Abstract
Background
High Body Mass Index (BMI) during pregnancy is associated with an increased risk of adverse health outcomes. Making healthy change during pregnancy is beneficial, especially for overweight and obese women.
Aims
The aim of this study was to explore the barriers and enablers identified by overweight and obese women that preclude and facilitate making healthy change during pregnancy.
Method
We conducted a retrospective analysis of patients who presented with suicide attempts to the Rockhampton Base Hospital Emergency Department, Queensland Australia from 1 September 2007 to 31 August 2009. Multivariate logistic regression was undertaken to identify risk factors for ICU and regular ward admission, and predictors of suicide method.
Results
The core concept of “being pregnant” indicated women consider this specific time as both a reason not to make healthy change as well as a motivation for change. Overweight and obese women cited the following barriers to making healthy change during pregnancy: physiological (e.g. pregnancy complications and tiredness); emotional (e.g. preference and mood); cognitive (e.g. lack knowledge); interpersonal (e.g. lack support); and environmental (e.g. availability of healthy choice). Similar enablers were identified by overweight and obese women: physiological (e.g. relief of pregnancy symptoms); emotional (e.g. approval and commitment); cognitive (e.g. knowledge and belief); interpersonal (e.g. family support); and environmental (e.g. help from others). More barriers than enablers were given, indicating that women were more sensitive to barriers than the enablers for making healthy change. Factors viewed by some women as barriers were viewed as enablers by others.
Conclusion
When designing interventions to promote healthy eating and physical activity during pregnancy, individually focused interventions must be implemented in conjunction with environmental-level interventions to facilitate behaviour change.
Keywords: Pregnancy, overweight, healthy change
What this study adds:
Interventions promoting healthy eating and physical activity among overweight and obese pregnant women require identification of barriers to and enablers of healthy change.
We utilised mind -maps to highlight what is really happening in women’s minds and what can be practical for future interventions studies to target based on information provided from real life women.
Future research and intervention should adapt an individual focus and test the effect of the involvement of family and friends.
Background
Obesity is a significant contributor to chronic disease worldwide,1 with current estimates suggesting that nearly half of women of reproductive age in the United States have a Body Mass Index (BMI) ≥ 25kg/m2.2 Being overweight or obese during pregnancy has been well recognised with increased risks of adverse health outcomes for both women and their infants, including an increased risk of both gestational diabetes and hypertensive conditions for women, and for the infant, perinatal death, congenital anomalies, birth trauma, and high birth weight.3-5
Observational studies suggest that among women who are overweight or obese, healthy diet and lifestyle during pregnancy has been associated with improved maternal cardiovascular function and reduced risk of their infant being born large for gestation.6,7 Furthermore, physical activity during pregnancy has been associated with a reduced risk of gestational diabetes, pre-eclampsia, preterm birth and operative birth.8-11 Pregnancy has been considered a “teachable moment”, which may motivate women to change their eating and exercise habits.12 While a number of interventions have been proposed for promoting healthy eating and physical activity among overweight and obese pregnant women, their success requires identification of barriers and enablers of healthy change.
There is considerable information available in the literature describing determinants of healthy eating during pregnancy, including eating habits prior to pregnancy,13 knowledge of nutrition requirements during pregnancy,14 and family support.15 In contrast, pregnancy symptoms including nausea and vomiting, maternal depression, low socioeconomic status, and community factors such as the availability of healthy foods have all been identified to limit maternal diet quality during pregnancy.16-19 A number of quantitative studies have investigated enablers of being active during pregnancy, including positive psychological feelings, family influence, and receiving advice.20-22 The most notable barriers identified preventing women from being active during pregnancy include pregnancy symptoms lack of time and child care, and concerns about safety.20,23-25 We have identified one qualitative study that has explored barriers to being physically active during pregnancy in overweight and obese women. While it reported a wide range of internal (physical and psychological) and external (work, family, time and environmental) barriers,26 the study failed to supply information about enablers or how to overcome these barriers.
While previous research has examined factors affecting healthy change in pregnancy, it has been primarily quantitative in nature and has been limited by small sample sizes and homogeneous samples. Furthermore, previous studies have focused on women of all BMI categories, with no distinct reporting for pregnant women who were overweight or obese. In order to devise health messages for overweight and obese pregnant women, qualitative research that comprehensively examines both barriers and enabling factors for change is required. Hence we proposed a qualitative study that asked the central question: What are the perceived barriers and enablers identified by overweight and obese women that preclude and facilitate making healthy change during pregnancy? This broad and open-ended question directed the research process and served as the focus around which all data were collected and analysed to ultimately allow a better understanding of the enablers and barriers for women who are overweight or obese to making healthy change during pregnancy.
Method
Theoretical basis:
A qualitative study was conducted to explore the concept of perceived barriers and enablers of making healthy change during pregnancy in women who were overweight or obese.27 Perceived barriers and enablers affect people’s behaviour indirectly by impacting motivations.27 When women perceive barriers, they become frustrated, lower their motivation to make healthy change and reduce their effort.28 Perceived enablers have the opposite effect.29 Because women believe that their efforts will be facilitated rather than hindered, they become more motivated. People act on the basis of those perceptions, regardless of whether those perceptions have any basis in reality.27 Therefore, it is important to have detailed descriptions about barriers and enablers in women who are overweight or obese so that future interventions promoting healthy change can be designed. Our research is based on the inductive thematic analysis methodology as it is not wedded to any pre-existing theoretical framework. This approach allows the freedom and flexibility of discovering all possible key features from a data set.30
Participants and sampling:
This study is nested within a randomised trial evaluating the effect of an antenatal intervention to limit weight gain among overweight and obese pregnant women on maternal and infant health outcomes (the LIMIT study).31 Recruitment to the LIMIT study was completed in January 2012 from three public maternity hospitals across the South Australian metropolitan area. The inclusion criteria were a booking BMI ≥25 kg/m2 at first antenatal visit between 10+0 and 20+0 weeks’ gestation, and a singleton pregnancy. Women with previously diagnosed type 1 or 2 diabetes prior to pregnancy were excluded. Baseline demographic details were collected at the time of study entry. A purposive sampling method was adapted for the recruitment of women to complete the interview.32 Participants were chosen from women recruited to the LIMIT study based on a selection matrix of BMI category (BMI<30 kg/m2 and ≥30 kg/m2), and parity (Parity 0 and 1+). Women were then approached via telephone and the purpose and methods of the interview were explained. Women who agreed undertook a face-to-face interview at 28 weeks of gestation.
The interview:
The interviewer (ZS) was a female health science researcher with trained interviewing skills and knowledge of pregnancy health. The interviewer had no previous connection with any participant. The interview took place at the time of the women’s oral glucose tolerance test, in a private hospital clinic room. Recruitment for the interview began in July 2011 and continued through to October 2011 when it was determined that data saturation had been achieved when no new insights were being gained.33 A semi-structured interview guide was developed to provide some direction to the researcher with a standard procedure to enable comparability, but during interviews women were invited to openly tell their stories to ensure their voices were heard and their experiences shared without a rigid adherence to the interview guide.34
Each interview started with the broad opening question, “Is this your first baby?” which served as a port of entry into this significant experience in a woman’s life. Participants were then asked to respond to two structured questions.
1. What makes it difficult to be physically active and what makes it easier to be physically active during pregnancy?
2. What makes it difficult to eat healthily and what makes it easier to eat healthily during pregnancy?
The interviewer then asked participants to give detailed explanations about their answers. Each interview lasted approximately 20-30 minutes. The interview procedure was piloted with an eligible woman and a psychological professional for feedback and corrections. All interviews were audio recorded and transcribed verbatim by the researcher to ensure further immersion in the data. Each interview transcription was addressed with a unique identifier (e.g. In01). Observational notes and journal reflections were maintained throughout data collection and analysis to supplement the in-depth interviews.34 The decision about data saturation was made via discussion between all authors. Approval to conduct this study was obtained from the following research and ethics committee and from the three hospitals where women were recruited: the CYWHS (Children, Youth and Women’s Health Service, Government of South Australia) Research Ethics Committee; Women's and Children's Hospital (Adelaide, South Australia); Flinders Medical Centre (Adelaide, South Australia); Lyell McEwin Health Service (Adelaide, South Australia). All participants signed a consent form and agreed to the researcher recording the interview. Participants were not offered financial incentives to participate in this study.
Data analysis:
Data analysis followed the six phases of thematic analysis procedure introduced by Braun and Clarke.30 After transcription, interviews were read and reviewed line by line, and each discreet idea or concept noted. Then initial codes were produced to identify all features of the data in a systematic fashion across the entire data set. All codes were further collated into potential themes. Themes were further reviewed to check if they worked in relation to the coded extracts and the entire data set. Mind-maps were created to represent the structures of themes and sub-themes.35 Themes were then defined, named and further refined. Examples and extracts were selected and reviewed to ensure clear description of themes before reporting results. The computer software program NVivo9 (QSR International Pty Ltd.) was used to store and manage the data and construct mind-maps.
Results
Participants:
All women who met the inclusion criteria were approached and agreed to participate in the study with no rejections. Twenty-six interviews were conducted to reach data saturation. The demographic characteristics of the 26 women who participated in this study are summarised in Table 1. The mean age was 32.5 years with a standard deviation of 1.1 years. The mean BMI of the women at baseline was 32.8 kg/m2 (standard deviation 6.0 kg/m2). Most of the women were Caucasian and were not smoking during pregnancy.
Table 1. Demographic characters of women interviewed.
| Characters | %(N) |
|---|---|
| Age | |
| 20-30 | 30.8(8) |
| 30-40 | 57.7(15) |
| 40+ | 11.5(3) |
| Parity | |
| 0 | 50.0(13) |
| 1+ | 50.0(13) |
| Weight category | |
| Overweight | 50.0(13) |
| Obese | 50.0(13) |
| Smoker | 7.7(2) |
| Ethnicity | |
| Caucasian | 88.5(23) |
| Asian | 11.5(3) |
The core category:
Following a protracted involvement with the data, the core category of “being pregnant” emerged to capture the experience of making healthy change during pregnancy and refers to a special period of life when women have different perceptions about weight and health. This is the terminology used by women to identify their weight, health status, eating habits, and exercise routine at this specific period of life. It provides a label for giving explanations to ‘let go' and not to make healthy changes. At the same time, pregnancy was viewed as a time for rising health concerns and becoming motivated for making healthy change. As frequently referred to in the interviews, “all pregnant women gain weight, there is nothing you can do about it… (I’m worried about) not being able to lose the gained weight after pregnancy.” It is suggested that this use of the label “being pregnant” provides safety for overweight and obese women in a society where the stigma around weight remains deeply entrenched and indicates they would rather make change after pregnancy.
The 26 women interviewed also identified five main categories of barriers to and enablers of making healthy change while being pregnant: physiological, emotional, cognitive, interpersonal, and environmental.
Barriers to make healthy change:
All women provided key concepts and examples of barriers toward making healthy change during pregnancy. There was no obvious difference in the number of barriers in the conversations between overweight women and obese women (55 responses in overweight women vs. 54 in obese women), or between women with no other child at home and women with at least one child at home (60 responses in women with parity 0 vs. 49 in women with parity ≥1). The key concept of barriers to making healthy change is summarised in Table 2 with examples attached. The coverage of this topic in the interviews is shown in Figure 1 which is the mind-map representing barriers as nested rectangular boxes. The larger the box, the more frequently this code was referred to in the interviews.
Table 2. Categories of barriers and enablers of making healthy change.
| Concepts | Barriers | Examples | Enablers | Examples |
|---|---|---|---|---|
| Physiological | -Pregnancy complications | - Nausea, vomit, back pain, muscle cramps | - Relief symptoms | - Less back ache, muscle cramps, constipation |
| - Health conditions | - Chronic conditions | - Being fit | - More energy | |
| - Tiredness | - Too tired to prepare meals or exercise | |||
| Emotional | - Preference | - Don’t like cooking/exercise | - Approval | - Want others approval |
| - Mood | - Don’t feel like cooking/exercise | - Commitment | - Commit to previously paid exercise class | |
| - Pregnancy as an excuse | ||||
| - Feeling | - Feel good, enjoyment, fun | |||
| Cognitive | - Lack knowledge | - Lack knowledge about adverse health outcomes, cooking skill, healthy eating information, safe exercise information | - Knowledge | - Understand safe exercise |
| - Have cooking skill and healthy eating information | ||||
| - Concern of neonatal health | - Worry about safety of the baby | - Health concern | - Want to improve maternal and neonatal health | |
| - Belief | - Believe it is important in life | |||
| - Self-efficacy | - Be able to make the change | |||
| Interpersonal | -No time | -Caring for other children | - More time | - Reduce work time |
| - Family/work commitment | - No other children, or have help for childcare | |||
| - Lack support | - No help | - Family support | - Preparing healthy food for/with family | |
| -Family don’t like healthy food | -Exercise with family | |||
| -No one to exercise with | ||||
| - No healthy habits | - No pre-pregnancy healthy routine | - Healthy routine | - Pre-pregnancy routine | |
| - Cost | - Healthy food/gym is expensive | - Peer-pressure | - Feel pressure from others to do so | |
| Environmental | - Physical environment | - Weather | - Community | - Meet and share experience with other pregnant women |
| - Availability | - Lack of healthy choices | - External help | - Health professionals, personal trainers | |
| - No safe exercise space |
Figure 1. Mind map of codes in women’s perceived barriers of making healthy change during pregnancy. The mind man represents the barriers of making healthy change expressed in the interviews as nested rectangular boxes. The size of each box represents how many of the sentences are coded by the grouped barriers. The larger the box is, the more frequently this barrier has been reported in the interview.
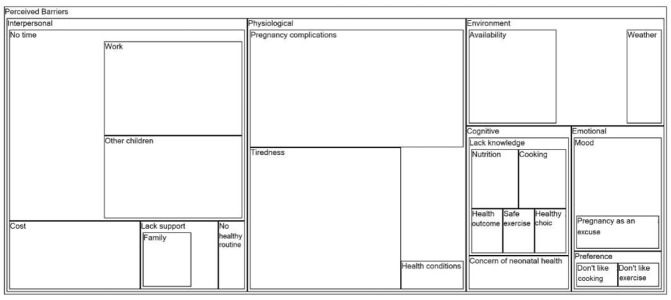
The category of interpersonal barriers was the most frequently referred to concept in the interviews, representing a large range of personal barriers, which also appeared to be highly individualised. The relatively mutual code was “no time” as women mentioned family and work commitment to be priorities in life. Other factors including cost of healthy eating and exercise classes, lack of support (e.g. from family, friends, health professionals, and community), and no pre-pregnancy healthy eating and exercise routine were identified to be barriers in individual cases. Some examples are:
…in between working, and picking up from child care, and cooking tea, there’s not much time left in the day. (In02, obese, parity 1) I'm studying, and working, and being pregnant, so, quite full on…and I’d like to join the gym, but you’ve just got to be realistic about affording it. (In05, obese, parity 0) I'm not used to eating healthy food. (In20, overweight, parity 0)
The next most frequently referred concept was the category of physiological barriers, including tiredness, pregnancy complication, and other non-pregnancy-related health conditions. This concept was related to both healthy eating and physical activity during pregnancy:
If I continue with walking after 30 minutes I get tired and I don't know why. (In20, overweight, parity 0) Before pregnancy I ate healthily. But now because I’m pregnant I think it's the change of the hormones and many other pregnancy symptoms that make me crave food more and just feeling hungry all the time. (In15, overweight, parity 0) …difficulty (with exercise) is when you’ve got a big belly and you just get really heavy and you can't do things as quickly as you used to do. (In14, obese, parity 1)
The category of environment barriers represents external factors from either the physical environment or the facilities in the community, which may affect women’s healthy eating or exercise behaviour:
…at work it (healthy eating) is really hard because the kind of food they serve there (is not healthy)… (In13, obese, parity 0) Obviously the weather at the moment makes it difficult to exercise, and getting dark very early. Those are things that stop you getting out and walking. (In24, overweight, parity 0)
The category of cognitive barriers represents messages in the interviews with women speaking often about knowledge of healthy eating, safe exercise during pregnancy, and the necessity of making change. In addition, women also indicated worry about the safety of the baby while exercising during pregnancy.
As a result of lack of knowledge about possible adverse health outcomes, nutrition, cooking skill, healthy choice, and safe exercise information, women identified it as a significant barrier to making healthy change during pregnancy. Example quotes are:
I'm not the good cook. So, maybe it's just that we are eating the same over and over again. So in the end I will say 'let's go out.' (In03, overweight, parity 0) There’s not a lot of information about what kind of exercise you can do. (In13, obese, parity 0)
The category of emotional barriers refers to those related to personal preference and mood. Women also indicated that they use the concept of being pregnant to explain their preference of not cooking and exercising:
I think at the moment (being pregnant) it's my mind set. If I feel like doing that (healthy eating), I’ll do it. If I don't want to do it, I don't do it. (In08, obese, parity 2)
Enablers of making healthy change:
Only 17 of the 26 women (65.4 per cent) interviewed provided concepts of enablers and examples of making healthy change during pregnancy. In women who provided no descriptions about enablers, three were overweight with no other children at home, two were overweight with at least one child at home, three were obese with no other children, and one was obese with parity greater than one. There was no obvious difference in the number of enablers referred to in the conversation between overweight (N=9) or obese women (N=8) (responses 19 vs. 22), or between women with no other child at home (N=8) and women with at least one child at home (N=9) (responses 18 vs. 23). Many concepts viewed by some women as barriers were seen as enablers by others. The key concept of enablers of making healthy change is summarised in Table 2 with examples attached. The coverage of this topic in the interviews is shown in Figure 2.
Figure 2. Mind map of codes in women’s perceived enablers of making healthy change during pregnancy. The mind map represents the enablers of making healthy change expressed in the interviews as nested rectangular boxes. The size of each box represents how many of the sentences are coded by the grouped enablers. The larger the box is, the more frequently this enabler has been reported in the interview.
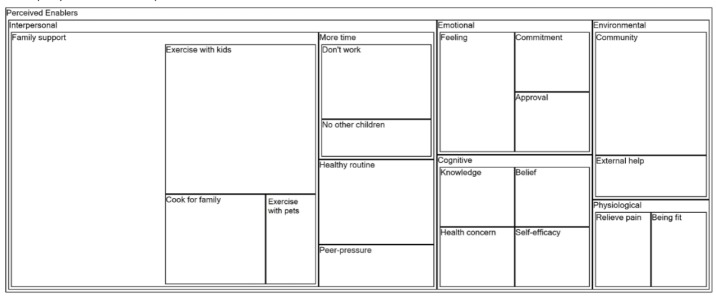
The most frequently cited enablers were those in the interpersonal category. A commonly reported enabler was that of family support which includes family and friends’ encouragement of healthy eating and exercise, obligation to cook healthy meals for the family, and opportunity to exercise with children and pets. Less work and family commitment, having a healthy routine prior to pregnancy, and positive peer-pressure were also reported as contributing to healthy changes during pregnancy. Some examples are:
The good thing is I do have him (the other child at home), so we can walk to the park. I chase after him. (In01, overweight, parity 1) I used to be around people who do cook and only make healthy choices. It is helpful. (In 21, overweight, parity 2) My husband is very supportive. He does heaps of cooking. Even if I don't have the energy, he'll cook the right food for me. (In22, obese, parity 0)
The category of emotional enablers including wanting others’ approval, commitment to previously paid classes, and feelings attached to healthy eating and exercise were mentioned more frequently than other physical or cognitive enablers.
(What makes exercise) easier...my yoga, I’ve already paid for the class so I need to go. (In12, overweight, parity 0) Exercise makes me feel better. The head space. You just feel good. (In21, overweight parity 2) I'm just trying to get into a routine to eat healthier. That's the real hard thing for me. But I know that I need to. I need to let them (family and friends) know I can do it. (In 24, obese, parity 0)
The category of cognitive enablers represents women who indicate having knowledge about healthy eating and safe exercise, concern about maternal and neonatal health, belief in healthy eating and exercise, and having selfefficacy to make changes.
Because it's (healthy eating) good for the mother and the baby. (In05, obese, parity 0) Many people think eating a healthy diet costs more and needs more time. They don't realise that making a salad costs 5 minutes. If you eat seasonal, it's always cheaper. (In17, overweight, parity 1) You need to be confident about it. (I’m) confident enough. I've done a lot of changes. (In03, overweight, parity 0)
The category of environmental enablers represents community support, e.g. arrangement to meet and share experience with other pregnant women, and other external help including information from health professionals.
A constant external reinforcement (about healthy eating and exercise) from the hospital or other pregnant women may help. (In24, obese, parity 0)
The category of physiological enablers was only briefly reported in the interviews and represents relief of symptoms and improving fitness after making changes. It is noted that physiological enablers only applied to exercise during pregnancy.
That (exercise) helps a lot with the back pain. You can tell the difference. (In16, obese, parity 2)
Discussion
We report here for the first time a detailed qualitative investigation of barriers to and enablers of making healthy change during pregnancy in overweight and obese women. We found that women used the core concept of “being pregnant” to identify their health status, eating habits, and exercise routine at this specific period of life. While this label acts as an explanation for some women to let go and not make healthy changes, for others it represents a concern and a motivation for change. We identified physiological, emotional, cognitive, interpersonal, and environmental categories to be the main themes of barriers and enablers, with women providing more information about barriers than enablers. In addition, we found no difference between overweight and obese women, and between women with no other child or women with at least one other child at home.
As previously reported by women of all BMI categories, having a healthy routine prior to pregnancy, having knowledge, family support, receiving external help, and positive psychological feelings associated with healthy eating and exercise are all enablers of healthy eating and active lifestyle during pregnancy.13,36 These findings were also identified in the interviews in our study. We report for the first time interpersonal enablers including family support, having more time, having a previous healthy routine, and peer-pressure, to be the more frequently referred to concepts, which may have a greater impact on women than emotional, cognitive, environmental and physiological enablers.
Research about barriers to making healthy change in women of all weight ranges shows that pregnancy symptoms, psychological feelings, low income, the environment, lack of time, and child care all negatively influence healthy eating and exercise during pregnancy, which is in consistent with our findings.16-19,25 In addition, Weir and colleagues’ investigation of barriers to physical activity during pregnancy in overweight and obese women found similar results but highlighted that lack of selfconfidence and motivation was of particular relevance as a barrier to change in overweight or obese women.26 In our study, when asking about factors that make it difficult to eat healthily or be more active during pregnancy, women did not raise weight as a particular concern. However, when asking about factors that make it easier to achieve healthy changes, women indicated self-efficacy to be an enabler under the cognitive theme. The slight difference in responses between the two studies may be explained by the different questions asked in the current research.
Similar to the findings of Weir and colleagues, women interviewed in our study were unconcerned about weight gain during pregnancy, except in mentioning that increasing abdominal girth made it difficult to engage in exercise. This attitude may reflect the current absence of formal recommendations for pregnancy weight gain and activity levels in women who are overweight or obese as a part of routine antenatal health care.
Although it has been suggested that pregnancy represents a timely opportunity to promote healthy change, most women in our study did not consider pregnancy a specific time to make change, although they did indicate a willingness to improve behaviours for the sake of maternal and neonatal health. In fact, women considered pregnancy as a particularly difficult time to make healthy change as they experienced pregnancy complications, tiredness, food craving, in addition to concerns about the safety of such changes on the pregnancy. In addition, women were more sensitive to barriers than enablers, indicating that future studies promoting healthy eating and physical activity should address barriers based on individual circumstances to enhance the effect of health promoting strategies.
Of particular importance, help from health professionals was not identified as a significant enabler to making healthy change. In contrast, women did identify family support, peer-pressure, and knowledge to be enablers of healthy change, indicating the relative importance of advice received from family and friends in initiating behaviour change. These findings are consistent with the reports of other qualitative investigations, identifying advice and support from a woman’s partner and friends to be significant factors for facilitating behaviour change during pregnancy.21,37 Hence, future health promotion during pregnancy should attempt to increase the involvement of family and friends to enlarge the educational effect.
Although not referred to as frequently as interpersonal factors, we identified environmental factors to be both barriers to and enablers of making healthy change during pregnancy. Previous research has recognised that food security and the availability of healthy food choices can limit healthy eating during pregnancy,13 while weather and the lack of a suitable exercise environment limit physical activity.38 Women interviewed in our study indicated that a community with knowledge and support of healthy eating and lifestyle could be a positive influence to pregnancy behaviours, raising the possibility of future studies to engage environment-level interventions rather than to consider this external influence as a barrier only.
In this study, validity was maximised as data saturation was achieved with 26 interviews. In addition, there was a pilot interview with an eligible women and a psychological expert to test the face validity of the interview content. In interpreting the findings of this study, it is important to acknowledge its limitations. Although we attained data saturation, we did not consider this separately for overweight or obese women. At the same time, we did not identify a significant difference in responses based on maternal BMI. As most of our participants were Caucasian, the findings may not be generalisable to women from other ethnicities where cultural norms and different lifestyles may have a significant impact on pregnancy behaviours.21
Conclusion
The detailed insights provided into the barriers and enablers which influence healthy behaviour change during pregnancy in women who were overweight or obese, may be targeted in future intervention studies. Although many of the themes from the current the study are similar to those reported from other settings, our study is the first comprehensive investigation of both barriers to and enablers of making both healthy eating and active lifestyle change in overweight and obese women. The confirmation of previous findings provides further confidence in the reliability of our results. We advise that when designing intervention studies during pregnancy to focus on healthy behaviour change, an individual focus must be adopted, addressing individual barriers to change. Future research should also test whether increased involvement of family and friends in health promotion during pregnancy can increase adherence to diet and lifestyle recommendations.
ACKNOWLEDGEMENTS
We are thankful to all the women who participated in this study on which this manuscript is based.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
FUNDING
The LIMIT study is supported through a NHMRC project grant (ID 519240)
ETHICS COMMITTEE APPROVAL
Approval to conduct this study has been obtained from the following research and ethics committees: the CYWHS(Children, Youth and Women’s Health Service, Government of South Australia) Research Ethics Committee (REC1839/6/2012); Women's and Children's Hospital (Adelaide, South Australia); Flinders Medical Centre (Adelaide, South Australia); Lyell McEwin Health Service (Adelaide, South Australia).
Please cite this paper as: Sui Z, Turnbull D, Dodd J. Enablers and barriers to making healthy change during pregnancy in overweight and obese women. AMJ 2013, 6, 11, 565-577.http//dx.doi.org/10.4066/AMJ.2013.1881
References
- 1.World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894(i-xii):1–253. [PubMed] [Google Scholar]
- 2.Vahratian A. Prevalence of overweight and obesity among women of childbearing age: results from the 2002 National Survey of Family Growth. Matern Child Health J. 2009 Mar;13(2):268–273. doi: 10.1007/s10995-008-0340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Callaway LK, Prins JB, Chang AM, McIntyre HD. The prevalence and impact of overweight and obesity in an Australian obstetric population. Med J Aust. 2006 Jan 16;184(2):56–59. doi: 10.5694/j.1326-5377.2006.tb00115.x. [DOI] [PubMed] [Google Scholar]
- 4.Dodd JM, Grivell RM, Crowther CA , Robinson JS. Antenatal interventions for overweight or obese pregnant women: a systematic review of randomised trials. BJOG. 2010 Mar 29; doi: 10.1111/j.1471-0528.2010.02540.x. [DOI] [PubMed] [Google Scholar]
- 5.Doherty DA, Magann EF, Francis J, Morrison JC, Newnham JP. Pre-pregnancy body mass index and pregnancy outcomes. Int J Gynaecol Obstet. 2006 Dec;95(3):242–247. doi: 10.1016/j.ijgo.2006.06.021. [DOI] [PubMed] [Google Scholar]
- 6.Rhodes ET, Pawlak DB, Takoudes TC, Ebbeling CB, Feldman HA, Lovesky MM, Cooke EA, Leidig MM, Ludwig DS. Effects of a low-glycemic load diet in overweight and obese pregnant women: a pilot randomized controlled trial. Am J Clin Nutr. 2010 Dec;92(6):1306–1315. doi: 10.3945/ajcn.2010.30130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moses RG, Luebcke M, Davis WS, Coleman KJ, Tapsell LC, Petocz P, Brand-Miller JC. Effect of a low-glycemic-index diet during pregnancy on obstetric outcomes. Am J Clin Nutr. 2006 Oct;84(4):807–812. doi: 10.1093/ajcn/84.4.807. [DOI] [PubMed] [Google Scholar]
- 8.Dempsey JC, Sorensen TK, Williams MA, Lee IM, Miller RS, Dashow EE, Luthy DA. Prospective study of gestational diabetes mellitus risk in relation to maternal recreational physical activity before and during pregnancy. Am J Epidemiol. 2004 Apr 1;159(7):663–670. doi: 10.1093/aje/kwh091. [DOI] [PubMed] [Google Scholar]
- 9.Sorensen TK, Williams MA, Lee IM, Dashow EE, Thompson ML, Luthy DA. Recreational physical activity during pregnancy and risk of preeclampsia. Hypertension. 2003 Jun;41(6):1273–1280. doi: 10.1161/01.HYP.0000072270.82815.91. [DOI] [PubMed] [Google Scholar]
- 10.Melzer K, Schutz Y, Soehnchen N, Othenin-Girard V, Martinez de Tejada B, Irion O, Boulvain M, Kayser B. Effects of recommended levels of physical activity on pregnancy outcomes. Am J Obstet Gynecol. 2010 Mar;202(3):e261–266. doi: 10.1016/j.ajog.2009.10.876. [DOI] [PubMed] [Google Scholar]
- 11.Hatch M, Levin B, Shu XO. M. Maternal leisuretime exercise and timely delivery. Am J Public Health. 1998 Oct;88(10):1528–1533. doi: 10.2105/ajph.88.10.1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Phelan S. Pregnancy: a "teachable moment" for weight control and obesity prevention. Am J Obstet Gynecol. 2010 Feb;202(2):135–138. doi: 10.1016/j.ajog.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fowles ER, Fowles SL. Healthy eating during pregnancy: determinants and supportive strategies. J Community Health Nurs. 2008 Jul-Sep;25(3):138–152. doi: 10.1080/07370010802221727. [DOI] [PubMed] [Google Scholar]
- 14.Dundas M, Taylor S. Perinatal factors, motivation, and attitudes concerning pregnancy affect dietary intake. Topics in Clinical Nutrition. 2002;17(2):71–79. [Google Scholar]
- 15.Fowles ER, Hendricks JA, Walker LO. Identifying healthy eating strategies in low-income pregnant women: applying a positive deviance model. Health Care Women Int. 2005 Oct;26(9):807–820. doi: 10.1080/07399330500230953. [DOI] [PubMed] [Google Scholar]
- 16.Pepper GV. Craig Roberts S. Rates of nausea and vomiting in pregnancy and dietary characteristics across populations. Proc Biol Sci. 2006 Oct 22;273(1601):2675–2679. doi: 10.1098/rspb.2006.3633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hurley KM, Caulfield LE, Sacco LM, Costigan KA, Dipietro JA. Psychosocial influences in dietary patterns during pregnancy. J Am Diet Assoc. 2005 Jun;105(6):963–966. doi: 10.1016/j.jada.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 18.Finch BK. Socioeconomic gradients and low birth-weight: empirical and policy considerations. Health Serv Res. 2003 Dec;38(6 Pt 2):1819–1841. doi: 10.1111/j.1475-6773.2003.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007 Mar;44(3):189–195. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 20.Duncombe D, Skouteris H, Wertheim EH, Kelly L, Fraser V, Paxton SJ. Vigorous exercise and birth outcomes in a sample of recreational exercisers: a prospective study across pregnancy. Aust N Z J Obstet Gynaecol. 2006 Aug;46(4):288–292. doi: 10.1111/j.1479-828X.2006.00594.x. [DOI] [PubMed] [Google Scholar]
- 21.Thornton PL, Kieffer EC, Salabarria-Pena Y, Odoms-Young A, Willis SK, Kim H, Salinas MA. Weight, diet, and physical activity-related beliefs and practices among pregnant and postpartum Latino women: the role of social support. Matern Child Health J. 2006 Jam;10(1):95–104. doi: 10.1007/s10995-005-0025-3. [DOI] [PubMed] [Google Scholar]
- 22.Clarke PE, Gross H. Women's behaviour, beliefs and information sources about physical exercise in pregnancy. Midwifery. 2004 Jun;20(2):133–141. doi: 10.1016/j.midw.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 23.Pereira MA, Rifas-Shiman SL, Kleinman KP, Rich-Edwards JW, Peterson KE, Gillman MW. Predictors of change in physical activity during and after pregnancy: Project Viva. Am J Prev Med. 2007 Apr;32(4):312–319. doi: 10.1016/j.amepre.2006.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Evenson KR, Savitz DA, Huston SL. Leisure-time physical activity among pregnant women in the US. Paediatr Perinat Epidemiol. 2004 Nov;18(6):400–407. doi: 10.1111/j.1365-3016.2004.00595.x. [DOI] [PubMed] [Google Scholar]
- 25.Symons Downs D, Hausenblas HA. Women's exercise beliefs and behaviors during their pregnancy and postpartum. J Midwifery Womens Health. Mar-Apr. 2004;49(2):138–144. doi: 10.1016/j.jmwh.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 26.Weir Z, Bush J, Robson SC, McParlin C, Rankin J, Bell R. Physical activity in pregnancy: a qualitative study of the beliefs of overweight and obese pregnant women. BMC Pregnancy Childbirt. 2010;10:18. doi: 10.1186/1471-2393-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lent RW, Brown SD, Hackett G. Contextual supports and barriers to career choice: a social cognitive analysis. J Couns Psychol. 2000 Jan;47(1):36–49. [Google Scholar]
- 28.Mathieu JE, Tannenbaum SL, Salas E. Influences of Individual and Situational Characteristics on Measures of Training Effectiveness. Acad Manage J. 1992 Oct;35(4):828–847. [Google Scholar]
- 29.Noe RA, Wilk SL. Investigation of the Factors That Influence Employees Participation in Development Activities. J Appl Psychol. 1993 Apr;78(2):291–302. [Google Scholar]
- 30.Braun V, Clarke V. Using thematic analysis in psychology. Using thematic analysis in psychology. 2006;3(2):77–101. [Google Scholar]
- 31.Dodd JM, Turnbull DA, McPhee AJ, Wittert G, Crowther CA, Robinson JS. Limiting weight gain in overweight and obese women during pregnancy to improve health outcomes: the LIMIT randomised controlled trial. BMC Pregnancy Childbirth. 2011;11:79. doi: 10.1186/1471-2393-11-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murray SA. Experiences with "rapid appraisal" in primary care: involving the public in assessing health needs, orientating staff, and educating medical students. BMJ. 1999 Feb 13;318(7181):440–444. doi: 10.1136/bmj.318.7181.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Strauss AL, Corbin JM. Newbury Park, Calif: Sage Publications; 1990. Basics of qualitative research : grounded theory procedures and techniques. [Google Scholar]
- 34.Charmaz K. Thousand Oaks, CA: Sage; 2006. Constructing grounded theory: A practical guide through qualitative analysis. [Google Scholar]
- 35.Brightman J. London, U.K.: IOE Conference; 2003. Mapping methods for qualitative data structuring (QDS). Strategies in Qualitative Research: Methodological issues and practices using QSR NVivo and NUDIST. [Google Scholar]
- 36.Gaston A, Cramp A. Exercise during pregnancy: a review of patterns and determinants. J Sci Med Sport. 2011 Jul;14(4):299–305. doi: 10.1016/j.jsams.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 37.Evenson KR, Moos MK, Carrier K, Siega-Riz AM. Perceived barriers to physical activity among pregnant women. Matern Child Health J. 2009 May;13(3):364–375. doi: 10.1007/s10995-008-0359-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Evenson KR, Aytur SA, Borodulin K. Physical activity beliefs, barriers, and enablers among postpartum women. J Womens Health (Larchmt) 2009 Dec;18(12):1925–1934. doi: 10.1089/jwh.2008.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]


