SUMMARY
Market-based solutions are often proposed to improve health care quality; yet evidence on the role of competition in quality in non-hospital settings is sparse. We examine the relationship between competition and quality in home health care. This market is different from other markets in that service delivery takes place in patients’ homes, which implies low costs of market entry and exit for agencies. We use 6 years of panel data for Medicare beneficiaries during the early 2000s. We identify the competition effect from within-market variation in competition over time. We analyze three quality measures: functional improvements, the number of home health visits, and discharges without hospitalization. We find that the relationship between competition and home health quality is nonlinear and its pattern differs by quality measure. Competition has positive effects on functional improvements and the number of visits in most ranges, but in the most competitive markets, functional outcomes and the number of visits slightly drop. Competition has a negative effect on discharges without hospitalization that is strongest in the most competitive markets. This finding is different from prior research on hospital markets and suggests that market-specific environments should be considered in developing polices to promote competition.
Keywords: competition, quality of care, home health care markets
1. INTRODUCTION
Deficiencies in quality of health care (Kohn et al., 1999; Institute of Medicine, 2001; McGlynn et al., 2003) suggest opportunities to improve quality exist throughout the health care system. Yet agreement on an effective approach is elusive which at its core can be traced to the debate over the extent to which policy should rely on market-based solutions. Extending the evidence on the role of market competition in enhancing quality can help inform this debate.
Economic theory suggests that competition can enhance quality in markets with regulated prices because providers will compete for patients by improving quality (Gaynor, 2006). Results from recent empirical studies in hospital markets appear to support this prediction, but the evidence for other markets is sparse. The reliance on market mechanisms to improve quality increases as quality reporting and pay-for-performance (P4P) programs are adopted in diverse settings; yet the role of the market in non-hospital settings remains unexamined.
We examine the relationship between competition and quality in home health care for Medicare beneficiaries.1 Home health care, which represents about 4% of Medicare expenditure, is a growing source of post-acute care for the elderly in US (Kaiser Family Foundation, 2009).2 Prior literature suggests that the relationship between competition and quality in post-acute care settings may be different from other markets because imperfect information of patients about provider quality is particularly severe (Hirth, 1999; Chou, 2002). If patients have difficulty in assessing quality, providers will not invest in quality (Akerlof, 1970), suggesting that the role of market in improving quality may be limited. Home health care markets further deviate from other markets because service delivery takes place in patients’ homes. This unique feature reduces the fixed costs of market entry for home health agencies and it reduces the market power of facility location. With these lower barriers to competition, market competition may have a stronger effect on quality than that in hospital markets. Yet low fixed costs also reduce friction for market exit; therefore, when facing competition, marginal home health agencies may choose to exit rather than invest in quality.
We estimate the effect of competition on home health quality using 6 years of panel data during the early 2000s. Because this was a period of expansion in the number of agencies, we identify the competition effect from the over-time change within a market using market fixed effects. Further, because some states have applied Certificate of Need (CON) laws that restrict market entries of providers to home health care, we conduct separate analysis by CON status of states and explore the role of easy exits in the relationship between competition and quality in markets where entries are relatively regulated.
2. BACKGROUND
The theoretical relationship between competition and quality is complex and has long been discussed in the literature. Gaynor (2006), in his review of the economic literature on the topic, concludes that theoretical predictions about the effect of competition on quality are ambiguous when providers set market prices but competition enhances quality in markets with administratively set prices. The idea is that if price is regulated, providers will compete over a different dimension than price (i.e., quality) to attract consumers, and if the regulated price is set above marginal cost, providers will increase quality until profit is zero. Several empirical studies examining Medicare hospital markets where prices are prospectively set based on patients’ diagnoses have reported that competition improves quality (Kessler and McClellan, 2000; Tay, 2003; Shen, 2003; Kessler and Geppert, 2005).
The price of Medicare home health care is also set administratively. Medicare prospectively pays agencies for a 60-day episode of care after adjusting for patients’ expected costs. While this price-setting mechanism is similar to that in hospital markets, competition may have different effects. As noted earlier, market entry does not incur large fixed costs in home health care. Thus, agencies can enter profitable markets with little up-front expenses. Thus when the market becomes competitive and profit declines, exit is more attractive to agencies than investing in quality, compared to sectors where high financial losses accompany exit. In fact, observers of this market have noted that the home health care industry comprises small and incompetent agencies that do not have the technical capacity to survive or adjust to market environments (Bishop et al., 1999). If this effect dominates, the theoretical relationship between competition and quality under regulated price could be reversed.
In addition, although it is assumed in the Gaynor (2006) model that consumers choose providers based on quality, little is known about the demand responsiveness to quality in home health care. As described earlier, prior literature indicates that consumers’ uncertainty about service quality is likely to be severe in post-acute settings (Hirth, 1999; Chou, 2002). If this is the case, even under competition, agencies may underinvest in quality or they may focus only on quality measures that are easily assessable by patients. Given these theoretical ambiguities, our objective is to empirically explore the relationship between competition and home health quality.
Addressing the issue of home health quality is important as demand for home health care is expected to continue to grow given technology advancement expanding the type of home health services (Levine et al., 2003; Han et al., 2007) and given that home health care is viewed as a cost-effective alternative to facility-based care (Chen et al., 2000; Konetzka et al., 2008). Recent quality initiatives by the Center for Medicare and Medicare Services in home health care include market-based approaches, such as public reporting and P4P programs. Since the success of these programs depends on well-functioning markets, it is important to assess the implications of competition on home health quality.
We exploit variation across two domains to identify the effect of competition. First, we use variation in competition over time. Home health care markets have shown fluctuations in agency supply given the ease of entry and exit. Between 1980 and 1990, more than 5,700 agencies entered the Medicare home health market whereas about 2,800 agencies exited the market (Scalzi et al., 1994). The number of Medicare-participating agencies was 10,927 in 1997 but dropped to 7,057 in 2002 and increased to 8,955 in 2006 (MedPAC, 2008). This latest expansion may partially result from the introduction of the Prospective Payment System (PPS) for Medicare home health care in 2000. During the post-PPS period (2002–2005), agency margins averaged about 16% (MedPAC, 2008).
Second, we exploit state variation in regulations to control agency entry through CON laws3 that impose restrictions on capital investment by providers (e.g., the construction of new facilities or purchasing of expensive technology) to contain costs (MHCC, 2001). However, because home health care is a labor-intensive industry, CON operates as a mechanism to restrict entry of new agencies. We therefore hypothesize that the quality disincentive of exit will predominate in markets in CON states.
3. EMPIRICAL MODEL
Our empirical model is based on Gaynor (2006) that specifies a firm’s quality choice at equilibrium (Q*) in markets with regulated prices as follows:
| (1) |
where P̄ is the service price, which is set administratively. C is marginal cost, D is market demand at Q*, and MS is the firm’s market share. Price, market demand, and the firm’s market share have positive relationships with quality, whereas marginal cost has a negative relationship with quality.
Equation (1) indicates that cost, market demand, and market share are in turn a function of quality. This endogeneity leads us to take a reduced-form approach with exogenous determinants of marginal cost, demand, and a measure of market competition as follows:
| (2) |
where QUALijmt is quality of the ith episode of the jth agency in the mth market in year t. CPTmt is the level of competition in the mth market in year t. COSTijmt and DMDijmt represent a vector of cost and demand shifters, respectively. Time dummies (Tt) capture year-specific effects.
Several concerns arise from this reduced-form equation. First, some variables that are correlated with both competition and quality are likely to be unobserved, such as health care utilization patterns. Patients in competitive markets may be high users of health services, which contribute to better health outcomes. We address this possibility using market fixed effects that control for all unobserved time-invariant market factors.
Second, a competition measure based on actual market shares is endogenous to quality because market shares are a function of quality. We thus construct our competition measure using predicted market shares of agencies.4
Finally, responses to competition in terms of quality may differ depending on the level of competition (Kessler and McClellan, 2000). We capture a potential nonlinear relationship using indicators of competition deciles.
Our final empirical model is written as follows:
| (3) |
where I(•) is an indicator function of competition deciles and is the level of competition in the mth market in year t, measured on the basis of predicted market shares. Mm are market fixed effects. COSTijmt, DMDijmt, and Tt are the same as equation (2). We follow the prior literature and define market areas for home health care by zip codes (Porell et al., 2006).
We explore the sensitivity of the model to alternative specifications of a linear model and a model without market fixed effects. We also estimate the model separately by CON status to examine whether the effect of exit is better observed in states with CON, which restricts entry but not exit. All models are estimated using linear regressions. Standard errors are corrected for clustering among observations at the market level.
3.1. Quality measures
We analyze three indicators of home health quality. The first indicator is a composite measure of improvements in functional status during an episode. An episode is a care period between a patient’s admission to an agency and discharge from the agency. Functional status represents how well patients perform activities of daily living, such as bathing, transferring, taking medications, and managing shortness of breath or incontinency. These activities are among the main targets of home health services, whose goal is to assist patients in independently managing daily activities. For each activity, we construct an indicator of the improvement in functional status between the start and end of an episode. Recent quality initiatives by Medicare use these indicators as quality measures (Murtaugh et al., 2007). A composite measure is computed as the proportion of indicators with improvement among activities that were not at the highest level of functioning at baseline. About 15% of observations, which could not experience improvement, were excluded from the analysis of functional improvements.
The second measure captures whether an episode ends without being interrupted by hospitalization (discharge without a hospitalization). Another focus of home health care is to help patients manage their conditions at home by identifying signs of problems and continuing care they need. A hospitalization during an episode thus indicates poor quality of care and also has been used in the quality programs by Medicare.
Finally, we use the number of visits because patients may assess home health quality on the basis of easy-to-observe aspects and agencies may compete over those features. We construct this measure as the weighted number of home health aide, skilled nursing, and therapy visits. As the weight, we use the relative value of each service type, which represents different intensities of care and hence different costs of resource use (Welch et al., 1996).
3.2. Competition measures
We measure competition by the Herfindahl–Hirschman Index (HHI). We use the predicted HHI following the approach developed by Kessler and McClellan (2000) to address the part of HHI that might be endogenous to quality. This is done as follows: (1) We estimate a patient-level conditional choice model that uses distance between the agency office and the patient’s residence to identify choice of agency independent of quality.5 This model predicts patients’ probabilities of choosing each agency in a market (zip code), from which we calculate the predicted market share of an agency in the market.6 We obtain the predicted HHI of each market from the predicted market shares of agencies. (2) We then construct an agency-level HHI, to reflect agencies’ quality decisions, as a weighted average of the predicted HHIs for all the markets that the agency serves, where the weight is the predicted share of the agency’s patients coming from each market. (3) Finally, we obtain a weighted average of the agency-level HHIs for all agencies serving the market, with the weight being each agency’s share of patients in the market.
This is our primary measure of competition and its variation comes from (1) agency entries/exits (i.e., openings/closings), (2) agencies’ strategic shifts in patient shares across their market areas, and (3) patients’ agency choice decisions.
3.3. Cost and demand shifters
Cost shifters include agency attributes, such as agency size, the number of nurses and aides, and Medicare tenure. Agencies with larger size, longer tenure, and more nurses/aides may be more efficient in organizing quality-related activities than their counterparts (Jung et al., 2010). Demand shifters capture patients’ illness severity and service needs. They include patient age, gender, race, Medicaid buy-in status, health-risk factors (smoking, alcohol dependency, obesity), health status (cognitive status, depression, vision impairment, behavioral problems, and baseline functional status), having a caregiver, hospital discharge within 14 days before the home health use, and the number of patients in a market. In the models without fixed effects, we use county-level measures of the availability of other post-acute care facilities (Skilled Nursing Facilities (SNF) and Long-term Care (LTC) hospitals), which capture both market demand for post-acute services and potential competition among post-acute care providers.
3.4. Sensitivity checks
We perform several sensitivity checks to examine how our competition measure and approach influence study results. First, we analyze the model using alternative competition measures that focus on the variation in competition due to agency entries/exits: (1) predicted HHIs at the county level and (2) the number of agencies—measured at both zip code and county levels. County-level HHI is not affected by changes in agencies’ patient shares across their market areas because agencies tend to operate within a county due to regulatory constraints. The agency count measures directly capture market entries/exits by agencies.
Next, we explore whether our results are affected by time-varying market factors, such as changes in patient compositions, which are not controlled by the fixed-effects specification. We limit our analysis to a relatively homogenous group—patients with congestive heart failure, which is a common diagnosis for home health care (NCHS, 2007). If this analysis shows results consistent with the primary analysis, it would suggest that our finding is not largely driven by time-varying patient characteristics.
Finally, we estimate the model separately for hospital-discharged and community-based patients. Many home health admissions follow hospital discharges because Medicare mainly covers post-acute home health services. If hospitals have close relationships with specific agencies or own agencies, patients from such hospitals may be steered to certain agencies (by discharge planners), which would weaken the impact of competition on quality among hospital-discharged patients.
4. DATA
We utilize data of elderly fee-for-service Medicare beneficiaries who used home health services between 2001 and 2006. The primary data source is the Outcome and Assessment Information Set (OASIS), which contains records on health risk, functional status, and health service utilization of every home health patient. From OASIS data, we construct demand factors, quality indicators (functional improvements; discharges without hospitalization), agency size, and the number of home health users in a market.
The conditional choice model to construct predicted HHI is also estimated using OASIS data. To obtain reliable estimates in the choice model, we exclude records from zip codes with fewer than 10 patients and records from agencies with fewer than 10 patients. These exclusions remove 2.5% of the original sample.
The Medicare denominator and claims files (2001–2006) supply demographic and home health visit information. We obtain agency characteristics from the Provider of Services file and county characteristics from the Area Resource File.
5. RESULTS
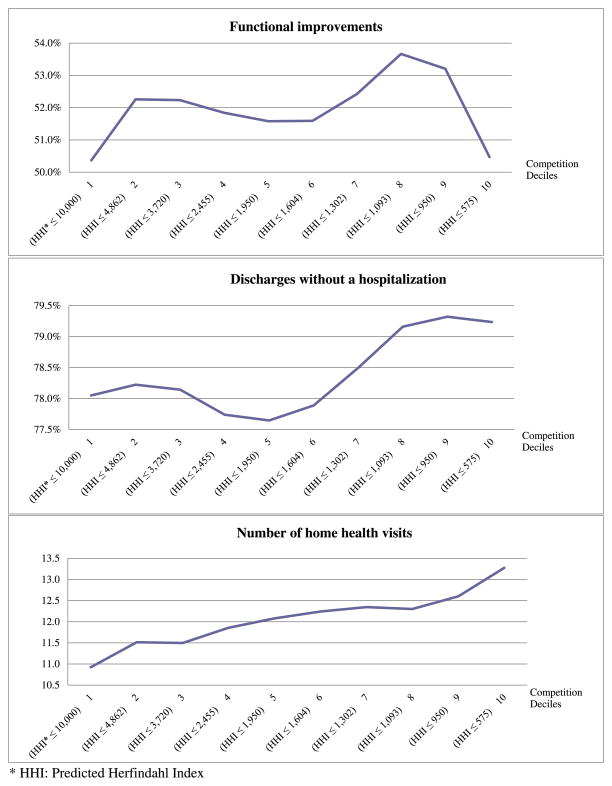
Figure 1 presents a relationship between average unadjusted quality scores and competition. Decile 1 represents the least competitive markets (HHI > 4,862) and decile 10 is the most competitive markets (HHI ≤ 575). For functional improvements, quality appears to increase with competition, but it falls sharply under intense competition and is the lowest in the most competitive markets. Performances in discharges without a hospitalization and the number of visits appear to be better in relatively competitive markets, but only the visit measure presents a unidirectional relationship with competition.
Figure 1.
Unadjusted quality scores by competition.
Table I reports descriptive statistics of all study variables. The study data consist of 12,244,537 home health episodes, and the table divides the data into three groups by the level of competition. The table indicates that highly competitive markets (HHI deciles 9 and 10) are different in several agency and market characteristics from other markets: those highly competitive markets tend to be urban areas and have a large number of hospital beds. A share of for-profit, free-standing, or newer agencies is larger in those markets than in other markets. Most agency entries/exits are observed in highly competitive markets.7 Over-time variability in HHI is also greater in those competitive markets (from 741.8 to 588.2 between 2001 and 2006; 21% decrease) than other markets (from 4,160.4 to 3,578.5; 14% decrease).8
Table I.
Descriptive statistics of study variables by the level of competition.
| Low competitiona (N = 1,127,179) |
Mid-range competition (N = 8,619,587) |
Intense competition (N = 2,497,771) |
||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Dependent variables | ||||||
| Functional improvements (%) | 50.37 | 0.32 | 52.23 | 0.32 | 51.84 | 0.32 |
| Discharges without hospitalization (%) | 78.05 | 0.41 | 78.19 | 0.41 | 79.28 | 0.41 |
| Number of home health visits | 10.92 | 8.22 | 11.98 | 8.89 | 12.94 | 8.98 |
| Competition measure | ||||||
| Predicted Herfindahl–Hirschman Index (HHI) | 6502 | 1363 | 2393 | 1025 | 585 | 247 |
| Explanatory variables | ||||||
| Age | 80.09 | 7.69 | 77.99 | 7.70 | 80.11 | 7.88 |
| Male | 0.36 | 0.48 | 0.35 | 0.48 | 0.35 | 0.48 |
| White | 0.96 | 0.21 | 0.87 | 0.34 | 0.75 | 0.43 |
| Medicaid buy-in status | 0.15 | 0.36 | 0.17 | 0.37 | 0.26 | 0.44 |
| Smoking | 0.07 | 0.25 | 0.06 | 0.24 | 0.05 | 0.22 |
| Drinking | 0.02 | 0.12 | 0.01 | 0.11 | 0.01 | 0.10 |
| Being obese | 0.16 | 0.36 | 0.13 | 0.34 | 0.12 | 0.33 |
| Cognitive problem | 0.37 | 0.48 | 0.36 | 0.48 | 0.41 | 0.49 |
| Vision impairment | 0.59 | 0.49 | 0.58 | 0.49 | 0.65 | 0.48 |
| Depression | 0.23 | 0.42 | 0.20 | 0.40 | 0.21 | 0.40 |
| Pain while walking at baseline | 1.30 | 1.04 | 1.21 | 1.04 | 1.32 | 1.00 |
| Shortness of breath at baseline | 1.23 | 1.15 | 1.22 | 1.14 | 1.39 | 1.13 |
| Incontinence at baseline | 0.44 | 0.57 | 0.42 | 0.57 | 0.45 | 0.57 |
| Dependency with bathing at baseline | 2.55 | 1.34 | 2.55 | 1.34 | 2.40 | 1.27 |
| Dependency with transferring at baseline | 0.85 | 0.81 | 0.95 | 0.87 | 1.06 | 0.91 |
| Dependency with ambulation at baseline | 1.25 | 0.91 | 1.33 | 0.96 | 1.38 | 0.99 |
| Dependency with taking medications at baseline | 0.83 | 0.78 | 0.84 | 0.79 | 0.88 | 0.79 |
| Having a caregiver | 0.82 | 0.39 | 0.85 | 0.36 | 0.86 | 0.34 |
| Behavioral problem | 0.39 | 1.26 | 0.45 | 1.35 | 0.50 | 1.40 |
| Hospital discharged | 0.60 | 0.49 | 0.56 | 0.50 | 0.47 | 0.50 |
| Distance | 10.36 | 15.16 | 12.56 | 15.18 | 11.95 | 12.12 |
| For profit agency | 0.12 | 0.32 | 0.37 | 0.48 | 0.73 | 0.44 |
| Facility-based | 0.52 | 0.50 | 0.31 | 0.46 | 0.12 | 0.33 |
| Branch operation | 0.33 | 0.47 | 0.40 | 0.49 | 0.24 | 0.43 |
| Number of Registered Nurse (RN) | ||||||
| RN 3–15 | 0.49 | 0.50 | 0.36 | 0.48 | 0.44 | 0.50 |
| RN >15 | 0.43 | 0.49 | 0.57 | 0.49 | 0.37 | 0.48 |
| Number of Licensed Practice Nurse | 0.16 | 0.37 | 0.34 | 0.48 | 0.35 | 0.48 |
| Number of aides | ||||||
| Aides 1–9 | 0.53 | 0.50 | 0.47 | 0.50 | 0.55 | 0.50 |
| Aides >9 | 0.32 | 0.47 | 0.38 | 0.48 | 0.16 | 0.36 |
| Medicare tenure | 22.92 | 10.48 | 20.23 | 11.01 | 11.12 | 9.51 |
| New entrants (<3 years) | 0.99 | 0.12 | 0.95 | 0.21 | 0.79 | 0.41 |
| Number of home health users | 47.82 | 63.09 | 99.33 | 113.2 | 206.63 | 200.48 |
| College educated (%) | 17.77 | 7.36 | 21.54 | 10.14 | 24.37 | 7.01 |
| Household median income ($1000) | 38.36 | 85.75 | 43.51 | 12.41 | 44.62 | 93.73 |
| Population age over 65 (%) | 15.38 | 3.61 | 13.17 | 3.44 | 11.41 | 4.48 |
| Rural (%) | 0.58 | 0.49 | 0.21 | 0.40 | 0.02 | 0.12 |
| Population density | 82.04 | 142.84 | 1092 | 4431 | 1685 | 1507 |
| Number of hospital beds/100 | 198.62 | 275.33 | 1309 | 2043 | 8434 | 9024 |
| Number of long-term facility beds/100 | 17.88 | 86.67 | 115.73 | 280.3 | 482.67 | 729.84 |
| Number of skilled nursing facility beds/100 | 407.72 | 470.11 | 2139.8 | 3070 | 11,340 | 13,504 |
| Number of nursing facilities beds/100 | 29.06 | 86.97 | 77.57 | 250.9 | 859.94 | 1373 |
| Number of patients per agency | 617.32 | 694.78 | 1757 | 4015 | 978.67 | 1111 |
| Agency entries/exits | ||||||
| Annual agency entries per zip | 0.01 | 0.10 | 0.12 | 0.42 | 1.57 | 2.92 |
| Annual agency exits per zip | 0.01 | 0.10 | 0.04 | 0.20 | 0.36 | 1.07 |
SD, standard deviation.
Low competition: predicted Herfindahl–Hirschman Index (HHI) decile 1 (HHI > 4862); mid-range competition: HHI deciles 2–8 (950 < HHI ≤ 4862); intense competition: HHI deciles 9 and 10 (HHI ≤ 950).
Table II reports the coefficients on competition from the fixed-effects regressions. For functional improvements, the decile approach indicates that the point estimates tend to increase as competition increases in relatively concentrated markets, but then fall steeply in highly competitive markets (deciles 9 and 10). Competition has a negative relationship with the non-hospitalization measure with the largest negative effects in the last two deciles, indicating the poorest outcomes in the most competitive markets. For the number of visits, competition has a positive effect in most ranges, but as in other measures, quality drops sharply in the most competitive markets. When the functional form of competition is restricted as linear, the regressions pick up the relationship only in the middle range in all measures and mask an important nonlinear relationship between competition and quality.
Table II.
Results from fixed effects regressions.
| Functional improvements
|
Discharges without a hospitalization
|
Number of visits
|
|
|---|---|---|---|
| (N = 10,332,027) | (N = 12,240,500) | (N = 11,937,168) | |
| Linear model | |||
| Competition (reversed HHIa) | 0.116** | −0.082** | 0.051*** |
| Nonlinear model (decile approach) | |||
| Competition deciles | |||
| Decile 1 (HHI ≤ 10,000)b | |||
| Decile 2 (HHI ≤ 4862) | 0.145 | 0.389*** | 0.028 |
| Decile 3 (HHI ≤ 3720) | 0.168 | 0.142 | 0.082** |
| Decile 4 (HHI ≤ 2455) | 0.145 | 0.045 | 0.148*** |
| Decile 5 (HHI ≤ 1950) | 0.422** | −0.354** | 0.272*** |
| Decile 6 (HHI ≤ 1604) | 0.191 | −0.407** | 0.236*** |
| Decile 7 (HHI ≤ 1302) | 0.462* | −0.498** | 0.206*** |
| Decile 8 (HHI ≤ 1093) | 0.319 | −0.927*** | 0.219*** |
| Decile 9 (HHI ≤ 950) | −0.453 | −1.526*** | 0.079 |
| Decile 10 (HHI ≤ 575) | −0.068 | −1.955*** | −0.057 |
| Three-category competition | |||
| Deciles 1–8 (HHI > 950)b | |||
| Decile 9 (HHI ≤ 950) | −0.806*** | −0.625*** | −0.147*** |
| Decile 10 (HHI ≤ 575) | −0.430** | −0.966*** | −0.290*** |
The values of Akaike information criterion (AIC) and Bayesian information criterion (BIC) measures are as follows: for functional outcomes, 4,445,822 and 4,446,388 for the linear model; 4,445,614 and 4,446,293 for the decile model; and 4,445,654 and 4,446,234 for the three-category model; for discharges without hospitalization, 7,986,837 and 7,987,393 for the linear model; 7,986,706 and 7,987,374 for the decile model; 7,986,745 and 7,987,315 for the three-category model; and for the number of visits, both AIC and BIC are 58,000,000 in all models.
Reversed HHI: predicted Herfindahl–Hirschman Index (HHI) values are subtracted from 10,000.
Reference group.
p < 0.10;
p < 0.05;
p < 0.01.
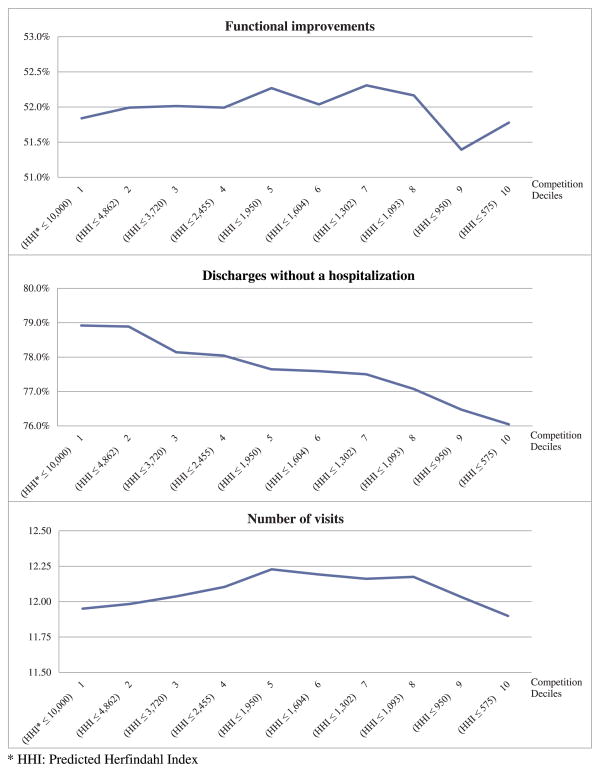
The patterns indicated by the coefficients from the nonlinear models can be easily seen in Figure 2, which displays the predicted values of quality scores. The figure shows that when competition becomes very intense (deciles 9 and 10; HHI ≤ 950), it puts large, downward pressure on quality for all three measures. The drop in the coefficients in these deciles is significant compared with other deciles for all measures (the bottom panel of Table II). This may be that the ease of exit makes exit a more viable option than investing in quality in very competitive markets.
Figure 2.
Predicted quality scores from fixed effects models by competition.
We examine the magnitude of competition effects on the basis of the results on deciles 9 and 10 where the competition effect is strong. Estimated effects of intense competition on quality are very small: The probability of improving functional status decreases by 0.43–0.81 percentage points in deciles 9 and 10 (HHI ≤ 950), compared with other markets. This effect is only 0.83–1.55% of the average functional improvements score (51.98%). For discharges without a hospitalization, there is a 0.63–0.97% point decrease in deciles 9 and 10 (HHI ≤ 950), compared with other markets, which corresponds to 0.80–1.21% of the mean value of the measure (78.3%). Finally, 0.3 fewer visits are offered in the most competitive markets than other markets (2.25% of the mean visits).
Results on other explanatory variables are generally consistent with basic expectations (Table AI). Health risk factors (smoking, drinking) and poor health status (e.g., depression) have negative effects on quality for all measures. Poorer functional status at baseline (e.g., having difficulty in transferring) has negative effects on functional improvements but results in more visits.
Table AI.
Regression results
| Variables | Functional improvements
|
Discharges without a hospitalization
|
Number of visits
|
|||
|---|---|---|---|---|---|---|
| (N = 10,332,027)
|
(N = 12,240,500)
|
(N = 11,937,168)
|
||||
| Without fixed effects | With fixed effects | Without fixed effects | With fixed effects | Without fixed effects | With fixed effects | |
| Competition | ||||||
| Decile 1 (HHI ≤ 10,000) | ||||||
| Decile 2 (HHI ≤ 4862) | 1.311 | 0.145 | −0.263 | 0.389 | 0.552 | 0.028 |
| Decile 3 (HHI ≤ 3720) | 1.330 | 0.168 | −0.442 | 0.142 | 0.520 | 0.082 |
| Decile 4 (HHI ≤ 2455) | 1.013 | 0.145 | −0.948 | 0.045 | 0.847 | 0.148 |
| Decile 5 (HHI ≤ 1950) | 1.102 | 0.422 | −0.702 | −0.354 | 0.880 | 0.272 |
| Decile 6 (HHI ≤ 1604) | 0.723 | 0.191 | −0.773 | −0.407 | 0.939 | 0.236 |
| Decile 7 (HHI ≤ 1302) | 1.621 | 0.462 | −0.435 | −0.498 | 0.948 | 0.206 |
| Decile 8 (HHI ≤ 1093) | 2.156 | 0.319 | −0.442 | −0.927 | 1.108 | 0.219 |
| Decile 9 (HHI ≤ 950) | 2.244 | −0.453 | −0.401 | −1.526 | 1.620 | 0.079 |
| Decile 10 (HHI ≤ 575) | 1.556 | −0.068 | 0.682 | −1.955 | 2.160 | −0.057 |
| Age | −0.400 | −0.396 | 0.086 | 0.079 | −0.008 | −0.009 |
| Male | 1.522 | 1.462 | −2.829 | −2.992 | −0.297 | −0.247 |
| White | 0.044 | 0.513 | 1.345 | 0.706 | −0.159 | −0.202 |
| Medicaid buy-in status | −3.564 | −3.432 | −1.291 | −1.459 | −0.505 | −0.468 |
| Smoking | −1.687 | −1.641 | −1.560 | −1.376 | −0.249 | −0.261 |
| Drinking | 1.426 | 1.363 | 1.431 | 1.271 | −0.139 | −0.065 |
| Being obese | −3.937 | −3.882 | 0.435 | 0.443 | 0.639 | 0.680 |
| Cognitive problem | −3.827 | −3.683 | 0.048 | 0.111 | −0.253 | −0.294 |
| Vision impairment | −2.608 | −2.501 | −0.773 | −0.650 | 0.498 | 0.462 |
| Depression | −1.658 | −1.552 | −3.378 | −3.432 | 0.522 | 0.491 |
| Pain while walking | 2.689 | 2.747 | 0.253 | 0.161 | 0.263 | 0.268 |
| Shortness of breath | 1.431 | 1.499 | −4.331 | −4.203 | 0.198 | 0.149 |
| Incontinency | −1.844 | −1.640 | −2.821 | −2.742 | 0.190 | 0.169 |
| Dependency in bathing | 2.026 | 2.036 | −0.769 | −0.794 | 0.800 | 0.840 |
| Dependency in transferring | −2.463 | −2.515 | −1.458 | −1.439 | 0.391 | 0.365 |
| Dependency with ambulation | 0.525 | 0.437 | −1.582 | −1.718 | 0.521 | 0.561 |
| Dependency in taking medications | −2.975 | −2.963 | −3.015 | −3.100 | 0.405 | 0.446 |
| Having a caregiver | −0.609 | −0.739 | 0.249 | 0.121 | −0.110 | −0.086 |
| Behavioral problem | −0.519 | −0.509 | 0.066 | 0.070 | −0.203 | −0.199 |
| Hospital discharged | 7.919 | 7.889 | −2.661 | −2.620 | −1.176 | −1.106 |
| Distance | −0.004 | −0.008 | 0.011 | 0.010 | −0.008 | −0.007 |
| For profit agency | −0.449 | −0.581 | −0.539 | −0.603 | 0.563 | 0.519 |
| Facility-based | 0.318 | 0.726 | 0.323 | 0.250 | −0.289 | −0.324 |
| Branch operation | −0.549 | −0.337 | −0.132 | −0.040 | −0.020 | −0.094 |
| Agency size (Number of patients) | ||||||
| 300–1000 | 2.536 | 2.016 | 2.269 | 1.346 | −0.599 | −0.370 |
| >1000 | 3.686 | 2.719 | 3.386 | 2.030 | −1.092 | −0.676 |
| Number of Registered Nurse | ||||||
| 3–15 | 0.515 | 0.300 | −0.458 | −0.445 | 0.028 | −0.013 |
| >15 | 0.597 | 0.334 | −1.179 | −0.930 | 0.209 | 0.016 |
| Number of Licensed Practice Nurse | −0.823 | −0.326 | −0.357 | −0.490 | 0.083 | 0.160 |
| Number of aides | ||||||
| 1–9 | −0.472 | −0.564 | −0.917 | −0.598 | 0.350 | 0.307 |
| >9 | −0.795 | −1.024 | −2.162 | −0.856 | 0.944 | 0.548 |
| Medicare tenure | −0.030 | −0.020 | −0.038 | −0.008 | −0.017 | −0.026 |
| New entrants (<3 years) | −0.186 | 0.107 | −0.310 | −0.458 | −0.105 | 0.064 |
| Year 2 | −0.287 | −0.001 | −1.055 | −0.526 | 0.120 | 0.188 |
| Year 3 | 1.293 | 1.644 | −1.033 | −0.419 | −0.148 | 0.000 |
| Year 4 | 3.029 | 3.480 | −1.028 | −0.275 | −0.354 | −0.153 |
| Year 5 | 4.142 | 4.758 | −0.707 | 0.135 | −0.244 | −0.032 |
| Year 6 | 6.250 | 6.696 | 0.474 | 1.099 | −0.288 | −0.077 |
| Number of home health users in a zip | 0.000 | 0.000 | 0.001 | 0.000 | 0.000 | 0.000 |
| College educated (%) | −0.048 | – | 0.068 | – | −0.002 | – |
| Median income | 0.000 | – | 0.000 | – | 0.000 | – |
| Population age over 65 years | 0.135 | – | 0.095 | – | −0.007 | – |
| Rural area | −0.796 | – | −1.294 | – | 0.194 | – |
| Population density | 0.000 | – | 0.000 | – | 0.000 | – |
| Hospital beds/100 | 0.000 | – | 0.001 | – | 0.000 | – |
| LTC facility beds/100 | 0.001 | – | 0.000 | – | 0.000 | – |
| SNF beds/100 | 0.000 | – | 0.000 | – | 0.000 | – |
| Nursing facilities beds | 0.000 | – | 0.000 | – | 0.000 | – |
| Constant | 69.435 | 74.082 | 86.752 | 90.881 | 9.324 | 9.731 |
HHI: predicted Herfindahl–Hirschman Index; decile 1 is the reference group.
p < 0.10;
p < 0.05;
p < 0.01.
For comparison purposes, we report the results from the regressions without fixed effects (Table AI). The results indicate a strong unidirectional association between competition and quality in all three measures, suggesting that time-invariant market factors correlated with both competition and quality are omitted in these regressions.
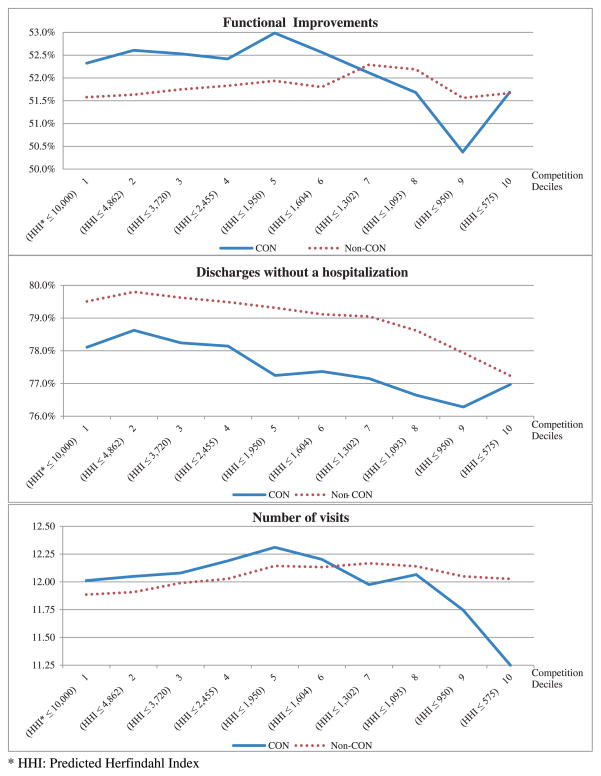
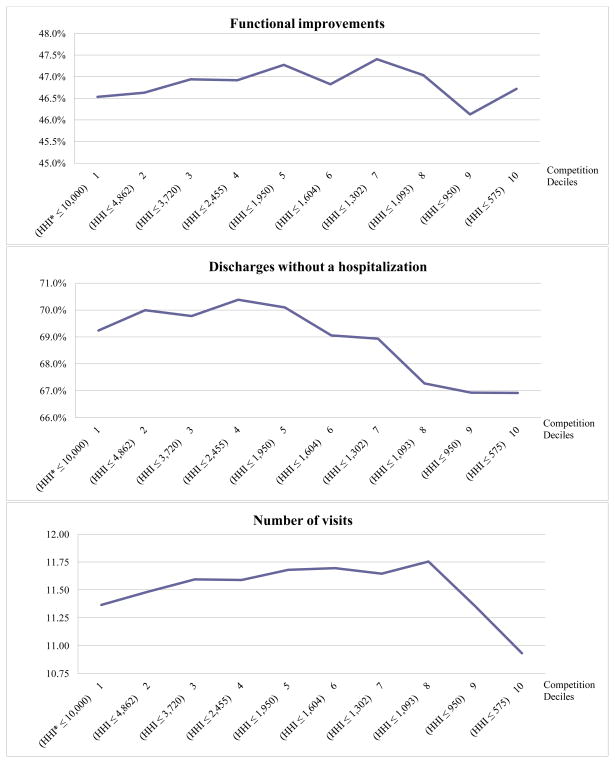
Table III reports the results from separate analysis by CON status (fixed-effects models). The overall pattern of the results is consistent with the primary analysis. The coefficients on competition deciles in the functional improvements and visit models are mostly positive in both groups, except those on deciles 9 and 10 in CON states. The model of discharges without a hospitalization presents negative coefficients on most deciles with the largest coefficients on deciles 9 or 10 in both groups. The negative coefficients are generally larger in the analysis of CON states when compared to non-CON states. This indicates a more rapid deterioration of quality when entry is restricted by CON, suggesting that ease of exit plays a role in reducing home health quality.
Table III.
Regression results by Certificate of Need (CON) status (fixed-effects models)
| N | Functional improvements
|
Discharges without hospitalization
|
Number of visits
|
|||
|---|---|---|---|---|---|---|
| CON statesa
|
Non-CON states
|
CON states
|
Non-CON states
|
CON states
|
Non-CON states
|
|
| 3,522,989 | 6,809,038 | 4,194,566 | 8,045,944 | 4,081,468 | 7,855,700 | |
| Decile approach | ||||||
| Competition deciles | ||||||
| Decile 1 (HHI ≤ 10,000)b | ||||||
| Decile 2 (HHI ≤ 4862) | 0.282 | 0.057 | 0.517*** | 0.290** | 0.037 | 0.022 |
| Decile 3 (HHI ≤ 3720) | 0.207 | 0.171 | 0.133 | 0.115 | 0.068 | 0.104** |
| Decile 4 (HHI ≤ 2455) | 0.093 | 0.253 | 0.034 | −0.021 | 0.177** | 0.141** |
| Decile 5 (HHI ≤ 1950) | 0.662** | 0.359 | −0.862*** | −0.194 | 0.299*** | 0.258*** |
| Decile 6 (HHI ≤ 1604) | 0.239 | 0.222 | −0.741** | −0.393 | 0.191* | 0.247*** |
| Decile 7 (HHI ≤ 1302) | −0.209 | 0.711** | −0.957*** | −0.460* | −0.037 | 0.282*** |
| Decile 8 (HHI ≤ 1093) | −0.642 | 0.612* | −1.463*** | −0.890*** | 0.054 | 0.254*** |
| Decile 9 (HHI ≤ 950) | −1.950*** | −0.016 | −1.824*** | −1.573*** | −0.267* | 0.164* |
| Decile 10 (HHI ≤ 575) | −0.636 | 0.092 | −1.138** | −2.272*** | −0.762*** | 0.141 |
| Three-category competition | ||||||
| Deciles 1–8 (HHI ≤ 1093)b | ||||||
| Decile 9 (HHI ≤ 950) | −1.335*** | −0.677*** | −0.379* | −0.703*** | −0.304*** | −0.109*** |
| Decile 10 (HHI ≤ 575) | 0.049 | −0.615*** | 0.379 | −1.304*** | −0.791*** | −0.144*** |
CON states are AL, AK, AR, GA, HI, KY, MD, MS, MT, NJ, NY, CA, SC, TN, VT, WA, WV, and DC.
HHI: predicted Herfindahl–Hirschman Index; decile 1 is the reference group.
p < 0.10;
p < 0.05;
p < 0.01.
Figure 3 shows the predicted values of quality scores from these models. Non-CON states have better functional outcomes and more visits than CON states in relatively competitive markets and have higher rates of discharges without a hospitalization in all ranges of competition. CON states show a steeper downward slope than non-CON states in relatively competitive markets for all quality measures. Although very intense competition (decile 10) appears to place slightly upward pressure on functional improvements in CON states, this hike is not significant compared with other deciles (the bottom panel of Table III).
Figure 3.
Predicted quality scores by competition by Certificate of Need (CON) status.
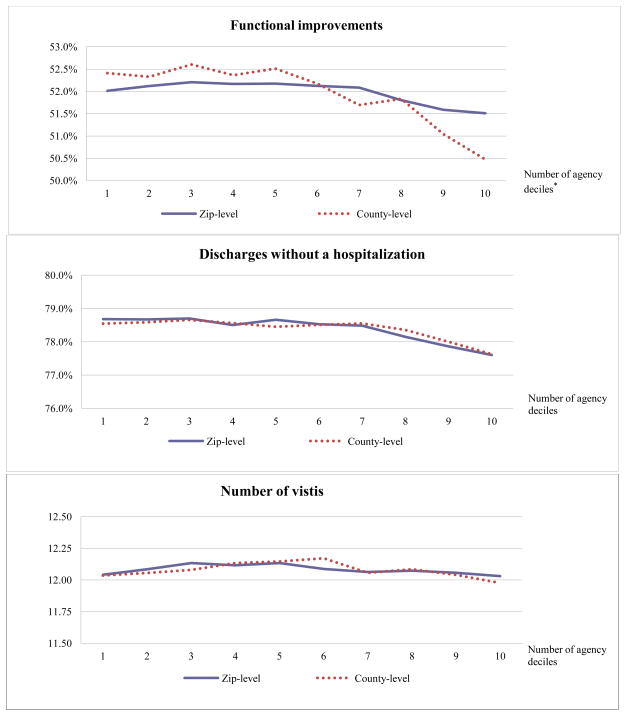
6. ROBUSTNESS CHECKS
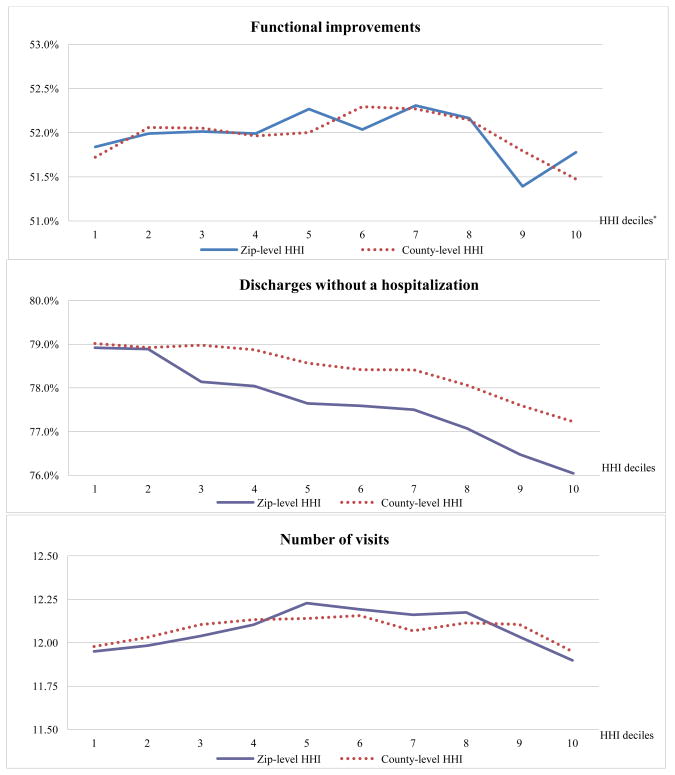
We estimate the model using other competition measures that better isolate agency entries/exits: county-level HHI and the number of agencies at zip code and county levels. The results from these analyses are consistent with the primary analysis (Figures S1 and S2): Competition has a nonlinear relationship with quality with a sharp fall in quality under intense competition. The estimated effects of competition on quality based on these alternative measures are slightly weaker than those from the primary analysis, possibly because alternative measures do not capture variation in competition from the changes in patient shares across market areas.
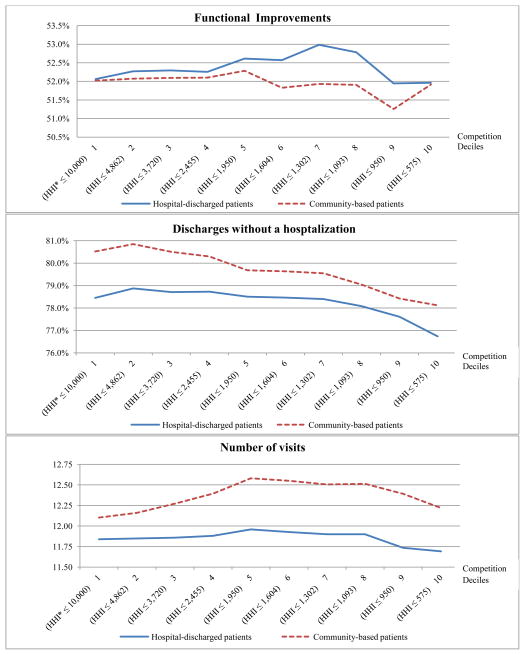
The results from other sensitivity analyses also confirm our finding in the primary analysis. The analysis with congestive heart failure patients shows a clear nonlinear relationship between competition and quality in all quality measures, suggesting that our finding is not driven by the over-time changes in patient compositions (Figure S3). The pattern of the competition effect from both analyses of hospital-discharged and community-based patients is also consistent with the overall analysis, implying that our finding is not influenced by possible hospital-agency relationships (Figure S4).
7. DISCUSSION AND CONCLUSION
Promotion of provider competition has been an important element of health care policies. Antitrust laws have been applied to hospital and health insurance markets, and models of managed competition have been adopted in several settings. Recently, market-based quality initiatives (e.g., public reporting or P4P programs) have expanded in several settings. Given this trend, empirical evidence on the effect of competition on quality in diverse settings is essential. Analyzing Medicare home health care markets, we report three findings:
First, we found a nonlinear relationship between competition and home health quality: When competition becomes intense, quality sharply dropped in all measures. Although small, this negative effect of competition on quality suggests that the ease of exit may restrict the ability of competition to improve quality in home health care markets; however, this possibility is limited to highly competitive markets where there may have been many easy entries and where exits are likely to be a viable option.
Second, the separate analysis by CON status indicates a slightly stronger negative effect of competition on quality in CON states than in non-CON states. This finding supports the importance of considering the ease of exits as a factor regarding the relationship between competition and home health quality.
Third, the effect of competition on quality in most ranges of competition (other than in markets with very intense competition) differed by quality measure. The number of visits increased as competition increases whereas discharges without a hospitalization decreased with competition. This suggests that agencies may focus on certain aspects of quality that are easily assessable by patients to attract patients as competition increases. Or it could be that resource requirement to help patients avoid hospitalizations may be greater than what is needed to improve other quality measures, which may lead some agencies to choose to exit under competition.
Our finding is different from the prior literature in hospital markets, and a negative relationship of intense competition to quality is counterintuitive. This is likely to be due to the unique feature in home health care–service delivery in patients’ homes. Thus, market entry does not require large capital investments, and some agencies may easily enter any profitable market and then simply leave the market if they are unable to attract consumers under competition. These low-cost entrants are likely to lack technical capacity to compete over and invest in quality (Bishop et al., 1999). We may see this effect in the most competitive markets because there is less of a threat from entry when an abundance of firms is already in the marketplace. It is also possible that agencies in highly competitive markets may be unable to hire/retain high-quality nurses, which are the key input of home health care, because of the limited workforce supply of the market.
Given the unique service delivery model of home health care, it is not surprising that the prior findings in hospital markets did not completely translate to this market. What is surprising is that prior to this paper, there had been no assessment of how competition affects home health quality. It may have been assumed that experience in other settings would apply to home health care, but our finding suggests that market-specific features need to be considered in assessing whether competition is a useful policy instrument to promote quality. More evidence is necessary to guide the development of market-based policies that would be appropriate to home health care.
Interpretation of findings should incorporate important limitations. First, competition may have occurred over other dimensions in those markets than the quality measures we used; for example, agencies under intense competition may offer longer time or better quality visits than those serving less competitive markets. Although such resource use may not have improved patients’ health outcomes, it may have increased patient satisfaction or comfort. Second, the fixed-effects analysis does not control for time-varying factors that affect both competition and patients’ health outcomes. Although the analysis of a relatively homogenous population shows that our results are unlikely to be greatly influenced by unmeasured case mix, it is still possible that agencies facing increasing competition may have treated sicker patients than agencies with little change in competition. Third, functional improvements and hospitalization-avoided measures were constructed from assessment data, which are coded by home health staff and thus are subject to measurement/reporting errors. However, the consistent results from the analysis of the visit measure, which is obtained from the claims data, suggest that this possibility is unlikely. Further, because we controlled for time-constant factors through fixed effects, measurement errors would influence our results only if the changes in those errors were related to competition.
In summary, our study is the first to assess the relationship between competition and home health quality. We report different results than studies on hospital markets. The finding of small but negative effects of competition calls for future research to investigate mechanisms behind the results. Further evaluation of and more evidence on how home health care markets function are essential to guide the development of policies to improve quality.
Acknowledgments
We thank Jianing Yang and Michael Harhay for assistance with data preparation. We are grateful to seminar participants at University of Pennsylvania and American Society of Health Economists conference for their helpful comments. This work is supported by NIH/NHLBI grant # R01 HL088586-01 and NIH/NIA grant # 1R03AG035098-01.
APPENDIX
Figure A1.
Predicted quality scores from fixed effects models using Herfindahl Index
* HHI: Predicted Herfindahl Index;
Zip-level and county-level cut-off values are: HHI ≤ 10,000 and HHI ≤ 10,000 (decile 1), HHI ≤ 4,862 and HHI ≤ 4,168 (decile 2), HHI ≤ 3,720 and HHI ≤ 3,043 (decile 3), HHI ≤ 2,455 and HHI ≤ 2,364 (decile 4), HHI ≤ 1,950 and HHI ≤ 1,822 (decile 5), HHI ≤ 1,604 and HHI ≤ 1,399 (decile 6), HHI ≤ 1,302 and HHI ≤ 1,066 (decile 7), HHI ≤ 1,093 and HHI ≤ 835 (decile 8), HHI ≤ 950 and HHI ≤ 585 (decile 9), and HHI ≤ 575 and HHI ≤ 306 (decile 10).
Figure A2.
Predicted quality scores from fixed effects models using number of agencies
* Zip-level and county-level cut-off values are: N ≤ 3 and N ≤ 7 (decile 1), N ≤ 4 and N ≤ 10 (decile 2), N ≤ 5 and N ≤ 14 (decile 3), N ≤ 6 and N ≤ 18 (decile 4), N ≤ 7 and N ≤ 24 (decile 5), N ≤ 8 and N ≤ 31 (decile 6), N ≤ 11 and N ≤ 40 (decile 7), N ≤ 14 and N ≤ 56 (decile 8), N ≤ 19 and N ≤ 122 (decile 9), and N ≤ 58 and N ≤ 378 (decile 10).
Figure A3.
Predicted quality scores for hospital-discharged and community-based patients
* HHI: Predicted Herfindahl Index
Figure A4.
Predicted quality scores from analysis of patients with congestive heart failure
* HHI: Predicted Herfindahl Index
Footnotes
Supporting information may be found in the online version of this article.
Agencies may have other revenue sources but we focus on Medicare patients because Medicare is the major revenue source (National Center for Health Statistics, 2007).
Medicare covers home health services used for rehabilitation or recovery during a limited time period. Another type of care includes non-medical and home-making services, which require long-term attention. These services are not covered by Medicare without concurrent prescriptions of skilled nursing services.
CON-regulated states are AL, AK, AR, CA, GA, HI, KY, MD, MS, MT, NJ, NY, SC, TN, VT, WA, WV, and DC.
It might be possible that over-time changes in competition—market entry/exit—were endogenous quality, which is not controlled for by the use of predicted market shares and market fixed effects. For example, agencies might have strategically entered or exited a market on the basis of market quality during the study period as markets slowly adjusted to the payment change made in 2000. To explore this possibility, we examined descriptive data of whether/how the degree of market entry/exit was related to market quality, but did not find that any systematic pattern between the degree of entry/exit and quality, which leads us to discount that possibility.
While home health patients do not need to travel, they may still choose an agency on the basis of distance, considering distance as a marker representing agency staff’s responsiveness to their needs. Home health care provision is a local activity involving nurses’ visits to patients’ homes. It is thus important for nurses to understand demand from the local community, and nurses employed by close agencies may better respond to patient demand in the community. Further, close agencies may offer services in a more timely fashion and more frequently than distant agencies. Our data indicate that 90% of patients chose an agency within 30 miles from their residence.
We estimate the choice model for each year to capture over-time variation in competition and for each state to reduce computational burdens. Each patient’s choice set includes all agencies serving the zip code of the patient’s residence in a given year. Variables included in the choice model are distance (decile indicators), agency attributes, and interactions between distance indicators and agency attributes.
These highly competitive markets tend to concentrate in several states. More than 30% of those markets are in four states (CA, FL, IL, and TX) that experienced large expansion of the home health care industry during the study period. We analyzed our model separately for these four states and all other states, but found that the results from both groups were consistent with the primary analysis (data not shown but available upon request).
The average HHI in all markets changed from 2,891.4 to 2,244.8.
CONFLICT OF INTEREST
No conflicts of interest exist.
References
- Akerlof GA. The market for “lemons”: quality uncertainty and the market mechanism. Quarterly Journal of Economics. 1970;84(3):488–500. [Google Scholar]
- Bishop CE, Kerwin J, Wallack S. The Medicare home health benefit: implications of recent payment changes. Care Management Journals. 1999;1(3):1–7. [PubMed] [Google Scholar]
- Chen Q, Kane RL, Finch M. –2001. The cost effectiveness of post-acute care for elderly Medicare beneficiaries. Inquiry. 2000;37(4):359–375. [PubMed] [Google Scholar]
- Chou S. Asymmetric information, ownership and quality of care: an empirical analysis of nursing homes. Journal of Health Economics. 2002;21:293–311. doi: 10.1016/s0167-6296(01)00123-0. [DOI] [PubMed] [Google Scholar]
- Gaynor M. National Bureau of Economic Research Working Paper No 12301. 2006. What do we know about competition and quality in health care markets? [Google Scholar]
- Han B, McAuley WJ, Remsburg RE. Agency ownership, patient payment source, and length of service in home care. The Gerontologist. 2007;47(4):438–446. doi: 10.1093/geront/47.4.438. [DOI] [PubMed] [Google Scholar]
- Hirth RA. Consumer information and competition between nonprofit and for-profit nursing homes. Journal of Health Economics. 1999;18:219–240. doi: 10.1016/s0167-6296(98)00035-6. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. The National Academies Press; Washington DC: 2001. [PubMed] [Google Scholar]
- Jung K, Shea D, Warner C. Agency characteristics and quality improvement after home health compare. Journal of Aging and Health. 2010;22(4):454–476. doi: 10.1177/0898264310362540. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. Medicare: a primer 2009. 2009 Available from: http://www.kff.org.
- Kessler DP, Geppert JJ. The effects of competition on variation in the quality and cost of medical care. Journal of Economics and Management Strategy. 2005;14(3):575–589. [Google Scholar]
- Kessler DP, McClellan M. Is hospital competition socially wasteful? Quarterly Journal of Economics. 2000;115(2):577–615. [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. The National Academies Press; Washington DC: 1999. [PubMed] [Google Scholar]
- Konetzka T, Spector W, Limcangco MR. Reducing hospitalizations from long-term care settings. Medical Care Research and Review. 2008;65(1):40–66. doi: 10.1177/1077558707307569. [DOI] [PubMed] [Google Scholar]
- Levine SA, Boal J, Boling PA. Home care. Journal of the American Medical Association. 2003;290:1203–1207. doi: 10.1001/jama.290.9.1203. [DOI] [PubMed] [Google Scholar]
- Maryland Health Care Commission. An analysis and evaluation of Certificate of Need regulation in Maryland: phase I final report. Baltimore, MD: 2001. [Google Scholar]
- McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. The New England Journal of Medicine. 2003;348:2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission. Report to the Congress: Medicare payment policy. 2008 Available from: www.medpac.gov/documents/mar08_entirereport.pdf [January 17, 2011]
- Murtaugh C, Peng T, Aykan H, Maduro G. Risk adjustment and public reporting on home health care. Health Care Financing Review. 2007;28(3):77–94. [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. National home and hospice care survey. 2007 Available from: http://www.cdc.gov/nchs/nhhcs.htm [January 17, 2010]
- Porell FW, Liu K, Brungo DP. Agency and market area factors affecting home health agency supply changes. Health Services Research. 2006;41(5):1847–1875. doi: 10.1111/j.1475-6773.2006.00561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scalzi C, Zinn J, Guilfoyle M, Perdue S. Medicare-certified home health services: national and regional supply in the 1980s. American Journal of Public Health. 1994;84(10):1646–1648. doi: 10.2105/ajph.84.10.1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen YS. The effect of financial pressure on the quality of care in hospitals. Journal of Health Economics. 2003;22(2):243–269. doi: 10.1016/S0167-6296(02)00124-8. [DOI] [PubMed] [Google Scholar]
- Tay A. Assessing competition in hospital care markets: the importance of accounting for quality differentiation. The RAND Journal of Economics. 2003;34(4):786–814. [PubMed] [Google Scholar]
- Welch HG, Wennberg DE, Welch WP. The use of Medicare home health care services. The New England Journal of Medicine. 1996;33(5):324–329. doi: 10.1056/NEJM199608013350506. [DOI] [PubMed] [Google Scholar]