Abstract
Diabetes mellitus has emerged as one of the fastest growing non communicable diseases worldwide. Management of diabetic patients during surgical and critically illness is of paramount challenge to anesthesiologist and intensivist. Among its major acute complications, hypoglycemia has been given lesser attention as compared to other major acute complications; diabetic ketoacidosis and hyperosmolar non ketotic coma. However, newer studies and literary evidence have established the serious concerns of morbidity and mortality, both long- and short-term, related to hypoglycemia. basis. Invariably, diabetic patients are encountered in our daily routine practice of anesthesia. During fasting status as well as the perioperative period, it is hypoglycemia that is of high concern to anesthesiologist. Management has to be based on clinical, pharmacological, social, and psychological basis, so as to completely prevent the complications arising from an acute episode of hypoglycemia. This review aims to highlight various aspects of hypoglycemia and its management both from endocrine and anesthesia perspective.
Keywords: Diabetes mellitus, hyperglycemia, hypoglycemia, insulin, insulin analogues
INTRODUCTION
Diabetes has become one of the leading causes of global burden of diseases, as described recently in the Lancet.[1] The increasing prevalence of diabetes mellitus (DM) has a significant impact on anesthesiology practice as it can directly and indirectly impact outcome in surgical patients. A strong need is felt among the endocrinologists, anesthesiologists, and intensivists to work in unison so as to manage the increasing number of surgical and critically ill patients with DM. A universal consensus on therapeutic management strategies in surgical and critically ill diabetic patients is mandatory among these specialties to counter this ever increasing burden of DM.
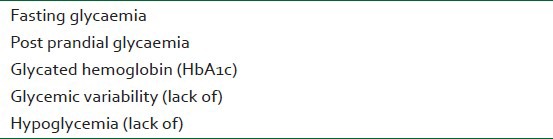
The challenges for anesthesiologists and the intensivists are manifold during the perioperative period and critical care of diabetic patients. Hypoglycemia is perhaps one of the most dreaded complications encountered among surgical and critically ill diabetic patients.[2,3] As newer drugs are made available, to use in an ever-widening array of permutations and combinations, the risk of hypoglycemia rises. This is especially so in the modern climate of result-oriented praxis, focusing on the end result of achieving the glycemic trial of glycated hemoglobin (HbA1c), fasting glycemia, and postprandial glycemia. In a bid to achieve the therapeutic targets of tight glycemic control, glycemic variability (GV), and hypoglycemia are often neglected clinical entities by the proponents of this numerophile strategy.[4] To improve surgical out come in diabetic patients, a cautious and treaded approach is highly desirable by laying stress on all the five components of the Glycemic Pentad [Table 1] so as to minimize the complication rates and thereby decreasing the overall morbidity and mortality in operative and critical care settings.
Table 1.
The glycemic pentad
Search strategies
This review is compiled to highlight the basic and essential clinical measures to prevent hypoglycemia in operative and critical care settings. The measures adopted included extensive scrutiny of literary evidence from internet resources, journals, and textbooks of endocrinology, anesthesiology and intensive care among endocrinologists, anesthesiologists and intensivists of high academic caliber. The strategies included exploration of full text articles and abstracts from various search engines such as PubMed, Medscape, Scopus, Science Direct, Medline, Yahoo, Google Scholar, using the key words: DM, glycemic control, hyperglycemia, hypoglycemia, and insulin.
Definition
The theoretical and practical variability in our day to day clinical practice while treating diabetes involve recommendations and definitions by various professional and regulatory bodies that differ in their cut off levels for the definition of hypoglycemia. According to the definition given by the American Diabetes Association (ADA), hypoglycemia can be defined as ‘any abnormally low plasma glucose concentration that exposes the subject to potential harm’, and proposes a threshold of more than 70 mg%.[5] However, the European school of clinical practice recommends a lower threshold of more than 60 mg% for definition of hypoglycemia.[6]
Epidemiology of hypoglycemia in clinical practice
Data pertaining to incidence of hypoglycemia in surgical and critically ill patients is highly variable across the nations that can possibly be attributed to nonuniform reporting, diversity of diabetes, wide spectrum of therapeutic regimens to control glycemia, demographic, and ethnic variations. The Diabetes Audit and Research in Tayside, Scotland (DARTS) study reported a prevalence of hypoglycemia of 7.1% in type 1 DM patients, 7.3% in type 2 DM patients on insulin, and 0.8% in those on oral sulfonylurea.[7] ‘OBSTACLE’, one of the major hypoglycemia studies in Asia, has reported a prevalence of hypoglycemia to the extent of 41.37% in persons taking sulfonylurea therapy for type 2 diabetes.[8]
Classification of hypoglycemia
Depending upon the presence or the absence of symptoms and corroborative glucose monitoring results, hypoglycemia can be classified as being biochemical, symptomatic, or both.[5] This classification is more or less based on the consensus of work group of American Diabetic Association (ADA) according to which a hypoglycemic episode can be classified as follows.
Severe hypoglycemia – the hypoglycemic episode in which active administration of carbohydrate, glucagon, or application of other resuscitative measures are required with an assistance of another person can be classified as severe hypoglycemia
Documented symptomatic hypoglycemia – a combination of measured plasma glucose concentration greater than equal to 70 mg/dl, accompanied by typical symptoms of hypoglycemia constitutes documented symptomatic hypoglycemia
Asymptomatic hypoglycemia – however, measured plasma glucose concentration more than equal to 70 mg/dl not accompanied by any of the known typical symptomatology of hypoglycemia can be labeled as asymptomatic hypoglycemia
Probable symptomatic hypoglycemia – an event during which symptoms of hypoglycemia are not accompanied by a plasma glucose determination (but that was presumably caused by a plasma glucose concentration greater than equal to 70 mg/dl)
Relative hypoglycemia – the presence of any of the typical symptoms of hypoglycemia in a known diabetic patient that are interpreted by the patient himself as an indication of hypoglycemia but with a measured plasma glucose concentration greater than equal to 70 mg/dl can be termed as relative hypoglycemia.
Clinical impact and significance
The face of hypoglycemia is much gloomier than is actually perceived in our daily routine operative and critical care practice. It should not be seen just as an acute complication of DM or a momentary uncomfortable symptom tobe tolerated. Rather, this acute phase complication of DM can be termed as a disease in itself if it is analyzed in the frame of biopsychosocial model of disease. It has significant clinical, biological, and psychological effects that can possibly enhance the morbidity and mortality in surgical diabetic patients if not managed appropriately [Table 2].
Table 2.
Biopsychosocial effects of hypoglycemia during perioperative, postoperative, and rehabilitation period
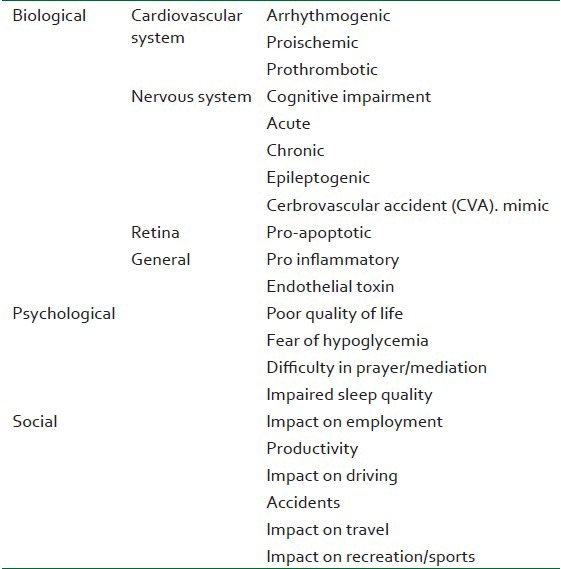
Previous studies have reported the facts that hypoglycemia can possibly enhance mortality to the extent of six-fold, increase costs of medical care, and loss of productivity due hypoglycemia. The landmark study of ‘Tight Glycemic Control’ by Van den Berghe was challenged by many researchers on account of higher mortality due to higher incidence of hypoglycemia in their respective studies.[9,10,11,12] One large study is the NICE sugar control study that has highlighted a negative role of hypoglycemia in enhancing the mortality and morbidity in critically ill diabetic patients.[12] Further there has been evidence that episodes of hypoglycemia can lead to prolonged ICU/hospital stay. The length of stay (LOS) in hospital was observed to be higher (2.8 days) on univariate analysis in diabetic patients with even a single episode of hypoglycemia as compared to patients who did not have any episode of hypoglycemia (P<0.0001).[13]
Causes and risk factors
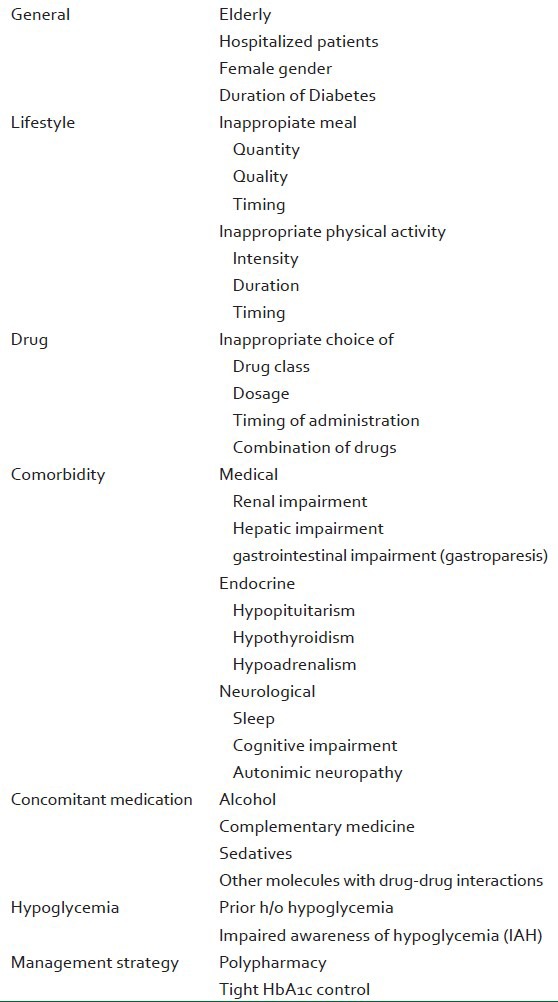
It is general perception that hypoglycemia is benign and is invariably associated with management of DM. In-depth knowledge and awareness of potential risk factors that can possibly induce hypoglycemia can help minimize the frequency of its occurrence. Factors such as lifestyle, medical, time on intensive insulin therapy, need for the dialysis, imbalance of time of nutritional supplementation and administration of required insulin, hemodynamic instability requiring vasopressors, sepsis, concurrent medical illnesses, and other drug related causes are highly associated with risk of hypoglycemia in surgical and critically ill patients.[14,15] Ironically, most of the factors that can cause hypoglycemia in operative and critically ill patients are modifiable or manageable and many of them require only educational, as opposed to pharmacological, interventions [Table 3].
Table 3.
Causes and risk factors of hypoglycemia anticipated during preanesthetic evaluation
Clinical symptomatology and evidence-based clinical outcome
The severity of hypoglycemia is considered to be an independent predictor of mortality in patients with or without diabetes but the mortality rates are significantly higher in diabetic patients.[16,17,18] In one of the large studies, it was observed that diabetic patients showed higher mortality and lower intolerance to fluctuating blood glucose values between 4.4-6.1 mmol/l; OR (95% CI) 0.33 (0.10-1.16, P=0.08) and 0.45 (0.18-1.14, P=0.09).[19] However, the variability in severity of hypoglycemia, difficulties in accurate monitoring of blood glucose, variable time interval between monitoring, patient specific factors, institutional protocols, and variable clinical state of the patient make the exact calculation of mortality associated with hypoglycemia an uncertain entity and thereby producing conflicting results.[20,21,22] Hypoglycemic episode and glycemic variability are associated with higher mortality ratio.[23,24,25,26] Hypoglycemic symptoms are often ill-recognized during surgical procedures due to hemodynamic variability and blunting by anesthetic agents while under general anesthesia, reporting of hypoglycemia is not possible.[27] The added responsibilities of an anesthesiologist, and performance of multiple concurrent tasks during surgical procedures hardly allows an anesthesiologist to accurately ensure the sampling frequency and point of care (POC) monitoring of blood glucose levels.[28] One of the prime vulnerable periods for occurrence of hypoglycemia includes ineffective patient handoff and poor communication during transition from ICU or medical ward to operation room.[29]
Timely detection and prevention of hypoglycemia is highly essential so as to prevent morbidity and mortality from this diabetic complication. Symptomatology resulting from hypoglycemia can be variable in clinical presentation and awareness of this varied phenomenon is mandatory for successful and timely treatment. Clinical symptomatology of hypoglycemia can be classified on the basis of operating pathophysiology mechanisms (neuroglycopenia, adrenergic counter regulation), as well as time of occurrence (symptoms suggestive of nocturnal hypoglycemia).
Hypoglycaemia is considered to be a marker of increased mortality in patients with shock and is a different clinical entity from iatrogenic hypoglycemia.[30,31] The detrimental effects of hypoglycemia can be seen in every organ, but brain can suffer irreversible injury during acute hypoglycemic episode.[32,33] Intraoperative hypoglycemia prevention though difficult, should be the goal especially made simpler with modern continuous blood glucose monitoring gadgets. The normal physiological adaptation of the body to hypoglycemia can be blunted to a large extent by analgesics and sedatives during postoperative period. The ischemic brain injury can be accentuated in the setting of hypoglycemia as glucose stores are depleted and hence production and utilization of lactate from glucose by the brain tissue are obtunded during the crisis time.[32,33]
The glycemic limits of 65-70 mg/dl usually serve as the threshold for activation of glucagon and epinephrine secretion. Further, neuroglycopenic complaints are preceded by adrenergic symptoms as the glycemic levels touch the ebbs of 50 mg%. A variable degree of autonomic neuropathy is largely responsible for a varied perception of hypoglycemic symptomatology especially in diabetic patients. However, with a plasma glucose level of more than 70 mg/dl, some patients with poor glycemic control may still experience the hypoglycemic symptoms. Conversely, those with antecedent hypoglycemia may develop impaired awareness of hypoglycemia (IAH) due to autonomic neuropathy in long-standing diabetics that reduces their ability to sense symptoms.[34,35]
Need to strengthen endocrine anesthesia
A close co-ordination among endocrinologists, anesthesiologists, and intensivists is a key to achieve harmony between diet, physical activity, antidiabetic therapy, and medication for co-morbid conditions or complications of DM, so as to minimize the incidence of hypoglycemia in surgical diabetic patients. Such co-ordinated efforts are highly essential during preanesthetic evaluation or just when the patients get admitted to ICU. This approach can be highly helpful even if a tight glycemic control is desired. However, it can be made possible if prudent use is made of available monitoring, investigational, and therapeutic strategies.[2,4]
Prevention and management of hypoglycemia
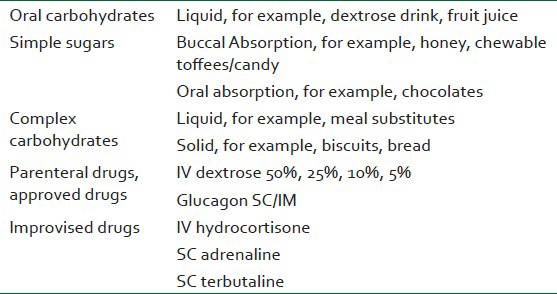
The present clinical scenario of diabetes management in operative and critically ill patients demands a therapeutic climate of aggressive polypharmacy-based strategies and tight glycemic targets. Observance of simple precautions during preopreative and perioperative period related to management of diabetes as well as drug administration helps in reducing the incidence of hypoglycemia [Tables 4 and 5]. The common threads running through all these suggestions are comprehensive patient education, awareness among physicians and nursing staff of various insulin injection guidelines, prudent physicians’ prescription, and vigilant monitoring in the operative area and ICU.[34,35] If hypoglycemia does occur, it should be managed with intravenous dextrose solution of 10% and 25%, depending upon the severity, or in conscious patients, administration of oral carbohydrates, either simple or complex carbohydrates is required. Management of hypoglycemia in operative fields and ICU requires training of nursing and other OT staff so as ensure that any single episode of hypoglycemia should not be missed at all and should be treated on an urgent basis [Tables 5 and 6].
Table 4.
Role of anesthesiologist and intensivist in educating and training for the prevention of hypoglycemia in diabetic patients during preoperative and postoperative period
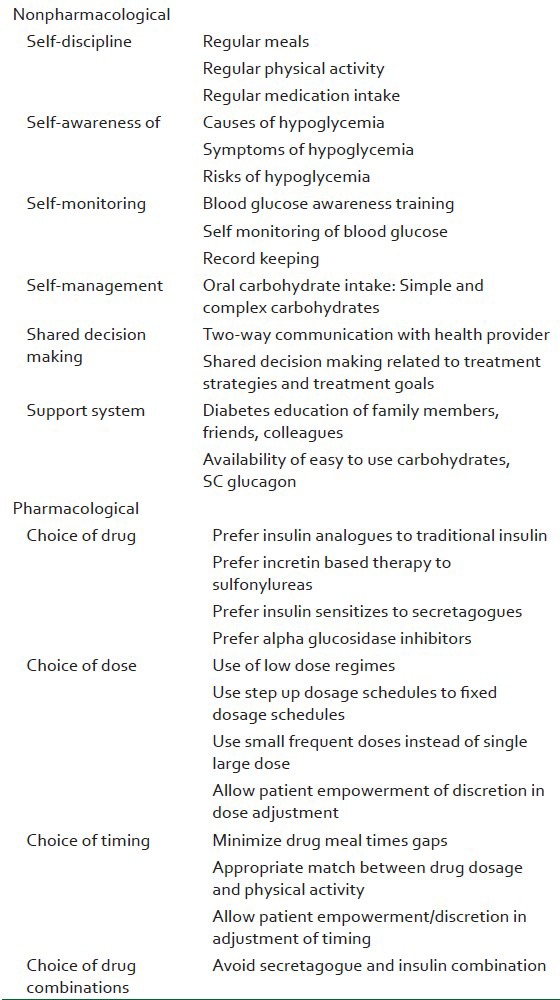
Table 5.
Ten C's to reduce hypoglycemia with insulin use
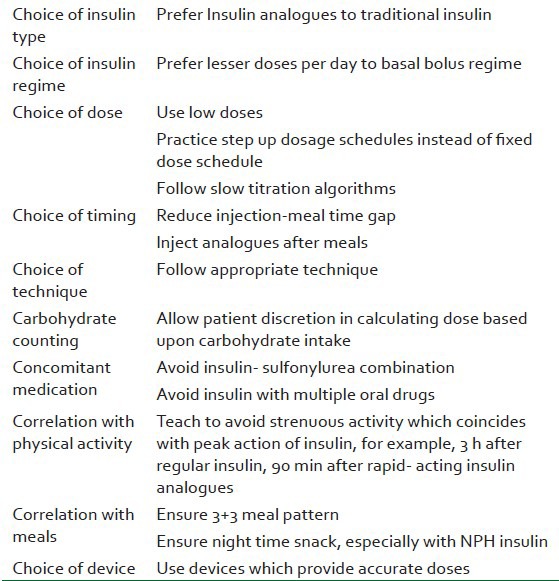
Table 6.
Management of hypoglycemia
CONCLUSION
Hypoglycemia is a common occurrence in day to day diabetes care in surgical and critically ill patients. Its myriad symptoms and multisyndrome effects make it a significant diagnostic and therapeutic challenge for the anesthesiologists and the intensivists. A strong need is felt to strengthen diabetoanesthesia in the background of increasing number diabetic patients presenting for surgery. Besides, a possible role of anesthesiologist and the intensivist is definitely going to be reframed in the near future to educate the people with diabetes, and their health care providers so as to maximally diagnose and prevent complications such as hypoglycemia both in general life and surgical settings.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bajwa SS, Kalra S. Bajaj S, et al., editors. Glycaemic control in ICU. Endocrine Society of India Manual of Clinical Endocrinology. 2012;1:115–23. [Google Scholar]
- 3.Bajwa SJ. Intensive care management of critically sick diabetic patients. Indian J Endocrinol Metab. 2011;15:349–50. doi: 10.4103/2230-8210.85603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bajwa SJ, Kalra S. Diabeto-anaesthesia: A subspecialty needing endocrine introspection. Indian J Anaesth. 2012;56:513–7. doi: 10.4103/0019-5049.104564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Workgroup on Hypoglycemia, American Diabetes Association. Defining and reporting hypoglycemia in diabetes: A report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005;28:1245–9. doi: 10.2337/diacare.28.5.1245. [DOI] [PubMed] [Google Scholar]
- 6.Amiel SA, Dixon T, Mann R, Jameson K. Hypoglycaemia in type 2 diabetes. Diabet Med. 2008;25:245–54. doi: 10.1111/j.1464-5491.2007.02341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Noh RM, Graveling AJ, Frier BM. Medically minimizing the impact of hypoglycemia in type 2 diabetes: A review. Expert Opin Pharmacother. 2011;12:2161–75. doi: 10.1517/14656566.2011.589835. [DOI] [PubMed] [Google Scholar]
- 8.Kalra S, Deepak MC, Narang P, Singh V, Uvaraj MG, Agrawal N. Usage pattern, glycemic improvement, hypoglycemia, and body mass index changes with sulfonylureas in real-life clinical practice: Results from OBSTACLE Hypoglycemia Study. Diabetes Technol Ther. 2013;15:129–35. doi: 10.1089/dia.2012.0237. [DOI] [PubMed] [Google Scholar]
- 9.van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345:1359–67. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- 10.Devos P, Presier JC. Current controversies around tight glucose control in critically Ill patients. Curr Opin Clin Nutr Metab Care. 2007;10:206–9. doi: 10.1097/MCO.0b013e3280147d2d. [DOI] [PubMed] [Google Scholar]
- 11.Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39. doi: 10.1056/NEJMoa070716. [DOI] [PubMed] [Google Scholar]
- 12.NICE-SUGAR Trial Investigators. Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283–97. doi: 10.1056/NEJMoa0810625. [DOI] [PubMed] [Google Scholar]
- 13.Turchin A, Matheny ME, Shubina M, Scanlon JV, Greenwood B, Pendergrass ML. Hypoglycemia and clinical outcomes in patients with diabetes hospitalized in the general ward. Diabetes Care. 2009;32:1153–7. doi: 10.2337/dc08-2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vriesendorp TM, van Santen S, DeVries JH, de Jonge E, Rosendaal FR, Schultz MJ, et al. Predisposing factors for hypoglycemia in the intensive care unit. Crit Care Med. 2006;34:96–101. doi: 10.1097/01.ccm.0000194536.89694.06. [DOI] [PubMed] [Google Scholar]
- 15.Arabi YM, Tamim HM, Rishu AH. Hypoglycemia with intensive insulin therapy in critically ill patients: Predisposing factors and association with mortality. Crit Care Med. 2009;37:2536–44. doi: 10.1097/CCM.0b013e3181a381ad. [DOI] [PubMed] [Google Scholar]
- 16.Graham BB, Keniston A, Gajic O, Trillo Alvarez CA, Medvedev S, Douglas IS. Diabetes mellitus does not adversely affect outcomes from a critical illness. Crit Care Med. 2010;38:16–24. doi: 10.1097/CCM.0b013e3181b9eaa5. [DOI] [PubMed] [Google Scholar]
- 17.Krinsley JS, Grover A. Severe hypoglycemia in critically ill patients: Risk factors and outcomes. Crit Care Med. 2007;35:2262–7. doi: 10.1097/01.CCM.0000282073.98414.4B. [DOI] [PubMed] [Google Scholar]
- 18.Hermanides J, Bosman RJ, Vriesendorp TM, Dotsch R, Rosendaal FR, Zandstra DF, et al. Hypoglycemia is associated with intensive care unit mortality. Crit Care Med. 2010;38:1430–4. doi: 10.1097/CCM.0b013e3181de562c. [DOI] [PubMed] [Google Scholar]
- 19.Egi M, Bellomo R, Stachowski E, French CJ, Hart GK, Hegarty C, et al. Blood glucose concentration and outcome of critical illness: The impact of diabetes. Crit Care Med. 2008;36:2249–55. doi: 10.1097/CCM.0b013e318181039a. [DOI] [PubMed] [Google Scholar]
- 20.Mowery NT, Guillamondegui OD, Gunter OL, Diaz JJ, Jr, Collier BR, Dossett LA, et al. Severe hypoglycemia while on intensive insulin therapy is not an independent predictor of death after trauma. J Trauma. 2010;68:342–7. doi: 10.1097/TA.0b013e3181c825f2. [DOI] [PubMed] [Google Scholar]
- 21.Hermanides J, Bosman RJ, Vriesendorp TM, Dotsch R, Rosendaal FR, Zandstra DF, et al. Hypoglycemia is associated with intensive care unit mortality. Crit Care Med. 2010;38:1430–4. doi: 10.1097/CCM.0b013e3181de562c. [DOI] [PubMed] [Google Scholar]
- 22.Kosiborod M, Inzucchi SE, Goyal A, Krumholz HM, Masoudi FA, Xiao L, et al. Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA. 2009;301:1556–64. doi: 10.1001/jama.2009.496. [DOI] [PubMed] [Google Scholar]
- 23.Al-Dorzi, Tamim HM, Arabi YM. Glycaemic fluctuation predicts mortality in critically ill patients. Anaesth Intensive Care. 2010;38:695–702. doi: 10.1177/0310057X1003800413. [DOI] [PubMed] [Google Scholar]
- 24.Egi M, Bellomo R. Reducing glycemic variability in intensive care unit patients: A new therapeutic target? J Diabetes Sci Technol. 2009;3:1302–8. doi: 10.1177/193229680900300610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freire AX, Murillo LC. How “sweet” complexity is and how “bitter” variability can be; The new aspect of intensive care unit hyperglycemia. Crit Care Med. 2010;8:996–7. doi: 10.1097/CCM.0b013e3181ce217e. [DOI] [PubMed] [Google Scholar]
- 26.Zhang XL, Lu JM, Shan GL, Yang ZJ, Yang WY. Association between glucose variability and adverse in-hospital outcomes for Chinese patients with acute coronary syndrome. Saudi Med J. 2010;31:1146–51. [PubMed] [Google Scholar]
- 27.Leese GP, Savage MW, Chattington PD, Vora JP. The diabetic patient with hypertension. Postgrad Med J. 1996;72:263–8. doi: 10.1136/pgmj.72.847.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rice MJ, Pitkin AD, Coursin DB. Review article: Glucose measurement in the operating room: More complicated than it seems. Anesth Analg. 2010;110:1056–65. doi: 10.1213/ANE.0b013e3181cc07de. [DOI] [PubMed] [Google Scholar]
- 29.Amato-Vealey EJ, Barba MP, Vealey RJ. Hand-off communication: A requisite for perioperative patient safety. AORN J. 2008;88:763–70. doi: 10.1016/j.aorn.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 30.Arabi YM, Tamim HM, Rishu AH. Hypoglycemia with intensive insulin therapy in critically ill patients: Predisposing factors and association with mortality. Crit Care Med. 2009;37:2536–44. doi: 10.1097/CCM.0b013e3181a381ad. [DOI] [PubMed] [Google Scholar]
- 31.Vriesendorp TM, van Santen S, DeVries JH, de Jonge E, Rosendaal FR, Schultz MJ, et al. Predisposing factors for hypoglycemia in the intensive care unit. Crit Care Med. 2006;34:96–101. doi: 10.1097/01.ccm.0000194536.89694.06. [DOI] [PubMed] [Google Scholar]
- 32.Nasraway SA., Jr Sitting on the horns of a dilemma: Avoiding severe hypoglycemia while practicing tight glycemic control. Crit Care Med. 2007;35:2435–7. doi: 10.1097/01.CCM.0000286520.50104.51. [DOI] [PubMed] [Google Scholar]
- 33.Egi M, Bellomo R, Stachowski E, French CJ, Hart G. Variability of blood glucose concentration and short-term mortality in critically ill patients. Anesthesiology. 2006;105:244–52. doi: 10.1097/00000542-200608000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Kedia N. Treatment of severe diabetic hypoglycemia with glucagon: An underutilized therapeutic approach. Diabetes Metab Syndr Obes. 2011;4:337–46. doi: 10.2147/DMSO.S20633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Choudhary P, Amiel SA. Hypoglycaemia: Current management and controversies. Postgrad Med J. 2011;87:298–306. doi: 10.1136/pgmj.2008.068197. [DOI] [PubMed] [Google Scholar]


