Abstract
Introduction
As a population profoundly affected by the HIV epidemic and in critical need of linkages to HIV treatment and care, PWID in Central Asia remain largely underserved. This paper provides an overview of the current state of HIV testing and counseling in Central Asia for PWID, identifies main barriers leading to gaps in service delivery, and discusses implications for improving strategies that promote HIV testing for PWID.
Methods
We reviewed a number of sources for this paper including unpublished government reports, published papers, and Ministries of Health of Kazakhstan, Kyrgyzstan, Tajikistan, and Uzbekistan country progress reports to the UN General Assembly Special Session on HIV/AIDS (UNGASS) for 2012.
Results
Between 29 to 65% of PLWH in some Central Asian countries have been tested for HIV in the last 12 months. The rates have been increasing in the recent years but still are relatively low. Stigma, discrimination, human rights violations, and repressive legislation are barriers to HTC for people who inject drugs (PWID).
Conclusion
The use of innovative evidence-based HTC models, such as community mobile-vans, self-testing at home, and rapid HIV testing among PWID in Central Asia are discussed and recommendations given regarding amendments in legislation and scaling up of existing community-based pilot projects to support HIV testing among PWID in CA.
Keywords: HIV testing, HIV, rapid tests, PWID, Central Asia
1. INTRODUCTION
Kazakhstan, Kyrgyzstan, Tajikistan, Uzbekistan, and Turkmenistan comprise Central Asia (CA), a region that, together with Eastern Europe, has the fastest growing epidemic of HIV/AIDS in the world, with 60% of HIV infections attributed to injection drug use (Spicer et al., 2011; Jolie et al., 2012; Thorn et al., 2010). In the era of effective and early initiated antiretroviral treatment, timely detection of HIV infection and prompt linkages to HIV care and treatment are crucial for improving quality of life, preventing complications, and reducing further transmission risks (Mounier-Jack et al., 2008; Wolf et al., 2010). Furthermore, HIV voluntary counseling and testing has been associated with a reduction of injecting drug and sexual risk behaviors (Degenhardt, et al., 2010; Manuakyan et al., 2009). Despite notable advances in expanding HIV testing for key populations, the number of PWID who have been tested for HIV in the last 12 months continues to be relatively low varying from 29% in Uzbekistan to 65% in Kazakhstan, according to the countries official governmental reports (Ministries of Health of Kazakhstan, Kyrgyzstan, Tajikistan, and Uzbekistan, 2012) .The WHO European Action Plan for 2012-2015 calls for reducing the number of undiagnosed individuals by increasing early uptake of HIV VCT services and sets as a target of no less than 90% of PWID aware of their HIV status by 2015. We reviewed a number of sources for this paper including countries HIV laws, government reports, published papers, and country progress reports to the UN General Assembly Special Session on HIV/AIDS (UNGASS) for 2007-2012.
This paper examines HIV testing policies and strategies for PWID in CA, addresses a number of structural barriers affecting HIV testing among PWID in CA, and discusses strategies that governments in the region should take to improve HIV testing among PWID.
2. HIV TESTING POLICIES AND STRATEGIES IN CA FOR PWID
The governments of each of the five Central Asian countries have expressed a commitment to work toward providing access to voluntary and confidential HIV testing for all people by adopting human rights legislation, international treaties, and specific national laws. All countries, except for Kazakhstan, have specific HIV programs. In Kazakhstan, HIV is mentioned as one of the strategic directions with in the overall national healthcare development program “Salamatty Kazakhstan,” 2011-2015. In theory, these existing policies guarantee full protection of human rights of PWID, by including anti-discriminatory provisions and provisions on informed consent, voluntary nature, and confidentiality of medical information (UNODC, 2010). However, there are wide provisions for mandatory and compulsory HIV testing of PWID under other HIV-related policies (i.e., ministerial and departmental instruction, guidelines, and orders) mandating HIV testing in all five countries (UNODC, 2010).
There is also a regional variability in legislation with regards to informed consent, counseling and confidentiality. Although as a general rule, laws require informed consent for HIV testing, the practice of obtaining such consent varies widely across the region. For instance, Kyrgyzstan is the only country requiring written informed consent (Government of the Kyrgyz Republic, 2006). In Turkmenistan, the law guarantees access to free, confidential and anonymous HIV testing but does not require informed consent (Government of Turkmenistan, 2005). In Uzbekistan, the law provides for voluntary and anonymous HIV testing with guaranteed confidentiality (Government of Uzbekistan, 2007). Counseling is provided by law in all Central Asian countries but is limited due to a shortage of trained counselors. Information about HIV status can be shared without the patient's consent and proper justification with law enforcement agencies and health facilities beyond AIDS Centers (UNOCD, 2010).
PWID are often subject to involuntary and mandatory HIV testing. The list of conditions for mandatory HIV testing of PWID in Kazakhstan include: partners using injection drugs together and registration in narcological services every 6 months (Ministry of Health of Kazakhstan, 2004). For detained and imprisoned PWID, despite national HIV laws in all countries, except for Turkmenistan, provides for voluntary HIV testing, there are subsequent contradictory provisions in orders from the Ministry of Health, Justice and/or Internal Affairs that impose compulsory testing during an entry into the prison system, 6 months later, and prior to release (UNICD, 2010). HIV testing of prisoners is involuntary in Turkmenistan.
WHO and UNAIDS strongly recommend anonymous voluntary HIV counseling and testing (VCT) for PWID (WHO, UNODC, 2009). Anonymous HIV testing is widely available in Kazakhstan and Kyrgyzstan and only recently in Tajikistan, when the new HIV protocol was issued (Ruziev, 2011, Soliev, 2011). VCT is being offered through a network of needle exchange programs (NEPs) and VCT clinics.
3. STATUS OF ACCESS TO HIV TESTING AMONG PWID IN CA
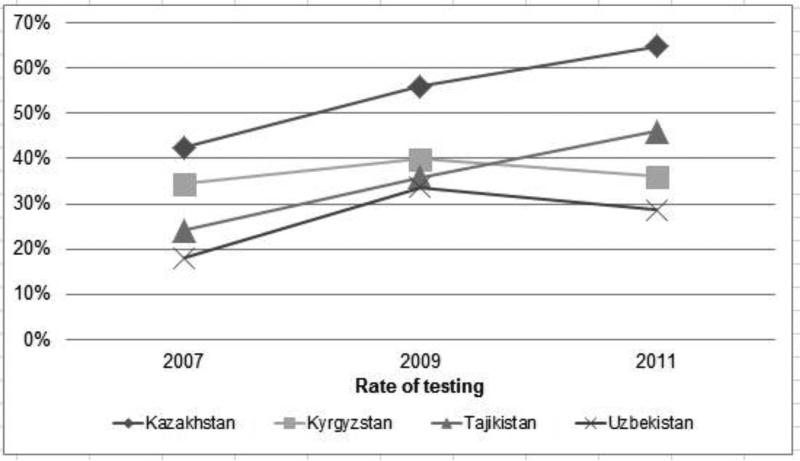
Rates of HIV testing among PWID in Central Asia has grown in recent years due to the programmatic efforts of the Global Fund recipients and others. Furthermore, rapid testing finally became available in 2009 (Manukyan et al., 2009). Reports from the national AIDS Centers Integrated Biobehavioral Surveys (IBBS) among PWID conducted annually in all CA countries show that the proportion of PWID who were tested for HIV over the last 12 months and know their HIV status varies across the region from very low (28.7%) in Uzbekistan to moderate (65%) in Kazakhstan (see Table 1). From 2009 to 2011, these rates have increased in Kazakhstan (from 52% to 65%) and in Tajikistan (from 40% to 54%) but dropped in Kyrgyzstan and Uzbekistan although insignificantly (see Figure 1; Ministries of Health of Kazakhstan, Kyrgyzstan, Tajikistan, and Uzbekistan, 2012). These figures are the percentages of people tested among the total sample of PWID included in the IBBS surveys. The sample sizes in each site were calculated based on HIV prevalence among PWID in the previous year and the estimated numbers of PWID. Because the government-run sentinel surveillance study samples consisted heavily of clients of HIV prevention services rather than non-clients, the figures should be considered with a degree of caution. The survey among non-clients showed significantly lower rates of HIV testing: 30% (Manukyan et al., 2009).
Table 1.
HIV Testing and Treatment among PWID
| Kazakhstan | Kyrgyzstan | Tajikistan | Uzbekistan | Turkmenistan | References | |
|---|---|---|---|---|---|---|
| Number of PWID (estimated/registered) | 186 | 44,000/1, | 25,000 (2009) | 80 | 11,148 | Country official reports (Form#4), 2012 |
| Proportion of drug users among tested for HIV | 1.5% | N/A | 1.7% | N/A | National AIDS Centers, IBBS surveys | |
| Proportion of PLWH among PWID | 3.8% | 14.6% | 13.5% | 8.4% | N/A | Ministry of Health Country progress report, 2012 |
| Proportion of PWID among PLHIV | 63% | 62% | 50.4% | 44.6% | ||
| Proportion of PWID, who were tested for HIV over the last 12 months and know their HIV status | 64.7 | 54% | 46.0% | 28.7% | N/A | Ministry of Health Country progress report, 2012 |
| HTC strategies available for PWID | Anonymous VCT (NEPs) community-based VCT (mobile vans, rapid tests) Mandatory and compulsory testing |
Anonymous VCT (NGOs) community-based VCT (rapid tests) Mandatory and compulsory testing |
Voluntary Counseling and testing Mandatory and compulsory testing |
Voluntary Counseling and testing Mandatory and compulsory testing |
N/A | National AIDS Centers |
Figure 1.
HIV testing among PWID in four Central Asian countries
4. STRUCTURAL BARRIERS TO HIV TESTING AMONG PWID
Studies around the world showed that multiple complex and interrelated structural barriers explain the low levels of HIV testing among PWID (Spicer et al., 2011). Existing HIV laws throughout CA fail to ensure that important services are made available in ways that respect and promote human rights of PWID (UNODC, 2010). Consent, confidentiality and counseling, frequently referred to as “the three C's” of HIV testing represent important human rights protections for people seeking and undergoing this procedure, are often violated throughout CA.
Criminalization of drug use and discriminatory practices among government service providers restrict access of PWID to NEPs and NGOs where HIV testing services are located. Based on interviews with drug users in Kazakhstan, Human Rights Watch (2007) reported that police often arrest clients of harm reduction services, confiscate drugs and syringes and extract bribes for possession of syringes/needles..
Medical staff and government health care providers also often stigmatize and discriminate against PWID, which results in negative experiences and lower levels of trust in what the services can offer. A long Soviet tradition of using health facilities for mandatory HIV testing without ensuring confidentiality of the test results contributes to the unattractiveness of these services to PWID (Human Rights Watch, 2007). Viale (2010), in her assessment of barriers to HIV testing among PWID in Kazakhstan, reports fear of their HIV status being made known through breaches in confidentiality, and a consequent backlash from families and communities preventing PWID from accessing VCT services. Lack of anonymous and confidential counseling in Kyrgyzstan for PWID was indicated as a reason for the decrease in HIV testing among this group (Olga Tylyakova, personal communication).
There are a number of organizational barriers to accessing government-run clinic-based VCT services for PWID in CA such as inconvenient hours, distant locations, and transportation costs (Deryabina, 2011). Other factors affecting availability and quality of pre- and post-test counseling include limited human resources specifically devoted to VCT, low VCT staff motivation, and limited qualifications and training (CAAP, 2010).
5. RESEARCH-BASED FACTORS AND INNOVATIVE STRATEGIES TO IMPROVE ACCESS TO HIV TESTING AMONG PWID IN CA
In our recent study with PWID in Kazakhstan, incarceration, a history of drug treatment, and utilization of syringe exchange programs were significantly associated with being tested for HIV: 72.2% of participants who indicated having an HIV test also reported an arrest in the past 90 days (p<0.001), 34.7% a history of drug treatment (p<0.001); and 12.9% reported participation in a syringe-exchange program (p<0.05). In a study in Russia, Niccolai et al. (2010) reported that PWID who recently visited a doctor have been significantly more likely to have recent testing (OR = 3.06, 95% CI=1.68 – 5.59, P<0.001). Niccolai et al. (2010) also reported gender-based differences in accessing HIV testing. Among men, having a physician visit in the past 12 months (OR = 3.66, 95% CI = 1.75–7.70, P\.01) and a history of incarceration (OR = 2.12, 95% CI = 1.08–4.42, P\.05) were associated with recent testing. Among women, having ever been pregnant was marginally associated (OR = 3.56, 95% CI = 0.74–17.2, P\.10). Clearly, wider and unrestricted access to medical care, drug treatment, harm reduction programs, and other medical and social services would lead to expanded access to HIV counseling and testing for PWID (El-Bassel, et al., in press).
A number of strategies that have been found to improve HIV testing coverage for PWID need to be scaled up in CA. Globally, peer-driven navigation, community, rapid and home-based HIV testing have been conducted in Africa for over a decade. Yet, these strategies are novel to CA and only a few have been recently introduced as pilots in some CA countries (see Table 1). Still, home-based self-testing for HIV is not available in CA.
An important strategy is a scale up of the community-based HIV testing with a use of mobile vans and rapid testing. Kazakhstan Ministry of Health (2012) reports 23 mobile NEPs covering 6% of all IDUs clients of HIV prevention programs in 2012 as compared to 5% in 2011. HIV rapid testing is currently available only in Kazakhstan and Kyrgyzstan. HIV rapid tests were used for 51% of all PWID who were tested for HIV through NEPs in Kazakhstan in 2012 (Ministry of Health of Kazakhstan, 2012). In November 2012, UNDP, with technical assistance from the USAID-funded Quality Healthcare Project, began to pilot a rapid HIV testing program with oral-fluid tests (OraQuick, USA) among non-governmental organizations (NGOs) serving MARPS in Kyrgyzstan (Daniyar Saliev, personal communication). From November 2012 until May 2013, 1810 PWID were tested for HIV using OraQuick, of which 131 (7.2%) tested positive. If the result of the screening rapid test was positive, the person was referred to the AIDS Center for confirmatory diagnostics and treatment, as needed.
6. CONCLUSION
HIV testing among PWID in CA remains comparatively low, with 35-65% of PWID in some CA countries not being tested for HIV in the last 12 months, as reported in official governmental documents. This situation demands immediate attention, amendments to laws, and scale up of existing effective initiatives. The laws and ministerial instructions should be changed to eliminate coercive HIV testing while ensuring complete confidentiality and informed consent. Providing wider and unrestricted access to medical, drug treatment, and harm reduction services to PWID will result in expanded access of PWID to HIV testing. Health and law enforcement agencies should get advanced training on the importance of HIV testing for early antiretroviral treatment, improved quality of life, prevented complications, and reduced further transmission risks. Effective strategies suggested to improve access to HIV testing in CA are community-based mobile vans and utilization of rapid HIV tests. Among the four CA countries, Kazakhstan has the highest coverage PWID with HIV testing. We speculate that this is the result of the country's utilization of the community-based testing strategies, including mobile vans and rapid tests. However, with only a few of the pilot community-based HIV testing programs in the region, the current extant of such efforts are inadequate and need to be scaled up.
Acknowledgments
Role of funding source
Nothing declared.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Terlikbayeva A. conceptualized the paper and wrote the first draft. Zhussupov, Primbetova, collected data and prepared tables and graphs. El-Bassel, Gilbert, Zhussupov and Primbetova reviewed the drafts and provided feedback. Atabekov, Giyasova, Ruziyev, and Soliyev collected the country data. All authors participated in approving the final version of the article.
Conflict of interest
No conflict declared.
REFERENCES
- Central Asia AIDS Control Project (CAAP) Assessment and evaluation of capacity of medical facilities to conduct provider-initiated VCT. 2010 [Google Scholar]
- Saliev Daniyar. UNDP Kyrgyzstan, personal communication on June 20th, 2013. [Google Scholar]
- Degenhardt L, Mathers B, Vickerman P, Rhodes T, Latkin C, Hickman M. Prevention of HIV infection for people who inject drugs: why individual, structural, and combination approaches are needed. Lancet. 2010;376:285–301. doi: 10.1016/S0140-6736(10)60742-8. [DOI] [PubMed] [Google Scholar]
- Deryabina A. Mapping of Key HIV Services, Assessment of Their Quality, andAnalysis of Gaps and Needs of Most-at-Risk Populations in Chui Oblast and Bishkek City, Kyrgyzstan. USAID's AIDS Support and Technical Assistance, Resources, AIDSTAR-One, Task Order 1; Arlington, VA: 2011. [Google Scholar]
- El-Bassel N, Gilbert L, Terlikbayeva A, Wu E, Beyrer C, Shaw S, Hunt T, Ma X, Chang M, Ismayilova L, Tukeyev M, Zhussupov B, Rozental Y. HIV among injection drug users and their intimate partners in Almaty. Kazakhstan: in press AIDS Behav. DOI 10.1007/s10461-013-0484-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Tajikistan On Procedure of testing in order to identify persons infected with HIV, their registration, medical assistance to and preventive care of people living with HIV, and the list of people obliged to undergo mandatory confidential HIV testing on epidemiological indications, Resolution No. 171. 2008.
- Government of the Kyrgyz Republic Law On HIV/AIDS, Article 8, Rules for medical examination to detect HIV, medical registration and observation of people with positive and ambiguous HIV tests in the Kyrgyz Republic”, Government Resolution No. 296. 2006.
- Government of Turkmenistan Law of Turkmenistan On prevention of HIV (2005 – 2010), Article 5. 2005.
- Government of Uzbekistan Strategic Program Against HIV Infection in the Republic of Uzbekistan for 2007 – 2011, approved by the Deputy Prime Minister of the Republic of Uzbekistan, Order No 07/10-115) 2007.
- Human Rights Watch, Fanning the Flames, supra, p. 18; see also J. Csete, Do Not Cross:Policing and HIV Risk Faced by People Who Use Drugs. HIV/AIDS Legal Network; Toronto: Canadian: 2007. online via www.aidslaw.ca/drugpolicy. [Google Scholar]
- Jolley E, Rhodes T, Platt L, Hope V, Latypov A, Donoghoe M, Wilson D. HIV among people who inject drugs in Central and Eastern Europe and Central Asia: a systematic review with implications for policy. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2012-001465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manukyan A, Beletsky L, Toussova O, Birgin R, Burrows D. Report on Project: Support to National AIDS Response to Scale Up HIV Prevention and Care Services in Tajikistan. APMG; Sydney: 2009. [Google Scholar]
- Ministry of Health of Kazakhstan Rules “Regarding Medical Examination of Citizens for The Detection of Infection with Human Immunodeficiency Virus ”. 2004 2002 Jun 11;(227) Orders No 575. [Google Scholar]
- Ministry of Health of Kazakhstan [April, 29, 2013];Country progress report 2012. 2012 http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_KZ_Narrative_Report.pdf.
- Ministry of Health of Kyrgyzstan [April 29, 2013];Country progress report 2012. 2012 http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_KG_Narrative_Report_0.pdf.
- Ministry of Health of Tajikistan [April 29, 2013];Country progress report 2012. 2012 http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_TJ_Narrative_Report[1].pdf.
- Ministry of Health of Uzbekistan [April, 29, 2013];Country progress report 2012. 2012 http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/Uzbekistan%202012%20Progress%20Report%20Rus.pdf.
- Mimiaga MJ, Safren SA, Dvoryak S, Reisner SL, Needle R, Woody G. We fear the police, and the police fear us: structural and individual barriers and facilitators to HIV medication adherence among injection drug users in Kiev, Ukraine. AIDS Care. 2010;22:1305–1313. doi: 10.1080/09540121003758515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mounier, Jack S, Nielsen S, Coker RJ. HIV testing strategies across European countries. HIV Med. 2008;9:13–19. doi: 10.1111/j.1468-1293.2008.00585.x. [DOI] [PubMed] [Google Scholar]
- Niccolai LM, Toussova OL, Verevochkin SV, Barbour R, Heimer R, Kozlov AP. High HIV Prevalence, Suboptimal HIV testing, and low knowledge of HIV-positive serostatus among injection drug users in St. Petersburg, Russia. AIDS Behav. 2010;14:932–941. doi: 10.1007/s10461-008-9469-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olga Tylyakova, Parents Against Drugs, Kyrgyzstan, personal communication on June 21st, 2013 [Google Scholar]
- Ruziev M. Review of HIV epidemiological situation in Tajikistan. Materials of the Regional research conference on HIV/AIDS in FSU countries. The Tajikistan Health Care; Dushanbe: Dec 5-6, 2011. 2011. pp. 34–39. [Google Scholar]
- Soliev A. Epidemiological characteristic of HIV infection in Tajikistan. Materials of the Regional research conference on HIV/AIDS in FSU countries. The Tajikistan Health Care; Dushanbe: Dec 5-6, 2011. 2011. pp. 94–95. [Google Scholar]
- Spicer N, Bogdan D, Brugha R, Harmer A, Murzalieva G, Semigina T. It is risky to walk in the city with syringes: understanding access to HIV/AIDS services for injecting drug users in the former Soviet Union countries of Ukraine and Kyrgyzstan. Growth. 2011;1:1–13. doi: 10.1186/1744-8603-7-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorne C, Ferencic N, Malyuta R, Mimica J, Niemiec T. Central Asia: hotspot in the worldwide HIV epidemic. Lancet Infect. Dis. 2010;10:479–488. doi: 10.1016/S1473-3099(10)70118-3. [DOI] [PubMed] [Google Scholar]
- UNAIDS [April 23, 2013];AIDS Epidemic Update. Geneva: UNAIDS. 2004 from http://whqlibdoc.who.int/unaids/2004/9291733903.pdf. [Google Scholar]
- UNODC Accessibility of HIV Prevention, Treatment and Care Services for People who use Drugs and Incarcerated People in Azerbaijan, Kazakhstan, Kyrgyzstan, Tajikistan,Turkemenistan and Uzbekistan: Legislative and Policy Analysis. Ashgabat, Turkemenistan. 2010.
- UNDP Reversing the Epidemic: HIV/AIDS in Eastern Europe and the Commonwealth of Independent States (UNDP Regional Office for Eastern Europe and the CIS. 2004:55. [Google Scholar]
- Viale BN. [April 29, 2013];How perceived barriers to voluntary counseling and testing impact actual HIV testing among injection drug users in Kazakhstan. Dissertation. 2010 from: http://sdsu-dspace.calstate.edu/handle/10211.10/624.
- WHO, UNAIDS [April 29, 2013];Guidance on testing and counseling in settings attended by people who inject drugs. Improving access to treatment, care, and prevention. 2009 http://www.who.int/hiv/pub/idu/searo_wpro_tc/en/ [PubMed] [Google Scholar]
- Wolfe D, Carrieri MP, Shepard D. Treatment and care for injecting drug users with HIV infection: a review of barriers and ways forward. Lancet. 2010;376:355–366. doi: 10.1016/S0140-6736(10)60832-X. [DOI] [PubMed] [Google Scholar]