Abstract
The landmark discovery of induced pluripotent stem cells (iPSCs) by Shinya Yamanaka has transformed regenerative biology. Previously, insights into the pathogenesis of chronic human diseases have been hindered by the inaccessibility of patient samples. However, scientists are now able to convert patient fibroblasts into iPSCs and differentiate them into disease-relevant cell types. This ability opens new avenues for investigating disease pathogenesis and designing novel treatments. In this review, we highlight the uses of human iPSCs to uncover the underlying causes and pathological consequences of diabetes and metabolic syndromes, multi-factorial diseases whose etiologies have been difficult to unravel using traditional methodologies.
Types of Diabetes and Metabolic Syndromes
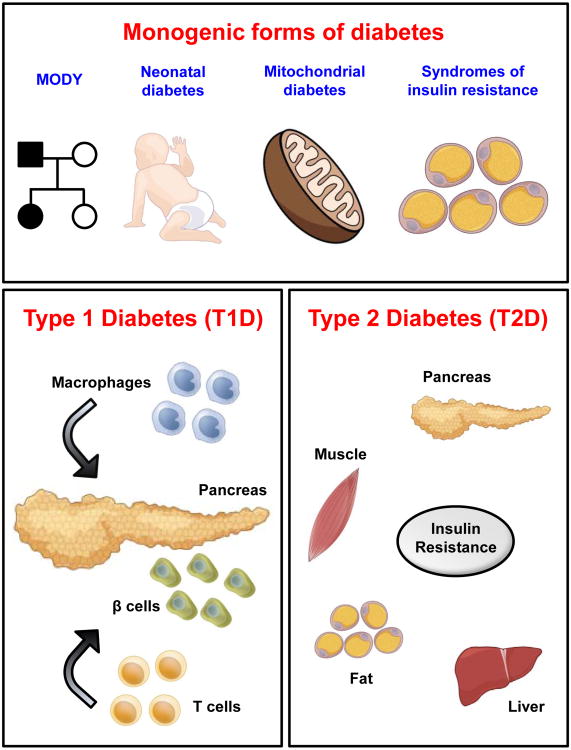
Diabetes is a multi-faceted, multi-factorial disease whereby the body is unable to secrete adequate amounts of biologically active insulin to maintain euglycemia. Clinical diagnosis of diabetes is evident when a patient exhibits persistent hyperglycemia [fasting blood glucose ≥ 7.0 mM or 126 mg/dl, blood glucose level 2 hours after a glucose load [oral glucose tolerance test (OGTT)] ≥ 11.1 mM or 200 mg/dl, or when glycated hemoglobin (HbA1c) is ≥ 6.5 %]. There are various types of diabetes and metabolic syndromes that can be modeled using induced pluripotent stem cells (iPSCs). These can be categorized into monogenic forms [maturity onset diabetes of the young (MODY), neonatal diabetes (Steck and Winter, 2011), mitochondrial diabetes and syndromes of insulin resistance (Doria et al., 2008)], Type 1 diabetes (T1D) and Type 2 diabetes (T2D) (Figure 1). Each of these subtypes is briefly discussed.
Figure 1. Types of diabetes and metabolic syndromes.
The various types of diabetes and metabolic syndromes that can be modeled using induced pluripotent stem cells (iPSCs) include monogenic forms of diabetes, Type 1 diabetes (T1D) and Type 2 diabetes (T2D). T1D occurs as a result of immune attack by immune cells such as macrophages and T cells whereas T2D occurs as a result of insulin resistance in the pancreas, muscle, fat and liver. Square represents male subjects whereas circle represents female subjects. Filled symbols denote subjects with diabetes.
Maturity onset diabetes of the young (MODY)
MODY is characterized by early (<25 years of age) onset of non-ketotic, non-insulin dependent diabetes and commonly presents as mild, asymptomatic hyperglycemia (fasting blood glucose 6-7 mM or 108-126 mg/dl), although some patients have varying degrees of glucose intolerance (OGTT blood glucose 7.8-11 mM or 140-198 mg/dl; seldom > 11.1 mM or 200 mg/dl) that develop into persistent fasting hyperglycemia. MODY exhibits an autosomal dominant mode of inheritance and thus only one copy of the abnormal gene from either parent is required for the inheritance (Fajans et al., 2001). To date, 11 MODYs have been described (Supplementary Table 1) and MODY1-5 are relatively better understood. Although most MODYs result from heterozygous mutations, homozygous mutations have been identified for MODY2 and MODY4 (Njolstad et al., 2001; Stoffers et al., 1997).
MODY1 occurs consequent to a mutation in the hepatocyte nuclear factor 4 alpha gene (HNF4A) (Yamagata et al., 1996a) and patients are characterized by hyperglycemia after an OGTT as compared to MODY2 (Pearson et al., 2001). They develop progressive hyperglycemia and commonly require oral hypoglycemic medications or even insulin (Fajans et al., 2001).
MODY2 is the first MODY to be described (Froguel et al., 1993). Homozygous mutations in the glucokinase gene (GCK) result in permanent neonatal diabetes due to complete GCK deficiency whereas heterozygous mutations result in MODY2 (Osbak et al., 2009). To date, more than 100 mutations have been found in GCK, and all result in a similar phenotype (Miller et al., 1999). Heterozygous GCK mutations often result in mild non-progressive hyperglycemia (fasting blood glucose 6.1-8.1 mM or 110-145 mg/dl) which responds to diet therapy (Pearson et al., 2001). Impaired glucose tolerance in MODY2 patients can be detected even at birth and insulin levels are usually normal. Eventually, less than 50 % of MODY2 patients present overt diabetes and have a lower prevalence of diabetic microvascular complications as compared to other MODYs.
MODY3 (Yamagata et al., 1996b) is the most common MODY, with more than 120 mutations identified to date in the hepatocyte nuclear factor 1 alpha gene (HNF1A) (Fajans et al., 2001). Similar to MODY1, MODY3 patients develop hyperglycemia that deteriorates over time. In some instances, patients may be sensitive to oral hypoglycemics (sulfonylureas) (Sovik et al., 1998). Ultimately, ∼40 % of these patients require insulin (Fajans et al., 2001). MODY3 is relatively serious compared to other MODYs because of a high frequency of diabetic complications (Fajans et al., 2001; Isomaa et al., 1998).
MODY4 (Stoffers et al., 1997) patients who are heterozygous for mutations in the pancreatic homeobox domain gene (PDX1) exhibit a severe impairment of insulin secretion and thus hyperglycemia (fasting blood glucose ∼9.2 mM or 165 mg/dl) (Clocquet et al., 2000). However, diabetes may develop at a later age as compared to other MODY patients. Some patients can be treated with oral sulfonylureas whilst others require insulin.
MODY5 patients manifest mutations in the hepatocyte nuclear factor 1 beta gene (HNF1B) (Horikawa et al., 1997) and commonly exhibit a low birth weight. Dorsal pancreatic agenesis occurs (Haldorsen et al., 2008) and insulin therapy is required. Besides diabetes, MODY5 patients exhibit severe non-diabetic renal dysfunction (Bingham et al., 2001). Given that hypoplastic glomerulocystic kidney disease can be diagnosed before glucose intolerance and diabetes occurs in these patients, it is likely that the kidney disease develops independent of the diabetic state. Renal dysfunction can occur as a result of renal cyst formation (Bingham et al., 2001), impaired creatinine clearance (<80-120 ml/min) (due to compromised glomerular filtration), proteinuria and chronic renal failure (Horikawa et al., 1997).
Several rare types of MODYs including MODY6 (NEUROD1) (Malecki et al., 1999), MODY7 (KLF11) (Neve et al., 2005), MODY8 (CEL) (Raeder et al., 2006), MODY9 (PAX4) (Plengvidhya et al., 2007), MODY10 (INS) (Molven et al., 2008) and MODY11 (BLK) (Borowiec et al., 2009) have been reported and their features are briefly tabulated in Supplementary Table 1.
Neonatal diabetes
Besides MODY, neonatal diabetes is the other main form of monogenic diabetes (Supplementary Table 2) and occurs in the first six months of life (Aguilar-Bryan and Bryan, 2008). It is diagnosed when infants exhibit persistent hyperglycemia (blood glucose > 8.3-11.1 mM or 150-200 mg/dl) due to insufficient insulin production leading to ketoacidosis (an excess of acid in the body). Permanent and transient neonatal diabetes each make up 50 % of the cases.
Permanent neonatal diabetes is more commonly caused by mutations in the ATP-sensitive potassium channel KCNJ11 (KIR6.2) and ABCC8 (SUR1) (Edghill et al., 2010), and insulin gene (INS) (Stoy et al., 2010). Infants with KCNJ11 mutations present clear correlations between genotype and phenotype compared to those with ABCC8 mutations (Edghill et al., 2010). Infants with KCNJ11 and ABCC8 mutations can be treated with oral sulfonylureas (Pearson et al., 2006). Interestingly, some patients with KCNJ11 mutations also develop a neurologic condition called DEND syndrome (developmental delay, epilepsy and neonatal diabetes). Transient neonatal diabetes is primarily caused by mutations/defects in ZAC/HYMAI (6q24) (Mackay and Temple, 2010). Diabetes occurs in the first six weeks of life, resolves by 18 months, may recur and usually requires insulin treatment.
It should be noted that patients with neonatal diabetes may suffer from secondary complications such as diabetic ketoacidosis and hypoglycemia, and over time retinopathy and nephropathy may also develop. Other less common mutations which lead to neonatal diabetes are highlighted in Supplementary Table 2.
Mitochondrial diabetes
Mitochondria DNA (mtDNA) which makes up ∼3-5 % of human cellular DNA encodes tRNAs and several metabolic enzymes. Often, mtDNA accumulate mutations with time, leading to diabetes. The most common mutation linked to diabetes is 3242A>G in the MT-TL1 gene which encodes tRNALeu(UUR) (Maassen et al., 2005). Mitochondrial mutations are maternally inherited and are commonly associated with neurosensory hearing impairment. The syndromes related to diabetes are maternally inherited diabetes and deafness (MIDD) (Maassen et al., 2005) and mitochondrial encephalopathy, lactic acidosis and stroke-like episodes (MELAS) (Sproule and Kaufmann, 2008). MELAS has a broad range of clinical manifestations and requires early treatment with insulin.
Syndromes of insulin resistance
Insulin resistance is a common feature of both obesity and Type 2 diabetes (Petersen and Shulman, 2006). Here, monogenic defects in the insulin signaling pathway, lipoatrophic diabetes and monogenic forms of obesity, all of which lead to insulin resistance, will be discussed (Tsigos et al., 2002).
Monogenic defects in insulin signaling pathway
Insulin can be defective at two levels: a) proinsulin or b) insulin gene. Impaired processing of proinsulin (R65H) results in familial hyperproinsulinemia (Gruppuso et al., 1984). High circulating levels of proinsulin affects glucose homeostasis, resulting in mild to moderate diabetes. Mutations in INS can also cause diabetes (Steiner et al., 1990). Patients present with high circulating levels of insulin due to increased insulin half-life and reduced receptor-mediated insulin clearance. Many INS mutations are heterozygous and there is only a mild impact on glucose homeostasis.
Defects in the insulin receptor can lead to extreme insulin resistance (Taylor, 1992). Syndromes of insulin resistance include Donohue syndrome, Type A syndrome and Rabson-Mendenhall syndrome (Semple et al., 2011). Donohue syndrome is the most severe form of insulin resistance caused either by homozygous mutations or compound heterozygous mutations. Patients with these mutations manifest developmental abnormalities including intrauterine and neonatal growth retardation. A high rate of early death occurs during infancy or in children less than 2 years of age. Type A syndrome of insulin resistance and Rabson-Mendenhall syndrome are usually caused by heterozygous mutations and the patients present with severe insulin resistance, acanthosis nigricans and hyperandrogenization with polycystic ovarian disease. Hyperandrogenism occurs due to hyperinsulinemia and insulin resistance (Semple et al., 2011).
Other monogenic forms of insulin resistance resulting in lipoatrophic diabetes
Besides defects in the insulin signaling pathway, monogenic defects in several other genes also result in insulin resistance (Hegele, 2003). Many of these mutations result in obesity but the severe insulin resistance is not caused by obesity. Mutations in nuclear membrane protein LMNA (lamin A/C) (Shackleton et al., 2000) and peroxisome proliferator activated receptor gamma (PPARγ) cause familial partial lipodystrophy, and mutations in AGPAT2 (1-acylglyerol-3-phosphate O-acyltransferase) and seipin (BSCL2) (Magre et al., 2001) cause congenital generalized lipodystrophy.
Monogenic forms of obesity
Genes involved in genetically determined obesity include leptin (LEP), leptin receptor (LEPR), pro-opiomelanocortin (POMC), prohormone convertase 1 (PC1) and the MC4 receptor (MC4R). Mutations in these genes affect neurological behavior, appetite and satiety control, leading to a predisposition to obesity. Leptin signaling is important for the regulation of energy homeostasis. Patients with congenital leptin deficiency due to ΔG133 frameshift mutation (Montague et al., 1997) respond to leptin therapy. A leptin receptor mutation has also been reported (Clement et al., 1998). Although mutations in LEP or LEPR have been reported, the more common defect in leptin metabolism occurs as a result of leptin resistance, which is still poorly understood.
In the hypothalamus, leptin activates catabolic POMC and switches off anabolic neuropeptide Y/agouti-related protein neurons. A loss-of-function mutation in catabolic POMC which possibly acts as a dietary fat sensor thus results in obesity (Krude et al., 1998). PC1 is also important for energy homeostasis in humans and a heterozygote for PC1 has been reported (Jackson et al., 1997). MC4R is a G-protein-coupled receptor for two peptide derivatives of POMC (α- and β-melanocyte-stimulating hormone (MSH)) that are synthesized in the hypothalamus. Patients with MC4R mutation have increased fat and lean mass. Accordingly, mutations in MC4R are quite common as compared to other human monogenic diseases (Farooqi et al., 2003) and commonly result in haploinsufficiency.
Type 1 diabetes (T1D)
Type 1 diabetes (T1D) accounts for 5-15 % of all diabetes cases, can occur at any age and is common before the age of 40. T1D occurs when pancreatic β cells are destroyed by an autoimmune response in the presence of autoantigens such as insulin, ZnT8, GAD65, IA-2 (Winter and Schatz, 2011), and others, thereby leading to absolute insulin deficiency (van Belle et al., 2011). T1D is a complex disease resulting from both genetic predisposition as well as environmental triggers. The autoimmune attack may be triggered by environmental factors such as diet, which affects the intestinal microbiome (Mathis and Benoist, 2012), and viral infections (Coppieters et al., 2012) in people who are genetically predisposed (Baker and Steck, 2011). Lack of insulin (little or none) in T1D disturbs glucose homeostasis and results in ketoacidosis. The constant exposure to hyperglycemia contributes to complications such as neuropathy, ischemic stroke, retinopathy, diabetic foot ulcer, cardiovascular disease and nephropathy. There is an absolute requirement for daily insulin injections in T1D patients.
Type 2 diabetes (T2D)
Type 2 diabetes (T2D) accounts for 85-95 % of the patients with diabetes. It usually occurs after the age of 40 when the peripheral tissues (skeletal muscle, adipose and liver) are unable to respond to insulin normally, a condition known as insulin resistance. In addition, pancreatic β cells are unable to respond to glucose stimulation and manifest defects in secretion (β cell dysfunction) (Kahn, 1994), leading to a relative insulin deficiency. Insulin resistance (commonly caused by obesity) (Petersen and Shulman, 2006) often occurs before glucose intolerance is detectable (Martin et al., 1992). By the time diabetes is diagnosed, more than 80 % of pancreatic β cells have failed. T2D is a complex disease arising from complicated interactions between genetics (probably multiple genes) and environmental factors (obesity, diet, lack of exercise) (Franks, 2011). It is often associated with obesity and is the most common metabolic disorder. Some genes that have been reported to be involved in T2D include insulin-receptor substrate-1 (IRS-1), glycogen synthase, glucagon receptor, ras-related protein associated with diabetes (RAD), histocompatibility antigens HLA locus-DR4, glycoprotein PC-1 and intestinal fatty acid binding protein (Kahn et al., 1996). Treatments include exercise, dietary changes, oral anti-diabetic medications and insulin injections.
Diabetic Complications
Diabetes is a severe chronic disease that has widespread impact on health. Often, patients with diabetes suffer from numerous co-morbidities collectively termed diabetic complications. Chronic hyperglycemia in these patients results in debilitating neuropathy, ischemic stroke, retinopathy, diabetic foot ulcer, cardiovascular diseases and nephropathy.
Diabetic neuropathy is caused by imbalance in metabolites of glucose and lipids (Vincent et al., 2011). Peripheral sensory neurons are damaged, resulting in abnormal or loss of sensation. Patients with diabetes have twice the risk of developing ischemic stroke and the hyperglycemia possibly affects recanalization after ischemic damage (Luitse et al., 2012). Diabetic retinopathy occurs as a result of microvascular complications in the retina and appears to be partly mediated by vascular endothelial growth factor (VEGF) (Abbate et al., 2011). Laser surgery is commonly required to retard disease progression (Antonetti et al., 2012). Diabetic foot ulcer occurs partly due to damaged nerves. Diabetic neuropathy is correlated with muscle weakness. Eventually, muscle atrophy occurs and the increased skin pressure results in foot ulcers (Andersen, 2012). Macro- and microvascular diabetic complications also impede wound healing that often results in gangrene and amputations, and an economic burden on society.
Cardiovascular disease risk doubles in patients with diabetes and the defects include diabetic cardiomyopathy leading to heart failure (Dhingra and Vasan, 2012) and atherosclerotic coronary artery disease (CAD) which leads to heart attacks (Bornfeldt and Tabas, 2011). Diabetic nephropathy is the most common cause of end-stage renal disease (ESRD). One hypothesis by which diabetes results in nephropathy is the stimulation of tubular growth and supranormal glomerular filtration rate (GFR), leading to injury and nephropathy (Vallon and Thomson, 2012).
Classical Strategies and Challenges for Studying Mechanisms Underlying Human Diabetes
Traditionally, approaches for investigating the molecular mechanisms underlying human diabetes have ranged from the popular use of naturally occurring and genetically engineered rodent models to population-based human genetics studies to small-scale cell explants obtained from diabetic patients. Each of these strategies will be briefly discussed.
Rodent models of diabetes
Diabetic animal models have been widely used to study human diabetes (King, 2012; Kulkarni and Zisman, 2003). This ranges from transgenic mice for MODY to the well studied non-obese diabetic (NOD) mouse for T1D (Driver et al., 2011). Rodent models have also been used to study T2D (Lee and Cox, 2011). An alternative type of rodent model involves experimental induction, including the use of streptozotocin (STZ), alloxan, partial pancreatectomy and diet induced obesity (DIO) (Islam and Loots du, 2009). Different rodent strains have been used in exercise physiology to study effects on obesity and diabetes (Ghosh et al., 2010). Obesity and hyperinsulinemia have also been modeled with animals including the obese Zucker rat, spontaneously hypertensive rat (SHR), the Koletsky rats (obese SHR), the Goto-Kakisaki (GK) rat and the Wistar Ottawa Karlsburg W rats (Aleixandre de Artinano and Miguel Castro, 2009).
In general, the inbred Bio-Breeding Zucker diabetic rat (BBZDR)/Wor rat has been used to study diabetic complications (Tirabassi et al., 2004). Other rodent models have also been developed to study diabetic retinopathy (DR) (Robinson et al., 2012), diabetic cardiomyopathy (Bugger and Abel, 2009) and atherosclerotic coronary artery disease (CAD) (Wu and Huan, 2007). Transgenic animals and the db/db mice have been used to study diabetic nephropathy (DN) (Brosius et al., 2009). The Akita and OVE26 mice which exhibit T1D, BTBR ob/ob mice with T2D, and two mouse models that lack endothelial nitric oxide synthase (eNOS) are among the well studied models which replicate late stages of DN (Alpers and Hudkins, 2011).
Although rodents have been extensively used to study metabolic disease and while considerable advances have been made to understand their pathophysiology, several limitations are evident. For example, the genetic background of mice plays a role in modifying the outcome of a phenotype even when the same mutation is expressed in mice with different genetic backgrounds. Further, rodent models do not fully recapitulate the disease phenotype present in humans. This is exemplified by the lack of a suitable rodent model which can replicate all stages of DN. It is also known that studies from rodents do not always translate to humans. In an attempt to overcome this barrier, humanized mice have been generated to study T1D (King et al., 2008). Non-human primates are also potentially suitable models for diabetes research as they may “replicate” (additional studies required to substantiate this claim) the pathology in humans (Harwood et al., 2012). However, the recent focus on limiting animal usage for research precludes this as a viable alternative.
Human genetics studies
Human genetics studies in the 1990s first involved genome-wide linkage studies. The human genome project in the 20th century then mapped the whole human genome and began the era of genome-wide association studies (GWAS). Analysis of single nucleotide polymorphisms (SNPs) aimed to understand how genetic variations amongst different individuals contribute to susceptibility towards a disease such as diabetes (Collins and Mansoura, 2001). However, to date, it has been difficult to ascribe a single variant that can fully account for the pathophysiology of T2D (Barker et al., 2012). GWAS is currently limited in its ability to identify variants in genes which are strongly associated with diabetes and metabolic disorders. Thus, it is not as straightforward to translate these studies and pinpoint genetic determinants of diabetes (Visscher et al., 2012). More recent high-throughput “–omics” data gave rise to systems biology, which is proving also to be limited for analyses and interpretation due to the complex biological networks that regulate mammalian physiology. In summary, human genetic studies to date have been informative but do not provide a complete understanding of the mechanisms underlying these complex disorders (Doria et al., 2008; Polychronakos and Li, 2011).
Cell explants
One approach to directly study human diabetes has been to isolate primary cells from subjects and study their properties in vitro. Thus, fibroblasts from skin biopsies have been derived from both diabetic and normal patients to determine the mechanisms underlying DN (Millioni et al., 2012). However, it is still uncertain whether physiological changes observed in skin fibroblasts truly mimic those occurring in renal fibroblasts.
Lymphoblasts have also been obtained from diabetic patients with DN (Davies et al., 1995). Recently, primary endothelial cells (ECs) have been obtained from humans to uncover potential defects that may promote various diabetic complications (Onat et al., 2011). Current limitations which preclude widespread use of human cell explants for diabetes research include the lack of donor availability, limited lifespan of primary cells in in vitro cultures, and the limited number of accessible and relevant cell types for study.
iPSCS Represent a New Model for Studying Human Diabetes
Induced pluripotent stem cells (iPSCs), generated by transcription factor-dependent nuclear reprogramming of differentiated somatic cells, are pluripotent stem cell lines that can be propagated indefinitely in culture and maintain the potential to differentiate into any cell type in the body. As iPSCs retain the same genetic make-up as the somatic cell targeted for reprogramming, these cells hold tremendous promise for uncovering novel genetic and biochemical factors that underlie diseases with complex and poorly understood genetic influences, such as diabetes. In addition, human iPSCs (hiPSCs) may one day provide a source of patient-specific “replacement” cells for β cells lost to diabetes, although realizing this possibility will also require effective strategies to block the underlying autoimmunity (in T1D) or insulin resistance (in T2D).
Strategies for producing iPSCs for experimental use
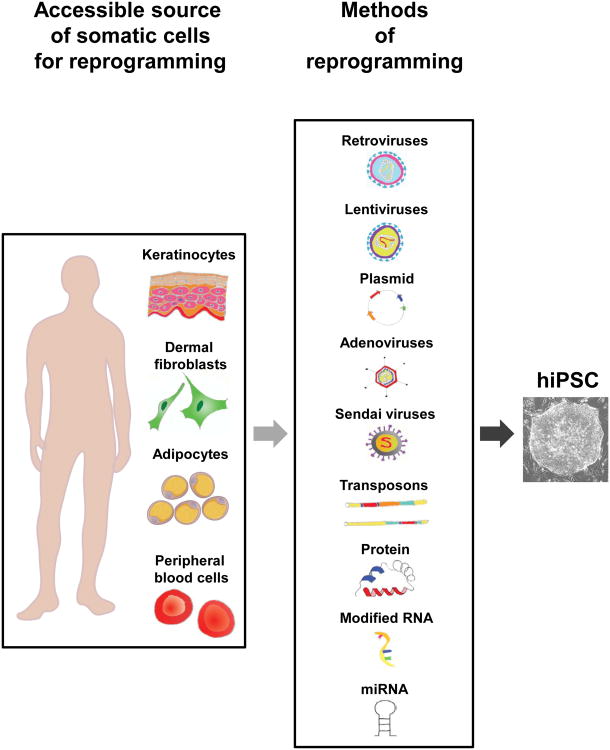
Tremendous progress has been made in generating iPSCs. Remarkably, delivery of genes encoding only three or four transcriptions factors, including Oct3/4, Sox2, Klf4, c-Myc, Lin28 and/or Nanog, or even a single microRNA cluster (miR302/367), is sufficient to reprogram mouse and human fibroblasts, as well as other adult somatic cells, into pluripotent cells (Takahashi and Yamanaka, 2006; Yu et al., 2007). These reprogrammed cells appear to be functionally equivalent to embryonic stem cells (ESCs) although a minority of iPSC lines may have distinct immunological properties (Zhao et al., 2011). Currently the greatest success in reprogramming is observed with the delivery of cDNAs contained within retroviral or lentiviral vectors into somatic cells. In some cases, these viral vectors have been modified to include flanking loxP elements, enabling transgene excision via transient delivery of Cre recombinase (Chang et al., 2009), and limiting the impact of integrational mutagenesis. An important goal for the long-term application of iPSCs in research and therapy is the ability to produce these cells without genotoxic events. Advances toward this goal have been made through the demonstration that target cells can be reprogrammed by transient transfection, non-integrating adenoviral or Sendai virus vectors, transposons, purified proteins, modified RNAs and miRNAs (see (Gonzalez et al., 2011) for references) (Figure 2); however, as yet, the low efficiency and high cost of many non-integrating methods have made their use in iPSC generation infrequent (Bellin et al., 2012). Although hiPSCs were first derived from skin fibroblasts, a cell type that is still commonly used, iPSCs also can be derived from keratinocytes, melanocytes, neural stem cells, mature B cells, renal tubular cells, adipose stem cells, liver and stomach cells, blood cells, as well as pancreatic β cells (see (Gonzalez et al., 2011; Robinton and Daley, 2012) for references) (Figure 2). Interestingly, some studies suggest that the cell type chosen for reprogramming may influence subsequent iPSC differentiation potential. Particularly at early passages, blood cell-derived iPSCs seem predisposed for differentiation along the hematopoietic lineage (Polo et al., 2010); while β cell-derived iPSCs show a predilection for producting β-like cells (Bar-Nur et al., 2011). Yet, this apparent “epigenetic memory” appears to be lost during extended in vitro passage (Polo et al., 2010) and has not been observed for all reprogrammed cell types (Tan et al., 2011).
Figure 2. Schematic of derivation of hiPSCs from patient somatic cells.
Types of human somatic cells which are relatively more accessible for reprogramming include keratinocytes, dermal fibroblasts, adipocytes and peripheral blood cells. Current reprogramming methods include the use of retroviruses, lentiviruses, plasmids, adenoviruses, Sendai viruses, transposons, protein, modified RNA and miRNA.
Production and uses of hiPSCs from diabetic patients
The generation of hiPSCs from humans with defined genetic susceptibilities and well-documented medical histories presents exciting new opportunities for understanding the complex processes that underlie disease initiation and pathology. A great diversity of human disorders have now been modeled using iPSCs, including amyotrophic lateral sclerosis (ALS), spinal muscular atrophy (SMA), familial dysautonomia (FD)/Riley-Day syndrome, Rett syndrome, schizophrenia, Parkinson 's disease, Hutchinson-Gilford progeria syndrome (HGPS), dyskeratosis congenita, Fanconi anaemia, LEOPARD syndrome, long QT syndrome, Timothy syndrome, alpha1-antitrypsin deficiency, familial hypercholesterolemia and glycogen storage disease type 1A (Bellin et al., 2012; Robinton and Daley, 2012).
hiPSCs have also been generated from patients with diabetes (Hua et al., 2013; Kudva et al., 2012; Maehr et al., 2009; Ohmine et al., 2012; Park et al., 2008; Teo et al., 2013; Thatava et al., 2012), although the small number of lines currently available does not represent the broad spectrum of phenotypes and genotypes seen in the clinic. Successful generation of diabetic iPSCs (DiPSCs) obviates one widely-held concern regarding the use of this technology for generating patient-specific cells and studying diabetes pathogenesis – that underlying genetic abnormalities or effects of systemic dysregulation of glucose homeostasis in diabetic patients might preclude effective reprogramming of their cells to generate fully competent iPSCs. Indeed, while the reprogramming efficiency of cells from diabetic patients may not be identical to that of healthy individuals, studies in several labs clearly establish the feasibility of deriving hiPSCs from these individuals. Nonetheless, there remains the real concern that the process of reprogramming which fundamentally alters the global epigenetic profile of the reprogrammed cells (Polo et al., 2010), may “erase” some key disease-contributing changes in gene regulation and expression. Loss of such disease-specific alterations, which may accumulate over many years in vivo, could complicate efforts to accurately model diabetes pathogenesis ex vivo using the reprogrammed cells.
DiPSCs have also been considered as a new and arguably inexhaustible source of “replacement cells” for transplantation approaches to restore β cell mass and reverse insulin dependency in diabetes. One advantage of this approach is the potential in certain situations to utilize autologous cells (derived from the same patient into whom they are ultimately re-implanted). However, if β cell dysfunction arises in whole or in part from cell intrinsic alterations, then correction of the disease-causing mutations will be necessary prior to differentiation and re-introduction into patients of iPSC-derived β cells. In these cases, allogeneic (non-self) cells may have some advantages, particularly in settings where the full spectrum of disease-contributing mutations are unknown and probably numerous (e.g., T2D); however, the use of allogeneic cells raises another challenge in that immunological tolerance to the transplanted cells must be achieved, traditionally through the use of immunosuppressive agents and/or encapsulation devices, which have their own respective limitations. Establishing immune tolerance will be particularly critical for using iPSC-derived cells to replace β cells lost to T1D, as the disease-instigating autoimmunity that remains in these patients will likely mediate prompt rejection of transplanted autologous cells. Thus, for T1D patients, transplantation-based approaches utilizing iPSC cell products may require replacement of both the diseased hematoimmune system [through production of engraftable hematopoietic stem cells (HSCs) from iPSCs] and the generation of glucose-responsive mature β cells (discussed further below).
Given the significant (though certainly not insurmountable) hurdles facing transplantation-based applications of iPSCs for the treatment of diabetes, it may be argued that the greatest near-term utility of these cells will be in their use as screening tools for identifying new genes and pathways that contribute to diabetes pathogenesis in humans and novel drugs that target these pathways. In this regard, patient-specific hiPSCs carrying mutations previously implicated through genome wide association studies (GWAS) in diabetes pathogenesis (see (McCarthy, 2010) for review), may be “corrected” [e.g., using sequence-specific zinc finger nuclease (ZFN), transcription activator-like effector nuclease (TALEN) or clustered regularly interspaced short palindromic repeat (CRISPR) technology] by introduction of “wild-type” sequence at the locus in question in order to evaluate the subsequent impact on cellular activities. Conversely, disease-associated polymorphisms can be introduced into the genomes of iPSCs from healthy donors (Ding et al., 2013a; Ding et al., 2013b). These approaches provide a much-needed functional test for the involvement of candidate diabetes loci in the disease (Merkle and Eggan, 2013), and an important alternative to mouse models, which can produce results that are not perfectly translatable to the human system (Odom et al., 2007; Tiscornia et al., 2011). However, such approaches will depend on the production of disease-relevant differentiated target cells in vitro – an ongoing challenge discussed further below.
In the long-term, in vitro studies using large panels of hiPSC-derived target cells may provide an early stage assessment of the toxicity and efficacy of new candidate pharmaceuticals, and allow correlation with human genetic diversity to specifically inform the design of subsequent clinical trials and ensure testing on the most relevant human populations. Indeed, published studies using iPSCs from SMA and FD patients have employed cell-level readouts (e.g. nullification of mRNA splicing errors) to identify compounds that reverse disease-associated phenotypes (Ebert et al., 2009; Lee et al., 2009). Similarly, a recent study testing the impact of small molecules on patient-derived motor neurons, differentiated in vitro from ALS-hiPSCs, actually predicted the failure of two compounds that indeed proved ineffective in recent ALS clinical trials (Yang et al., 2013).
In addition to neurological diseases, hiPSCs from patients with cardiovascular disease have also been used for drug screening. Cardiomyocytes from Type 1 long QT syndrome-hiPSCs could be treated with β-adrenergic receptor blockers (Moretti et al., 2010), and iPSC-derived cardiomyocytes have also been tested for compounds that might exacerbate disease (Kannankeril et al., 2010). Similar analysis of cardiomyocytes derived from Type 2 long QT syndrome-hiPSCs have identified classes of molecules either aggravate or ameliorate disease phenotype (Itzhaki et al., 2011).
Thus, cells derived from patient-specific hiPSCs have identified drugs that are beneficial, as well as those that may be ineffective or even detrimental, providing a novel means for predicting drug efficacy and toxicity against particular cell types in a disease-specific manner. The use of similar approaches with DiPSCs may discover new drugs for intervention in diabetes and its complications.
Human Induced Pluripotent Stem Cells as a Tool to Model Diabetes In Vitro
Conventional models for studying diabetes frequently involved the use of inbred rodents. Since humans are genetically diverse, this could partly account for some clinical trial failures when translating rodent findings to humans. Indeed, use of human cells where available, is probably the most fitting model for studying human diseases. Therefore, DiPSCs serve as a valuable resource for studying diabetes mechanisms. Cells derived from DiPSCs can be used to understand the developmental events that have gone awry during pancreatic organogenesis, or development of diabetic complications or insulin resistance. As discussed above, since diabetes is a complex disease resulting from alterations in both genes and environment, modeling diabetes using hiPSCs can be most easily achieved in monogenic forms of diabetes followed by efforts aimed at understanding T1D and T2D. Among the monogenic forms of diabetes, hiPSCs have only been reported for MODY and mitochondrial diabetes (Fujikura et al., 2012; Hua et al., 2013; Teo et al., 2013). hiPSCs from T1D patients (Kudva et al., 2012; Maehr et al., 2009; Park et al., 2008; Thatava et al., 2012) and T2D patients (Kudva et al., 2012; Ohmine et al., 2012) have also been generated.
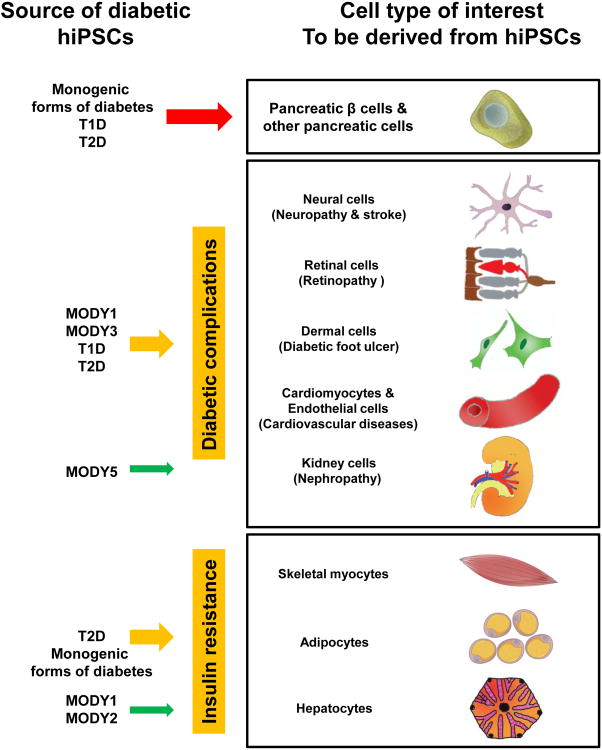
Differentiation into diabetes-relevant cells types (neural, retinal, and dermal cells, cardiomyocytes, endothelial cells, kidney cells, skeletal myocytes, adipocytes and hepatocytes) is essential to fully harness the potential of DiPSCs for understanding the pathogenesis of the various types of diabetes and their complications. hiPSCs derived from MODY patients and infants with neonatal diabetes can be used to understand the importance of causal genes in human pancreas development and islet/β cell function. hiPSCs derived from patients with mitochondrial diabetes can be differentiated into β cells to understand the mitochondrial defect that leads to diabetes. Similarly, hiPSCs derived from patients with monogenic defects in the insulin gene can be differentiated into β cells to understand the impact of the specific mutation. hiPSCs from patients with insulin receptor defects and monogenic forms of insulin resistance can be differentiated into β cells, myocytes, adipocytes or hepatocytes to understand the pathogenesis of insulin resistance whereas hiPSCs from patients suffering from monogenic forms of obesity can be differentiated into adipocytes to study obesity and the initiation of insulin resistance. T1 D-hiPSCs can be used to model the immune attack on β cells or islet progenitors in vitro whilst T2D-hiPSCs can be used to study mechanisms underlying insulin resistance. Efficient and reproducible differentiation protocols are urgently required in order to carry out the afore-mentioned in vitro disease modeling approaches. To date, most protocols have been developed by mimicking developmental events: modifying the dose and timing of activators, repressors and growth factors (Murry and Keller, 2008). Many of these protocols have been initially designed for human embryonic stem cells (hESCs) and subsequently applied to hiPSCs, collectively known as human pluripotent stem cells (hPSCs). These will be highlighted and further elaborated in the following sections focusing on the differentiation of DiPSCs into pancreatic cells as well as cell types involved in diabetic complications and insulin resistance.
Differentiating hiPSCS from Diabetic Patients Into Pancreatic Cells to Study The “Disease Phenotype” In Vitro
There have been numerous attempts to derive pancreatic cells from hPSCs to treat diabetes and, as a corollary, to study human pancreas development in vitro (see Supplementary Table 3 for references). These efforts have frequently been based on a stepwise differentiation of hPSCs towards definitive endoderm, primitive gut tube, foregut, ventral and dorsal pancreatic endoderm, pancreatic progenitors and ultimately to insulin producing β-like cells. Indeed, the ability of islet transplantation via the Edmonton protocol to render diabetic patients insulin-independent (Shapiro, 2011) suggests a potential for hPSC-derived pancreatic β-like cells to treat T1D (see Supplementary Table 3 for reviews).
ViaCyte was among the first to demonstrate the ability of hESC-derived pancreatic progenitors to mature in vivo after ∼5 months, into glucose-responsive insulin-secreting β-like cells (Kroon et al., 2008). Further, they recently succeeded in scaling their protocol towards a typical manufacturing process. This manufacturing scale could eventually make the derivation of these cells feasible for clinical use (Schulz et al., 2012). Alternatively, in order to produce large quantities of differentiated β-like cells, endodermal progenitor cells can be established from hPSCs (Cheng et al., 2012). Nonetheless, all protocols established to date are only able to produce immature “β-like” cells at best. That said, although the generation of mature and fully functional hPSC-derived β cells in vitro is far from reality, the significant progress made by these approaches can be effectively translated to DiPSCs in order to better understand diabetes disease mechanisms which are still poorly understood. In addition to β cells, hPSC-derived α cells are also significant in the context of diabetes given its importance in regulating glucose homeostasis (Rezania et al., 2011), as well as the emerging evidence that α cells can transdifferentiate into β cells (see Supplementary Table 3 for references). Notwithstanding, both cell types can be derived to investigate how their direct interaction regulates insulin versus glucagon secretion. In the following section, we will briefly discuss the relevance of DiPSC-derived pancreatic cells for each type of diabetes.
Monogenic forms of diabetes
HNF4A (MODY1) mutations affect the secretory function of β (Byrne et al., 1995), α and PP cells (Ilag et al., 2000), leading to low basal and stimulated insulin secretion, and severe diabetes which often requires insulin therapy (Fajans et al., 2001). The availability of MODY1-hiPSC-derived β cells provides an opportunity to specifically investigate the role of HNF4A in human pancreas development and β cell function. GCK (MODY2 and neonatal diabetes) controls the rate of glucose entry into the glycolytic pathway (glucose phosphorylation) and the rate of its subsequent metabolism (Matschinsky et al., 1998). The majority of GCK mutations render β cells insensitive to normal extracellular glucose levels (glucose-sensing defect; glucose blindness; decreased glycolytic flux), causing modest hyperglycemia, an increase in blood glucose threshold that triggers insulin secretion (insulin secretion impairment) (Velho et al., 1992) and glucose intolerance, leading to a mild form of diabetes. MODY2-hiPSC-derived pancreatic β cells would be important in unraveling the impact of specific GCK mutations on pancreatic β cell function (Hua et al., 2013). MODY3 (HNF1A) has an extremely similar β cell phenotype to MODY1 likely because HNF4A regulates HNF1A gene expression (Ferrer, 2002). The major function of HNF1A is probably to ensure that the machinery required by β cells to respond to glucose and other stimuli is in place. β cell dysfunction in MODY3 patients is hypothesized to be caused by dominant negative effects (Yamagata et al., 1998) or loss-of-function mechanisms such as reduced DNA binding, impaired transcriptional activation, and defects in subcellular localization (Bjorkhaug et al., 2003). This is still to be determined for each specific mutation. Pdx1 (MODY4 and neonatal diabetes) is an extremely important gene required for embryonic development of pancreatic islets, without which near complete pancreatic agenesis occurs (Jonsson et al., 1994). The impact of various PDX1 mutations on pancreas development and β cell function is yet to be determined. HNF1B (MODY5 and neonatal diabetes) is a member of the complex transcriptional regulatory network that includes HNF1A and HNF4A. HNF1B and HNF1A proteins share a high degree of sequence homology (Mendel et al., 1991), accounting for common pathophysiological mechanisms between β cells of MODY5 and MODY3. Hnf1β−/− mice rescued by tetraploid complementation do not form the ventral bud and exhibit pancreatic agenesis by E13.5 (Haumaitre et al., 2005). Interestingly, some MODY5 patients exhibit dorsal pancreatic agenesis (Haldorsen et al., 2008). Mechanisms underlying HNF1B mutation and diabetes remain to be thoroughly explored.
Neurogenic differentiation 1 (NEUROD1)/beta cell E-box transactivator 2 (BETA2) (MODY6 and neonatal diabetes) is involved in regulating pancreatic endocrine development. NeuroD1−/− mice exhibit abnormal pancreatic islet morphogenesis (reduced number of endocrine cells and no formation of islets) and decreased expression of insulin gene (Naya et al., 1997). The impact of NEUROD1 mutations on human pancreatic function is to be further studied. Little is known about the role of Sp1/KrÜppel-like factor 11 (KLF11) (MODY7) in pancreas development and β cell function except that it regulates PDX1 gene expression (Fernandez-Zapico et al., 2009). Klf11−/− mice are surprisingly normal (Song et al., 2005). Pancreatic cells differentiated from MODY7-hiPSCs will certainly shed light on the mechanism by which KLF11 mutation causes diabetes. Carboxyl ester lipase (CEL) (MODY8) or bile salt-dependent lipase (BSDL) is a major component of pancreatic juice and is responsible for duodenal hydrolysis of cholesterol esters. Cel−/− mice exhibit normal glucose metabolism and do not seem to exhibit MODY8 phenotype (Vesterhus et al., 2010). MODY8 patients exhibit pancreatic exocrine disease before diabetes and the exocrine disturbance is linked to an abnormal structure of the pancreas. How mutations in the quantity of variable number of tandem repeats (VNTR) result in diabetes is yet unclear (Raeder et al., 2006). Thus, differentiation of MODY8-hiPSCs into pancreatic exocrine tissue could shed light on the disease mechanisms. Although there has been relatively less interest in differentiating hPSCs into pancreatic exocrine tissue, an EB differentiation protocol has been recently reported (Shirasawa et al., 2011). Pax4 (MODY9) regulates gene expression patterns in pancreatic endocrine progenitors. Pax4−/− mice exhibit a loss of β (Collombat et al., 2005) and δ cells (Prado et al., 2004). MODY9-hiPSCs serve to explore the impact of mutations affecting the function of PAX4 in pancreatic β cells. Insulin (INS) (MODY10 and neonatal diabetes) is a hormone produced by pancreatic β cells to regulate carbohydrate and fat metabolism, thereby maintaining euglycemia.
Loss of insulin is the main cause of diabetes. MODY10-hiPSCs can be used to study insulin structural defects caused by mutations in the INS gene (Molven et al., 2008). Similarly, hiPSCs derived from infants with neonatal diabetes can be used to study how mutations result in preproinsulin or proinsulin structural abnormalities. B lymphocyte kinase (BLK) (MODY11) is a non-receptor tyrosine-kinase of the src family of proto-oncogenes (Dymecki et al, 1990) expressed in β cells. It is yet unknown why BLK mutations result in diabetes. No metabolic phenotype was reported in Blk−/− mice (Texido et al, 2000) although BLK is involved in upregulating Pdx1 and Nkx6.1 gene expression to enhance insulin synthesis and secretion (Borowiec et al, 2009).
KCNJ11 and ABCC8 (neonatal diabetes) encode for ATP-sensitive inward rectifier potassium channel 11 (Kir6.2) and ATP-binding cassette transporter sub-family C member 8 (SUR1) respectively, components of the β cell KATP channel. In infants with KCNJ11 or ABCC8 mutation, the KATP channels are dysfunctional and cannot close properly. The intracellular ATP is unable to close the KATP channel due to reduced ATP sensitivity. The resulting increased KATP current hyperpolarizes the β cell membrane, thereby suppressing Ca2+ entry. As a result, glucose-stimulated insulin secretion (GSIS) cannot occur (Hattersley and Ashcroft, 2005). DiPSCs derived from these infants could be differentiated into β cells to study their electrophysiology and to determine how each mutation affects the conformational change of the KATP channel. The MT-TL1 gene (mitochondrial diabetes) transfers leucine during polypeptide synthesis. It is involved in synthesizing proteins which participate in oxidative phosphorylation reactions and ATP production in the mitochondria. The A3243G mutation leads to impaired insulin secretion in the presence of normal insulin sensitivity as cells are unable to produce sufficient ATP (Maassen et al., 2005). It is still unclear how the mutation specifically impairs pancreatic β cells and causes age-dependent loss of β cell function.
Type 1 diabetes (T1D) and Type 2 diabetes (T2D)
T1 D-hiPSCs can be used for differentiation into pancreatic β cells and various immune cells to determine the specific mechanisms of autoimmune attack. The severity of attack by each type of immune cell, the cytotoxic cytokines secreted by the cells and whether there is synergism between different types of immune cells acting on the pancreatic β cells can be explored. T2D-hiPSC-derived pancreatic β cells would be useful for modeling mechanisms of secretory dysfunction and the effects of insulin resistance. Potential areas of study include stimulus-secretion coupling, mitochondrial function, growth factor (e.g. insulin, IGF-I) signaling and for testing inducers of T2D-pancreatic β cell failure.
Concluding remarks
Modeling monogenic forms of diabetes with the use of DiPSC-derived pancreatic β cells can potentially inform us about human pancreas development. Correction of the mutations with the use of ZFNs, TALENs or CRISPRs will provide ideal isogenic controls for such studies. Similarly, T1D- and T2D-hiPSC-derived pancreatic β cells will provide unprecedented access into mechanisms of β cell failure and diabetes disease progression. Eventually, these hiPSC-derived β cells can also be subjected to treatment with pharmaceutical compounds to identify drugs that can effectively 1) stimulate GSIS in these defective β cells and 2) stimulate β cell proliferation.
Differentiation Of DiPSCS into Non-Pancreatic Lineages (Involved in Complications of Diabetes and Insulin Resistance)
Prolonged hyperglycemia affects many other cell types in the body besides pancreatic β cells. In most instances these human cells are inaccessible for investigation. Therefore, hiPSCs derived from patients with diabetes due to diverse etiologies can be used to study the disease progression in cell types involved in complications (neural, retinal and dermal cells, cardiomyocytes, endothelial cells, and kidney cells including mesangial cells and podocytes) as well as cell types involved in insulin resistance (skeletal myocytes, adipocytes and hepatocytes) (Figure 3).
Figure 3. Differentiation of diabetic hiPSCs into various cell types forin vitrodisease modeling.
Each type/source of diabetic hiPSCs can be differentiated into relevant cell types of interest for investigating disease mechanisms. Cell types of interest include pancreatic cells, cells involved in diabetic complications and cells involved in insulin resistance.
Neural cells for diabetic neuropathy and ischemic stroke
Diabetic neuropathy is a pathophysiological condition which generally affects all peripheral nerves and the autonomic nervous system. This condition is partly attributed to microvascular complications since reduced blood flow results in neuronal ischemia. Mechanisms underlying diabetic neuropathy are poorly understood. Co-culture of endothelial cells (discussed below) with sensory/motor/inter-neurons derived from DiPSCs can potentially be used to study the impact of hyperglycemia on blood vessel cells and neurons in conditions of diabetic neuropathy.
Ischemic stroke is a severe complication in patients with diabetes whose occurrence in the cerebral cortex, cerebellum and brain stem can result in varied symptoms due to the specialized functions of the central nervous system. The area of the brain which is affected probably loses its function. Thrombosis (blood clot obstruction) or arterial embolism results in blood flow blockade, thereby affecting brain function. Thrombosis occurs gradually and thus the onset of ischemic stroke is slow. However, the blockade of an artery by a moving clot (embolus) is sudden, resulting in a severe and immediate onset of ischemic stroke. Occlusion of blood vessels in the brain depletes oxygen and glucose necessary for aerobic metabolism and cell survival. Neuronal death subsequently occurs and neural circuits are disrupted.
Neural cells in the brain include neurons, astrocytes and oligodendrocytes. The majority of the neurons in the brain are either glutamatergic (release glutamate; excitatory in general) or GABAergic (release gamma aminobutyric acid (GABA); inhibitory in general). Other types include cholinergic (release acetylcholine), dopaminergic (release dopamine) and serotonergic (release serotonin). Neural differentiation from hPSCs (Erceg et al., 2009) has advanced considerably due to its relative ease as compared to deriving other cell types of the body. hPSCs can be differentiated into neural precursors readily (see Supplementary Table 3 for references) and even more specifically to neural cells such as motor neurons (Boulting et al., 2011), dopaminergic neurons (Swistowski et al., 2010) and glutamatergic neurons (Zeng et al., 2010). hPSC-derived neural precursors have been reported to engraft in the rodent forebrain and promote recovery after a stroke (Oki et al., 2012). Although neural differentiation is relatively advanced, the differentiation of hPSCs into more specialized neuronal subtypes is still needed in order to study mechanisms underlying diabetic neuropathy in vitro.
Retinal cells for diabetic retinopathy
Retinopathy is a leading cause of blindness and occurs when blood vessels of the retina are damaged, leading to vascular leakage in patients with diabetes. Vascular leakage can lead to macular edema, retina ischemia and neovascularization followed by vitreous hemorrhage and retinal detachment. DiPSCs can be differentiated into retinal cells and endothelial cells (discussed below), and the interactions between these two cell types can be studied in vitro. Besides using DiPSCs primarily for understanding mechanisms underlying diabetic retinopathy, hiPSCs can also potentially be a source of cells for stem cell therapy in retinal diseases (Rowland et al., 2012).
Significant progress has been made in the differentiation of hPSCs into progenitor cells with a retinal cell fate (see Supplementary Table 3 for references), and hPSC-derived retinal cells have been reported to integrate into rodent retina, demonstrating survivability and compatibility (Hambright et al., 2012). Swine-iPSC-derived photoreceptors can integrate into the subretinal space of pigs (Zhou et al., 2011), thereby establishing a larger animal model for cell transplantation. One can now distinguish between the various types of retinal cells derived from hPSCs due to their unique transcriptional profile (Siegert et al., 2012).
Dermal cells for diabetic foot ulcer
Diabetic foot ulcer occurs due to diabetic neuropathy as well as macro/microvascular complications. Peripheral neuropathy (loss of feeling in extremities) and muscle atrophy initially occurs, leading to foot ulcers. The wound healing process is impaired, thereby leading to gangrene and amputation. DiPSCs can be differentiated into neural cells and myocytes (discussed in other sections) to investigate how neuropathy affects skeletal muscle integrity and function. Specific to dermal cells, DiPSCs can be differentiated into keratinocytes and fibroblasts to study the relationship between extracellular matrix (ECM) replacement and prolonged inflammatory process in diabetic wounds.
Dermal cells derived from DiPSCs are valuable for studying ultrastructural components such as endoplasmic reticulum, changes in secreted ECM proteins as well as tissue remodeling enzymes. They also have the potential to be used in skin grafts (Pellegrini and De Luca, 2010). hESCs have been reported to differentiate into keratinocyte precursors and keratinocytes, and into structures resembling the skin (see Supplementary Table 3 for references). Once keratinocytes and fibroblasts are obtained, a three-dimensional human skin reconstruction (Li et al., 2011) could potentially be developed to model diabetic foot ulcer.
Cardiomyocytes for diabetic cardiomyopathy
Cardiovascular complications in patients with diabetes include cardiomyopathy which commonly occurs in the presence of hypertension and atherosclerotic coronary artery disease (CAD). Cardiomyopathy is initiated with some form of left ventricular dysfunction followed by cardiomyocyte hypertrophy and an eventual long QT interval indicative of fibrosis. In the face of constant hyperglycemia, cardiomyocytes develop metabolic abnormalities, denervation due to neuropathy and dysregulated Ca2+, Na+ and K+ ion homeostasis. Usually, the heart obtains up to 70 % of the total required ATP via oxidation of fatty acids. However, this is increased to 100 % (Oliver and Opie, 1994) due to a decrease in glucose metabolism as the cardiomyocytes down regulate insulin-dependent glucose transporter GLUT4 to protect themselves from hyperglycemia. The increased lipid uptake translates to triacylglyceride (TAG) synthesis and these metabolic changes ultimately lead to diabetic cardiomyopathy.
Cardiomyocytes can now be derived from hPSCs with relative ease (see Supplementary Table 3 for reviews). Thus, DiPSCs can be differentiated into cardiomyocytes (see Supplementary Table 3 for references) to study the impact of hyperglycemia on cardiomyocytes themselves. This approach is useful since it is virtually impossible to access human cardiomyocytes to study disease mechanism(s).
Endothelial cells for various diabetic complications
Persistent extracellular hyperglycemia results in endothelial cells (ECs) lining the blood vessels to be exposed to intracellular hyperglycemia as they are unable to regulate glucose uptake in contrast to myocytes or hepatocytes. This leads to endothelial dysfunction and blood vessel damage (angiopathy) (Brownlee, 2005). Complications in patients with diabetes arising from impaired ECs can be categorized into macrovascular (arteries) or microvascular (small blood vessels: arterioles and capillaries) complications. Macrovascular complications implicate ischemic stroke, diabetic foot ulcer and atherosclerotic coronary artery disease (CAD) whereas microvascular complications lead to diabetic neuropathy, retinopathy, cardiomyopathy and nephropathy.
In macroangiopathy, endothelial dysfunction affects blood flow, and possibly capillary occlusion. Thus, all cells which depend on blood vessels for glucose and oxygen potentially suffer from ischemia and eventually die. CAD is a severe cardiovascular disease which occurs as a result of narrowing of the lumen of artery due to plaque accumulation. The restriction of blood flow to the myocardium results in myocardial ischemia and ultimately myocardial infarction (tissue death; heart attack). Hyperglycemia also results in basement membrane thickening and changes in blood vessel permeability. This condition of microangiopathy results in leakage of fluid and protein, edema, and decreased blood flow to tissues and cells. The impact of hyperglycemia on EC function is variable in the various diabetic conditions. Thus, it would be fruitful to differentiate DiPSCs into endothelial cells and cell types which are location and condition-specific to determine the specific dysfunctions in ECs. hPSCs can be differentiated into vascular endothelial cells. See (Supplementary Table 3) for reviews and references to protocols involving the differentiation of ECs from hPSCs.
Kidney cells for diabetic nephropathy
Diabetic nephropathy occurs when blood vessels in the kidney glomeruli suffer from microangiopathy. The glomeruli thicken and leak serum albumin in the urine (microalbuminuria), and this defect progresses to macroalbuminuria and proteinuria. Often, these patients have increased serum creatinine and decreased estimated glomerular filtration rates (eGFR). Untreated diabetic nephropathy may progress towards end-stage renal disease (ESRD) whereby the kidney fails to function. The mechanisms underlying diabetic nephropathy have been difficult to study in humans due to inaccessibility of the renal corpuscle (which filters the blood) during disease progression. The renal corpuscle is made up of the glomerulus and the Bowman 's capsule. Fluid from the blood passes through the endothelial cells of the glomerulus, the mesangial cells (pericytes) around the blood vessels and the podocytes lining the Bowman 's capsule. Thus, the reconstitution of these components in vitro with the use of DiPSC-derived cells may provide insights into the mechanisms underlying disease progression.
Unfortunately, thus far there has been little success in deriving kidney cells from hPSCs. Three reports suggest the feasibility of deriving renal progenitors from hESCs (Batchelder et al., 2009; Lin et al., 2010; Narayanan et al., 2013). To understand the interactions between endothelial cells, mesangial cells and podocytes, these renal progenitors need to be derived in vitro. While mesangial cells are known to communicate with the endothelial cells (Kida and Duffield, 2011), additional efforts are required to derive these cell types in order to model diabetic nephropathy.
Skeletal myocytes for diabetic foot ulcer and insulin resistance
Skeletal myocytes can potentially be derived from DiPSCs to study the progression of diabetic foot ulcer, as well as mechanisms underlying insulin resistance. How diabetic neuropathy and damaged innervation result in muscle weakness and atrophy is not well understood in diabetic foot ulcer. In patients with insulin resistance, skeletal myocytes do not respond appropriately to insulin to absorb glucose and convert it to glycogen. Less glucose is absorbed from the blood and less glycogen is produced.
Skeletal muscle contains a resident stem cell population (satellite cells) that supports regenerative myogenesis, and several groups have attempted to derive these cells as well as differentiated skeletal myoblasts from hPSCs. Skeletal myocytes derived from hPSCs may be useful to study the initiation and development of insulin resistance in vitro. However, the establishment of robust protocols for deriving such cells from hPSCs has proved challenging. One report described skeletal myocyte derivation from human embryonic germ cells (Kim et al., 2005). Most published protocols to date typically rely on enforced expression of myogenic transcription factors or inclusion of an intermediate step in which hPSCs are first differentiated into multipotent mesenchymal stromal cells (MSCs), which must be further cultured to allow differentiation into myocytes (see Supplementary Table 3 for additional references).
Adipocytes for monogenic diabetes and insulin resistance
Various gene mutations affect adipocyte development/function and result in syndromes of insulin resistance. Indeed, insulin resistance in T2D also affects adipocytes. Thus, one new exciting area of research is to differentiate DiPSCs into adipocytes to study mechanisms of development of insulin resistance. Adipocytes normally respond to insulin by taking up glucose and converting it into triacylglycerides (TAGs), and by taking up excess lipids for storage. In states of insulin resistance, dysfunctional adipocytes exhibit reduced lipid uptake and increased hydrolysis to TAGs, increasing circulating free fatty acids (FFA). The inability to store excess lipids in fat leads to lipid accumulation in myocytes and hepatocytes. Adipocyte growth and expansion also results in inflammation. Cytokines are produced, leading to the recruitment of macrophages. Macrophage accumulation leads to further production of cytokines and ultimately the promotion of inflammation in tissues including the islets (insulitis). All these cumulative events may contribute to insulin resistance. Several of these pathways could be investigated at early stages of differentiation of DiPSCs into adipocytes. Primate ESCs, similar to hPSCs, can be differentiated into adipocytes (see Supplementary Table 3 for references). Alternatively, hPSCs can be differentiated into multipotent MSCs and subsequently to preadipocytes via BMP4 (see Supplementary Table 3 for references).
Hepatocytes for monogenic diabetes and insulin resistance
HNF4A (MODY1) plays a critical role in liver development (Hayhurst et al., 2001) besides pancreatic development. MODY1 patients exhibit lower levels of serum protein, TAG concentrations (Shih et al, 2000) and esterified cholesterol (Pramfalk et al, 2009). GCK (MODY2) is also expressed in hepatocytes besides pancreatic β cells (Iynedjian et al, 1989). In fact, most of the GCK in the body is found in hepatocytes. GCK has β cell and hepatocyte-specific promoters which can produce different GCK isoforms (Stoffel et al, 1992). Clearly, the role of GCK in hepatocyte and β cell is different as GCK in the liver generally processes all available glucose whereas it is a glucose sensor in the pancreas.
Hepatocyte-like cells have been derived from hPSCs (see Supplementary Table 3 for references). MODY1-hiPSC-derived hepatocytes can be used to investigate the importance of HNF4A in hepatocyte development and function. Given that GCK is largely expressed in hepatocytes, the differentiation of MODY2-hiPSCs into hepatocytes is a good model to study the effect of GCK mutations on hepatocyte glucose metabolism. In addition, the same GCK mutant protein can be compared in MODY2-hiPSC differentiated pancreatic β cells versus hepatocytes. Mutant GCK results in impaired insulin secretion and abnormal liver glucose metabolism (Velho et al., 1996). It will be important to understand the impact of mutant GCK on pancreatic β cell and hepatocyte function, independent of their physiological cross-talk. The differentiation of T2D-hiPSCs into hepatocytes would allow the creation of a useful in vitro model to study insulin resistance in hepatocytes, independent of whole body physiology.
Using hiPSC Derivatives to Investigate (Metabolic) Signaling Pathways Relevant to Maintenance of Pluripotency and Differentiation
Traditional metabolic signaling pathways such as the insulin/IGF-I signaling pathway are emerging as important in iPSC biology due to their diverse roles in growth, metabolism and relevance throughout the developmental stages of cellular differentiation. The pathways regulated by insulin/IGF-I and their downstream proteins PI3K/Akt and Raf/Mek/Erk (MAPK) signaling will be briefly discussed.
Insulin/IGF-I signaling
Insulin and insulin-like growth factors (IGF-I and IGF-II) are ubiquitous growth factors that modulate growth as well as glucose and lipid metabolism. They bind to insulin receptor (IR) and/or insulin-like growth factor 1 receptor (IGF1R), both receptor tyrosine kinases (RTKs), leading to autophosphorylation of the IR/IGF1R. This initiates a chain of signaling events, including the phosphorylation of insulin receptor substrate (IRS) proteins, recruitment of adaptor molecules and activation of 1) PI3K/Akt/PKB or 2) Raf/Mek/Erk (MAPK) signaling pathways (Taniguchi et al., 2006) (discussed below).
Insulin/IGF-I signaling has been suggested to play important roles in both the maintenance of hPSC pluripotency (Chen et al., 2011) as well as cell metabolism in adult tissues (Rask-Madsen and Kahn, 2012). IGF-I regulates hESC pluripotency (Wang et al., 2007) whereas IGF-II promotes hESC proliferation, expansion and prevention of apoptosis (Bendall et al., 2007). In using DiPSCs to study disease mechanisms, one can also investigate the role of insulin/IGF-I signaling from the pluripotent state of hiPSCs, during directed differentiation, as well as in specific cell types involved in glucose and lipid metabolism. In this respect, how the requirement for insulin/IGF-I signaling in maintaining pluripotency (McLean et al., 2007) tapers and transits towards early differentiation can provide new insights into energy usage. Furthermore, in defined cell types such as myocytes and adipocytes, one can investigate the switch in insulin/IGF-I signaling pathway in the regulation of glucose uptake.
PI3K/Akt signaling pathway
Phosphoinositide 3-kinase (PI3K), a lipid kinase, consists of a p85 regulatory subunit and a p110 catalytic subunit. Activation of PI3K signaling pathway results in phosphorylation of phosphatidylinositol (4,5) bisphosphate (PtdIns(4,5)P2), formation of Ptd(3,4,5)P3 and activation/phosphorylation of serine/threonine kinase Akt/protein kinase B (PKB). Akt then phosphorylates and inhibits glycogen synthase kinase 3 (GSK-3) and induces glycogen synthesis. Activated Akt also participates in cell survival, inhibition of pro-apoptotic signals, cell proliferation, cell growth and protein synthesis (Cantley, 2002).
Insulin signaling via PI3K signaling pathway can increase epiblast cell number (Campbell et al., 2012), suggesting the importance of this pathway in hPSC proliferation. In addition, PI3K signaling is also important for the maintenance of pluripotency of hPSCs as its suppression by LY294002 and/or AKT1-II is required for the transition from pluripotency to differentiation (McLean et al., 2007). A decrease in PI3K/Akt signaling pathway has been reported following hESC differentiation (Armstrong et al., 2006). Given that PI3K/Akt signaling mediates stem cell fate (Welham et al., 2007), the dynamics of PI3K/Akt signaling can be studied upon differentiation of hiPSCs into diverse cell types.
Raf/Mek/Erk (MAPK) signaling pathway
Mitogen-activated protein kinases (MAPKs) are serine/threonine protein kinases and their signaling pathway involves adaptor proteins, guanine nucleotide exchange factors and small GTP binding proteins. These then activate MAPK kinase kinase (MAPKKK)/Raf which phosphorylates MAPK kinase (MAPKK)/MEK1/2, which in turn phosphorylates MAPK/ERK1/2. This signaling cascade is important for cell growth, cell proliferation, cell movement, cell differentiation and cell death (Keshet and Seger, 2010).
Insulin/IGF-I signaling pathway activation activates the MAPK signaling pathway. FGF2, an important component required to maintain pluripotency of hPSCs, activates FGFR2 and also stimulates MAPK signaling (Eiselleova et al., 2009). FGF2 reinforces the pluripotent state, self-renewal and survival, and it has been reported that a high basal level of MAPK signaling pathway maintains pluripotency in hESCs, in contrast to mESCs (Li et al., 2007). Also, upon hESC differentiation, there is a decrease in MAPK signaling pathway (Armstrong et al., 2006). Since both insulin/IGF-I and FGF2 independently activate MAPK signaling in hPSCs, it would be interesting to determine their relative roles in the maintenance of pluripotency. MAPK signaling also regulates developmental cell fate specification (Craig et al., 2008) and stem cell lineage commitment (Binetruy et al., 2007). Given that insulin/IGF-I and FGF2 are also known to play mitogenic roles during differentiation of hiPSCs, this signaling network can be actively studied during the differentiation of DiPSCs into the various cell types.
Future Directions and the Road to Therapy
In conclusion, hiPSCs derived from patients with diabetes or various types of metabolic syndromes can be effectively derived and used to study disease development and pathology in vitro. In this regard, the study of monogenic diabetic or metabolic diseases may be more straightforward to model with hiPSCs compared to complex diseases such as T1D and T2D, as the lengthy evolution and ever-changing genetic-environmental interactions that occur in T1D and T2D are potentially harder to decipher using cell-based systems. Understanding the significance of MODY genes in the differentiation and maturation of pancreatic islet cells may be particularly illuminating for enhancing ex vivo strategies to produce mature, functional β cells. Likewise, small molecule screening using DiPSC-derived cells may identify patient-specific susceptibilities to therapy and advance personalized approaches to diabetes treatment. It must be cautioned, however, that considerable progress is still necessary to achieve accurate specification of fully mature cells from differentiating hiPSCs, and to enable delivery of hiPSC-derived cells to appropriate target organs in vivo. Continued progress on these fronts will be critical in uncovering new mechanisms underlying diabetes pathology and advancing treatment options for diabetes patients.
Supplementary Material
Acknowledgments
The authors would like to thank Julia Li for assistance with the graphics and apologize to all those whose work was not discussed and cited due to space constraints. A.K.K.T. is supported by a Juvenile Diabetes Research Foundation Postdoctoral Fellowship. R.N.K. is supported by National Institute of Health Grants RO1 DK 67536 and RO1 DK 055523, the Harvard Stem Cell Institute, a JDRF/Sanofi Strategic Alliance Grant and a grant from the Astra Zeneca. This work was also supported by a Diabetes Research Center grant (NIH P30DK036836) to the Joslin Diabetes Center.
Footnotes
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abbate M, Cravedi P, Iliev I, Remuzzi G, Ruggenenti P. Prevention and treatment of diabetic retinopathy: evidence from clinical trials and perspectives. Curr Diabetes Rev. 2011;7:190–200. doi: 10.2174/157339911795843168. [DOI] [PubMed] [Google Scholar]
- Aguilar-Bryan L, Bryan J. Neonatal diabetes mellitus. Endocr Rev. 2008;29:265–291. doi: 10.1210/er.2007-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleixandre de Artinano A, Miguel Castro M. Experimental rat models to study the metabolic syndrome. Br J Nutr. 2009;102:1246–1253. doi: 10.1017/S0007114509990729. [DOI] [PubMed] [Google Scholar]
- Alpers CE, Hudkins KL. Mouse models of diabetic nephropathy. Curr Opin Nephrol Hypertens. 2011;20:278–284. doi: 10.1097/MNH.0b013e3283451901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen H. Motor dysfunction in diabetes. Diabetes Metab Res Rev. 2012;28(1):89–92. doi: 10.1002/dmrr.2257. [DOI] [PubMed] [Google Scholar]
- Antonetti DA, Klein R, Gardner TW. Diabetic retinopathy. N Engl J Med. 2012;366:1227–1239. doi: 10.1056/NEJMra1005073. [DOI] [PubMed] [Google Scholar]
- Armstrong L, Hughes O, Yung S, Hyslop L, Stewart R, Wappler I, Peters H, Walter T, Stojkovic P, Evans J, et al. The role of PI3K/AKT, MAPK/ERK and NFkappabeta signalling in the maintenance of human embryonic stem cell pluripotency and viability highlighted by transcriptional profiling and functional analysis. Hum Mol Genet. 2006;15:1894–1913. doi: 10.1093/hmg/ddl112. [DOI] [PubMed] [Google Scholar]
- Baker PR, 2nd, Steck AK. The past, present, and future of genetic associations in type 1 diabetes. Curr Diab Rep. 2011;11:445–453. doi: 10.1007/s11892-011-0212-0. [DOI] [PubMed] [Google Scholar]
- Bar-Nur O, Russ HA, Efrat S, Benvenisty N. Epigenetic memory and preferential lineage-specific differentiation in induced pluripotent stem cells derived from human pancreatic islet beta cells. Cell Stem Cell. 2011;9:17–23. doi: 10.1016/j.stem.2011.06.007. [DOI] [PubMed] [Google Scholar]
- Barker A, Langenberg C, Wareham NJ. Genetic determinants of glucose homeostasis. Best Pract Res Clin Endocrinol Metab. 2012;26:159–170. doi: 10.1016/j.beem.2011.12.002. [DOI] [PubMed] [Google Scholar]
- Batchelder CA, Lee CC, Matsell DG, Yoder MC, Tarantal AF. Renal ontogeny in the rhesus monkey (Macaca mulatta) and directed differentiation of human embryonic stem cells towards kidney precursors. Differentiation. 2009;78:45–56. doi: 10.1016/j.diff.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellin M, Marchetto MC, Gage FH, Mummery CL. Induced pluripotent stem cells: the new patient? Nat Rev Mol Cell Biol. 2012;13:713–726. doi: 10.1038/nrm3448. [DOI] [PubMed] [Google Scholar]
- Bendall SC, Stewart MH, Menendez P, George D, Vijayaragavan K, Werbowetski-Ogilvie T, Ramos-Mejia V, Rouleau A, Yang J, Bosse M, et al. IGF and FGF cooperatively establish the regulatory stem cell niche of pluripotent human cells in vitro. Nature. 2007;448:1015–1021. doi: 10.1038/nature06027. [DOI] [PubMed] [Google Scholar]
- Binetruy B, Heasley L, Bost F, Caron L, Aouadi M. Concise review: regulation of embryonic stem cell lineage commitment by mitogen-activated protein kinases. Stem Cells. 2007;25:1090–1095. doi: 10.1634/stemcells.2006-0612. [DOI] [PubMed] [Google Scholar]
- Bingham C, Bulman MP, Ellard S, Allen LI, Lipkin GW, Hoff WG, Woolf AS, Rizzoni G, Novelli G, Nicholls AJ, et al. Mutations in the hepatocyte nuclear factor-1beta gene are associated with familial hypoplastic glomerulocystic kidney disease. Am J Hum Genet. 2001;68:219–224. doi: 10.1086/316945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorkhaug L, Sagen JV, Thorsby P, Sovik O, Molven A, Njolstad PR. Hepatocyte nuclear factor-1 alpha gene mutations and diabetes in Norway. J Clin Endocrinol Metab. 2003;88:920–931. doi: 10.1210/jc.2002-020945. [DOI] [PubMed] [Google Scholar]
- Bornfeldt KE, Tabas I. Insulin resistance, hyperglycemia, and atherosclerosis. Cell Metab. 2011;14:575–585. doi: 10.1016/j.cmet.2011.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borowiec M, Liew CW, Thompson R, Boonyasrisawat W, Hu J, Mlynarski WM, El Khattabi I, Kim SH, Marselli L, Rich SS, et al. Mutations at the BLK locus linked to maturity onset diabetes of the young and beta-cell dysfunction. Proc Natl Acad Sci U S A. 2009;106:14460–14465. doi: 10.1073/pnas.0906474106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulting GL, Kiskinis E, Croft GF, Amoroso MW, Oakley DH, Wainger BJ, Williams DJ, Kahler DJ, Yamaki M, Davidow L, et al. A functionally characterized test set of human induced pluripotent stem cells. Nat Biotechnol. 2011;29:279–286. doi: 10.1038/nbt.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brosius FC, 3rd, Alpers CE, Bottinger EP, Breyer MD, Coffman TM, Gurley SB, Harris RC, Kakoki M, Kretzler M, Leiter EH, et al. Mouse models of diabetic nephropathy. J Am Soc Nephrol. 2009;20:2503–2512. doi: 10.1681/ASN.2009070721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54:1615–1625. doi: 10.2337/diabetes.54.6.1615. [DOI] [PubMed] [Google Scholar]
- Bugger H, Abel ED. Rodent models of diabetic cardiomyopathy. Dis Model Mech. 2009;2:454–466. doi: 10.1242/dmm.001941. [DOI] [PubMed] [Google Scholar]
- Byrne MM, Sturis J, Fajans SS, Ortiz FJ, Stoltz A, Stoffel M, Smith MJ, Bell GI, Halter JB, Polonsky KS. Altered insulin secretory responses to glucose in subjects with a mutation in the MODY1 gene on chromosome 20. Diabetes. 1995;44:699–704. doi: 10.2337/diab.44.6.699. [DOI] [PubMed] [Google Scholar]
- Campbell JM, Nottle MB, Vassiliev I, Mitchell M, Lane M. Insulin increases epiblast cell number of in vitro cultured mouse embryos via the PI3K/GSK3/p53 pathway. Stem Cells Dev. 2012;21:2430–2441. doi: 10.1089/scd.2011.0598. [DOI] [PubMed] [Google Scholar]
- Cantley LC. The phosphoinositide 3-kinase pathway. Science. 2002;296:1655–1657. doi: 10.1126/science.296.5573.1655. [DOI] [PubMed] [Google Scholar]
- Chang CW, Lai YS, Pawlik KM, Liu K, Sun CW, Li C, Schoeb TR, Townes TM. Polycistronic lentiviral vector for “hit and run” reprogramming of adult skin fibroblasts to induced pluripotent stem cells. Stem Cells. 2009;27:1042–1049. doi: 10.1002/stem.39. [DOI] [PubMed] [Google Scholar]
- Chen G, Gulbranson DR, Hou Z, Bolin JM, Ruotti V, Probasco MD, Smuga-Otto K, Howden SE, Diol NR, Propson NE, et al. Chemically defined conditions for human iPSC derivation and culture. Nat Methods. 2011;8:424–429. doi: 10.1038/nmeth.1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng X, Ying L, Lu L, Galvao AM, Mills JA, Lin HC, Kotton DN, Shen SS, Nostro MC, Choi JK, et al. Self-renewing endodermal progenitor lines generated from human pluripotent stem cells. Cell Stem Cell. 2012;10:371–384. doi: 10.1016/j.stem.2012.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clement K, Vaisse C, Lahlou N, Cabrol S, Pelloux V, Cassuto D, Gourmelen M, Dina C, Chambaz J, Lacorte JM, et al. A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction. Nature. 1998;392:398–401. doi: 10.1038/32911. [DOI] [PubMed] [Google Scholar]
- Clocquet AR, Egan JM, Stoffers DA, Muller DC, Wideman L, Chin GA, Clarke WL, Hanks JB, Habener JF, Elahi D. Impaired insulin secretion and increased insulin sensitivity in familial maturity-onset diabetes of the young 4 (insulin promoter factor 1 gene) Diabetes. 2000;49:1856–1864. doi: 10.2337/diabetes.49.11.1856. [DOI] [PubMed] [Google Scholar]
- Collins FS, Mansoura MK. The Human Genome Project. Revealing the shared inheritance of all humankind. Cancer. 2001;91:221–225. doi: 10.1002/1097-0142(20010101)91:1+<221::aid-cncr8>3.3.co;2-0. [DOI] [PubMed] [Google Scholar]
- Collombat P, Hecksher-Sorensen J, Broccoli V, Krull J, Ponte I, Mundiger T, Smith J, Gruss P, Serup P, Mansouri A. The simultaneous loss of Arx and Pax4 genes promotes a somatostatin-producing cell fate specification at the expense of the alpha- and beta-cell lineages in the mouse endocrine pancreas. Development. 2005;132:2969–2980. doi: 10.1242/dev.01870. [DOI] [PubMed] [Google Scholar]
- Coppieters KT, Wiberg A, Tracy SM, von Herrath MG. Immunology in the clinic review series: focus on type 1 diabetes and viruses: the role of viruses in type 1 diabetes: a difficult dilemma. Clin Exp Immunol. 2012;168:5–11. doi: 10.1111/j.1365-2249.2011.04554.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig EA, Stevens MV, Vaillancourt RR, Camenisch TD. MAP3Ks as central regulators of cell fate during development. Dev Dyn. 2008;237:3102–3114. doi: 10.1002/dvdy.21750. [DOI] [PubMed] [Google Scholar]
- Davies JE, Siczkowski M, Sweeney FP, Quinn PA, Krolewski B, Krolewski AS, Ng LL. Glucose-induced changes in turnover of Na+/H+ exchanger of immortalized lymphoblasts from type I diabetic patients with nephropathy. Diabetes. 1995;44:382–388. doi: 10.2337/diab.44.4.382. [DOI] [PubMed] [Google Scholar]
- Dhingra R, Vasan RS. Diabetes and the risk of heart failure. Heart Fail Clin. 2012;8:125–133. doi: 10.1016/j.hfc.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Q, Lee YK, Schaefer EA, Peters DT, Veres A, Kim K, Kuperwasser N, Motola DL, Meissner TB, Hendriks WT, et al. A TALEN genome-editing system for generating human stem cell-based disease models. Cell Stem Cell. 2013a;12:238–251. doi: 10.1016/j.stem.2012.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Q, Regan SN, Xia Y, Oostrom LA, Cowan CA, Musunuru K. Enhanced efficiency of human pluripotent stem cell genome editing through replacing TALENs with CRISPRs. Cell Stem Cell. 2013b;12:393–394. doi: 10.1016/j.stem.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doria A, Patti ME, Kahn CR. The emerging genetic architecture of type 2 diabetes. Cell Metab. 2008;8:186–200. doi: 10.1016/j.cmet.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driver JP, Serreze DV, Chen YG. Mouse models for the study of autoimmune type 1 diabetes: a NOD to similarities and differences to human disease. Semin Immunopathol. 2011;33:67–87. doi: 10.1007/s00281-010-0204-1. [DOI] [PubMed] [Google Scholar]
- Dymecki SM, Niederhuber JE, Desiderio SV. Specific expression of a tyrosine kinase gene, blk, in B lymphoid cells. Science. 1990;247:332–336. doi: 10.1126/science.2404338. [DOI] [PubMed] [Google Scholar]
- Ebert AD, Yu J, Rose FF, Jr, Mattis VB, Lorson CL, Thomson JA, Svendsen CN. Induced pluripotent stem cells from a spinal muscular atrophy patient. Nature. 2009;457:277–280. doi: 10.1038/nature07677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edghill EL, Flanagan SE, Ellard S. Permanent neonatal diabetes due to activating mutations in ABCC8 and KCNJ11. Rev Endocr Metab Disord. 2010;11:193–198. doi: 10.1007/s11154-010-9149-x. [DOI] [PubMed] [Google Scholar]
- Eiselleova L, Matulka K, Kriz V, Kunova M, Schmidtova Z, Neradil J, Tichy B, Dvorakova D, Pospisilova S, Hampl A, et al. A complex role for FGF-2 in self-renewal, survival, and adhesion of human embryonic stem cells. Stem Cells. 2009;27:1847–1857. doi: 10.1002/stem.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erceg S, Ronaghi M, Stojkovic M. Human embryonic stem cell differentiation toward regional specific neural precursors. Stem Cells. 2009;27:78–87. doi: 10.1634/stemcells.2008-0543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fajans SS, Bell GI, Polonsky KS. Molecular mechanisms and clinical pathophysiology of maturity-onset diabetes of the young. N Engl J Med. 2001;345:971–980. doi: 10.1056/NEJMra002168. [DOI] [PubMed] [Google Scholar]
- Farooqi IS, Keogh JM, Yeo GS, Lank EJ, Cheetham T, O'Rahilly S. Clinical spectrum of obesity and mutations in the melanocortin 4 receptor gene. N Engl J Med. 2003;348:1085–1095. doi: 10.1056/NEJMoa022050. [DOI] [PubMed] [Google Scholar]
- Fernandez-Zapico ME, van Velkinburgh JC, Gutierrez-Aguilar R, Neve B, Froguel P, Urrutia R, Stein R. MODY7 gene, KLF11, is a novel p300-dependent regulator of Pdx-1 (MODY4) transcription in pancreatic islet beta cells. J Biol Chem. 2009;284:36482–36490. doi: 10.1074/jbc.M109.028852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer J. A genetic switch in pancreatic beta-cells: implications for differentiation and haploinsufficiency. Diabetes. 2002;51:2355–2362. doi: 10.2337/diabetes.51.8.2355. [DOI] [PubMed] [Google Scholar]
- Franks PW. Gene x environment interactions in type 2 diabetes. Curr Diab Rep. 2011;11:552–561. doi: 10.1007/s11892-011-0224-9. [DOI] [PubMed] [Google Scholar]
- Froguel P, Zouali H, Vionnet N, Velho G, Vaxillaire M, Sun F, Lesage S, Stoffel M, Takeda J, Passa P et al. Familial hyperglycemia due to mutations in glucokinase. Definition of a subtype of diabetes mellitus. N Engl J Med. 1993;328:697–702. doi: 10.1056/NEJM199303113281005. [DOI] [PubMed] [Google Scholar]
- Fujikura J, Nakao K, Sone M, Noguchi M, Mori E, Naito M, Taura D, Harada-Shiba M, Kishimoto I, Watanabe A, et al. Induced pluripotent stem cells generated from diabetic patients with mitochondrial DNA A3243G mutation. Diabetologia. 2012;55:1689–1698. doi: 10.1007/s00125-012-2508-2. [DOI] [PubMed] [Google Scholar]
- Ghosh S, Golbidi S, Werner I, Verchere BC, Laher I. Selecting exercise regimens and strains to modify obesity and diabetes in rodents: an overview. Clin Sci (Lond) 2010;119:57–74. doi: 10.1042/CS20090389. [DOI] [PubMed] [Google Scholar]
- Gonzalez F, Boue S, Izpisua Belmonte JC. Methods for making induced pluripotent stem cells: reprogramming a la carte. Nat Rev Genet. 2011;12:231–242. doi: 10.1038/nrg2937. [DOI] [PubMed] [Google Scholar]
- Gruppuso PA, Gorden P, Kahn CR, Cornblath M, Zeller WP, Schwartz R. Familial hyperproinsulinemia due to a proposed defect in conversion of proinsulin to insulin. N Engl J Med. 1984;311:629–634. doi: 10.1056/NEJM198409063111003. [DOI] [PubMed] [Google Scholar]
- Haldorsen IS, Vesterhus M, Raeder H, Jensen DK, Sovik O, Molven A, Njolstad PR. Lack of pancreatic body and tail in HNF1B mutation carriers. Diabet Med. 2008;25:782–787. doi: 10.1111/j.1464-5491.2008.02460.x. [DOI] [PubMed] [Google Scholar]
- Hambright D, Park KY, Brooks M, McKay R, Swaroop A, Nasonkin IO. Long-term survival and differentiation of retinal neurons derived from human embryonic stem cell lines in un-immunosuppressed mouse retina. Mol Vis. 2012;18:920–936. [PMC free article] [PubMed] [Google Scholar]
- Harwood HJ, Jr, Listrani P, Wagner JD. Nonhuman primates and other animal models in diabetes research. J Diabetes Sci Technol. 2012;6:503–514. doi: 10.1177/193229681200600304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hattersley AT, Ashcroft FM. Activating mutations in Kir6.2 and neonatal diabetes: new clinical syndromes, new scientific insights, and new therapy. Diabetes. 2005;54:2503–2513. doi: 10.2337/diabetes.54.9.2503. [DOI] [PubMed] [Google Scholar]
- Haumaitre C, Barbacci E, Jenny M, Ott MO, Gradwohl G, Cereghini S. Lack of TCF2/vHNF1 in mice leads to pancreas agenesis. Proc Natl Acad Sci U S A. 2005;102:1490–1495. doi: 10.1073/pnas.0405776102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayhurst GP, Lee YH, Lambert G, Ward JM, Gonzalez FJ. Hepatocyte nuclear factor 4alpha (nuclear receptor 2A1) is essential for maintenance of hepatic gene expression and lipid homeostasis. Mol Cell Biol. 2001;21:1393–1403. doi: 10.1128/MCB.21.4.1393-1403.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegele RA. Monogenic forms of insulin resistance: apertures that expose the common metabolic syndrome. Trends Endocrinol Metab. 2003;14:371–377. doi: 10.1016/s1043-2760(03)00142-5. [DOI] [PubMed] [Google Scholar]
- Horikawa Y, Iwasaki N, Hara M, Furuta H, Hinokio Y, Cockburn BN, Lindner T, Yamagata K, Ogata M, Tomonaga O, et al. Mutation in hepatocyte nuclear factor-1 beta gene (TCF2) associated with MODY. Nat Genet. 1997;17:384–385. doi: 10.1038/ng1297-384. [DOI] [PubMed] [Google Scholar]
- Hua H, Shang L, Martinez H, Freeby M, Gallagher MP, Ludwig T, Deng L, Greenberg E, Leduc C, Chung WK, et al. iPSC-derived beta cells model diabetes due to glucokinase deficiency. J Clin Invest. 2013 doi: 10.1172/JCI67638. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Ilag LL, Tabaei BP, Herman WH, Zawacki CM, D'Souza E, Bell GI, Fajans SS. Reduced pancreatic polypeptide response to hypoglycemia and amylin response to arginine in subjects with a mutation in the HNF-4alpha/MODY1 gene. Diabetes. 2000;49:961–968. doi: 10.2337/diabetes.49.6.961. [DOI] [PubMed] [Google Scholar]
- Islam MS, Loots du T. Experimental rodent models of type 2 diabetes: a review. Methods Find Exp Clin Pharmacol. 2009;31:249–261. doi: 10.1358/mf.2009.31.4.1362513. [DOI] [PubMed] [Google Scholar]
- Isomaa B, Henricsson M, Lehto M, Forsblom C, Karanko S, Sarelin L, Haggblom M, Groop L. Chronic diabetic complications in patients with MODY3 diabetes. Diabetologia. 1998;41:467–473. doi: 10.1007/s001250050931. [DOI] [PubMed] [Google Scholar]
- Itzhaki I, Maizels L, Huber I, Zwi-Dantsis L, Caspi O, Winterstern A, Feldman O, Gepstein A, Arbel G, Hammerman H, et al. Modelling the long QT syndrome with induced pluripotent stem cells. Nature. 2011;471:225–229. doi: 10.1038/nature09747. [DOI] [PubMed] [Google Scholar]
- Iynedjian PB, Pilot PR, Nouspikel T, Milburn JL, Quaade C, Hughes S, Ucla C, Newgard CB. Differential expression and regulation of the glucokinase gene in liver and islets of Langerhans. Proc Natl Acad Sci U S A. 1989;86:7838–7842. doi: 10.1073/pnas.86.20.7838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson RS, Creemers JW, Ohagi S, Raffin-Sanson ML, Sanders L, Montague CT, Hutton JC, O'Rahilly S. Obesity and impaired prohormone processing associated with mutations in the human prohormone convertase 1 gene. Nat Genet. 1997;16:303–306. doi: 10.1038/ng0797-303. [DOI] [PubMed] [Google Scholar]
- Jonsson J, Carlsson L, Edlund T, Edlund H. Insulin-promoter-factor 1 is required for pancreas development in mice. Nature. 1994;371:606–609. doi: 10.1038/371606a0. [DOI] [PubMed] [Google Scholar]
- Kahn CR. Banting Lecture. Insulin action, diabetogenes, and the cause of type II diabetes. Diabetes. 1994;43:1066–1084. doi: 10.2337/diab.43.8.1066. [DOI] [PubMed] [Google Scholar]
- Kahn CR, Vicent D, Doria A. Genetics of non-insulin-dependent (type-II) diabetes mellitus. Annu Rev Med. 1996;47:509–531. doi: 10.1146/annurev.med.47.1.509. [DOI] [PubMed] [Google Scholar]
- Kannankeril P, Roden DM, Darbar D. Drug-induced long QT syndrome. Pharmacol Rev. 2010;62:760–781. doi: 10.1124/pr.110.003723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keshet Y, Seger R. The MAP kinase signaling cascades: a system of hundreds of components regulates a diverse array of physiological functions. Methods Mol Biol. 2010;661:3–38. doi: 10.1007/978-1-60761-795-2_1. [DOI] [PubMed] [Google Scholar]
- Kida Y, Duffield JS. Pivotal role of pericytes in kidney fibrosis. Clin Exp Pharmacol Physiol. 2011;38:467–473. doi: 10.1111/j.1440-1681.2011.05531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim MS, Hwang NS, Lee J, Kim TK, Leong K, Shamblott MJ, Gearhart J, Elisseeff J. Musculoskeletal differentiation of cells derived from human embryonic germ cells. Stem Cells. 2005;23:113–123. doi: 10.1634/stemcells.2004-0110. [DOI] [PubMed] [Google Scholar]
- King AJ. The use of animal models in diabetes research. Br J Pharmacol. 2012;166:877–894. doi: 10.1111/j.1476-5381.2012.01911.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Pearson T, Rossini AA, Shultz LD, Greiner DL. Humanized mice for the study of type 1 diabetes and beta cell function. Ann N Y Acad Sci. 2008;1150:46–53. doi: 10.1196/annals.1447.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroon E, Martinson LA, Kadoya K, Bang AG, Kelly OG, Eliazer S, Young H, Richardson M, Smart NG, Cunningham J, et al. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat Biotechnol. 2008;26:443–452. doi: 10.1038/nbt1393. [DOI] [PubMed] [Google Scholar]
- Krude H, Biebermann H, Luck W, Horn R, Brabant G, Gruters A. Severe early-onset obesity, adrenal insufficiency and red hair pigmentation caused by POMC mutations in humans. Nat Genet. 1998;19:155–157. doi: 10.1038/509. [DOI] [PubMed] [Google Scholar]
- Kudva YC, Ohmine S, Greder LV, Dutton JR, Armstrong A, De Lamo JG, Khan YK, Thatava T, Hasegawa M, Fusaki N, et al. Transgene-free disease-specific induced pluripotent stem cells from patients with type 1 and type 2 diabetes. Stem Cells Transl Med. 2012;1:451–461. doi: 10.5966/sctm.2011-0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni RN, Zisman A. Lessons for human diabetes from experimental mouse models. Curr Diab Rep. 2003;3:168–175. doi: 10.1007/s11892-003-0041-x. [DOI] [PubMed] [Google Scholar]
- Lee AW, Cox RD. Use of mouse models in studying type 2 diabetes mellitus. Expert Rev Mol Med. 2011;13:e1. doi: 10.1017/S1462399410001729. [DOI] [PubMed] [Google Scholar]
- Lee G, Papapetrou EP, Kim H, Chambers SM, Tomishima MJ, Fasano CA, Ganat YM, Menon J, Shimizu F, Viale A, et al. Modelling pathogenesis and treatment of familial dysautonomia using patient-specific iPSCs. Nature. 2009;461:402–406. doi: 10.1038/nature08320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Wang G, Wang C, Zhao Y, Zhang H, Tan Z, Song Z, Ding M, Deng H. MEK/ERK signaling contributes to the maintenance of human embryonic stem cell self-renewal. Differentiation. 2007;75:299–307. doi: 10.1111/j.1432-0436.2006.00143.x. [DOI] [PubMed] [Google Scholar]
- Li L, Fukunaga-Kalabis M, Herlyn M. The three-dimensional human skin reconstruct model: a tool to study normal skin and melanoma progression. J Vis Exp. 2011 doi: 10.3791/2937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin SA, Kolle G, Grimmond SM, Zhou Q, Doust E, Little MH, Aronow B, Ricardo SD, Pera MF, Bertram JF, et al. Subfractionation of differentiating human embryonic stem cell populations allows the isolation of a mesodermal population enriched for intermediate mesoderm and putative renal progenitors. Stem Cells Dev. 2010;19:1637–1648. doi: 10.1089/scd.2010.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luitse MJ, Biessels GJ, Rutten GE, Kappelle LJ. Diabetes, hyperglycaemia, and acute ischaemic stroke. Lancet Neurol. 2012;11:261–271. doi: 10.1016/S1474-4422(12)70005-4. [DOI] [PubMed] [Google Scholar]
- Maassen JA, Janssen GM, t Hart LM. Molecular mechanisms of mitochondrial diabetes (MIDD) Ann Med. 2005;37:213–221. doi: 10.1080/07853890510007188. [DOI] [PubMed] [Google Scholar]
- Mackay DJ, Temple IK. Transient neonatal diabetes mellitus type 1. Am J Med Genet C Semin Med Genet. 2010;154C:335–342. doi: 10.1002/ajmg.c.30272. [DOI] [PubMed] [Google Scholar]
- Maehr R, Chen S, Snitow M, Ludwig T, Yagasaki L, Goland R, Leibel RL, Melton DA. Generation of pluripotent stem cells from patients with type 1 diabetes. Proc Natl Acad Sci U S A. 2009;106:15768–15773. doi: 10.1073/pnas.0906894106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magre J, Delepine M, Khallouf E, Gedde-Dahl T, Jr, Van Maldergem L, Sobel E, Papp J, Meier M, Megarbane A, Bachy A, et al. Identification of the gene altered in Berardinelli-Seip congenital lipodystrophy on chromosome 11q13. Nat Genet. 2001;28:365–370. doi: 10.1038/ng585. [DOI] [PubMed] [Google Scholar]
- Malecki MT, Jhala US, Antonellis A, Fields L, Doria A, Orban T, Saad M, Warram JH, Montminy M, Krolewski AS. Mutations in NEUROD1 are associated with the development of type 2 diabetes mellitus. Nat Genet. 1999;23:323–328. doi: 10.1038/15500. [DOI] [PubMed] [Google Scholar]
- Martin BC, Warram JH, Krolewski AS, Bergman RN, Soeldner JS, Kahn CR. Role of glucose and insulin resistance in development of type 2 diabetes mellitus: results of a 25-year follow-up study. Lancet. 1992;340:925–929. doi: 10.1016/0140-6736(92)92814-v. [DOI] [PubMed] [Google Scholar]
- Mathis D, Benoist C. The influence of the microbiota on type-1 diabetes: on the threshold of a leap forward in our understanding. Immunol Rev. 2012;245:239–249. doi: 10.1111/j.1600-065X.2011.01084.x. [DOI] [PubMed] [Google Scholar]
- Matschinsky FM, Glaser B, Magnuson MA. Pancreatic beta-cell glucokinase: closing the gap between theoretical concepts and experimental realities. Diabetes. 1998;47:307–315. doi: 10.2337/diabetes.47.3.307. [DOI] [PubMed] [Google Scholar]
- McCarthy MI. Genomics, type 2 diabetes, and obesity. The New England journal of medicine. 2010;363:2339–2350. doi: 10.1056/NEJMra0906948. [DOI] [PubMed] [Google Scholar]
- McLean AB, D'Amour KA, Jones KL, Krishnamoorthy M, Kulik MJ, Reynolds DM, Sheppard AM, Liu H, Xu Y, Baetge EE, et al. Activin a efficiently specifies definitive endoderm from human embryonic stem cells only when phosphatidylinositol 3-kinase signaling is suppressed. Stem Cells. 2007;25:29–38. doi: 10.1634/stemcells.2006-0219. [DOI] [PubMed] [Google Scholar]
- Mendel DB, Hansen LP, Graves MK, Conley PB, Crabtree GR. HNF-1 alpha and HNF-1 beta (vHNF-1) share dimerization and homeo domains, but not activation domains, and form heterodimers in vitro. Genes Dev. 1991;5:1042–1056. doi: 10.1101/gad.5.6.1042. [DOI] [PubMed] [Google Scholar]
- Merkle FT, Eggan K. Modeling human disease with pluripotent stem cells: from genome association to function. Cell Stem Cell. 2013;12:656–668. doi: 10.1016/j.stem.2013.05.016. [DOI] [PubMed] [Google Scholar]
- Miller SP, Anand GR, Karschnia EJ, Bell GI, LaPorte DC, Lange AJ. Characterization of glucokinase mutations associated with maturity-onset diabetes of the young type 2 (MODY-2): different glucokinase defects lead to a common phenotype. Diabetes. 1999;48:1645–1651. doi: 10.2337/diabetes.48.8.1645. [DOI] [PubMed] [Google Scholar]
- Millioni R, Puricelli L, Iori E, Trevisan R, Tessari P. Skin fibroblasts as a tool for identifying the risk of nephropathy in the type 1 diabetic population. Diabetes Metab Res Rev. 2012;28:62–70. doi: 10.1002/dmrr.1287. [DOI] [PubMed] [Google Scholar]
- Molven A, Ringdal M, Nordbo AM, Raeder H, Stoy J, Lipkind GM, Steiner DF, Philipson LH, Bergmann I, Aarskog D, et al. Mutations in the insulin gene can cause MODY and autoantibody-negative type 1 diabetes. Diabetes. 2008;57:1131–1135. doi: 10.2337/db07-1467. [DOI] [PubMed] [Google Scholar]
- Montague CT, Farooqi IS, Whitehead JP, Soos MA, Rau H, Wareham NJ, Sewter CP, Digby JE, Mohammed SN, Hurst JA, et al. Congenital leptin deficiency is associated with severe early-onset obesity in humans. Nature. 1997;387:903–908. doi: 10.1038/43185. [DOI] [PubMed] [Google Scholar]
- Moretti A, Bellin M, Welling A, Jung CB, Lam JT, Bott-Flugel L, Dorn T, Goedel A, Hohnke C, Hofmann F, et al. Patient-specific induced pluripotent stem-cell models for long-QT syndrome. N Engl J Med. 2010;363:1397–1409. doi: 10.1056/NEJMoa0908679. [DOI] [PubMed] [Google Scholar]
- Murry CE, Keller G. Differentiation of embryonic stem cells to clinically relevant populations: lessons from embryonic development. Cell. 2008;132:661–680. doi: 10.1016/j.cell.2008.02.008. [DOI] [PubMed] [Google Scholar]
- Narayanan K, Schumacher KM, Tasnim F, Kandasamy K, Schumacher A, Ni M, Gao S, Gopalan B, Zink D, Ying JY. Human embryonic stem cells differentiate into functional renal proximal tubular-like cells. Kidney Int. 2013;83:593–603. doi: 10.1038/ki.2012.442. [DOI] [PubMed] [Google Scholar]
- Naya FJ, Huang HP, Qiu Y, Mutoh H, DeMayo FJ, Leiter AB, Tsai MJ. Diabetes, defective pancreatic morphogenesis, and abnormal enteroendocrine differentiation in BETA2/neuroD-deficient mice. Genes Dev. 1997;11:2323–2334. doi: 10.1101/gad.11.18.2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neve B, Fernandez-Zapico ME, Ashkenazi-Katalan V, Dina C, Hamid YH, Joly E, Vaillant E, Benmezroua Y, Durand E, Bakaher N, et al. Role of transcription factor KLF11 and its diabetes-associated gene variants in pancreatic beta cell function. Proc Natl Acad Sci U S A. 2005;102:4807–4812. doi: 10.1073/pnas.0409177102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Njolstad PR, Sovik O, Cuesta-Munoz A, Bjorkhaug L, Massa O, Barbetti F, Undlien DE, Shiota C, Magnuson MA, Molven A, et al. Neonatal diabetes mellitus due to complete glucokinase deficiency. N Engl J Med. 2001;344:1588–1592. doi: 10.1056/NEJM200105243442104. [DOI] [PubMed] [Google Scholar]
- Odom DT, Dowell RD, Jacobsen ES, Gordon W, Danford TW, MacIsaac KD, Rolfe PA, Conboy CM, Gifford DK, Fraenkel E. Tissue-specific transcriptional regulation has diverged significantly between human and mouse. Nat Genet. 2007;39:730–732. doi: 10.1038/ng2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohmine S, Squillace KA, Hartjes KA, Deeds MC, Armstrong AS, Thatava T, Sakuma T, Terzic A, Kudva Y, Ikeda Y. Reprogrammed keratinocytes from elderly type 2 diabetes patients suppress senescence genes to acquire induced pluripotency. Aging (Albany NY) 2012;4:60–73. doi: 10.18632/aging.100428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oki K, Tatarishvili J, Wood J, Koch P, Wattananit S, Mine Y, Monni E, Tornero D, Ahlenius H, Ladewig J, et al. Human-induced pluripotent stem cells form functional neurons and improve recovery after grafting in stroke-damaged brain. Stem Cells. 2012;30:1120–1133. doi: 10.1002/stem.1104. [DOI] [PubMed] [Google Scholar]
- Oliver MF, Opie LH. Effects of glucose and fatty acids on myocardial ischaemia and arrhythmias. Lancet. 1994;343:155–158. doi: 10.1016/s0140-6736(94)90939-3. [DOI] [PubMed] [Google Scholar]
- Onat D, Brillon D, Colombo PC, Schmidt AM. Human vascular endothelial cells: a model system for studying vascular inflammation in diabetes and atherosclerosis. Curr Diab Rep. 2011;11:193–202. doi: 10.1007/s11892-011-0182-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osbak KK, Colclough K, Saint-Martin C, Beer NL, Bellanne-Chantelot C, Ellard S, Gloyn AL. Update on mutations in glucokinase (GCK), which cause maturity-onset diabetes of the young, permanent neonatal diabetes, and hyperinsulinemic hypoglycemia. Hum Mutat. 2009;30:1512–1526. doi: 10.1002/humu.21110. [DOI] [PubMed] [Google Scholar]
- Park IH, Arora N, Huo H, Maherali N, Ahfeldt T, Shimamura A, Lensch MW, Cowan C, Hochedlinger K, Daley GQ. Disease-specific induced pluripotent stem cells. Cell. 2008;134:877–886. doi: 10.1016/j.cell.2008.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson ER, Flechtner I, Njolstad PR, Malecki MT, Flanagan SE, Larkin B, Ashcroft FM, Klimes I, Codner E, Iotova V, et al. Switching from insulin to oral sulfonylureas in patients with diabetes due to Kir6.2 mutations. N Engl J Med. 2006;355:467–477. doi: 10.1056/NEJMoa061759. [DOI] [PubMed] [Google Scholar]
- Pearson ER, Velho G, Clark P, Stride A, Shepherd M, Frayling TM, Bulman MP, Ellard S, Froguel P, Hattersley AT. beta-cell genes and diabetes: quantitative and qualitative differences in the pathophysiology of hepatic nuclear factor-1alpha and glucokinase mutations. Diabetes. 2001;50(1):S101–107. doi: 10.2337/diabetes.50.2007.s101. [DOI] [PubMed] [Google Scholar]
- Pellegrini G, De Luca M. Human embryonic stem cell-derived keratinocytes: how close to clinics? Cell Stem Cell. 2010;6:8–9. doi: 10.1016/j.stem.2009.12.002. [DOI] [PubMed] [Google Scholar]
- Petersen KF, Shulman GI. Etiology of insulin resistance. Am J Med. 2006;119:S10–16. doi: 10.1016/j.amjmed.2006.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plengvidhya N, Kooptiwut S, Songtawee N, Doi A, Furuta H, Nishi M, Nanjo K, Tantibhedhyangkul W, Boonyasrisawat W, Yenchitsomanus PT, et al. PAX4 mutations in Thais with maturity onset diabetes of the young. J Clin Endocrinol Metab. 2007;92:2821–2826. doi: 10.1210/jc.2006-1927. [DOI] [PubMed] [Google Scholar]
- Polo JM, Liu S, Figueroa ME, Kulalert W, Eminli S, Tan KY, Apostolou E, Stadtfeld M, Li Y, Shioda T, et al. Cell type of origin influences the molecular and functional properties of mouse induced pluripotent stem cells. Nat Biotechnol. 2010;28:848–855. doi: 10.1038/nbt.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polychronakos C, Li Q. Understanding type 1 diabetes through genetics: advances and prospects. Nat Rev Genet. 2011;12:781–792. doi: 10.1038/nrg3069. [DOI] [PubMed] [Google Scholar]
- Prado CL, Pugh-Bernard AE, Elghazi L, Sosa-Pineda B, Sussel L. Ghrelin cells replace insulin-producing beta cells in two mouse models of pancreas development. Proc Natl Acad Sci U S A. 2004;101:2924–2929. doi: 10.1073/pnas.0308604100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pramfalk C, Karlsson E, Groop L, Rudel LL, Angelin B, Eriksson M, Parini P. Control of ACAT2 liver expression by HNF4{alpha}: lesson from MODY1 patients. Arterioscler Thromb Vasc Biol. 2009;29:1235–1241. doi: 10.1161/ATVBAHA.109.188581. [DOI] [PubMed] [Google Scholar]
- Raeder H, Johansson S, Holm PI, Haldorsen IS, Mas E, Sbarra V, Nermoen I, Eide SA, Grevle L, Bjorkhaug L, et al. Mutations in the CEL VNTR cause a syndrome of diabetes and pancreatic exocrine dysfunction. Nat Genet. 2006;38:54–62. doi: 10.1038/ng1708. [DOI] [PubMed] [Google Scholar]
- Rask-Madsen C, Kahn CR. Tissue-specific insulin signaling, metabolic syndrome, and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2012;32:2052–2059. doi: 10.1161/ATVBAHA.111.241919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezania A, Riedel MJ, Wideman RD, Karanu F, Ao Z, Warnock GL, Kieffer TJ. Production of functional glucagon-secreting alpha-cells from human embryonic stem cells. Diabetes. 2011;60:239–247. doi: 10.2337/db10-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson R, Barathi VA, Chaurasia SS, Wong TY, Kern TS. Update on animal models of diabetic retinopathy: from molecular approaches to mice and higher mammals. Dis Model Mech. 2012;5:444–456. doi: 10.1242/dmm.009597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinton DA, Daley GQ. The promise of induced pluripotent stem cells in research and therapy. Nature. 2012;481:295–305. doi: 10.1038/nature10761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowland TJ, Buchholz DE, Clegg DO. Pluripotent human stem cells for the treatment of retinal disease. J Cell Physiol. 2012;227:457–466. doi: 10.1002/jcp.22814. [DOI] [PubMed] [Google Scholar]
- Schulz TC, Young HY, Agulnick AD, Babin MJ, Baetge EE, Bang AG, Bhoumik A, Cepa I, Cesario RM, Haakmeester C, et al. A scalable system for production of functional pancreatic progenitors from human embryonic stem cells. PLoS One. 2012;7:e37004. doi: 10.1371/journal.pone.0037004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple RK, Savage DB, Cochran EK, Gorden P, O'Rahilly S. Genetic syndromes of severe insulin resistance. Endocr Rev. 2011;32:498–514. doi: 10.1210/er.2010-0020. [DOI] [PubMed] [Google Scholar]
- Shackleton S, Lloyd DJ, Jackson SN, Evans R, Niermeijer MF, Singh BM, Schmidt H, Brabant G, Kumar S, Durrington PN, et al. LMNA, encoding lamin A/C, is mutated in partial lipodystrophy. Nat Genet. 2000;24:153–156. doi: 10.1038/72807. [DOI] [PubMed] [Google Scholar]
- Shapiro AM. State of the art of clinical islet transplantation and novel protocols of immunosuppression. Curr Diab Rep. 2011;11:345–354. doi: 10.1007/s11892-011-0217-8. [DOI] [PubMed] [Google Scholar]
- Shih DQ, Dansky HM, Fleisher M, Assmann G, Fajans SS, Stoffel M. Genotype/phenotype relationships in HNF-4alpha/MODY1: haploinsufficiency is associated with reduced apolipoprotein (AII), apolipoprotein (CIII), lipoprotein(a), and triglyceride levels. Diabetes. 2000;49:832–837. doi: 10.2337/diabetes.49.5.832. [DOI] [PubMed] [Google Scholar]
- Shirasawa S, Yoshie S, Yue F, Ichikawa H, Yokoyama T, Nagai M, Tomotsune D, Hirayama M, Sasaki K. Pancreatic exocrine enzyme-producing cell differentiation via embryoid bodies from human embryonic stem cells. Biochem Biophys Res Commun. 2011;410:608–613. doi: 10.1016/j.bbrc.2011.06.036. [DOI] [PubMed] [Google Scholar]
- Siegert S, Cabuy E, Scherf BG, Kohler H, Panda S, Le YZ, Fehling HJ, Gaidatzis D, Stadler MB, Roska B. Transcriptional code and disease map for adult retinal cell types. Nat Neurosci. 2012;15:487–495. S481–482. doi: 10.1038/nn.3032. [DOI] [PubMed] [Google Scholar]
- Song CZ, Gavriilidis G, Asano H, Stamatoyannopoulos G. Functional study of transcription factor KLF11 by targeted gene inactivation. Blood Cells Mol Dis. 2005;34:53–59. doi: 10.1016/j.bcmd.2004.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sovik O, Njolstad P, Folling I, Sagen J, Cockburn BN, Bell GI. Hyperexcitability to sulphonylurea in MODY3. Diabetologia. 1998;41:607–608. doi: 10.1007/s001250050956. [DOI] [PubMed] [Google Scholar]
- Sproule DM, Kaufmann P. Mitochondrial encephalopathy, lactic acidosis, and strokelike episodes: basic concepts, clinical phenotype, and therapeutic management of MELAS syndrome. Ann N Y Acad Sci. 2008;1142:133–158. doi: 10.1196/annals.1444.011. [DOI] [PubMed] [Google Scholar]
- Steck AK, Winter WE. Review on monogenic diabetes. Curr Opin Endocrinol Diabetes Obes. 2011;18:252–258. doi: 10.1097/MED.0b013e3283488275. [DOI] [PubMed] [Google Scholar]
- Steiner DF, Tager HS, Chan SJ, Nanjo K, Sanke T, Rubenstein AH. Lessons learned from molecular biology of insulin-gene mutations. Diabetes Care. 1990;13:600–609. doi: 10.2337/diacare.13.6.600. [DOI] [PubMed] [Google Scholar]
- Stoffel M, Froguel P, Takeda J, Zouali H, Vionnet N, Nishi S, Weber IT, Harrison RW, Pilkis SJ, Lesage S, et al. Human glucokinase gene: isolation, characterization, and identification of two missense mutations linked to early-onset non-insulin-dependent (type 2) diabetes mellitus. Proc Natl Acad Sci U S A. 1992;89:7698–7702. doi: 10.1073/pnas.89.16.7698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoffers DA, Zinkin NT, Stanojevic V, Clarke WL, Habener JF. Pancreatic agenesis attributable to a single nucleotide deletion in the human IPF1 gene coding sequence. Nat Genet. 1997;15:106–110. doi: 10.1038/ng0197-106. [DOI] [PubMed] [Google Scholar]
- Stoy J, Steiner DF, Park SY, Ye H, Philipson LH, Bell GI. Clinical and molecular genetics of neonatal diabetes due to mutations in the insulin gene. Rev Endocr Metab Disord. 2010;11:205–215. doi: 10.1007/s11154-010-9151-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swistowski A, Peng J, Liu Q, Mali P, Rao MS, Cheng L, Zeng X. Efficient generation of functional dopaminergic neurons from human induced pluripotent stem cells under defined conditions. Stem Cells. 2010;28:1893–1904. doi: 10.1002/stem.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- Tan KY, Eminli S, Hettmer S, Hochedlinger K, Wagers AJ. Efficient generation of iPS cells from skeletal muscle stem cells. PLoS One. 2011;6:e26406. doi: 10.1371/journal.pone.0026406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taniguchi CM, Emanuelli B, Kahn CR. Critical nodes in signalling pathways: insights into insulin action. Nat Rev Mol Cell Biol. 2006;7:85–96. doi: 10.1038/nrm1837. [DOI] [PubMed] [Google Scholar]
- Taylor SI. Lilly Lecture: molecular mechanisms of insulin resistance. Lessons from patients with mutations in the insulin-receptor gene. Diabetes. 1992;41:1473–1490. doi: 10.2337/diab.41.11.1473. [DOI] [PubMed] [Google Scholar]
- Teo AK, Windmueller R, Johansson BB, Dirice E, Njolstad PR, Tjora E, Raeder H, Kulkarni RN. Derivation of human induced pluripotent stem cells from patients with maturity onset diabetes of the young. J Biol Chem. 2013;288:5353–5356. doi: 10.1074/jbc.C112.428979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Texido G, Su IH, Mecklenbrauker I, Saijo K, Malek SN, Desiderio S, Rajewsky K, Tarakhovsky A. The B-cell-specific Src-family kinase Blk is dispensable for B-cell development and activation. Mol Cell Biol. 2000;20:1227–1233. doi: 10.1128/mcb.20.4.1227-1233.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thatava T, Kudva YC, Edukulla R, Squillace K, De Lamo JG, Khan YK, Sakuma T, Ohmine S, Terzic A, Ikeda Y. Intrapatient Variations in Type 1 Diabetes-specific iPS Cell Differentiation Into Insulin-producing Cells. Mol Ther. 2012 doi: 10.1038/mt.2012.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirabassi RS, Flanagan JF, Wu T, Kislauskis EH, Birckbichler PJ, Guberski DL. The BBZDR/Wor rat model for investigating the complications of type 2 diabetes mellitus. ILAR J. 2004;45:292–302. doi: 10.1093/ilar.45.3.292. [DOI] [PubMed] [Google Scholar]
- Tiscornia G, Vivas EL, Belmonte JC. Diseases in a dish: modeling human genetic disorders using induced pluripotent cells. Nat Med. 2011;17:1570–1576. doi: 10.1038/nm.2504. [DOI] [PubMed] [Google Scholar]
- Tsigos C, Kyrou I, Raptis SA. Monogenic forms of obesity and diabetes mellitus. J Pediatr Endocrinol Metab. 2002;15:241–253. doi: 10.1515/JPEM.2002.15.3.241. [DOI] [PubMed] [Google Scholar]
- Vallon V, Thomson SC. Renal function in diabetic disease models: the tubular system in the pathophysiology of the diabetic kidney. Annu Rev Physiol. 2012;74:351–375. doi: 10.1146/annurev-physiol-020911-153333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Belle TL, Coppieters KT, von Herrath MG. Type 1 diabetes: etiology, immunology, and therapeutic strategies. Physiol Rev. 2011;91:79–118. doi: 10.1152/physrev.00003.2010. [DOI] [PubMed] [Google Scholar]
- Velho G, Froguel P, Clement K, Pueyo ME, Rakotoambinina B, Zouali H, Passa P, Cohen D, Robert JJ. Primary pancreatic beta-cell secretory defect caused by mutations in glucokinase gene in kindreds of maturity onset diabetes of the young. Lancet. 1992;340:444–448. doi: 10.1016/0140-6736(92)91768-4. [DOI] [PubMed] [Google Scholar]
- Velho G, Petersen KF, Perseghin G, Hwang JH, Rothman DL, Pueyo ME, Cline GW, Froguel P, Shulman GI. Impaired hepatic glycogen synthesis in glucokinase-deficient (MODY-2) subjects. J Clin Invest. 1996;98:1755–1761. doi: 10.1172/JCI118974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vesterhus M, Raeder H, Kurpad AJ, Kawamori D, Molven A, Kulkarni RN, Kahn CR, Njolstad PR. Pancreatic function in carboxyl-ester lipase knockout mice. Pancreatology. 2010;10:467–476. doi: 10.1159/000266284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent AM, Callaghan BC, Smith AL, Feldman EL. Diabetic neuropathy: cellular mechanisms as therapeutic targets. Nat Rev Neurol. 2011;7:573–583. doi: 10.1038/nrneurol.2011.137. [DOI] [PubMed] [Google Scholar]
- Visscher PM, Brown MA, McCarthy MI, Yang J. Five years of GWAS discovery. Am J Hum Genet. 2012;90:7–24. doi: 10.1016/j.ajhg.2011.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Schulz TC, Sherrer ES, Dauphin DS, Shin S, Nelson AM, Ware CB, Zhan M, Song CZ, Chen X, et al. Self-renewal of human embryonic stem cells requires insulin-like growth factor-1 receptor and ERBB2 receptor signaling. Blood. 2007;110:4111–4119. doi: 10.1182/blood-2007-03-082586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welham MJ, Storm MP, Kingham E, Bone HK. Phosphoinositide 3-kinases and regulation of embryonic stem cell fate. Biochem Soc Trans. 2007;35:225–228. doi: 10.1042/BST0350225. [DOI] [PubMed] [Google Scholar]
- Winter WE, Schatz DA. Autoimmune markers in diabetes. Clin Chem. 2011;57:168–175. doi: 10.1373/clinchem.2010.148205. [DOI] [PubMed] [Google Scholar]
- Wu KK, Huan Y. Diabetic atherosclerosis mouse models. Atherosclerosis. 2007;191:241–249. doi: 10.1016/j.atherosclerosis.2006.08.030. [DOI] [PubMed] [Google Scholar]
- Yamagata K, Furuta H, Oda N, Kaisaki PJ, Menzel S, Cox NJ, Fajans SS, Signorini S, Stoffel M, Bell GI. Mutations in the hepatocyte nuclear factor-4alpha gene in maturity-onset diabetes of the young (MODY1) Nature. 1996a;384:458–460. doi: 10.1038/384458a0. [DOI] [PubMed] [Google Scholar]
- Yamagata K, Oda N, Kaisaki PJ, Menzel S, Furuta H, Vaxillaire M, Southam L, Cox RD, Lathrop GM, Boriraj VV, et al. Mutations in the hepatocyte nuclear factor-1alpha gene in maturity-onset diabetes of the young (MODY3) Nature. 1996b;384:455–458. doi: 10.1038/384455a0. [DOI] [PubMed] [Google Scholar]
- Yamagata K, Yang Q, Yamamoto K, Iwahashi H, Miyagawa J, Okita K, Yoshiuchi I, Miyazaki J, Noguchi T, Nakajima H, et al. Mutation P291fsinsC in the transcription factor hepatocyte nuclear factor-1alpha is dominant negative. Diabetes. 1998;47:1231–1235. doi: 10.2337/diab.47.8.1231. [DOI] [PubMed] [Google Scholar]
- Yang YM, Gupta SK, Kim KJ, Powers BE, Cerqueira A, Wainger BJ, Ngo HD, Rosowski KA, Schein PA, Ackeifi CA, et al. A Small Molecule Screen in Stem-Cell-Derived Motor Neurons Identifies a Kinase Inhibitor as a Candidate Therapeutic for ALS. Cell Stem Cell. 2013;12:713–726. doi: 10.1016/j.stem.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J, Vodyanik MA, Smuga-Otto K, Antosiewicz-Bourget J, Frane JL, Tian S, Nie J, Jonsdottir GA, Ruotti V, Stewart R, et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318:1917–1920. doi: 10.1126/science.1151526. [DOI] [PubMed] [Google Scholar]
- Zeng H, Guo M, Martins-Taylor K, Wang X, Zhang Z, Park JW, Zhan S, Kronenberg MS, Lichtler A, Liu HX, et al. Specification of region-specific neurons including forebrain glutamatergic neurons from human induced pluripotent stem cells. PLoS One. 2010;5:e11853. doi: 10.1371/journal.pone.0011853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao T, Zhang ZN, Rong Z, Xu Y. Immunogenicity of induced pluripotent stem cells. Nature. 2011;474:212–215. doi: 10.1038/nature10135. [DOI] [PubMed] [Google Scholar]
- Zhou L, Wang W, Liu Y, Fernandez de Castro J, Ezashi T, Telugu BP, Roberts RM, Kaplan HJ, Dean DC. Differentiation of induced pluripotent stem cells of swine into rod photoreceptors and their integration into the retina. Stem Cells. 2011;29:972–980. doi: 10.1002/stem.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.