Abstract
Free fibula transfer can be associated with a slow and tedious dissection/harvest due to difficulty in visualizing the deeper structures. The purpose of this article is to review the first author's (Y.D.) experience with a novel technique for expedited harvest of fibula free flaps for mandibular reconstruction. A retrospective chart review was performed using the first author's clinical practice using chart data from September 1997 to August of 2007. All patients with available chart data who had undergone free fibular transfer for oromandibular reconstruction were included in this study. Charts that met the specified inclusion criteria were reviewed for patient demographic information, reason for free tissue transfer, flap loss rates (partial and total) and reasons for flap loss, average fibula harvest time (tourniquet time), and foot and ankle function postoperatively. During this time, a total of 283 fibula free flaps were performed in 276 patients. The average fibula harvest time (tourniquet time) for all cases was 22.6 minutes, with a range of 14 to 29 minutes. A total of 13 flaps were unsuccessful (failure rate of 4.6%, with 5 total and 8 partial flap losses). This newly described technique will allow for expedited and simplified harvest of fibula free flaps.
Keywords: free fibula, fibula harvest, tunneling technique, mandibular reconstruction
Free fibula transfer was originally described in 1975 by Taylor et al for reconstruction of an open fracture of the leg.1 At this time, he raised the flap through a posterior approach. Later on, Gilbert is credited with the more commonly used lateral approach.2 All of these were nonskin-bearing flaps. Chen and Yan were the first to delineate the successful use of osteomyocutaneous fibula free tissue transfer, which Hidalgo later applied to mandibulectomy defects.3 4 The downside to this beneficial procedure is the need for specialized training and expertise, as well as the significant operative time required for tissue dissection and harvest. In this article, we will describe our successful technique for fibula free tissue harvest that we have found to be safe, expeditious, and easy to both perform and teach to residents.
Materials and Methods
Study Design
A 10-year retrospective chart review was performed using the first author's (Y.D.) clinical practice. All patients with available chart data who had undergone free fibular transfer for oromandibular reconstruction were included in this study.
Technique
The flap is designed by centering it along a vertical line approximately 1 cm anterior to the palpable position of the posterior intermuscular septum, which is generally more anterior than is appreciated by palpation alone. The skin paddle, if needed, is oriented lengthwise and is centered over this line or somewhat posterior to it (Fig. 1). Under tourniquet control of 350 mm Hg, the skin paddle is incised circumferentially and relaxing incisions carried inferiorly to within 5 to 6 cm of the ankle mortise and superiorly to within 4 cm of the head of the fibula taking care to be aware of and avoid the peroneal nerve in this region. The incision is carried right down to the peroneal muscles. Dissection is then carried posteriorly to the intermuscular septum within which lie the septocutaneous perforators (Fig. 1).
Figure 1.
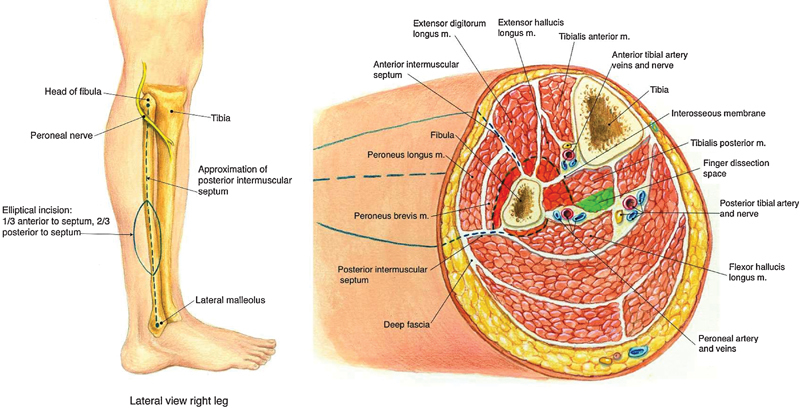
Topographical anatomy and cross-sectional anatomy of the lower leg demonstrating approximate position of the finger dissection tunnel medial and anterior to the pedicle.
Metzenbaum scissors are then used to serially section the peroneus longus and brevis muscles from the anterolateral aspect of the fibula bone, with the surgeon's nondominant thumb hooking the resected muscles anteriorly out of the way (Fig. 2). Next a small perforation is made in the central portion of the interosseous membrane (Fig. 2). A finger is then passed into this perforation and run superiorly and inferiorly along the length of the fibula to release the membrane completely in the zone of anticipated fibula harvest (Fig. 3).
Figure 2.
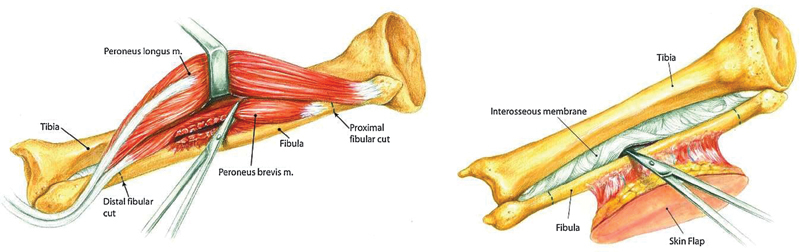
The left figure demonstrates retraction of the peroneus longus and scissors section of the brevis from the fibula. This will result in preservation of the periosteum by leaving a few millimeters of brevis on the fibula bone. The right figure demonstrates release of the interosseous membrane by sharp incision centrally, first.
Figure 3.
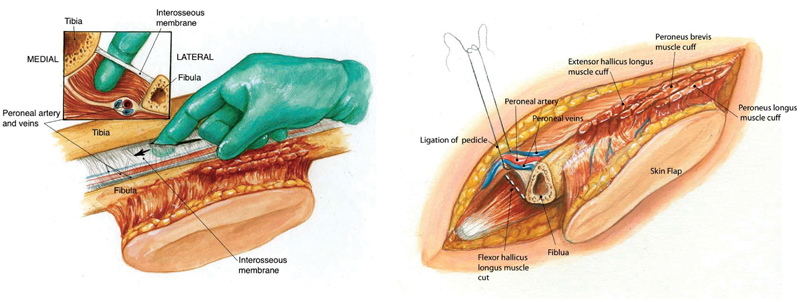
The surgeon's finger then slides superiorly and inferiorly along the length of the fibula bone that is planned for harvest, releasing the interosseous membrane (left). Once the proximal and distal osteotomy is made in the fibula bone, the pedicle is controlled with ties or clips distally (right).
Next, a periosteal elevator is used to elevate the periosteum around the fibula bone circumferentially both proximally and distally in the area of proposed osteotomy. The elevator is then placed medial to the bone in the area of elevated periosteum to help protect the pedicle. An oscillating saw is then used to perform an osteotomy distally then proximally. The hallucis longus muscle is then sectioned and the distal pedicle controlled with hemoclips (Fig. 3). The tunnel of dissection deep to the tibialis posterior and medial to the vessels is then entered easily. This is a loose areolar, avascular plane that runs superiorly to the takeoff of the peroneal artery in all cases. The scissors are then used to section the tibialis posterior muscle superficial to the index finger which rests within the dissection tunnel (Fig. 4). Once the takeoff of the peroneal is identified, it is typically noted to course medially. At this point, the posterior muscle cuts are made from inferior to superior. Muscular perforators are often noted in this region and should be controlled with hemoclips or ties. Now, the fibula osteomyocutaneous flap should be pedicled just on the peroneal artery and its paired venae comitantes (Fig. 4). The tourniquet is removed and the pedicle is tied off once vascularity is verified.
Figure 4.
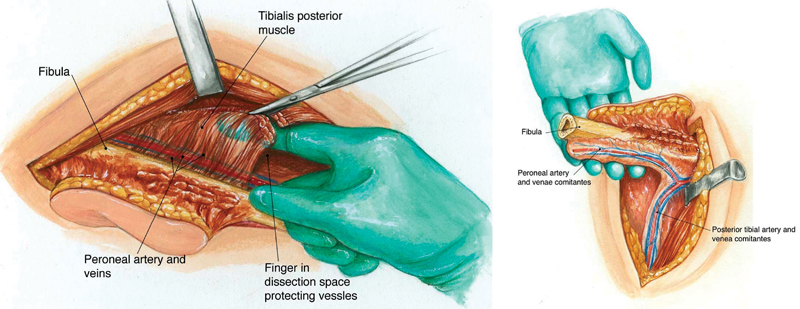
Dissection space is entered inferiorly with the surgeon's finger, protecting the pedicle laterally (left). Pedicle is traced proximally following tunnel to its origin. The tunnel leads directly to the peroneal take-off, veering medially, naturally, and consistently (right).
A demonstration of the senior author's method for free fibula tissue harvest can be seen in the supplemental video file.
Video
A demonstration of the senior author's (Y.D.) method for free fibula tissue harvest can be seen in this supplemental video file. Online content including video sequences viewable at: www.thieme-connect.com/ejournals/html/10.1055/s-0033-1349208
Chart Review
Charts that met the specified inclusion criteria were reviewed for patient demographic information, reason for free tissue transfer, flap loss rates (partial and total) and reasons for flap loss, average fibula harvest time (tourniquet time), and foot and ankle function postoperatively.
Results
A total of 283 fibula free flaps were performed in 276 patients. The male:female ratio was 188:88 with an average age of 62.4 years (range 8 to 94 years). The reason for free tissue transfer included status following extirpative oncologic surgery (both for aggressive benign and malignant pathology) in 212 cases, osteoradionecrosis in 53 cases, and following traumatic loss in 18 cases. A total of 13 flaps were unsuccessful (failure rate of 4.6%) with 5 complete flap losses and 8 partial flap losses (skin paddle only). Of the 13 partial and total flap losses, postoperative hypotension (n = 5), cardiac arrest (n = 3), hematoma (n = 2), and wound infection (n = 3) were felt to be causative factors. Average fibula harvest time (tourniquet time) was 22.6 minutes with a range of 14 to 29 minutes. Foot and ankle function following fibula free tissue harvest was noted to be excellent long-term, as was previously reported in a small subset of these patients by the first author (Y.D.).5
Discussion and Conclusion
One of the primary concerns for the novice surgeon with harvest of the free fibula flap is concern over damage to deeper structures during dissection. The inability to visualize the pedicle and other neurovascular structures in the small confined spaces of the lower leg tends to slow the dissection. Because of this, the senior author (Y.D.) has developed a harvest technique employing the “blind” development of tunnels along natural planes that ensure that division of the more superficial layers of the flap can be accomplished without risk to the deeper components. It also places the intramuscular feeding vessels under tension, allowing for clear visualization and control.
Through the use of this procedure, one of the major drawbacks of free tissue transfer, that is, increased anesthesia time can effectively be overcome. This can subsequently allow for this once lengthy procedure that required a “two-team” approach to be easily performed by one surgeon due to the reduced time required to raise the fibula flap.
References
- 1.Taylor G I, Miller G DH, Ham F J. The free vascularized bone graft. A clinical extension of microvascular techniques. Plast Reconstr Surg. 1975;55(5):533–544. doi: 10.1097/00006534-197505000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Gilbert A. Vascularized transfer of a fibula shaft. Int J Microsurg. 1979;1(2):100–102. [Google Scholar]
- 3.Chen Z W, Yan W. The study and clinical application of the osteocutaneous flap of fibula. Microsurgery. 1983;4(1):11–16. doi: 10.1002/micr.1920040107. [DOI] [PubMed] [Google Scholar]
- 4.Hidalgo D A. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg. 1989;84(1):71–79. [PubMed] [Google Scholar]
- 5.Garrett A, Ducic Y, Athre R S, Motley T, Carpenter B. Evaluation of fibula free flap donor site morbidity. Am J Otolaryngol. 2006;27(1):29–32. doi: 10.1016/j.amjoto.2005.07.003. [DOI] [PubMed] [Google Scholar]


