Abstract
Objective
To assess the direct annual health care costs for children and adolescents with Down syndrome in Western Australia and to explore the variation in health care utilisation including respite, according to age and disease profile.
Study design
Population-based data were derived from a cross sectional questionnaire which was distributed to all families who had a child with Down Syndrome up to 25 years of age in Western Australia.
Results
Seventy-three percent of families (363/500) responded to the survey. Mean annual cost was $4,209 AUD ($4,287 USD) for direct health care including hospital, medical, pharmaceutical, respite and therapy with a median cost of $1,701. Overall, costs decreased with age. The decline in costs was a result of decreasing utilisation of hospital, medical and therapy costs with age. Conversely, respite increased with age and also with dependency. Health care costs were greater in all age groups with increasing dependency and for a previous or current diagnosis of congenital heart disease. Annual health care costs did not vary by parental income, including cost of respite.
Conclusions
Direct health care costs for children with Down syndrome decrease with age to approximate population costs, although costs of respite show an increasing trend.
Keywords: Down syndrome, direct health care costs, health care utilisation
Although cognitive impairment in children and adults with intellectual disability affects every day functioning, for many individuals health profiles are unremarkable. In contrast, the effects of Down syndrome involve a range of medical conditions including intellectual disability which may be identified at birth or develop over the life span.1,2 There have been considerable improvements in medical and surgical management, particularly of the early identified co-morbidities, leading to increased infant, child3 and adult survival4 overall although ethnic disparities still persist.3,5 Changes in clinical practice along with changes in attitudes to the management of children with disabilities also appears to lead to benefits for ongoing health with likely better quality of life for those affected and their families. Nevertheless the medical burden associated with Down syndrome is not trivial and the use at least of hospital services has been shown to be greater than for the equivalent general population.1,6
Down syndrome is the commonest known cause of intellectual disability with a live birth prevalence approaching 1 per 1000 births7 in Western Australia (WA) which is consistent with data from other developed countries.8 Although the birth prevalence in WA has remained fairly stable over time, changes in epidemiology have occurred with an increase in Down syndrome conceptions associated with overall increase in maternal age balanced by an increase in prenatal screening, diagnosis and terminations of affected pregnancies. Worldwide there continues to be variation in the birth prevalence of Down syndrome associated with availability of prenatal screening in addition to legislation, socio-cultural and religious attitudes to termination.1
Despite recognized demands on the health care system, few studies have reported the health costs for children with this condition. One study from the U.S. reported the health care costs for children with Down syndrome was up to 13 times higher than for children without Down syndrome9. However costs were reported only for children who were members of a health insurance organisation, which may represent a more highly serviced group. A study of adolescents in Denmark demonstrated that health costs for Down syndrome individuals were just under twice that of controls.10
The aim of this study was to explore the health costs for Down syndrome throughout childhood and adolescence by comparing data from a cross-sectional survey of health resource utilisation for individuals with Down syndrome with age specific population data. Costs are presented as mean costs per year to provide information on total resource needs for this group and hence to understand the total resource needs in relation to age. Costs are also presented as median costs to better reflect the typical health resource needs for a child with Down syndrome. Costs are of interest in relation to age-adjusted mean population costs and previously reported costs, and provide important data for the evaluation of cost-effectiveness of treatments for this group. This information is also useful for policy makers to effect change and to make adequate provision for individuals with Down syndrome.
Methods
Children with Down syndrome aged less than 25 years in 2004 were identified from the IDEA (Intellectual Disability Exploring Answers) database, a population-based register of children with intellectual disability in WA.11 With the approval of the Ethics Committee of the Women and Children Health Services in WA and the backing of the parent support group ‘Down Syndrome WA’, families of all 500 children/young adults with Down syndrome registered with the Disability Services Commission and able to be contacted were invited to participate in a cross-sectional survey. Preliminary pilot testing ensured that the questionnaire was relevant and captured important resource, health, functional and family characteristics while being sensitive to the complexity of ongoing care-giving demands. Information was sought to describe the demographics, associated health conditions and direct health care costs attributable to families with a child with Down syndrome. Health resource needs included hospital, medical, pharmaceutical, community and respite care throughout the previous year. Hours or days of respite were based on the care provided to families as reported by them to the study. Information included the number of hours, the frequency and the providing agency and was separated according to overnight or day care. Data collection was completed during 2005. Three quarters of families completed the questionnaire on paper, 12.6% online, and 12.4% by telephone interview. None of the children among the respondent families were living in an institution.
Measurement of independent functioning in this group has been published previously12 using a modified version of the WeeFIM.13 The WeeFIM consists of questions concerning 18 tasks in six domains of functioning - self-care (feeding, grooming, dressing and bathing), sphincter control (maintaining continency), transfers, locomotion, communication and social cognition. For each task, parents were asked to tick one box and one sub-box next to the statements that best matched their child’s level of competency at the task. Answers were scored (with the highest possible score on each question being 7) for a maximum total score of 126.
Costs
Resource items were calculated according to survey results reported by the family, computed to units per year and costed according to the unit price in Australian dollars in 2009. Costs were adjusted where necessary using Australian health index deflators.14 Australian dollars are roughly at parity with US dollars. ($1AUD equals $1.02 USD). Medical and dental costs were derived from the Medical Benefit Schedule. Therapy services and paid Home and Community Care services were based on data from the Disability Services Commission (DSC) and included short and long term respite care. Hospital admission costs were based on a mean bed day cost in 2008.15 Costs for medications were derived from the Schedule of Pharmaceutical Benefits. Complementary medicines, non-durable health-related products and therapeutic devices were based on expenditure provided by the parents. Costs were calculated from the health system perspective and therefore do not generally reflect out of pocket costs to the families.
Statistical Methods
Costs were presented as both mean cost per person – to represent the total cost burden, and as median cost – to represent the likely expected cost for an individual. The total costs for different groups of individuals with Down syndrome were compared using non-parametric methods to account for the highly non-normal distribution of costs within groups. Linear regression was used to predict differences resulting from single-point increases in continuous measures such as the WeeFIM.
Results
Of the 500 families invited to participate, 363 (73%) families completed the survey. The age of the affected individuals ranged from 0 to 24 years with a mean age of 12.3 years and a median age of 13 years (Table I). Forty-four percent were females and 56% males which is representative of the sex ratio for Down syndrome overall.16 Three quarters of the families resided in the metropolitan area. Two individuals were excluded from the cost analysis due to lack of information (n=361).
Table 1.
Total annual health care costs for individuals with Down syndrome, by age and area of expenditure
| Age group | Subjects | Total mean health care cost (median) | Total mean cost of hospital care (median) | Total mean cost of medical care (GP and Specialist) (median) | Total mean cost of pharmaceutical care (median) | Total ‘other costs’ (median) | |
|---|---|---|---|---|---|---|---|
| M | F | ||||||
| 0-4 n = 58 | 29 | 29 | $8491 ($6199) | $3450 ($1282) | $695 ($621) | $126 ($36) | $4219 ($126) |
| 5- 9 n = 75 | 40 | 35 | $4207 ($2468) | $762 ($36) | $660 ($553) | $189 ($46) | $2595 ($189) |
| 10 - 14 n = 86 | 51 | 35 | $3048 ($1262) | $1040 ($0) | $504 ($348) | $88 ($13) | $1416 ($88) |
| 15-19 n = 81 | 45 | 36 | $2687 ($798) | $450 ($17) | $426 ($323) | $87 ($10) | $1724 ($87) |
| 20-24 n = 61 | 39 | 22 | $3798 ($569) | $2001 ($0) | $393 ($267) | $113 ($20) | $1290 ($113) |
| Total n = 361 | 204 | 157 | $4209 ($1701) | $1400 ($35) | $531 ($416) | $119 ($24) | $2159 ($119) |
All costs reported in $AUD2009
A description of the medical conditions has recently been reported.2 Forty five percent were reported to have ever had a heart condition. Other commonly reported conditions, were eye (most common), ear, and respiratory problems, although some of these, particularly heart conditions, were no longer ongoing.
The total mean annual health care costs across all age groups was $4,209, with a median of $1,701 and a standard deviation $6,705 (Table I). This skewed distribution occurs with most disease costs - almost half the total costs (46%) were accounted for by 10% individuals. Total cost by quartiles was $428, $1,701, $4,760. Mean costs declined with increasing age, except for the 20-24 age group, which contained a single high-cost outlier. Median costs are shown in the Figure, which demonstrates that for the typical individual with Down syndrome, most costs were borne within the first two years of life and rapidly decreased thereafter.
Figure.
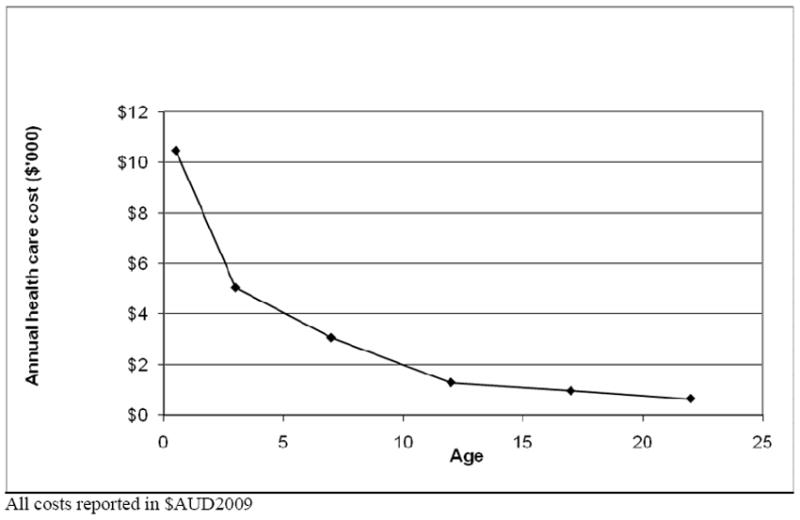
Median annual health care cost per person with Down syndrome by age
Breakdown of the total health cost indicated that hospital cost is a significant contributor, but this is exceeded in most age groups by ‘other’ costs which primarily comprised therapy and respite care (87%). Although therapy (most commonly but not limited to physiotherapy, occupational therapy, hydrotherapy and speech therapy) dominated this cost category in the younger age groups, respite was the major cost in the older age groups. Therapy represented 85% ‘other costs’ in the 0-4 year age group, but declined to 35% for ages over 20 years. Conversely, respite increased from 4% to 60% of ‘other’ costs across the same age groups.
The most commonly utilised therapy was speech therapy for 84 individuals at a mean cost of $1,878 per year, followed by occupational therapy (52 cases, mean cost $1505 per year) and hydrotherapy/swimming classes (46 cases, mean cost $1,442 per year).
Respite care was accessed for only 14% individuals, although use increased with age and dependency. Although rare among the 0-4 year age group (a single case), some respite care was accessed for approximately one third of the individuals aged over 15 years.
The cost of medical visits decreased with increasing age. The mean number of visits to a general practitioner (GP) declined from 6 per year in the under 5 year age group, to 3 per year for age groups over 10 years, which attained mean population GP attendance rates in Australia.17
The trend in use of medication also showed some decrease with age, although the difference was not statistically significant and the proportion using regular medication remained high in all age groups. (Eighty three percent in age groups under 10 years compared with 70% in older age groups).
No large differences in mean or median total or sub-total health costs were evident between those living in rural WA (mean total cost $3,424, 95% CI $2,482 - $4,366, median total cost $1,804, interquartile range (IQR) $392 - $4,774) and those living in the metropolitan area (mean total cost $4,466, 95% CI $3,536 - $5,396, median total cost $1437, IQR $555 - $4,230, p value=0.95 for rank sum test).
Comparison with mean population costs
Mean annual health costs were compared with population age-adjusted mean costs, and the results are shown in Table II. Health costs were higher for individuals with Down syndrome at all ages, but the differential decreased from four times the mean cost in young children, to 1.7 times the mean cost in adolescents and young adults. The cost for a typical individual with Down syndrome (as indicated by the median) approached the population mean during adolescence. (Mean population costs were lowest in the 5-14 year age group and increased in the 15-24 year age group.)
Table 2.
Total mean annual health costs for individuals with Down syndrome, compared with population data, 2009
| Age group | Total mean annual health costs | ||
|---|---|---|---|
| Down syndrome | Australian mean | Ratio | |
| 0-4 | $8,491 | $2,023 | 4.2 |
| 5-14 | $3,588 | $935 | 3.8 |
| 15-24 | $3,164 | $1,844 | 1.7 |
All costs reported in $AUD2009
Costs by presence of congenital heart disease
Total health costs were compared according to whether or not there had been a diagnosis of congenital heart disease (CHD) (current or previous). Three hundred and sixty families provided information about CHD, of whom 45% reported that their child had ever been diagnosed. As shown in Table III, the difference in total health cost was significant between the two groups (p=0.02). Individual age groups did not show statistically significant differences, although the difference in the 0-1 year age group approached significance (p=0.07). The sharp decline in total cost with increasing age was reflected in both groups, and the differential between the two groups also decreased with increasing age.
Table 3.
Total annual health care cost according to ‘ever’ diagnosis of congenital heart disease (CHD)
| Age group | No CHD | CHD (ever diagnosis) | ||
|---|---|---|---|---|
| Total annual health care cost | Total annual health care cost | |||
| Mean | Median | Mean | Median | |
| 0 - 1 yrs | $9,612 | $6,072 | $12,978 | $12,016 |
| n=26 | ||||
| 2 - 5 yrs | $5,730 | $5,514 | $5,845 | $4,945 |
| n = 32 | ||||
| 5 - 9 yrs | $3,765 | $2,594 | $4,725 | $3,695 |
| n = 75 | ||||
| 10 - 14 yrs | $2,536 | $1,280 | $3,693 | $1,326 |
| n = 86 | ||||
| 15-19 yrs | $2,149 | $639 | $3,469 | $1,030 |
| n = 81 | ||||
| 20-24 yrs | $4,059 | $535 | $3,221 | $821 |
| n = 61 | ||||
| Total n=361 | $3,537 | $1,523 | $5,035 | $2,487 |
All costs reported in $AUD2009
Cost by level of functional ability
A single point increase in functional independence in the WeeFIM scale was associated with a large decrease ($87) in total cost, a fairly large decrease in hospital costs and other costs, and small decreases in medical and pharmacy costs (adjusted for age). When WeeFIM scores were grouped by categories according to complete independence (requiring no help), partially independent (requiring supervision) and dependent (requiring help) these relationships were again demonstrated, with the most dependent having the highest total costs, in particular, higher hospital, medical and other costs, even after adjusting for age. For those in the least able group, total cost was $3520.84 (CI $2420- $5123), in the next most able group, costs were $1492.48 (CI $1173 - $1899), and for those in the most able group costs were $590.44 with (CI 458 - $759).
Cost by income
The total cost of health care was compared with annual parental income to assess whether additional services were accessed more by those able to afford them. The highest and lowest income groups reported very similar health care costs throughout the year of reporting, although middle income groups reported spending less. Differences were not statistically significant. The comparison of use of respite care across income groups also demonstrated no significant differences.
Discussion
We report health care cost data throughout childhood and adolescence for Down syndrome. The total mean annual cost of medical care was $4,209 across age groups with a median cost of $1,701. The distribution was skewed in terms of age, where most costs occurred during the first year of life, and in terms of a small number contributing disproportionately to overall cost. The major costs were hospitalisation and ‘other health costs’, comprising costs for therapy and respite care. Highest costs overall were most likely to be associated with young children requiring hospitalisation for heart surgery.
Total health care cost was more than 4 times the population mean in young children but decreased to only 1.7 times the population mean by the end of adolescence. Diagnosis of congenital heart disease and level of independence influenced total healthcare cost, independently of age.
Total mean health care costs were similar to those reported for type-1 diabetes ($3,640 AUD in 2009 for all ages),18 although Down syndrome costs were much higher in the first years of life, direct health care costs for type-1 diabetes increase throughout life. Costs for individuals aged 15-24 years were similar in both groups ($2,267 for type-1 diabetes compared with $2,407 for Down syndrome).
Our costs are considerably less than those estimated by Boulet et al,9 who found that costs in 0-4 year old children with Down syndrome were 12-13 times higher for members of a health insurance organisation than for the mean child of this age in the United States. Unlike the United States, Australia provides universal health care and hence our study is more likely to be representative of the general population. Also in comparison, our study demonstrated a lower proportion of costs attributable to inpatient care in 0-4 year olds (41% in our study compared with 60% in theirs). Our hospital costs did not include respite care but, as shown above, this component was minimal for the 0-4 age group. Both studies demonstrated sharp declines in cost after the first year of life, and our study also established that this typically continues throughout childhood albeit more gradually. The differential between CHD and non CHD was also much higher in the U.S. study compared with ours, however both studies demonstrated a declining disparity according to age, and our study showed longer term continuation of this trend. Our results were consistent with the study by Goldstein10 which demonstrated that the cost of health services for adolescents with Down syndrome was 1.12 times the cost for controls compared with 1.7 in this study.
The one component that demonstrated an opposing trend was the cost of respite which increased with age. Further research is required to explore trends in older age groups. Interestingly, the demand for respite did not vary according to parental income, which may suggest needs are being met, or alternatively that needs are being met by unpaid (and unquantified) assistance.
There was wide variation in costs as demonstrated by the standard deviation, which is not unexpected given the variety of conditions and severities evident among individuals with Down syndrome. Because of the potential for a small number of outliers to influence the mean, the typical cost, as demonstrated by the median is an important indicator of expected resource needs for an individual with Down syndrome. Median costs demonstrated clearly identified trends with age.
Although we had a 73% response, we do not have information on the severity of Down syndrome in the individuals who were not represented. However the proportions of associated conditions were found to be consistent with reported frequencies, for example almost half our cohort reported a diagnosis of a heart condition.16 Similarly our rural – metropolitan distribution of individual cases was consistent with the population distribution in WA.
This study describes only direct health care costs attributable to children and young adults with Down syndrome and does not address overall costs to families affected by Down syndrome, such as special education, individual transport needs, housing modifications and related costs to family members, for example in relation to employment opportunities.
We conclude that health care costs for children and young adults with Down syndrome are highest in the first years of life, and cost predictors include diagnosis of heart disease and level of independent functioning. An important finding is that the demands on health services decline significantly with age to approach population levels during adolescence, indicating the general level of good health within this group. The exception is in the component of respite which increases with age.
Acknowledgments
The authors gratefully acknowledge the participation and ongoing contributions of families in the Down Syndrome NOW Study. We would also like to thank Down Syndrome WA and staff at the Disability Services Commission for their ongoing assistance in the study.
Funded by the National Institutes of Health (5R01HD043100-05) and NHMRC (fellowship #634341). H.L. was previously funded by NHMRC program grant 353514, and is currently funded by NHMRC Senior Research Fellowship #572568. A.B. is funded by NHMRC program grant 572742.
Footnotes
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Elizabeth A Geelhoed, School of Population Health M431, The University of Western Australia, 35 Stirling Hwy, Crawley WA 6009, Ph: + 61 8 6488 7129, Fax: + 61 8 6488 1188, Elizabeth.Geelhoed@uwa.edu.au.
Ami Bebbington, Telethon Institute of Child Health Research, Centre for Child Health Research, University of Western Australia, PO Box 855 West Perth WA 6872 Australia.
Carol Bower, Telethon Institute of Child Health Research, Centre for Child Health Research, University of Western Australia, PO Box 855 West Perth WA 6872 Australia.
Aditya Deshpande, Telethon Institute of Child Health Research, Centre for Child Health Research, University of Western Australia, PO Box 855 West Perth WA 6872 Australia.
Helen Leonard, Telethon Institute of Child Health Research, Centre for Child Health Research, University of Western Australia, PO Box 855 West Perth WA 6872 Australia.
References
- 1.Thomas K, Bourke J, Girdler S, Bebbington A, Jacoby P, Leonard H. Variation over time in medical conditions and health service utilisation of children with Down syndrome. J Pediatr. doi: 10.1016/j.jpeds2010.08.045. In press. [DOI] [PubMed] [Google Scholar]
- 2.Leonard S, Bower C, Petterson B, Leonard H. Medical aspects of school-aged children with Down syndrome. Dev Med Child Neurol. 1999;41:683–688. doi: 10.1017/s0012162299001401. [DOI] [PubMed] [Google Scholar]
- 3.Leonard S, Bower C, Petterson B, Leonard H. Survival of infants born with Down’s syndrome: 1980-96. Paediatr Perinat Epidemiol. 2000;14:163–171. doi: 10.1046/j.1365-3016.2000.00252.x. [DOI] [PubMed] [Google Scholar]
- 4.Bittles AH, Glasson EJ. Clinical, social, and ethical implications of changing life expectancy in Down syndrome. Dev Med Child Neurol. 2004;46:282–6. doi: 10.1017/s0012162204000441. [DOI] [PubMed] [Google Scholar]
- 5.Rasmussen SA, Wong LY, Correa A, Gambrell D, Friedman JM. Survival in infants with Down syndrome, Metropolitan Atlanta, 1979-1998. J Pediatr. 2006;148:806–812. doi: 10.1016/j.jpeds.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 6.Dye DE, Maxwell KS, Goldblatt J, Bower C, Leonard H, Bourke J, et al. The impact of single gene and chromosomal disorders on hospital admissions of children and adolescents: a population based study. Public Health Genomics. 2010 Dec 1; doi: 10.1159/000321767. Published online. [DOI] [PubMed] [Google Scholar]
- 7.Bower C, Rudy E, Callaghan A, Quick J, Cosgrove P, Nassar N. Report of the Birth Defects Registry of Western Australia 1980-2008. Perth: King Edward Hospital, Women and Newborn Health Service; 2009. Number 16. [Google Scholar]
- 8.Thomas K, Girdler S, Bourke J, Deshpande A, Bathgate K, Fehr S, et al. Overview of Health Issues in School-aged Children with Down Syndrome. In: Urbano RC, editor. International Review of Research in Mental Retardation. Academic Press; 2010. pp. 67–106. [Google Scholar]
- 9.Boulet SL, Molinari NA, Grosse SD, Honein MA, Correa-Villaseñor A. Health care expenditures for infants and young children with Down syndrome in a privately insured population. J Pediatr. 2008;153:241–6. doi: 10.1016/j.jpeds.2008.02.046. [DOI] [PubMed] [Google Scholar]
- 10.Goldstein H. One year of health and social services for adolescents with Down’s syndrome. A calculation of costs in a representative area of Denmark. Soc Psychiatry Psychiatr Epidemiol. 1989;24:30–4. doi: 10.1007/BF01788197. [DOI] [PubMed] [Google Scholar]
- 11.Petterson B, Leonard H, Bourke J, Sanders R, Chalmers R, Jacoby P, et al. IDEA (Intellectual Disability Exploring Answers): A population-based database for intellectual disability in Western Australia. Ann Hum Biol. 2005;32:237–243. doi: 10.1080/03014460500075035. [DOI] [PubMed] [Google Scholar]
- 12.Bourke J, Ricciardo B, Bebbington A, Aiberti K, Jacoby P, Dyke P, et al. Physical and mental health in mothers of children with Down syndrome. J Paediatr. 2008;153:320–6. doi: 10.1016/j.jpeds.2008.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leonard S, Msall M, Bower C, Tremont M, Leonard H. Functional status of school-aged children with Down syndrome. J Paediatr Child Health. 2001;38:160–165. doi: 10.1046/j.1440-1754.2002.00736.x. [DOI] [PubMed] [Google Scholar]
- 14.Australian Institute of Health and Welfare. Health expenditure Australia 2007-2008. Health and welfare expenditure series 37 Cat no HWE 46. 2009a Available at: http://www.aihw.gov.au/publications/index.cfm/title/10954.
- 15.Australian Institute of Health and Welfare. Health services series no 33 Cat no HSE 71. Canberra: AIHW; 2009b. Australian hospital statistics 2007–08. [Google Scholar]
- 16.Staples AJ, Sutherland GR, Haan EA, Clisby S. Epidemiology of Down Syndrome in South Australia, 1960-89. Am J Hum Genet. 1991;49:1014–24. [PMC free article] [PubMed] [Google Scholar]
- 17.Britt H, Miller GC, Charles J, Henderson J, Bayram C, Valenti L, et al. General practice series no 28 Cat no GEP 28. Canberra: AIHW; 2010. General practice activity in Australia 2000–01 to 2009–10: 10 year datatables. [Google Scholar]
- 18.Colagiuri Stephen University of Sydney. Boden Institure of Obesity, Nutrition and Exercise (BIONE) & University of Sydney. Menzies Centre for Health Policy. Diabetes Unit & Diabetes Australia. Eli Lilly Australia. & Juvenile Diabetes Research Foundation. DiabCo$t Australia: Type 1: assessing the burden of type 1 diabetes in Australia / Stephen Colagiuri [et al] Diabetes Australia; A.C.T: 2009. [Google Scholar]


