Abstract
Background:
Patients undergoing orthodontic treatment experience varying degrees of pain with separator insertion. A survey of patients’ attitude towards orthodontic treatment revealed that pain was the most discouraging factor related to their treatment. Moreover, it was the highest ranking reason for wanting to discontinue care. The purpose of this study was to determine the effect of low-level laser irradiation on dental pain induced by forces from separators in orthodontic treatment.
Materials and Methods:
This study was an experimental clinical trial. Twenty-nine patients were recruited for this research. Low-level laser irradiation was applied on one half of the maxillary and mandibular arches for 5 days. The opposite half of the arches was considered the control group. Laser irradiation was applied for 30 seconds in the alveolar bone between the second premolars, first molars, and second molars. Pain perception was evaluated with a standardized questionnaire that was answered by patients before and after laser irradiation. Data was analyzed by Wilcoxon and Friedman test. P value ≤0.05 was considered significant.
Results:
The highest pain level was reported at day 1 following separator placement and decreased gradually until day 5. At day 4 and 5, the pain intensity was lower in the laser group than in the control group; however, this finding was not statistically significant. At day 1 and 3, the pain intensity was higher in the laser group than in the control group; however, it was not statistically significant. At day 2, the pain intensity was lower in the laser group than in the control group and was statistically significant.
Conclusion:
Our findings suggest that there is no statistically significant difference in pain by using low-level laser irradiation.
Keywords: Low-level laser therapy, orthodontics, pain, separator
INTRODUCTION
Creating space mesially and distally to teeth, which are to be banded, forms the initial step in fixed orthodontic mechanotherapy. It is well-known that placement of orthodontic separators (brass wire, elastomeric, spring type steel separators, and latex elastics) results in a painful experience for almost all patients.[1,2] Two controlled clinical trials performed by Ngan et al.,[2,3] concluded that there was discomfort associated with separator placement, which usually starts within 4 hours of insertion. The level of discomfort increases over the next 24 hours and decreases to pre-placement level within 7 days. Another report[1] has also addressed this issue. They evaluated and compared the separation effect and patient perception of pain and discomfort to two types of orthodontic separators (elastomeric and spring type) but found no statistically significant difference between the discomforts caused by the two types of separators. They reported that the worst pain was experienced at day 2 and subsided almost completely by day 5.
An electromyographic (EMG) study, performed to evaluate the motor and sensory changes associated with separator placement, showed a decrease in motor output as well as pressure pain threshold in muscles of mastication.[4] They suggested this to be a protective mechanism against further damage to the injured part of the masticatory system. It is clear that pain is associated with the process of orthodontic separation and starts within 4 hours of its placement with a peak level at day 2 that may last for 7 days.
Pain, which includes sensations evoked by, and reactions to, noxious stimuli, is a complex experience and often accompanies orthodontic appointments. This, among the most cited negative effects of orthodontic treatment, is of major concern to patients as well as clinicians.[5,6] It is also evident in other publications.[7,8] Surveys performed to determine the experience of orthodontic pain have rated it as a key deterrent to orthodontic therapy and a major reason for discontinuing treatment.[5,6,9,10] One survey rated pain as the greatest dislike during treatment and fourth among major fears and apprehensions prior to orthodontic treatment.[11]
Pain is a subjective response, which shows large individual variations. It is dependent upon factors such as age, gender, individual pain threshold, the magnitude of the force applied, present emotional state and stress, cultural differences, and previous pain experiences.[2,9,12,13,14] Surveys regarding the percentage of patients experiencing pain have reported values ranging from 70% (Caucasian population) to 95% (Asian population).[6,13,14] Surprisingly, this important area, in clinical practice as well as research, is ignored, as evidenced by the scarcity of publications. There is no doubt that the perception of orthodontic pain is part of an inflammatory reaction causing changes in blood flow following orthodontic force application. This is known to result in the release of various chemical mediators eliciting a hyperalgesic response. Smith and Burstone[15] reported an immediate and delayed painful response after orthodontic force application. They attributed the initial response to compression and the delayed response to hyperalgesia of the periodontal ligament (PDL). This hyperalgesia has been related to prostaglandins (PGEs), which make the PDL sensitive to released algogens such as histamine, bradykinin, PGEs, serotonin, and substance P.[16,17] It is clear that all orthodontic procedures will create tension and compression zones in the PDL space resulting in a painful experience for the patients.
In order to study or evaluate pain, patient interview/questionnaire and ratings with Visual Analogue Scales (VAS), McGill pain questionnaire (MPQ), Verbal Rating Scales (VRS), and algometers can be effectively used.
It is imperative that pain control during orthodontic treatment should be considered an important aspect of orthodontic mechanotherapy.
The existing literature supports the use of non-steroidal anti-inflammatory drugs (NSAIDs) for pain control, even though other methods (such as anesthetic gel, bite wafers, transcutaneous electrical nerve stimulation, low-level laser use, and vibratory stimulation) have been suggested. The major concern regarding NSAIDs is the interference produced on inflammation associated with tooth movement process. Low doses administered for 1 or 2 days in the initial stages will not affect the tooth movement process as such. Dental interest in lasers has been high and research has continued to improve dental treatment through laser application.[18] The effect of low-level laser therapy (LLLT) on orthodontic pain is still controversial. Lim et al.,[19] in a clinical investigation on the efficacy of LLLT in reducing orthodontic pain found discouraging results, and it was not found to produce immediate pain relief in orthodontic patients. Other investigations show the effect of LLLT on reducing pain during orthodontic treatment. LLLT has no pharmacological side effects.
The aim of this study was to assess the effect of low-level laser radiation on the pain caused by the placement of orthodontic separators. This was a controlled clinical trial with a split mouth design on 29 patients.
MATERIALS AND METHODS
Twenty-nine consenting volunteers (24 males and five females), ages from 12 to 22 (mean = 15.03) years, were included in this study. Participation was based on the following inclusion criteria:
No systemic disease.
No use of medication that might interfere with bone metabolism and gingival tissue.
No gingivitis or periodontitis.
The teeth must be free from any pathologic conditions.
Bilateral symmetry (Presence of teeth on both sides of the arch).
Exclusion criteria:
Patients who did not return the completed questionnaires.
Patients who used any form of analgesics during the experiment.
Removal or loss of the separator during the experiment.
Patients who did not show up for any of the experimental sessions.
Each patient was submitted to an anamnesis, intraoral clinical exam. Elastic orthodontic separators (Dentaurum, Germany) were placed on the mesial and distal of the first maxillary and mandibular molars.
Immediately after separator placement, the pain sensitivity index was determined through the VAS.
The side of the dental arch for laser irradiation was selected randomly. In each jaw, one side which phototherapy was applied considered as test side and the other side was considered as control side. In the control side phototherapy was applied with the equipment turned off. Phototherapy was applied 30 seconds daily for 5 days. Pain level before and after of each therapy was recorded by VAS.
Phototherapy
The Phototherapy procedures were done with Gallium arsenide (GaAs) laser (DLT-101, Behsazgostar, Iran). This laser is in Infrared spectrum and is pulsating (wavelength 904 nm). One of specific features of this device is very short pulses (40-100 nanosec). It also called “super pulsing” and as result of high power pulses, has high power of penetrance in the tissue (30-50 mm of tissue penetration. Mean output power was 200 mW and dose of treatment was 6 J. Radiation was applied punctually, touching the gum perpendicularly on two points of the vestibular side and on the lingual side of the separated molars; both points were in the cervical and radicular region. The diameter of tip was 7 mm.
Ethical aspect
This study was submitted to the Research ethics committee of Hamedan Dental School (Iran) following ethical guidelines for human testing according to the principles of the legislation for human research.
Statistical analysis
Data was analyzed by Wilcoxon and Friedman test. P value ≤0.05 was considered significant.
RESULTS
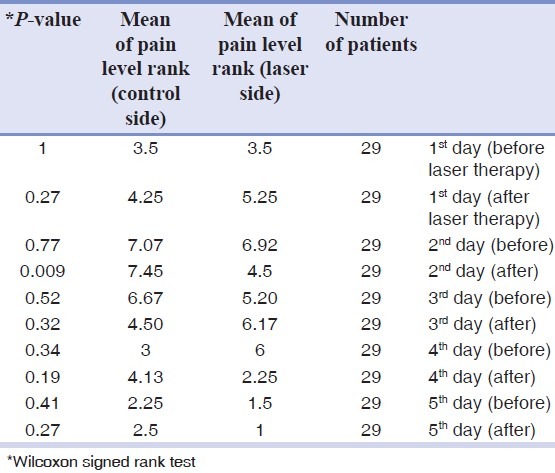
Data shows mean of pain level rank is similar in both sides except 2nd day after laser therapy [Table 1]. Table 1 also shows pain level in the test side decreased by passing time and it was statistically significant.(P = 0.03) and the maximum of pain level was day 2 before laser therapy and minimum was day 5 after laser therapy. Pain level in the Control side decreased by passing time and it was statistically significant. (P = 0.02) and the maximum of pain level was on 2nd day after laser therapy and minimum was on 5th day before laser therapy.
Table 1.
Comparison between laser side and control side
DISCUSSION
In this study, we used orthodontic tooth movement (placing separator) as a model to evaluate the effect of LLLT on the level of pain.
Pain levels were measured for 5 days following initial placement of separators. It has been shown that pain increases after two hours of placement and continues 7 days later. Patients with anxiety disorders and chronic pain were excluded from study. Ngan et al., reported maximum pain perception perceived after 4 and 24 hours following placement of separator or archwire.[2,3] Bernhardt et al.,[20] noted that pain following placement of separator initiated after 2 hours and reaches its maximum during sleep. The second highest grade of pain was reported after 24 hours. Erdinc et al.,[21] reported the same result, but Berguis et al.,[12] reported the highest grade of pain was recorded 1 day after placement of separators.
According to our study, the maximum level of pain on the test side was recorded 1 day after placement of separators which gradually declined until the 5th day. Turhani et al.,[22] showed that laser irradiation at the beginning of orthodontic treatment reduced pain after 6 and 30 hours.
Lim et al., evaluated the effect of LLLT on pain control after placement of separators. They observed mean level of pain was lower in LLLT group than placebo group, but the results were not statistically significant.[19] Yousef et al.,[23] found that pain severity in the laser group was in the lower level. Artes-Ribas et al.,[24] evaluated the pain sensation that orthodontic patients experience when elastic separators are placed between molars and premolars and to determine the degree of analgesic efficacy of LLLT compared to a placebo treatment. They found that pain intensity was significantly lower in the laser-treated quadrant (mean, 7.7 mm) than in the placebo-treated quadrant (mean, 14.14 mm; P = 0.0001). It seems the results of studies are controversial and our study shows the mean level of pain in both control and test sides, whether before or after laser irradiation are not statistically different. The only exception is the 2nd day after laser therapy, which in this time the mean level of pain in the test side was significantly lower than the control side (P = 0.009). The mean level of pain was reduced gradually by time significantly (P = 0.005) on both sides.
CONCLUSIONS
The maximum level of pain was recorded 1 day after separator placement.
Pain caused by separator was reduced significantly in both laser group and control group by passing time.
The mean rank of pain in both groups was not statistically significant except for the 2nd day after laser irradiation.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Bondemark L, Fredriksson K, Ilros S. Separation effect and perception of pain and discomfort from two types of orthodontic separators. World J Orthod. 2004;5:172–6. [PubMed] [Google Scholar]
- 2.Ngan P, Kess B, Wilson S. Perception of discomfort by patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1989;96:47–53. doi: 10.1016/0889-5406(89)90228-x. [DOI] [PubMed] [Google Scholar]
- 3.Ngan P, Wilson S, Shanfeld J, Amini H. The effect of ibuprofen on the level of discomfort in patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1994;106:88–95. doi: 10.1016/S0889-5406(94)70025-7. [DOI] [PubMed] [Google Scholar]
- 4.Michelotti A, Farella M, Martina R. Sensory and motor changes of the human jaw muscles during induced orthodontic pain. Eur J Orthod. 1999;21:397–404. doi: 10.1093/ejo/21.4.397. [DOI] [PubMed] [Google Scholar]
- 5.Kluemper GT, Hiser DG, Rayens MK, Jay MJ. Efficacy of a wax containing benzocaine in the relief of oral mucosal pain caused by orthodontic appliances. Am J Orthod Dentofacial Orthop. 2002;122:359–65. doi: 10.1067/mod.2002.126405. [DOI] [PubMed] [Google Scholar]
- 6.Oliver RG, Knapman YM. Attitudes to orthodontic treatment. Br J Orthod. 1985;12:179–88. doi: 10.1179/bjo.12.4.179. [DOI] [PubMed] [Google Scholar]
- 7.Asham AA. Readers’ forum: Orthodontic pain. Am J Orthod Dentofacial Orthop. 2004;125:18A. doi: 10.1016/j.ajodo.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 8.Keim RG. Managing orthodontic pain. J Clin Orthod. 2004;38:641–2. [PubMed] [Google Scholar]
- 9.Brown DF, Moerenhout RG. The pain experience and psychological adjustment to orthodontic treatment of preadolescents, adolescents, and adults. Am J Orthod Dentofacial Orthop. 1991;100:349–56. doi: 10.1016/0889-5406(91)70073-6. [DOI] [PubMed] [Google Scholar]
- 10.Haynes S. Discontinuation of orthodontic treatment relative to patient age. J Dent. 1974;2:138–42. doi: 10.1016/0300-5712(74)90041-4. [DOI] [PubMed] [Google Scholar]
- 11.O’Connor PJ. Patients’ perceptions before, during, and after orthodontic treatment. J Clin Orthod. 2000;34:591–2. [PubMed] [Google Scholar]
- 12.Bergius M, Kiliaridis S, Berggren U. Pain in orthodontics. A review and discussion of the literature. J Orofac Orthop. 2000;61:125–37. doi: 10.1007/BF01300354. [DOI] [PubMed] [Google Scholar]
- 13.Firestone AR, Scheurer PA, Burgin WB. Patients’ anticipation of pain and pain-related side effects, and their perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1999;21:387–96. doi: 10.1093/ejo/21.4.387. [DOI] [PubMed] [Google Scholar]
- 14.Scheurer PA, Firestone AR, Burgin WB. Perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1996;18:349–57. doi: 10.1093/ejo/18.4.349. [DOI] [PubMed] [Google Scholar]
- 15.Smith RJ, Burstone CJ. Mechanics of tooth movement. Am J Orthod. 1984;85:294–307. doi: 10.1016/0002-9416(84)90187-8. [DOI] [PubMed] [Google Scholar]
- 16.Ferreira SH, Nakamura M, de Abreu Castro MS. The hyperalgesic effects of prostacyclin and prostaglandin E2. Prostaglandins. 1978;16:31–7. doi: 10.1016/0090-6980(78)90199-5. [DOI] [PubMed] [Google Scholar]
- 17.Polat O, Karaman AI, Durmus E. Effects of preoperative ibuprofen and naproxen sodium on orthodontic pain. Angle Orthod. 2005;75:791–6. doi: 10.1043/0003-3219(2005)75[791:EOPIAN]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Raji SH, Birang R, Majdzade F, Ghorbanipour R. Evaluation of shear bond strength of orthodontic brackets bonded with Er-YAG laser etching. Dent Res J (Isfahan) 2012;9:288–93. [PMC free article] [PubMed] [Google Scholar]
- 19.Lim HM, Lew KK, Tay DK. A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic postadjustment pain. Am J Orthod Dentofacial Orthop. 1995;108:614–22. doi: 10.1016/s0889-5406(95)70007-2. [DOI] [PubMed] [Google Scholar]
- 20.Bernhardt MK, Southard KA, Batterson KD, Logan HL, Baker KA, Jakobsen JR. The effect of preemptive and/or postoperative ibuprofen therapy for orthodontic pain. Am J Orthod Dentofacial Orthop. 2001;120:20–7. doi: 10.1067/mod.2001.115616. [DOI] [PubMed] [Google Scholar]
- 21.Erdinc AM, Dincer B. Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod. 2004;26:79–85. doi: 10.1093/ejo/26.1.79. [DOI] [PubMed] [Google Scholar]
- 22.Turhani D, Scheriau M, Kapral D, Benesch T, Jonke E, Bantleon HP. Pain relief by single low-level laser irradiation in orthodontic patients undergoing fixed appliance therapy. Am J Orthod Dentofacial Orthop. 2006;130:371–7. doi: 10.1016/j.ajodo.2005.04.036. [DOI] [PubMed] [Google Scholar]
- 23.Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M. The effect of low-level laser therapy during orthodontic movement: A preliminary study. Lasers Med Sci. 2008;23:27–33. doi: 10.1007/s10103-007-0449-7. [DOI] [PubMed] [Google Scholar]
- 24.Artés-Ribas M, Arnabat-Dominguez J, Puigdollers A. Analgesic effect of a low-level laser therapy (830 nm) in early orthodontic treatment. Lasers Med Sci. 2012;28:335–41. doi: 10.1007/s10103-012-1135-y. [DOI] [PubMed] [Google Scholar]


