Abstract
Background:
Periodontitis and gingivitis are one of the most infectious diseases in human. Several studies have been carried out on dependence of periodontitis and stroke. The aim of this study was to investigate the gingivitis and periodontitis as a risk factor for stroke in Iranian population.
Materials and Methods:
A case-control study was conducted on 100 patients suffering from stroke as case group, and 100 hospitalized patients as control group. The case group included 42 males and 58 females, and in control group there were 44 males and 56 females. Using a University of North Carolina-15 manual probe, the clinical attachment level, the distance between the cemento-enamel junction and the probed base of the periodontal pocket, were recorded by gingival and periodontal indexes. The data were analyzed by multiple logistic regressions, Chi-square test, Fisher's test, t-test, Man Whitney, and SPSS11.5 software program. P > 0.05 was considered as significant.
Results:
The case group included 42 males and 58 females, and in control group 44 males and 56 females were included. In this investigation, the average of gingival index in men and women of case group was 1.22 ± 0.55 and 1.31 ± 0.55, respectively. This study showed that the average of gingival index in case group was more than control group. Periodontal index in both groups in men was more than women. The moderate and severe periodontitis in case group were more than that of control group (P = 0.003, P = 0.001).
Conclusion:
The result of this study shows that there is a significant relation between stroke and periodontal index; however, there isn’t any significant relation between stroke and gingival index.
Keywords: Gingivitis, periodontitis, risk factors, stroke
INTRODUCTION
Epidemiologic studies have shown that cerebrovascular accident (CVA) is the 3rd cause of death in developed countries with 0.8 % prevalence in whole population. Although, prevalence rate of stroke is reduced but yet is one of the most important health problem in United State.[1,2]
CVA risk factors are hypertension, diabetes, smoking and cardiovascular disease. Not only urinary tract infections independently increase the risk of ischemic stroke, but also, mainly acute respiratory tract infection. Although, in many patients especially, young patients none of these risk factors doesn’t exist. Today, inflammatory parameters and chronic and acute infectious diseases are considered as the risk factors for this disease.[3,4] Though, there is not any single infection as a major independent predictor. In order to lower this burden it is essential to identify risk factors and respective preventive strategies besides the established stroke risk factors.[5]
Periodontitis and gingivitis are two most infectious man diseases. Today, it is estimated that about 35% of people over 30-year-old in America and 50-55% of people in developing countries are involved with these diseases. These diseases are due to the practice of chronic bacterial infection and inflammatory response of host.[3,4,6]
The relationship between periodontitis and CVA was first introduced by Mackenzi and Milard in 1963 but the importance of this issue was not understood.[7] Periodontal infection can be a complex multiphase disease by associating this infection with organ systems such as cardiovascular, endocrine, reproductive, and respiratory systems.[8]
Nowadays, periodontitis is considered as a risk factor for atherosclerosis and thromboembolic disease.[6] Furthermore, periodontal infections may effect the onset and development of atherosclerosis by special mechanisms. Periodontitis and atherosclerosis have complex etiologic factors that are influenced by combination of hereditary and environmental factors. These diseases have many common risk factors and also have known similarity in essential pathogenic mechanism. Several studies have been carried out on dependence of periodontitis and stroke.[9,10,11,12,13,14] Therefore, doing more investigation for determination of prevalence of periodontal disease in these patients for finding relationship between periodontal disease and CVA is completely necessary.[7]
Research works in Iran have shown that there is a high prevalence rate of periodontal diseases in Iranian population, such that 1.2-10.5% of people have normal periodontium.[15] Besides, the prevalence rate of stroke is between 0.43% and 0.74% in this region.[16,17] Hence, regarding to the high prevalence of periodontal diseases in Iranian people and also noticing the fact that there is only one study about prevalence of periodontal disease and CVA patients in Iran,[18] the present research work seems necessary to be carried out.
MATERIALS AND METHODS
A case-control study was conducted on 100 non-fatal stroke cases at the Shafa hospital, Kerman, Iran, and 100 hospitalized patients (control group). The matching between two groups was carried out according to this way that at first 100 patients from Neuroscience ward were examined by gingival and periodontal indexes. Then, based on the number of males and females and the age, 100 patients from others hospital wards were chosen.
Medical specialists diagnosed stroke by using brain imaging from magnetic resonance imaging and/or computerized tomography.[18]
Using a University of North Carolina-15 manual probe, the clinical attachment level (CAL), the distance between the cemento-enamel junction (CEJ) and the probed base of the periodontal pocket, were recorded by a dentist. Data were collected by questionnaires, patient hospital records and clinical examinations. In the questionnaire, many items were included which are the demographic information (name, gender, profession, date of admission if hospitalized, diabetes mellitus, hypertension, heart valve disease, atrial fibrillation, peripheral arterial disease, previous stroke/ischemic attack, smoking, a positive family history of stroke, and renal failure) and information about cholesterol, triglyceride, Complete Blood Count (CBC) and evaluation of gingival and periodontal condition according to gingival index and periodontal disease index criteria.[18]
Examination of all patients was carried out by a specially trained dentist for all subjects that had been trained 1 week in periodontal part of faculty. Examiner was tested in order to reduce the intra-examination error. Before the examination of each person, the goal of this study and method of examination was explained to patient and satisfaction form was gained from them. Furthermore, we gave confidence to patients that all of their information remain secret. All examination was carried out on patients with blue light, a mouth mirror and a periodontal probe (after isolation with cotton roles). For obvious reasons, the dentist could not be blinded for the patient's status. Smoking and nonsmoking and its rate was asked from patients and also blood pressure of patients and result of laboratory tests were gained from patient hospital records.[18] The distance between the probed base of the pocket and the CEJ was considered as the main variable in CAL of periodontitis. In the following four sites of each available tooth, including distofacial papilla, facial gingival margin, mesio-facial papilla and lingual gingival margin, probing was performed and mean values were individually calculated. Attachment levels were analyzed as continuous variables. Using the Loe and Silness gingival index,[19] gingivitis was determined by probing the teeth at four sites. For this purpose, scoring criterias for gingival are as follows:[19] G0: normal gingival without inflammation, G1: mild inflammation, slight change in colour and texture and no bleeding on probing, G2: moderate inflammation, shiny redness, edema and bleeding on very slight and light probing, G3: severe inflammation, marked shiny redness, edema, ulceration, and spontaneous bleeding on very slight and light probing.[18,19] The data of this research were analyzed by use of multiple logistic regressions, Chi-square test, Fisher's test, t-test and SPSS11.5 software program. P ˂ 0.05 was considered as significant.
RESULTS
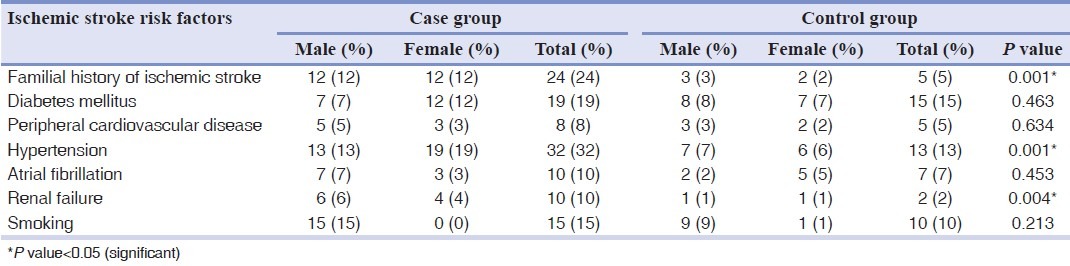
In this study, 100 patient suffering from stroke as case group and 100 hospitalized patients as control group were selected. Average age of case group was 51.89 ± 15.51 and average of control group was 52.59 ± 17.3. The case group included 42 (42%) males and 58 (58%) females, and in control group 44 males (44%) and 56 females (56%) were included. The mean time of examination after admission was 3.2 days for stroke patients and 2.9 days for hospitalized control. Risk factors for cerebral ischemia are shown in Table 1.
Table 1.
Risk factors for ischemic stroke in case and control groups
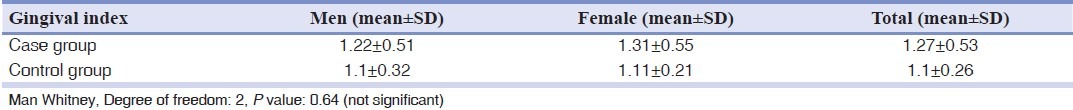
In this investigation, the average of gingival index in men and women of case group in order was 1.22 ± 0.55 and 1.31 ± 0.55 with this fact that this number in women is more than men. However, there wasn’t any significant difference between gender and gingival index (P = 0.42). Furthermore, the average of gingival index in case group was more than control group but there isn’t any significant difference between them (P = 0.64) [Table 2].
Table 2.
Gingival index condition in case and control groups
In Table 3, the condition of gingival inflammation in two groups has been shown. In all criteria (mild, moderate and severe inflammation) in case group and in women is more than men, however, there isn’t any significant relationship between gender and gingival index in two groups. Furthermore, there wasn’t any significant difference about gingival inflammation between groups. According to our result, none of patients in two groups have not normal gingival.
Table 3.
Gingival inflammation condition according to gingival index in case and control groups based on gender
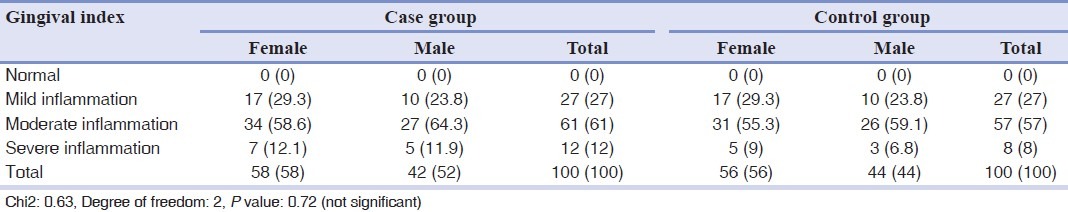
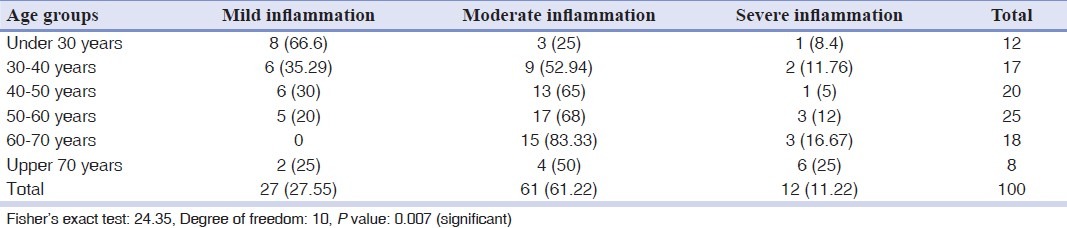
Table 4, shows the frequency of gingivitis in case group according age groups. Relationship between age and gingivitis in case group was significant (P = 0.007).
Table 4.
Gingival inflammation condition in case group in different age groups
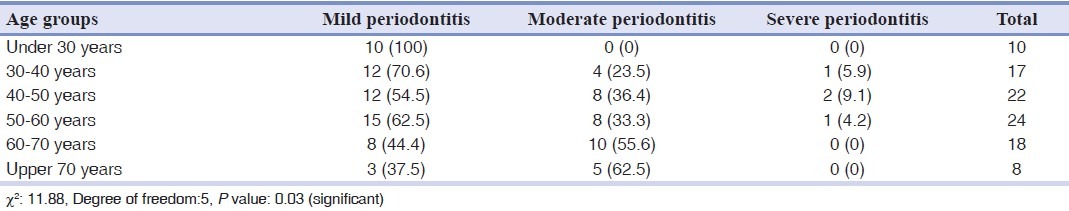
Periodontal index in both groups in men was more than women and there was significant relationship between this index and gender (P = 0.031). Furthermore, periodontal index in case group was more than control group (P = 0.001) [Table 5]. The moderate and severe periodontitis in case group was more than control group and there was significant relationship between this index in two groups [Table 6]. Relationship between age and periodontal disease in case group was significant (P = 0.03) [Table 7].
Table 5.
Periodontal index condition in case and control groups
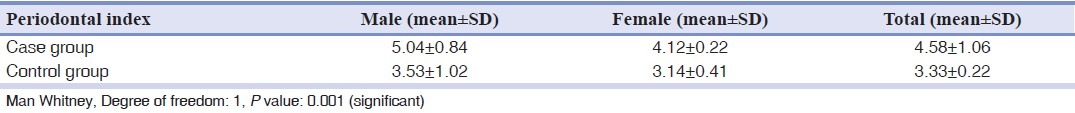
Table 6.
Frequency of periodontitis in case and control groups
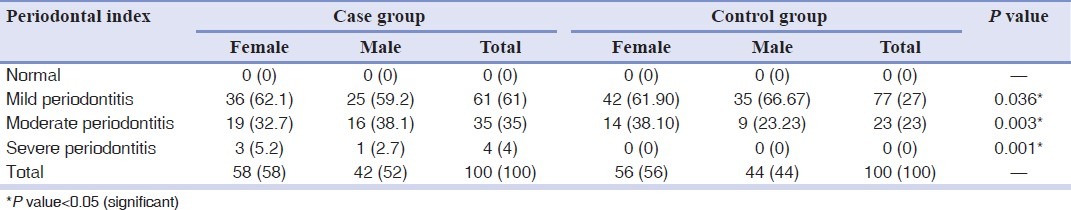
Table 7.
Periodontitis condition in case group in different age groups
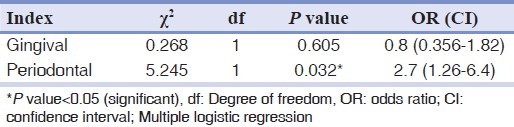
After considering age, gender, and other confounding factors in the multiple logistic regression models in the present work, it is found that periodontal index is associated with increased risk of stroke [Table 8].
Table 8.
Gingival and periodontal index in case group in different age groups
We furthermore evaluated the association of the presence of periodontal disease with the risk factors of ischemic stroke. Results indicate that after omission of confounding factors only hypertension and renal failure are effective on periodontal and gingival condition in case group and significant association was observed (P = 0.001).
DISCUSSION
Chronic infections have been reported to be as risk factors for ischemic stroke. However, the association of ischemic stroke with periodontal disease, which is also a chronic inflammatory disease, needs to be evaluated.[18] This study showed that prevalence of gingival index and periodontal index in case group is more than control group.
In 2000, the American general surgeon committee published the first report about oral health and hygiene with emphasize on this point that oral hygiene is beyond having intact teeth and is the main part of general health. Based on surgeon idea, mouth is the way for entering microbial infection that influence on general health situation. Furthermore, mouth is a vital and functional tissue that can have important role focus for general health, and having healthy life.[20]
During two recent decades, studies about oral hygiene, atherosclerosis and CVA have been carried out.[9,10,11,12,13,14,15,16,17,18,21,22,23,24,25] Stroke risk factors include aging, smoking, race, hypertension, diabetes mellitus, cardiovascular disease, alcoholism, inflammatory disease, and Obesity.[11] Inflammatory risk factors of stroke have been assessed and in the opinion of researchers periodontitis is dependent to stroke.[14,26]
There are several potential mechanisms for relationship between periodontal disease and stroke.[7,10,26,27] Periodontitis causes an increase in the systemic inflammation that leads to arthrosclerosis and cerebrovascular attacks. Acute periodontal inflammation may cause a stage of prothrombin, bacteremia, platelet activation, increasing in coagulator's factors and risk of stroke. Furthermore, periodontal microorganism was observed in atheroma. The endotoxin of this microorganisms can destroy endothelial cells and cause smooth muscle proliferation.[11,26] Periodontal disease produces inflammatory markers and coagulator's factors such as C-reactive protein, fibrinogen and increases platelets aggregation and cause atherosclerosis and thrombosis.[11,28] Furthermore, chronic gingival infections decreases glucose tolerances and decreases blood lipids.[18]
The periodontal infection have a main role by creation stable bacterial environment and take part in inflammatory processes derived from monocytes and macrophages that cause atheromatosis and narrowing of blood vessels. Furthermore, bacteremia deriving from subgingival and supragingival plaque can increase platelets aggregation by takeing part in thromboses formation and subsequently embolism which are the main causes of stroke.[29]
Because of multifactorial nature of dental infection and CVA, founding a distinguished factor is difficult and results have contradiction with each other. The most principle problem of these studies is insufficient control on numerous confounding factors that cause lower estimation of risk factors.
In this study, periodontitis was indicated as an independent risk factor for stroke, especially, in men and young subjects. Associations between cerebral ischemia and periodontitis was distinguished by several epidemiological studies.[9,22,23,24]
One meta-analysis of retrospective and prospective study has shown that periodontal disease may increase risk of CVA up to 20%. Similarly, reported relative risk between periodontal disease and stroke from 2.85 to 1.74 is changeable.[30]
The study by Mendez et al. on 80 subjects during 25-30 years follow-up showed that patients with clinically apparent periodontal disease, are 2.27 times more than others in the risk of peripheral vessels disease.[31] These researchers concluded that periodontal disease is an independent risk factor for peripheral vessels disease. Furthermore, in a report by Wu et al. there was clear relationship between periodontal disease and stroke.[32] In other retrospective studies by Morrison et al. an indistinctive relation between periodontal disease and stroke has been shown. This evaluation detected that this relationship increases to 2.12% for fatal ischemia.[25]
It was concluded by Janket et al. that there is a small but significant increase in the risk of cardiovascular disease among patients with periodontal disease at baseline.[33] In another research by Grau et al. periodontitis were distinguished as an independent risk factor for cerebral ischemia, especially, in men and young patients.[9] This finding is similar to that obtained by Kim et al., Pradeep et al., Dörfer et al., Geerts et al., which are in agreement with the present study.[21,22,34,35]
Jimenez et al. in a current study revealed an association between history of periodontitis but not current periodontal inflammation and incidence of cerebrovascular disease in men, independent of established cardiovascular risk factors, particularly among men aged >65 years.[36]
One study has reported that men with periodontal disease in comparison with men without periodontal disease almost 3 times more likely to have stroke risk.[7] Furthermore, study of Joshipura et al. on 41380 men without cardiovascular disease during 12 years follow-up showed that during this period, 349 persons were affected with stroke. Men with gingival index more than 1.5 were under the stroke risk about 1.3 times more than others.[13]
Abolfazli et al. showed that patients (case group) have higher loss of attachment than controls, whereas gingivitis isn’t associated with the risk of cerebral ischemia. Furthermore, the more severe periodontitis was detected among men in patients with cerebral ischemia.[18]
In similar studies,[9,10,13,18] gingivitis and periodontitis were reported in men more than women. That is because of less oral hygiene compliance in men and infrequent referring to dentist.
Present study shows that there isn’t significant relationship between gingival indexes between 2 groups. Although, in some study severe gingivitis have been propounded as a more important risk factor in CVA patient in comparison to periodontitis.[9,11] Researchers believe that gingivitis is a start to periodontal diseases, although, in one cohort study, any association between these two factors was not found.[32]
In this study, in fully adjusted logistic regression analysis, a probing pocket depth of <4.5 mm was found to be the most significant factor for stroke (odds ratio = 2.7; confidence interval = 1.26-6.4; P = .032).
Sfyroeras et al. carried out six prospective and seven retrospective studies about association between periodontal disease and stroke. These researchers showed that overall adjusted risk of stroke in subjects with periodontitis is 1.47 times higher than in subjects without periodontitis in prospective studies (95% confidence interval, 1.13-1.92; P = 0.0035) and 2.63 times (95% confidence interval, 1.59-4.33; P = 0.0002) in retrospective studies.[37]
Studies that assessed tooth loss or periodontal disease as risk factor of stroke lead to different results and the relation between oral condition and CVA is yet unclear. In the absence of any cause-effect relation, this relationship may explain by common risk factors. Therefore, more epidemiologic studies are needed to discover the role of nutrition and other inflammatory mediators.
CONCLUSION
The result of this study showed that there is significant relation between stroke and periodontal index, however, there isn’t any significant relation between stroke and gingival index. Furthermore, it was found that periodontal index in women and age groups more 40 years are high.
ACKNOWLEDGMENTS
This study was supported by the Kerman Neuroscience Research Center. The authors would like to thank the Research Deputy for their financial support.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Greenburg M, Glick M. Burket's Oral Medicine.11 th ed. 11th ed. Hamilton: BC Decker; 2009. pp. 98pp. 115–6. [Google Scholar]
- 2.Little JW, Falace DA, Miller CS, Rhodus NL. Dental Management of the Medically Compromised Patients. 2nd ed. Philaderphia: WB Sunders; 2003. pp. 121–48. [Google Scholar]
- 3.Lindsberg PJ, Grau AJ. Inflammation and infections as risk factors for ischemic stroke. Stroke. 2003;34:2518–32. doi: 10.1161/01.STR.0000089015.51603.CC. [DOI] [PubMed] [Google Scholar]
- 4.Chala S, Abouqal R, Abdallaoui F. Prevalence of apical periodontitis and factors associated with the periradicular status. Acta Odontol Scand. 2011;69:355–9. doi: 10.3109/00016357.2011.568967. [DOI] [PubMed] [Google Scholar]
- 5.Elkind MS, Ramakrishnan P, Moon YP, Boden-Albala B, Liu KM, Spitalnik SL, et al. Infectious burden and risk of stroke: The northern Manhattan study. Arch Neurol. 2010;67:33–8. doi: 10.1001/archneurol.2009.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scannapieco FA. Position paper of The American Academy of Periodontology: Periodontal disease as a potential risk factor for systemic diseases. J Periodontol. 1998;69:841–50. [PubMed] [Google Scholar]
- 7.Beck J, Garcia R, Heiss G, Vokonas PS, Offenbacher S. Periodontal disease and cardiovascular disease. J Periodontol. 1996;67:1123–37. doi: 10.1902/jop.1996.67.10s.1123. [DOI] [PubMed] [Google Scholar]
- 8.Saini R, Marawar PP, Shete S, Saini S. Periodontitis, a true infection. J Glob Infect Dis. 2009;1:149–50. doi: 10.4103/0974-777X.56251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grau AJ, Buggle F, Ziegler C, Schwarz W, Meuser J, Tasman AJ, et al. Association between acute cerebrovascular ischemia and chronic and recurrent infection. Stroke. 1997;28:1724–9. doi: 10.1161/01.str.28.9.1724. [DOI] [PubMed] [Google Scholar]
- 10.Howell TH, Ridker PM, Ajani UA, Hennekens CH, Christen WG. Periodontal disease and risk of subsequent cardiovascular disease in U.S. male physicians. J Am Coll Cardiol. 2001;37:445–50. doi: 10.1016/s0735-1097(00)01130-x. [DOI] [PubMed] [Google Scholar]
- 11.Desvarieux M, Schwahn C, Völzke H, Demmer RT, Lüdemann J, Kessler C, et al. Gender differences in the relationship between periodontal disease, tooth loss, and atherosclerosis. Stroke. 2004;35:2029–35. doi: 10.1161/01.STR.0000136767.71518.36. [DOI] [PubMed] [Google Scholar]
- 12.Grau AJ, Becher H, Ziegler CM, Lichy C, Buggle F, Kaiser C, et al. Periodontal disease as a risk factor for ischemic stroke. Stroke. 2004;35:496–501. doi: 10.1161/01.STR.0000110789.20526.9D. [DOI] [PubMed] [Google Scholar]
- 13.Joshipura KJ, Hung HC, Rimm EB, Willett WC, Ascherio A. Periodontal disease, tooth loss, and incidence of ischemic stroke. Stroke. 2003;34:47–52. doi: 10.1161/01.str.0000052974.79428.0c. [DOI] [PubMed] [Google Scholar]
- 14.Syrjänen J, Peltola J, Valtonen V, Iivanainen M, Kaste M, Huttunen JK. Dental infections in association with cerebral infarction in young and middle-aged men. J Intern Med. 1989;225:179–84. doi: 10.1111/j.1365-2796.1989.tb00060.x. [DOI] [PubMed] [Google Scholar]
- 15.Arabi SR, Torkzaban P, Gholami L, Taghavi M, Hatami M. Comparative evaluation of periodontal indices in patients with ischemic heart disease and positive myocardial perfusion scan. Dent J Hamadan Univ. 2010;1:17–20. [Google Scholar]
- 16.Oveisgharan S, Sarrafzadegan N, Shirani S, Hosseini S, Hasanzadeh P, Khosravi A. Stroke in Isfahan, Iran: Hospital admission and 28-day case fatality rate. Cerebrovasc Dis. 2007;24:495–9. doi: 10.1159/000110418. [DOI] [PubMed] [Google Scholar]
- 17.Ghandehari K, Moud ZI. Incidence and etiology of ischemic stroke in Persian young adults. Acta Neurol Scand. 2006;113:121–4. doi: 10.1111/j.1600-0404.2005.00515.x. [DOI] [PubMed] [Google Scholar]
- 18.Abolfazli N, Ghoreishizadeh A, Ayramlu H, Ghavimi M, Ghoreishizadeh M, Salehsaber F. Periodontal disease and risk of cerebral ischemic stroke. J Neurol Sci. 2011;28:307–16. [Google Scholar]
- 19.Newman MG, Takei HH, Carranza FA. Carranza 's Clinical Periodontology. 10th ed. Hamilton: WB Sunders; 2006. pp. 112–22.pp. 333–53. [Google Scholar]
- 20.Rose LF, Mealey B, Minsk L, Cohen DW. Oral care for patients with cardiovascular disease and stroke. J Am Dent Assoc. 2002;133:37S–44. doi: 10.14219/jada.archive.2002.0378. [DOI] [PubMed] [Google Scholar]
- 21.Pradeep AR, Hadge P, Arjun Raju P, Shetty SR, Shareef K, Guruprasad CN. Periodontitis as a risk factor for cerebrovascular accident: A case-control study in the Indian population. J Periodontal Res. 2010;45:223–8. doi: 10.1111/j.1600-0765.2009.01220.x. [DOI] [PubMed] [Google Scholar]
- 22.Dörfer CE, Becher H, Ziegler CM, Kaiser C, Lutz R, Jörss D, et al. The association of gingivitis and periodontitis with ischemic stroke. J Clin Periodontol. 2004;31:396–401. doi: 10.1111/j.1600-051x.2004.00579.x. [DOI] [PubMed] [Google Scholar]
- 23.Khader YS, Albashaireh ZS, Alomari MA. Periodontal diseases and the risk of coronary heart and cerebrovascular diseases: A meta-analysis. J Periodontol. 2004;75:1046–53. doi: 10.1902/jop.2004.75.8.1046. [DOI] [PubMed] [Google Scholar]
- 24.Lee HJ, Garcia RI, Janket SJ, Jones JA, Mascarenhas AK, Scott TE, et al. The association between cumulative periodontal disease and stroke history in older adults. J Periodontol. 2006;77:1744–54. doi: 10.1902/jop.2006.050339. [DOI] [PubMed] [Google Scholar]
- 25.Morrison HI, Ellison LF, Taylor GW. Periodontal disease and risk of fatal coronary heart and cerebrovascular diseases. J Cardiovasc Risk. 1999;6:7–11. doi: 10.1177/204748739900600102. [DOI] [PubMed] [Google Scholar]
- 26.Elter JR, Offenbacher S, Toole JF, Beck JD. Relationship of periodontal disease and edentulism to stroke/TIA. J Dent Res. 2003;82:998–1001. doi: 10.1177/154405910308201212. [DOI] [PubMed] [Google Scholar]
- 27.Ziegler CM, Schwarz W, Grau A, Buggle F, Hassfeld S, Mühling J. Odontogenic focus as the etiology of cerebral ischemia. Mund Kiefer Gesichtschir. 1998;2:316–9. doi: 10.1007/s100060050079. [DOI] [PubMed] [Google Scholar]
- 28.Noack B, Genco RJ, Trevisan M, Grossi S, Zambon JJ, De Nardin E. Periodontal infections contribute to elevated systemic C-reactive protein level. J Periodontol. 2001;72:1221–7. doi: 10.1902/jop.2000.72.9.1221. [DOI] [PubMed] [Google Scholar]
- 29.Mealey BL. Influence of periodontal infections on systemic health. Periodontol 2000. 1999;21:197–209. doi: 10.1111/j.1600-0757.1999.tb00176.x. [DOI] [PubMed] [Google Scholar]
- 30.Meurman JH, Sanz M, Janket SJ. Oral health, atherosclerosis, and cardiovascular disease. Crit Rev Oral Biol Med. 2004;15:403–13. doi: 10.1177/154411130401500606. [DOI] [PubMed] [Google Scholar]
- 31.Mendez MV, Scott T, LaMorte W, Vokonas P, Menzoian JO, Garcia R. An association between periodontal disease and peripheral vascular disease. Am J Surg. 1998;176:153–7. doi: 10.1016/s0002-9610(98)00158-5. [DOI] [PubMed] [Google Scholar]
- 32.Wu T, Trevisan M, Genco RJ, Dorn JP, Falkner KL, Sempos CT. Periodontal disease and risk of cerebrovascular disease: The first national health and nutrition examination survey and its follow-up study. Arch Intern Med. 2000;160:2749–55. doi: 10.1001/archinte.160.18.2749. [DOI] [PubMed] [Google Scholar]
- 33.Janket SJ, Baird AE, Chuang SK, Jones JA. Meta-analysis of periodontal disease and risk of coronary heart disease and stroke. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:559–69. doi: 10.1067/moe.2003.107. [DOI] [PubMed] [Google Scholar]
- 34.Kim HD, Sim SJ, Moon JY, Hong YC, Han DH. Association between periodontitis and hemorrhagic stroke among Koreans: A case-control study. J Periodontol. 2010;81:658–65. doi: 10.1902/jop.2010.090614. [DOI] [PubMed] [Google Scholar]
- 35.Geerts SO, Legrand V, Charpentier J, Albert A, Rompen EH. Further evidence of the association between periodontal conditions and coronary artery disease. J Periodontol. 2004;75:1274–80. doi: 10.1902/jop.2004.75.9.1274. [DOI] [PubMed] [Google Scholar]
- 36.Jimenez M, Krall EA, Garcia RI, Vokonas PS, Dietrich T. Periodontitis and incidence of cerebrovascular disease in men. Ann Neurol. 2009;66:505–12. doi: 10.1002/ana.21742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sfyroeras GS, Roussas N, Saleptsis VG, Argyriou C, Giannoukas AD. Association between periodontal disease and stroke. J Vasc Surg. 2012;55:1178–84. doi: 10.1016/j.jvs.2011.10.008. [DOI] [PubMed] [Google Scholar]


