychosis. The first effective drugs were chlorpromazine (Delay et al., 1952) and the related phenothiazines, followed by the haloperidol-type antipsychotics and the more recent second generation antipsychotics, with their diverse structures and receptor binding profiles. Despite the different chemical structures and the multi-receptor affinity of many of the effective drugs, a common target for all the antipsychotics is now recognized to be the so-called antipsychotic receptor, more commonly known as the dopamine D2 receptor (Seeman et al., 1975).
While D2-blocking drugs usually alleviate delusions and hallucinations within a matter of a few days (Delay et al., 1952; Kapur et al., 2005), the dissipation of negative symptoms, such as apathy, and the cognitive difficulties associated with schizophrenia, may require antipsychotics that act on targets other than the D2 receptor. At present, however, potentially new antipsychotic drugs acting on other targets such as receptors for dopamine D1, D3, D4, D5, cannabinoid-1, neurokinin-3, serotonin, neurotensin, ampakines, and sigma sites have not been shown to be clinically effective.
While there is renewed interest in the hypoglutamate theory of psychosis based on the fact that glutamate antagonists such as phencyclidine and ketamine trigger psychosis, it is known clinically that haloperidol (which has high affinity for D2, but low affinity for glutamate receptors) effectively alleviates the psychosis secondary to phencyclidine or ketamine (Giannini et al., 1984–1985–2000). Moreover, it is uncertain whether glutamate receptor agonists such as pomaglumetad methionil or LY404,039 have any antipsychotic efficacy. A four-week trial had little or no efficacy against positive symptoms or negative signs when compared to olanzapine (Kinon et al., 2011; Seeman, 2012a).
2. The historical view of schizophrenia as a reaction
The view of schizophrenia as a reaction to a variety of potential causes was promoted by the Swiss American psychiatrist, Adolf Meyer (1866–1950), in the early 1900s (Noll, 2011; Yuhas, 2013). Meyer reframed mental illness in terms of biopsychosocial “reaction types” rather than biologically-specific disease entities. As early as 1906, Meyer considered dementia praecox to be a “reaction type,” a cluster of maladaptations that, together, constituted an attempt to cope with biopsychosocial stressors.
The present suggestion that schizophrenia may be a hyperactive dopamine supersensitive reaction to a variety of possible causes fits Meyer’s general framework of schizophrenia as a reactive disorder.
3. The dopamine supersensitive reaction
The present work develops the idea that synaptic dopamine supersensitivity compensates for an original early injury (or mutation) by heightening dopamine neurotransmission pathways. Subjectively, the patient experiences this as overstimulation, a generally unpleasant sensation that leads to symptoms and to attempts at adaptation. Out of such attempts at compensation arise the variety of signs and symptoms that have been identified with schizophrenia. Patients with schizophrenia, whether treated or untreated, are known to be supersensitive to dopamine-like compounds (Lieberman et al., 1987), with intensification of symptoms or the development of new symptoms following the administration of dopamine-like agonists. The present mini-review outlines “the schizophrenia reaction” in terms of the molecular components of synaptic dopamine receptor sensitivity and the patient’s automatic compensation.
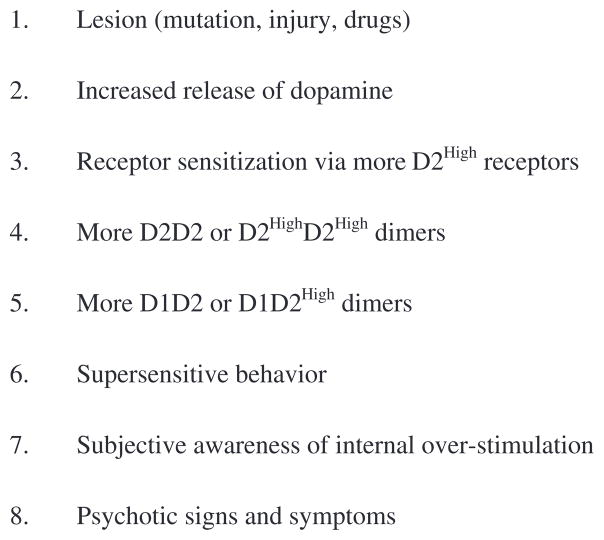
While there are many molecular components underlying the biological basis of the schizophrenia reaction, it is not known, of course, in what sequence such components become active. Nevertheless, for the present purpose of this mini-review, the order of these components is organized as follows (see also Fig. 1):
Fig. 1.
Biochemical progression from lesion to psychosis.
Neuron cell pruning.
Activation of dopamine release.
Activation of dopamine D2 receptors.
Induction of dopamine D2High receptors.
At present, the evidence indicates that the signs and symptoms of psychosis, originating from whatever cause, are associated with an overactive dopamine system. This may result from a combination of increased presynaptic neural pruning, a high release of dopamine (Howes et al., 2012), altered numbers of dopamine D2 receptors (Seeman, 2013a, in press), and/or an increased sensitivity of the D2 receptor to dopamine (Seeman, 2011). This view is supported by the fact that the positive symptoms of delusions and hallucinations are alleviated in the majority of patients by D2-blocking medications.
4. The schizophrenia supersensitive reaction and presynaptic neuron pruning
The automatic reduction of central nervous system neurons, known as pruning, is a well-known phenomenon (see Maor-Nof and Yaron, 2013, for refs.). In humans, pruning of dopamine neurons occurs between 2 and 20 years of age and then slowly continues at between 2% and 3% per decade (Seeman et al., 1987a,b).
However, in the schizophrenia thalamus, several reports show evidence that suggest that there may be fewer than normal presynaptic D2 receptors and fewer presynaptic terminals, as monitored by benzamide ligands (Buchsbaum et al., 2006; Kegeles et al., 2010; Talvik et al., 2003, 2006; Tuppurainen et al., 2006; Yasuno et al., 2004), especially in association with a genetic variant in the dopamine D2 receptor (with a T in rs 1076560 in intron 6) (reviewed by Seeman, in press). Such reductions may be a result of neural pruning in the thalamus.
Neural presynaptic pruning would be expected to lead to denervation supersensitivity in a given specific brain region, analogous to that which occurs in early stages of Parkinson’s disease.
5. The schizophrenia supersensitive reaction via dopamine release
It has been established that patients with schizophrenia release more endogenous dopamine than do individuals without schizophrenia, as measured by a challenge with a low dose of amphetamine (Laruelle et al., 1999). This effect of amphetamine occurs during the acute stages of schizophrenia but not when the patients are in clinical remission.
In the case of animal studies, it is not known whether dopamine release is increased in all of the many animal models of psychotic activity.
6. The schizophrenia supersensitive reaction via dopamine D2 receptors
As for the number of dopamine D2 receptors in the human brain striatum, these have finally been determined to be approximately normal (reviewed by Seeman, 2013a, in press), following an extensive number of earlier reports (e.g., Corripio et al., 2011; Farde et al., 1990).
However, as mentioned above, there is consistent suggestive evidence of reduced presynaptic terminals and reduced presynaptic numbers of dopamine D2 receptors in the schizophrenia thalamus (Seeman, in press). Such reductions would inevitably lead to denervation supersensitivity in this region.
7. The schizophrenia supersensitive reaction, dopamine D2High receptors, and dimers
Although the total number of D2 receptors in the human striatum may be normal, animal models of psychotic behavior (brain lesions, gene mutations, or harm from psychotogens) all lead to an increase in D2High receptors, which is the high-affinity state or the functional state of the D2 receptor (Seeman, 2011). Such factors include brain lesions in the hippocampus, frontal cortex, or substantia nigra, and various gene knock-out mutations in mice, including those for the metabotropic glutamate receptors 2 and 3, the GABA B1 receptor, the trace amine 1 receptor, the dopamine D4 receptor, the beta-adrenoceptor, and genes for dopamine-beta-hydroxylase, G-protein receptor kinase, the postsynaptic density 95, catecholamine-O-methyl-transferase, the dopamine transporter, and RGS-9 (Regulator of G-protein signaling 9).
In addition, the proportion of D2High receptors increased in rat striata after administration of the following drugs: corticosterone, amphetamine, methamphetamine, phencyclidine, cocaine, caffeine, marijuana congeners, and quinpirole.
Such an elevation of D2High receptors in more than twenty animal models of psychosis (Seeman, 2011) is consistent with the long-standing observation that schizophrenia patients are more sensitive than control subjects to dopamine-like stimulants such as methylphenidate (Lieberman et al., 1987).
However, at present, the functional state of the D2 receptor cannot be measured in humans. The agonists (such as [11C]PHNO) that have been used to study this issue (Graff-Guerrero et al., 2009) do not selectively label D2High receptors. Radioactive agonists such as [11C] PHNO label both D2High and D2Low receptors, which may explain the inability to selectively measure D2High receptor numbers in human brain scans (Seeman, 2012b). However, the new long-lived [18F]-agonist ligand may be able to label D2High sites successfully in the future (Sromek et al., 2011).
In addition to an increase in the proportion of D2High receptors, there is an increase in the proportion of D2D2 dimers (Wang et al., 2010) and D1D2 dimers (Perreault et al., 2010) in postmortem schizophrenia brain striatal tissue (compared to non-affected brains), findings that are associated with an elevation in D2High receptors.
While it is well established that long-term administration of antipsychotic medication can increase the number of dopamine D2 and D2High receptors and their sensitivity to dopamine (Samaha, 2013; Silvestri et al., 2000), the antipsychotics at the same time effectively reduce the number of D2High receptors that have previously been induced by a psychotogen such as amphetamine (Seeman, 2009).
8. Idiopathic supersensitivity in schizophrenia, and antipsychotic-induced supersensitivity
Moreover, while the schizophrenia reaction may be based on dopamine supersensitivity, prolonged antipsychotic treatment can also add to such supersensitivity. This view is supported by the general clinical observation that sudden withdrawal of antipsychotics can precipitate an acute episode of psychosis (Chouinard and Chouinard, 2008).
Because the dopamine supersensitive reaction in schizophrenia is somewhat similar to the dopamine supersensitivity that is induced by antipsychotic drugs, clarifications have been made by Chouinard and colleagues. For example, these authors earlier hypothesized that schizophrenia was an idiopathic dopamine deficiency disease associated with dopamine supersensitivity (Chouinard and Jones, 1978; Reith et al., 1994). They later suggested that some severe and persistent psychotic symptoms could emerge in association with antipsychotic-induced dopamine supersensitivity (Chouinard, 1990; see also Iyo et al., 2013; Kimura et al., 2013; Tadokoro et al., 2012).
In addition, antipsychotic-induced dopamine supersensitivity can occur together with tardive dyskinesia, which appears to be associated with a loss of cholinergic neurons as well as dopamine neurons (Miller and Chouinard, 1993; Seeman and Tinazzi, 2013).
9. The schizophrenia experiential/behavioral reaction to the supersensitive synapse
Supersensitivity at the level of the synapse can lead to clinical symptoms either directly or via compensation to dopamine overactivity. This is seen in the core symptoms of schizophrenia such as a) misattributions or delusions, b) altered perceptions or hallucinations, c) cognitive deficits, d) disorganization (thought disorder), e) isolation and amotivation (negative signs), and also in symptoms that frequently accompany schizophrenia, such as f) altered mood (depression, ecstasy, and terror) and g) altered movement (agitation, dyskinesia, and catatonia).
9.1. Misattributions or delusions
The dopamine supersensitive state can lead to excess thoughts and excess speed of thoughts, which makes them especially vivid. These actions can be replicated by a variety of hallucinogen agonists known to be active at the dopamine D2 receptor (Seeman et al., 2009). The vividness of the thoughts lends to them a sense of urgency and an aura of certainty. Delusions are misattributions that are experienced as imperative and believed in with unshakeable conviction. There is evidence that overactivity of the dopamine system can kick start the procession of events that leads to delusion formation (Howes and Kapur, 2009).
9.2. Hallucinations
Hallucinations are most frequently understood as defects of source monitoring (Garrett and Silva, 2003). Memories and inner thoughts that flood the brain through supersensitive D2 receptors are experienced as coming from the outside. This has been empirically validated by Brébion et al. (2009). The more rapid the perceptions, the more errors in context processing and subsequent experience of attributing inner sensations to external stimuli. Abnormal perceptions such as voices heard in one’s head, visions, smells, and somatic sensations may all result from dopamine overactivity.
9.3. Cognitive deficits
The probability that dopamine supersensitivity can lead to cognitive difficulties is shown by the fact that D2 receptors, selectively genetically elevated in the striatum, reduce cognitive performance in animals (Kellendonk et al., 2006). Attention and memory problems in schizophrenia may directly result from dopamine overstimulation and are worsened by the lowered self-confidence that ensues from them.
9.4. Thought disorder
Thought disorder may fall into the category of compensation rather than result directly from overstimulated synapses. Patients frequently appear to be playing with words, rearranging them idiosyncratically as poets do. This has been referred to as ‘swerves and cryptic references’ (Byerley et al., 2005), a form of juggling thoughts that come too swiftly, perhaps to make them more manageable. A problem with communication or ‘unconventional discourse’ is a hallmark of schizophrenia (Elvevåg et al., 2010). Many of the brain regions where dopamine sensitivity occurs are intimately associated with the language. In addition to Broca’s area, these regions include Wernicke’s area (comprehension), the left temporal gyrus (language storage and retrieval), the insula, the anterior cingulate gyrus, the left inferior frontal cortex, as well as portions of the thalamus, and cerebellum (Chouvardas, 1996; Nieuwenhuys et al., 2008). All these brain regions contain dopamine D2 receptors, but at densities that are between 20% and 50% of the densities found in the caudate/putamen region (Charuchinda et al., 1987; Hall et al., 1995).
9.5. Negative signs and symptoms
The negative signs and symptoms of schizophrenia, such as social isolation, amotivation, lethargy, can be understood as wholly reactive —compensations designed to ward off dopamine overstimulation (Corin and Lauzon, 1992).
9.6. Mood changes
Many individuals with schizophrenia suffer from oscillations of mood. The biochemical basis may well be the existence of high- and low-affinity states of the D2 receptor, with the D2High and D2Low receptors rapidly interconverting, depending on the metabolism of GDP and GTP within the cell (Seeman, 2013b). It should be noted that the two states of D2High and D2Low are constantly interconverting, and that synaptic and clinical dopamine sensitivity can change in a matter of minutes, depending on the metabolism of these two guanine nucleotides. Ups and downs of mood are dealt with differently by different individuals. Routinization and stereotypy are one way, accounting for the prevalence of obsessive–compulsive symptoms (nearly one third of patients) in schizophrenia (Byerly et al., 2005). Some strategies for dealing with mood oscillation, such as quickly ‘jumping to conclusions’ (which, incidentally, encourages delusion formation) may be an attempt to rapidly establish certainty in order to ward off the chaos and ambiguity that results from supersensitive synapses.
9.7. Movement disorder
Adventitious movements such as exaggerated or purposeless arm and leg motions, tics, grimacing, repetitive activity, and altered reflexes occur in patients with schizophrenia even when they are not taking antipsychotic drugs. They are probably a direct result of hyper-transmission at dopamine synapses (Van Rossum, 1967) whereas, after drugs, they reflect dopamine/cholinergic imbalance (Campos et al., 2010; Pappa and Dazzan, 2009; Peluso et al., 2012). Psychomotor slowing and catatonia are further examples of movement problems associated with schizophrenia and can be viewed as compensations.
10. Psychotogens
Another way of attempting to control chaos is through the use of mind-altering substances. Supersensitivity at the dopamine receptor enhances the reward from nicotine and alcohol, and possibly to marijuana and its congeners (see also Seeman, 2011), further reinforcing the abuse of these compounds. A high proportion of patients with schizophrenia also develop substance use disorder with common street drugs (Volkow, 2009).
A possible biochemical progression from brain injury or gene mutation to the psychotic state is summarized in Fig. 1. The original brain anomaly leads to elevated numbers of D2, D2High, D2D2 dimers, and D1D2 dimers. In addition, there is abnormal pruning and the heightened release of endogenous dopamine. These factors combine to induce abnormal sensations and behaviors. The patient attempts to compensate as best he or she can, and this results in the various manifestations of schizophrenia.
11. Clinical treatment implications
Adolf Meyer did not believe that schizophrenia was something that a person “had” or “was born with” but, rather, that it was a pattern of symptoms and behaviors that evolved from multiple original causes and to which the person tried to adapt, sometimes successfully, sometimes not (Meyer, 1922).
Like Meyer, it is here suggested that patterns of clinical expression in schizophrenia evolve in recurrent cycles of event, reaction and counter-reaction. As such they are relatively unique to every individual and unpredictable in terms of course. There is no finality to a diagnosis of schizophrenia. As Meyer wrote: “… it is also important to lay stress upon traits of personality, cultural influences, environmental stressors, evasive and regressive modes of adaptation” (Double, 2007).
It is further here suggested that dopaminergic overdrive is a necessary step on the path between initial causation and symptom expression. As such, therapeutic interventions need to focus on preventing dopamine overstimulation through a combination of means: biological (dampening dopamine release and transmission), psychological (muting stress that is mediated through dopamine pathways), and sociological (alleviating poverty and discrimination, which raise dopamine activity in large swaths of the population).
Acknowledgments
Funding
This work was supported by the Dr. Karolina Jus estate, the Medland family, Pamela and Desmond O’Rorke, Janet Marsh Frosst, David Medland, Judith Rockert, and Constance E. Lieber and Stephen Lieber.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- Brébion G, David AS, Bressan RA, Ohlsen RI, Pilowsky LS. Hallucinations and two types of free-recall intrusion in schizophrenia. Psychol Med. 2009;39:917–26. doi: 10.1017/S0033291708004819. [DOI] [PubMed] [Google Scholar]
- Buchsbaum MS, Christian BT, Lehrer DS, Narayanan TK, Shi B, Mantil J, et al. D2/D3 dopamine receptor binding with [F-18]fallypride in thalamus and cortex of patients with schizophrenia. Schizophr Res. 2006;85:232–44. doi: 10.1016/j.schres.2006.03.042. [DOI] [PubMed] [Google Scholar]
- Byerly M, Goodman W, Acholonu W, Bugno R, Rush AJ. Obsessive compulsive symptoms in schizophrenia: frequency and clinical features. Schizophr Res. 2005;76:309–16. doi: 10.1016/j.schres.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Campos MS, Garcia-Jalon E, Gilleen JK, David AS, Peralta VM, Cuesta MJ. Motor behavior abnormalities in drug naive patients with schizophrenia spectrum disorders. Mov Disord. 2010;25:1068–76. doi: 10.1002/mds.23050. [DOI] [PubMed] [Google Scholar]
- Charuchinda C, Supavilai P, Karobath M, Palacios JM. Dopamine D2 receptors in the rat brain: autoradiographic visualization using a high-affinity selective agonist ligand. J Neurosci. 1987;7:1352–60. doi: 10.1523/JNEUROSCI.07-05-01352.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chouinard G. Severe cases of neuroleptic-induced supersensitivity psychosis: diagnostic criteria for the disorder and its treatment. Schizophr Res. 1990;5:21–33. doi: 10.1016/0920-9964(91)90050-2. [DOI] [PubMed] [Google Scholar]
- Chouinard G, Chouinard VA. Atypical antipsychotics: CATIE study, drug-induced movement disorder and resulting iatrogenic psychiatric-like symptoms, supersensitivity rebound psychosis and withdrawal discontinuation syndromes. Psychother Psychosom. 2008;77:69–77. doi: 10.1159/000112883. [DOI] [PubMed] [Google Scholar]
- Chouinard G, Jones BD. Schizophrenia as dopamine-deficiency disease. Lancet II. 1978:99–100. doi: 10.1016/s0140-6736(78)91409-5. [DOI] [PubMed] [Google Scholar]
- Chouvardas J. The symbolic and literal in schizophrenic language. Perspect Psychiatr Care. 1996;32:20–2. doi: 10.1111/j.1744-6163.1996.tb00502.x. [DOI] [PubMed] [Google Scholar]
- Corin E, Lauzon G. Positive withdrawal and the quest for meaning: the reconstruction of experience among schizophrenics. Psychiatry. 1992;55:266–78. doi: 10.1080/00332747.1992.11024600. [DOI] [PubMed] [Google Scholar]
- Corripio I, Escartí MJ, Portella MJ, Pérez V, Grasa E, Sauras RB, et al. Density of striatal D2 receptors in untreated first-episode psychosis: an I(123)-IBZM SPECT study. Eur Neuropsychopharmacol. 2011;21:861–6. doi: 10.1016/j.euroneuro.2011.03.004. [DOI] [PubMed] [Google Scholar]
- Delay J, Deniker P, Harl J-M. Traitement des états d’excitation et d’agitation par une méthode médicamenteuse dérivée de l’hibernithérapie (Therapeutic method derived from hiberno-therapy in excitation and agitation states) Ann Med Psychol (Paris) 1952;110:267–73. [PubMed] [Google Scholar]
- Double DB. Adolf Meyer’s psychobiology and the challenge for biomedicine. Philos Psychiatr Psychol. 2007;14:331–9. [Google Scholar]
- Elvevåg B, Wisniewski E, Storms G. Conceptual combination and language in schizophrenia. Schizophr Res. 2010;120:238–9. doi: 10.1016/j.schres.2010.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farde L, Wiesel FA, Stone-Elander S, Halldin C, Nordström AL, Hall H, et al. D2 dopamine receptors in neuroleptic-naive schizophrenic patients. A positron emission tomography study with [11C]raclopride. Arch Gen Psychiatry. 1990;47:213–9. doi: 10.1001/archpsyc.1990.01810150013003. [DOI] [PubMed] [Google Scholar]
- Garrett M, Silva R. Auditory hallucinations, source monitoring, and the belief that “voices” are real. Schizophr Bull. 2003;29:445–57. doi: 10.1093/oxfordjournals.schbul.a007018. [DOI] [PubMed] [Google Scholar]
- Giannini AJ, Nageotte C, Loiselle RH, Malone DA, Price WA. Comparison of chlorpromazine, haloperidol and pimozide in the treatment of phencyclidine psychosis: DA-2 receptor specificity. J Toxicol Clin Toxicol. 1984–1985;22:573–9. doi: 10.3109/15563658408992586. [DOI] [PubMed] [Google Scholar]
- Giannini AJ, Underwood NA, Condon M. Acute ketamine intoxication treated by haloperidol: a preliminary study. Am J Ther. 2000;7:389–91. doi: 10.1097/00045391-200007060-00008. [DOI] [PubMed] [Google Scholar]
- Graff-Guerrero A, Mizrahi R, Agid O, Marcon H, Barsoum P, Rusjan P, et al. The dopamine D2 receptors in high-affinity state and D3 receptors in schizophrenia: a clinical [11C]-(+)-PHNO PET study. Neuropsychopharmacology. 2009;34:1078–86. doi: 10.1038/npp.2008.199. [DOI] [PubMed] [Google Scholar]
- Hall H, Halldin C, Nyberg S, Farde L, Sedvall G. Effect of clozapine and risperidone on 5-HT2 and D2-dopamine receptor binding in the post-mortem human brain. An autoradiographic study. Eur Neuropsychopharmacol. 1995;5:19–25. doi: 10.1016/0924-977x(94)00127-w. [DOI] [PubMed] [Google Scholar]
- Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: version III — the final common pathway. Schizophr Bull. 2009;35:549–56. doi: 10.1093/schbul/sbp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howes OD, Kambeitz J, Kim E, Stahl D, Slifstein M, Abi-Dargham A, et al. The nature of dopamine dysfunction in schizophrenia and what this means for treatment. Arch Gen Psychiatry. 2012;69(8):776–86. doi: 10.1001/archgenpsychiatry.2012.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyo M, Tadokoro S, Kanahara N, Hashimoto T, Niitsu T, Watanabe H, et al. Optimal extent of dopamine D2 receptor occupancy by antipsychotics for treatment of dopamine supersensitivity psychosis and late-onset psychosis. J Clin Psychopharmacol. 2013;33:398–404. doi: 10.1097/JCP.0b013e31828ea95c. [DOI] [PubMed] [Google Scholar]
- Kapur S, Arenovich T, Agid O, Zipursky R, Lindborg S, Jones B. Evidence for onset of antipsychotic effects within the first 24 hours of treatment. Am J Psychiatry. 2005;162:939–46. doi: 10.1176/appi.ajp.162.5.939. [DOI] [PubMed] [Google Scholar]
- Kegeles LS, Slifstein M, Xu X, Urban N, Thompson JL, Moadel T, et al. Striatal and extrastriatal dopamine D2/D3 receptors in schizophrenia evaluated with [18F] fallypride positron emission tomography. Biol Psychiatry. 2010;68:634–41. doi: 10.1016/j.biopsych.2010.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellendonk C, Simpson EH, Polan HJ, Malleret G, Vronskaya S, Winiger V, et al. Transient and selective overexpression of dopamine D2 receptors in the striatum causes persistent abnormalities in prefrontal cortex functioning. Neuron. 2006;49:603–15. doi: 10.1016/j.neuron.2006.01.023. [DOI] [PubMed] [Google Scholar]
- Kimura H, Kanahara N, Watanabe H, Iyo M. Potential treatment strategy of risperidone in long-acting injectable form for schizophrenia with dopamine supersensitivity psychosis. Schizophr Res. 2013;145:130–1. doi: 10.1016/j.schres.2013.01.008. [DOI] [PubMed] [Google Scholar]
- Kinon BJ, Zhang L, Millen BA, Osuntokun OO, Williams JE, Kollack-Walker S, et al. A multicenter, inpatient, phase 2, double-blind, placebo-controlled dose-ranging study of LY2140023 monohydrate in patients with DSM-IV schizophrenia. J Clin Psychopharmacol. 2011;31:349–55. doi: 10.1097/JCP.0b013e318218dcd5. [DOI] [PubMed] [Google Scholar]
- Laruelle M, Abi-Dargham A, Gil R, Kegeles L, Innis R. Increased dopamine transmission in schizophrenia: relationship to illness phases. Biol Psychiatry. 1999;46:56–72. doi: 10.1016/s0006-3223(99)00067-0. [DOI] [PubMed] [Google Scholar]
- Lieberman JA, Kane JM, Alvir J. Provocative tests with psychostimulant drugs in schizophrenia. Psychopharmacology (Berl) 1987;91:415–33. doi: 10.1007/BF00216006. [DOI] [PubMed] [Google Scholar]
- Madras BK. History of the discovery of the antipsychotic dopamine D2 receptor: a basis for the dopamine hypothesis of schizophrenia. J Hist Neurosci. 2013;22(1):62–78. doi: 10.1080/0964704X.2012.678199. [DOI] [PubMed] [Google Scholar]
- Maor-Nof M, Yaron A. Neurite pruning and neuronal cell death: spatial regulation of shared destruction programs. Curr Opin Neurobiol. 2013 doi: 10.1016/j.conb.2013.06.007. http://dx.doi.org/10.1016/j.conb.2013.06.007Epub ahead of print. [DOI] [PubMed]
- Meyer A. Constructive formulation of schizophrenia. Am J Psychiatry. 1922;78(3):355–64. [Google Scholar]
- Miller R, Chouinard G. Loss of striatal cholinergic neurons as a basis of tardive and L-dopa-induced dyskinesias, and neuroleptic-induced supersensitivity psychosis. Biol Psychiatry. 1993;34:713–38. doi: 10.1016/0006-3223(93)90044-e. [DOI] [PubMed] [Google Scholar]
- Nieuwenhuys R, Voogd J, Van Huijzen C. The human central nervous system. 4. Berlin Heidelberg: Springer; 2008. pp. 626–31. [Google Scholar]
- Noll R. American madness: the rise and fall of dementia praecox. Cambridge, MA: Harvard University Press; 2011. [Google Scholar]
- Pappa S, Dazzan P. Spontaneous movement disorders in antipsychotic-naive patients with first-episode psychoses: a systematic review. Psychol Med. 2009;39:1065–76. doi: 10.1017/S0033291708004716. [DOI] [PubMed] [Google Scholar]
- Peluso MJ, Lewis SW, Barnes TR, Jones PB. Extrapyramidal motor side-effects of first- and second-generation antipsychotic drugs. Br J Psychiatry. 2012;200:387–92. doi: 10.1192/bjp.bp.111.101485. [DOI] [PubMed] [Google Scholar]
- Perreault ML, Hasbi A, Alijaniaram M, Fan T, Varghese G, Fletcher PJ, et al. The dopamine D1–D2 receptor heteromer localizes in dynorphin/enkephalin neurons: increased high affinity state following amphetamine and in schizophrenia. J Biol Chem. 2010;285:36625–34. doi: 10.1074/jbc.M110.159954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reith J, Benkelfat C, Sherwin A, Yasuhara Y, Kuwabara H, Andermann F, et al. Elevated dopa decarboxylase activity in living brain of patients with psychosis. Proc Natl Acad Sci. 1994;91:11651–4. doi: 10.1073/pnas.91.24.11651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samaha A-N. Can antipsychotic treatment contribute to drug addiction in schizophrenia? Prog Neuropsychopharmacol Biol Psychiatry. 2013 doi: 10.1016/j.pnpbp.2013.06.008. http://dx.doi.org/10.1016/j.pnpbp.2013.06.008. [pii: S0278-5846(13)00119-X, [Epub ahead of print]] [DOI] [PubMed]
- Seeman P. Schizophrenia model of elevated D2High receptors: haloperidol reverses the amphetamine-induced elevation in dopamine D2High. Schizophr Res. 2009;109(1–3):191–2. doi: 10.1016/j.schres.2008.12.024. [DOI] [PubMed] [Google Scholar]
- Seeman P. All roads to schizophrenia lead to dopamine supersensitivity and elevated dopamine D2High receptors. CNS Neurosci Ther. 2011;17:118–32. doi: 10.1111/j.1755-5949.2010.00162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman P. Comment on “A multicenter, inpatient, phase 2, double-blind, placebo-controlled dose-ranging study of LY2140023 monohydrate in patients with DSM-IV schizophrenia” by Kinon, B.J et al. J Clin Psychopharmacol. 2012a;32:291–2. doi: 10.1097/JCP.0b013e318248daaa. [DOI] [PubMed] [Google Scholar]
- Seeman P. Dopamine agonist radioligand binds to both D2High and D2Low receptors, explaining why alterations in D2High are not detected in human brain scans. Synapse. 2012b;66:88–93. doi: 10.1002/syn.20987. [DOI] [PubMed] [Google Scholar]
- Seeman P. Schizophrenia and dopamine receptors. Eur Neuropsychopharmacol. 2013a;23:999–1009. doi: 10.1016/j.euroneuro.2013.06.005. [DOI] [PubMed] [Google Scholar]
- Seeman P. Are dopamine D2 receptors out of control in psychosis? Prog Neuropsychopharmacol Biol Psychiatry. 2013b;46:146–52. doi: 10.1016/j.pnpbp.2013.07.006. [DOI] [PubMed] [Google Scholar]
- Seeman P. Schizophrenia thalamus imaging: low benzamide binding to dopamine D2 receptors suggests fewer D2Short receptors and less presynaptic terminals. Psychiatry Res: Neuroimaging. 2013c doi: 10.1016/j.pscychresns.2013.09.013. in press. [DOI] [PubMed] [Google Scholar]
- Seeman P, Tinazzi M. Loss of dopamine neuron terminals in antipsychotic-treated schizophrenia; relation to tardive dyskinesia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;44:178–83. doi: 10.1016/j.pnpbp.2013.02.011. [DOI] [PubMed] [Google Scholar]
- Seeman P, Chau-Wong M, Tedesco J, Wong K. Brain receptors for antipsychotic drugs and dopamine: direct binding assays. Proc Natl Acad Sci U S A. 1975;72:4376–80. doi: 10.1073/pnas.72.11.4376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman P, Bzowej NH, Guan HC, Bergeron C, Becker LE, Reynolds GP, et al. Human brain dopamine receptors in children and aging adults. Synapse. 1987a;1(5):399–404. doi: 10.1002/syn.890010503. [DOI] [PubMed] [Google Scholar]
- Seeman P, Bzowej NH, Guan HC, Bergeron C, Reynolds GP, Bird ED, et al. Human brain D1 and D2 dopamine receptors in schizophrenia, Alzheimer’s, Parkinson’s, and Huntington’s diseases. Neuropsychopharmacology. 1987b;1(1):5–15. doi: 10.1016/0893-133x(87)90004-2. [DOI] [PubMed] [Google Scholar]
- Seeman P, Guan H-C, Hirbec H. Dopamine D2High receptors stimulated by phencyclidines, LSD, salvinorin A, and modafinil. Synapse. 2009;63(8):698–704. doi: 10.1002/syn.20647. [DOI] [PubMed] [Google Scholar]
- Silvestri S, Seeman MV, Negrete JC, Houle S, Shammi CM, Remington GJ, et al. Increased dopamine D2 receptor binding after long-term treatment with antipsychotics in humans: a clinical PET study. Psychopharmacology (Berl) 2000;152(2):174–80. doi: 10.1007/s002130000532. [DOI] [PubMed] [Google Scholar]
- Sromek AW, Neumeyer JL, Si Y-G, Zhang T, Seeman P, George SR, et al. Development of high affinity, highly selective agonist ligands for positron emission tomography imaging of the dopamine D2 receptor. 243rd Amer Chem Soc meeting; San Diego, CA. 2011. [Google Scholar]
- Tadokoro S, Okamura N, Sekine Y, Kanahara N, Hashimoto K, Iyo M. Chronic treatment with aripiprazole prevents development of dopamine supersensitivity and potentially supersensitivity psychosis. Schizophr Bull. 2012;38(5):1012–20. doi: 10.1093/schbul/sbr006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talvik M, Nordström AL, Olsson H, Halldin C, Farde L. Decreased thalamic D2/D3 receptor binding in drug-naive patients with schizophrenia: a PET study with [11C]FLB 457. Int J Neuropsychopharmacol. 2003;6:361–70. doi: 10.1017/S1461145703003699. [DOI] [PubMed] [Google Scholar]
- Talvik M, Nordström AL, Okubo Y, Olsson H, Borg J, Halldin C, et al. Dopamine D2 receptor binding in drug-naïve patients with schizophrenia examined with raclopride-C11 and positron emission tomography. Psychiatry Res: Neuroimaging. 2006;148:165–73. doi: 10.1016/j.pscychresns.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Tuppurainen H, Kuikka JT, Laakso MP, Viinamäki H, Husso M, Tiihonen J. Midbrain dopamine D2/3 receptor binding in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2006;256:382–7. doi: 10.1007/s00406-006-0649-3. [DOI] [PubMed] [Google Scholar]
- Van Rossum JM. The significance of dopamine-receptor blockade for the action of neuroleptic drugs. In: Brill H, Cole J, Deniker P, Hippius H, Bradley PB, editors. Neuropsychopharmacology, Proc 5th Collegium Int Neuropsychopharmacologicum. Amsterdam: Excerpta Medica Foundation; 1967. pp. 321–9. [Google Scholar]
- Volkow ND. Substance use disorders in schizophrenia — clinical implications of comorbidity. Schizophr Bull. 2009;35:469–72. doi: 10.1093/schbul/sbp016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M, Pei L, Fletcher PJ, Kapur S, Seeman P, Liu F. Schizophrenia, amphetamine-induced sensitized state and acute amphetamine exposure all show a common alteration: increased dopamine D2 receptor dimerization. Mol Brain. 2010;3:25–34. doi: 10.1186/1756-6606-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasuno F, Suhara T, Okubo Y, Sudo Y, Inoue M, Ichimiya T, et al. Low dopamine d(2) receptor binding in subregions of the thalamus in schizophrenia. Am J Psychiatry. 2004;161:1016–22. doi: 10.1176/appi.ajp.161.6.1016. [DOI] [PubMed] [Google Scholar]
- Yuhas D. Throughout history, defining schizophrenia has remained a challenge (timeline) Sci Am Mind. 2013 Mar; Retrieved March 2, 2013. [Google Scholar]