Abstract
Introduction
Atopic dermatitis (AD) is a chronic inflammatory skin disease, characterized by intense itch, typical localization and a specific image of skin lesions. Pathogenesis of pruritus in AD is not fully understood, but recent studies emphasize the role of interleukin-31 (IL-31). This relatively recently described cytokine is considered to be a potential mediator inducing pruritus in AD.
Aim
To assess the correlation of serum IL-31 level and the disease severity in children with AD.
Material and methods
Twenty-five children (16 girls and 9 boys) with AD aged from 4 months to 17 years (mean age: 4.2 years) were enrolled in the study. Disease severity in children with AD was assessed using the SCORAD (Severity SCORing of Atopic Dermatitis) index. Serum IL-31 levels were measured using ELISA with standard kits from EIAab R&D Systems.
Results
Serum IL-31 level was significantly higher in AD children than in healthy children. There was no statistic correlation between serum IL-31 level and the disease severity or itch intensity.
Conclusions
The disease severity and itch intensity do not correlate with serum IL-31 level in children with atopic dermatitis.
Keywords: atopic dermatitis, interleukin 31, SCORAD, pruritus, children
Introduction
Atopic dermatitis (AD) is a chronic, relapsing and pruritic inflammatory skin disease, characterized by typical localization and a specific image of skin lesions, with coexistence of other atopic diseases. Diagnostic criteria for AD elaborated by Hanifin and Rajka have been universally accepted, due to a large variety of the clinical picture [1].
Pruritus is one of the most common symptoms in AD, practically occurring in each patient. Therefore, it has been included as one of the four major diagnostic criteria [1, 2]. Scoring the intensity of pruritus is an integral part of the SCORAD (Severity SCORing of Atopic Dermatitis) index, which is commonly used to determine the severity of the disease [3]. The etiology of pruritus in AD is not fully explained, however the participation of some endogenous mediators, neurotransmitters, arachidonic derivatives and cytokines has been taken into consideration in itch pathophysiology [4]. Recently, in numerous studies, interleukin-31 (IL-31) has been associated with the pathogenesis of pruritus in chronic inflammatory skin diseases [5]. This relatively newly described cytokine is preferentially produced by activated T cells skewed towards Th2 [6]. Interleukin-31 is related to the IL-6 cytokine family [7]. It signals through a heterodimeric receptor composed of IL-31 receptor α (IL-31RA) also known as gp130-like receptor (GPL) and oncostatin M receptor (OSMR) [6, 8, 9]. Dillon et al. demonstrated the development of severe pruritus and skin lesions similar to AD in transgenic mice with overexpression of IL-31 [7]. Other studies revealed that IL-31 serum levels are higher in patients with AD comparing to healthy controls [10]. Moreover, serum IL-31 levels correlate with the disease activity in atopic patients [11]. Evidence of the importance of IL-31 in the pathogenesis of pruritus is also present in studies on IL-31 inhibitors relevant to the treatment of AD [12, 13].
Aim
The aim of the study was to assess the correlation between serum IL-31 levels and the disease severity in patients with AD.
Material and methods
Twenty-five children (16 girls and 9 boys) with AD aged from 4 months to 17 years (mean age: 4.2 years) were enrolled in the study. The control group (CG) consisted of 20 healthy children diagnosed due to recurrent diseases of the respiratory tract with no immunodeficiencies, atopic and dermatological diseases with accompanying pruritus. Atopic dermatitis was diagnosed according to criteria proposed by Hanifin and Rajka [1]. Disease severity was determined using the SCORAD (Severity SCORing of Atopic Dermatitis) index including subjective symptoms, extent and intensity of the lesions. Subjective itch intensity was measured using a patient/parent-reported 0-10 scale (0: no pruritus, 10: extremely severe pruritus). Sixteen children had moderate AD (SCORAD index 25-50) and 9 children had severe AD (SCORAD index over 50). Children included in the study were hospitalized in the Department of Pediatrics, Immunology and Nephrology of the Polish Mother's Research Memorial Institute in Lodz in 2011-2012.
Serum IL-31 levels were measured using ELISA with standard kits from EIAab R&D Systems. Serum was stored at –30°C until assayed. All analyses were performed according to the manufacturer's protocol. The tests were performed in the immunological laboratory – APC Medical Analysis in Lodz.
Statistical analysis
The statistical analysis was performed with the use of Statistica programme 10.0PL (StatSoft, Poland). The data were presented as a median value and interquartile range (IQR) or as a mean value and standard error (SE) according to the normal distribution and the number of patients in the group. Normal distribution was tested with Shapiro-Wilk test, accepting p < 0.05 as the value different from normal distribution. In all cases, statistically significant probability of α error (p) was considered as less than 0.05. Correlations between serum IL-31 level in the study and control groups and the disease severity in AD patients were assessed using U Mann-Whitney test. The Spearman rank test was used to evaluate the relationship between serum levels of IL-31 and itch intensity.
Results
Serum IL-31 levels in both groups
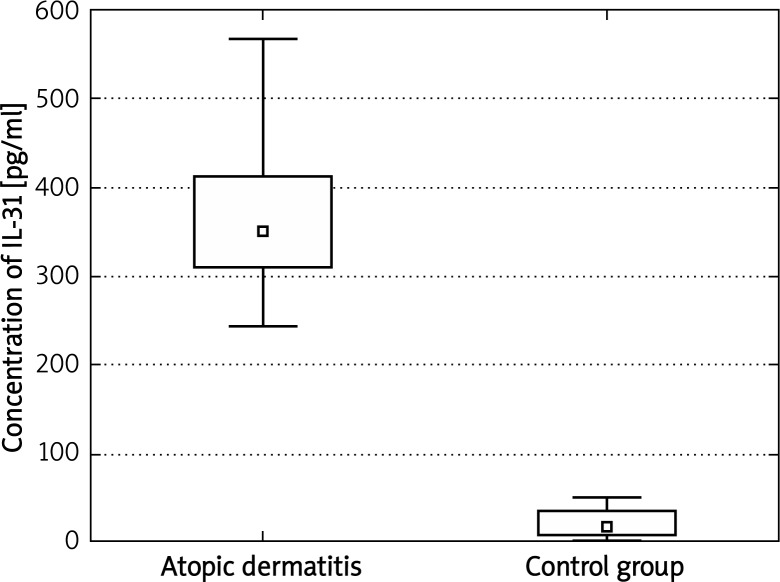
Table 1 shows the median and quartile values of serum IL-31 level in both groups. We found significant differences between the group of patients with AD and CG (Figure 1).
Table 1.
The median and quartile values of serum IL-31 level in AD and healthy children (CG). Significant differences be-tween research groups were found
| Group | Concentration of IL-31 | ||
|---|---|---|---|
| Q25 | Median | Q75 | |
| Control | 8.1300 | 17.3200 | 35.9100 |
| Atopic dermatitis | 309.0000 | 350.6000 | 412.5000 |
| All | 19.8800 | 252.2000 | 350.9000 |
Figure 1.
Comparison of the median and quartil values of serum IL-31 levels between the group of patients with AD and the control group
The statistical analysis showed that serum IL-31 level was significantly higher in AD than in the control group (AD vs. CG, p < 0.000001).
Correlation between serum IL-31 level and the disease severity
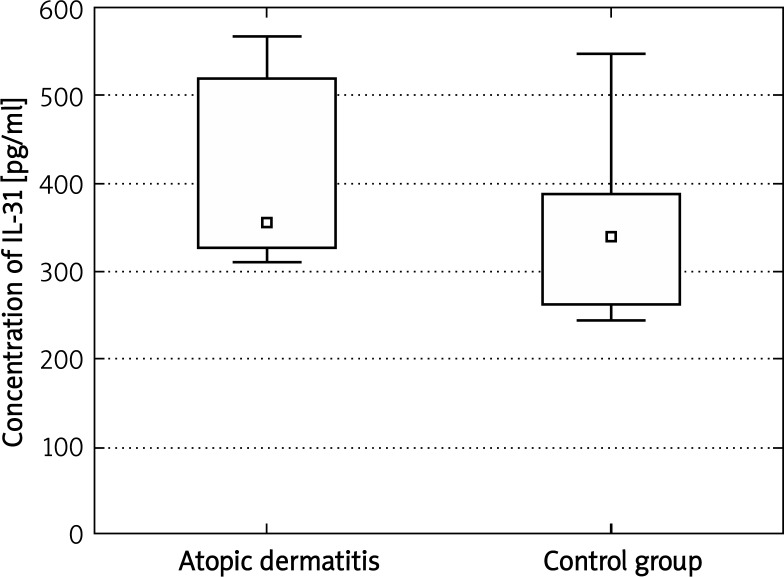
Serum IL-31 level was inversely correlated with the disease severity by SCORAD index (p = 0.1). The test result close to 0.1, and Figure 2 showing the median and quartile values in the group of patients with severe AD (SCORAD > 50 points) and moderate AD (SCORAD 25–50 points) are suggestive of a small number of patients in groups.
Figure 2.
Comparison of IL-31 level in patients with severe AD (SCORAD > 50) and moderate AD (SCORAD 25–50)
Correlation between serum IL-31 level and itch intensity
Serum cytokine level was not significantly correlated with itch intensity in patients with AD (p = 0.372), as shown in Table 2.
Table 2.
Correlation of itch intensity with serum IL-31 level
| Pair of variables | N | Spearman R | t (N – 2) | Value of p |
|---|---|---|---|---|
| Itch and IL-31 | 25 | 0.186388 | 0.909828 | 0.372349 |
Discussion
In the present study, we have shown that serum IL-31 level was higher in children with AD than in healthy patients, which is consistent with the results given by other authors. There are numerous reports in the literature indicating the involvement of IL-31 in the pathogenesis of AD.
Sonokoly et al. and Raap et al., as one of the first, achieved significantly higher serum IL-31 levels in the group of patients with AD [11]. Similar results were obtained by Ezzat et al. and Kim et al., comparing serum IL-31 levels in AD patients with healthy ones. Analysis of serum IL-31 levels were performed in both cases using ELISA method, obtaining significantly higher results in AD patients [14, 15]. Nobbe et al. demonstrated increased immunoreactivity of IL-31 in infiltrating inflammatory cells in AD compared with pruritic or Th2-mediated diseases [16]. Szegedi et al. proved that T cells in chronic AD skin produce IL-31 and that AD lesions contain increased levels of these IL-31-producing T cells [17].
In this study there was no correlation between the severity of the disease and serum IL-31 levels, which may be partly consistent with Neiss et al.'s study, who found statistically increased mRNA levels of IL-31 in biopsy specimens of patients with AD, irrespective of the disease severity [18]. Similar reports with presented results can also be found in the literature.
Ezzat et al. show a positive correlation by classifying patients into three groups: severe, moderate and mild AD [14]. Kim et al. point out to a positive correlation and a strong interrelation between serum levels of IL-31, the degree of the disease severity and mRNA level for this cytokine in skin biopsies of patients with AD [15].
In the present study we have also shown no correlation between itch intensity and serum level of tested cytokine in AD patients. Kim et al. obtained different results and demonstrated a correlation between subjective itch intensity and serum IL-31 levels, what was suggestive of a possible involvement of IL-31 as a mediator inducing not only inflammation, but also pruritus in AD.
Important factors in the analysis of the presented results are subjectivity of pruritus severity assessment and the number of the research groups. Studies performed on a mouse model of dermatitis using a monoclonal antibody neutralizing the effects of IL-31 are promising, due to no conclusive results that indicate a role of IL-31 not only in the process of itching, but also its intensity. Studies show a significant reduction in itching and inflammatory symptoms [19]. Venereau et al. generated in experimental studies and gave a description of the potential antagonist for IL-31 formed by external portions of oncostatin M receptor (OSMR) and gp130-like receptor (GPL) fused with a linker, which neutralized activity of IL-31 in different bioassays [13].
Certainly, further research on the pathomechanism of pruritus in atopic dermatitis is warranted for the complete understanding of the relations described in the literature.
Conclusions
Serum IL-31 level was significantly higher in AD than in healthy children. There was no correlation between the disease severity, itch intensity and serum level of the tested cytokine.
Acknowledgments
Work funded by the Medical University of Lodz with research task No. 502-03/5-047-01/502-54-048.
References
- 1.Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Dermatol Venereol (Stockh) 1980;(92 Suppl.):44–7. [Google Scholar]
- 2.Hanifin JM, Thurston M, Omoto M, et al. The eczema area and severity index (EASI): assessment of reliability in atopic dermatitis. EASI Evaluator Group. Exp Dermatol. 1994;10:11–8. doi: 10.1034/j.1600-0625.2001.100102.x. [DOI] [PubMed] [Google Scholar]
- 3.European Task Force on Atopic Dermatitis. Severity scoring of atopic dermatitis: the SCORAD index. Dermatology. 1993;186:23–31. doi: 10.1159/000247298. [DOI] [PubMed] [Google Scholar]
- 4.Ständer S, Steinhoff M. Pathophysiology of pruritus in atopic dermatitis: an overview. Exp Dermatol. 2002;11:12–24. doi: 10.1034/j.1600-0625.2002.110102.x. [DOI] [PubMed] [Google Scholar]
- 5.Castellani ML, Salini V, Frydas S, et al. Interleukin-31: A new cytokine involved in inflammation of the skin. Int J Immunopathol Pharmacol. 2006;19:1–4. [PubMed] [Google Scholar]
- 6.Heinrich PC, Behrmann I, Haan S, et al. Principles of interleukin (IL)-6-type cytokine signalling and its regulation. Biochem J. 2003;374:1–20. doi: 10.1042/BJ20030407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dillon SR, Sprecher C, Hammond A, et al. Intreleukin 31, a cytokine produced by activated T cells, induces dermatitis in mice. Nat Immunol. 2004;5:752–60. doi: 10.1038/ni1084. [DOI] [PubMed] [Google Scholar]
- 8.Ghilardi N, Li J, Hongo JA, et al. A novel type I cytokine receptor is expressed on monocytes, signals proliferation, and activates STAT-3 and STAT-5. J Biol Chem. 2002;277:16831–6. doi: 10.1074/jbc.M201140200. [DOI] [PubMed] [Google Scholar]
- 9.Yamaoka K, Okayama Y, Kaminuma O, et al. Proteomic approach to FcepsilonRI aggregation-initiated signal transduction cascade in human mast cells. Int Arch Allergy Immunol. 2009;149:73–6. doi: 10.1159/000211376. [DOI] [PubMed] [Google Scholar]
- 10.Nobbe S, Dziunycz P, Mühleisen B, et al. IL-31 expression by inflammatory cells is preferentially elevated in atopic dermatitis. Acta Derm Venereol. 2012;92:24–8. doi: 10.2340/00015555-1191. [DOI] [PubMed] [Google Scholar]
- 11.Raap U, Wichmann K, Bruder M, et al. Correlation of IL-31 serum levels with severity of atopic dermatitis. J Allergy Clin Immunol. 2008;122:421–3. doi: 10.1016/j.jaci.2008.05.047. [DOI] [PubMed] [Google Scholar]
- 12.Metz S, Naeth G, Heinrich PC, et al. Novel inhibitors for murine and human leukemia inhibitory factor based on fused soluble receptors. J Biol Chem. 2008;283:5985–95. doi: 10.1074/jbc.M706610200. [DOI] [PubMed] [Google Scholar]
- 13.Venereau E, Diveu C, Grimaud L, et al. Definition and characterization of an inhibitor for interleukin-31. J Biol Chem. 2010;285:14955–63. doi: 10.1074/jbc.M109.049163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ezzat MH, Hasan ZE, Shaheen KY. Serum measurement of interleukin-31 (IL-31) in paediatric atopic dermatitis: elevated levels correlate with severity scoring. J Eur Acad Dermatol Venereol. 2011;25:334–9. doi: 10.1111/j.1468-3083.2010.03794.x. [DOI] [PubMed] [Google Scholar]
- 15.Kim S, Kim HJ, Yang HS, et al. IL-31 serum protein and tissue mRNA levels in patients with atopic dermatitis. Ann Dermatol. 2011;23:468–73. doi: 10.5021/ad.2011.23.4.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nobbe S, Dziunycz P, Mühleisen B, et al. IL-31 expression by inflammatory cells is preferentially elevated in atopic dermatitis. Acta Derm Venereol. 2012;92:24–8. doi: 10.2340/00015555-1191. [DOI] [PubMed] [Google Scholar]
- 17.Szegedi K, Kremer AE, Kezic S, et al. Increased frequencies of IL-31-producing T cells are found in chronic atopic dermatitis skin. Exp Dermatol. 2012;21:431–6. doi: 10.1111/j.1600-0625.2012.01487.x. [DOI] [PubMed] [Google Scholar]
- 18.Neiss MM, Peters B, Dreuw A, et al. Enhanced expression levels of IL-31 correlate with IL-4 and IL-13 in atopic and allergic contact dermatitis. J Allergy Clin Immunol. 2006;118:930–7. doi: 10.1016/j.jaci.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 19.Grimstad O, Sawanobori Y, Vestergaard C, et al. Anti-interleukin-31-antibodies ameliorate scratching behaviour in NC/Nga mice: a model of atopic dermatitis. Exp Dermatol. 2009;18:35–43. doi: 10.1111/j.1600-0625.2008.00766.x. [DOI] [PubMed] [Google Scholar]