Abstract
Background
The usual-frequency case-crossover method, comparing exposure before an event with typical exposure of the same person, is widely used to estimate the risk of injury related to acute alcohol use. Prior results suggest that risk estimates might be biased upward compared with other methods.
Methods
Using data from 15 emergency-room studies in 7 countries, we compared the usual-frequency case-crossover method with case-control analysis, using non-injury patients as controls. Control-crossover analysis was performed to examine potential bias and to adjust risk estimates.
Results
The cross-study pooled odds ratio (OR) of injury related to drinking was 4.7 (2.6–8.5) in case-crossover analysis and 2.1 (1.6–2.7) in case-control analysis. A control-crossover analysis found an indication of bias (OR=2.2 [1.8–2.8]), which was larger among less frequent drinkers.
Conclusion
Findings suggest that the potential overestimation of injury risk based on the usual-frequency case-crossover method might be best explained by recall bias in usual-frequency estimates.
The case-crossover design was introduced to evaluate the effect of transient exposures on the risk of acute outcomes.1,2 One application has been in studies of emergency-room patients to estimate the risk of injury related to alcohol consumption. Unlike traditional case-control studies using non-injury emergency-room patients3 or community samples4 as controls, the case-crossover design compares injury patients’ drinking before the event with their own alcohol intake during an earlier control period. Two commonly used approaches to assessing exposures for the control period are the usual frequency of drinking (e.g., within the last year) 5–8 and drinking during one or several matched prior intervals (e.g., the same time one week before injury).6,9–11
Results from previous studies, however, suggest that risk estimates produced using the usual-frequency case-crossover method might be biased upward when compared with other methods. For example, the usual-frequency method generated larger estimates than the matched interval case-crossover method in the two studies employing both approaches.6,9 A usual-frequency case-crossover analysis on emergency-room data in 16 countries produced a pooled odds ratio (OR) of 5.7 (95% confidence interval (CI)= 4.0–8.0) for injury related to any drinking,7 substantially larger than the pooled odds ratio of 1.6 (1.2–1.9) from a 5-country case-control study using non-injury patient controls.12
This study examines potential bias using the usual-frequency case-crossover method, compared with the case-control design for estimating risk of injury from drinking. A case-crossover analysis on control (i.e., non-injury) patients (called the control-crossover approach) is also conducted to inform this comparison. Because the excess risk with control-crossover is expected to be zero, the approach has been widely used in case-crossover studies as a validity check and to adjust biased estimates.9,13–18
METHODS
Our analyses are based on data from the Emergency Room Collaborative Alcohol Analysis Project,12,19 including 15 studies (each typically covering a city or region) in 7 countries. Data from probability samples of emergency-room patients admitted for injury or illness were collected using a similar methodology.20 By using data from various regions around the world, findings from these analyses are more robust, with risk estimates examined in various socioeconomic and cultural conditions thought to be associated with alcohol use and injury, as well as varying levels of emergency-room utilization.
Cases and controls were defined as patients who reported their primary reason for visiting the emergency room as either injury or non-injury illness. Injury and non-injury patients were compared in case-control analysis, whereas only injury patients were used in the case-crossover analysis and only non-injury patients in the control-crossover analysis. For the injury and non-injury samples, exposure to acute drinking was defined as consumption of any alcoholic beverage by the patient during the six-hour period prior to either the injury or the illness event that led to their emergency room visit.
In case-control analysis, adjusted ORs were estimated from unconditional logistic regressions comparing acute drinking between injury and non-injury patients, controlling for sex and age. For the usual-frequency case- or control-crossover analysis, risk estimates were generated comparing acute drinking of the injury or non-injury patients before the event to their usual frequency of drinking. The case or control-crossover analysis can be considered as a stratified self-matched case-control analysis with the OR generated from the Mantel-Haenszel estimator for dichotomous exposure21 (any drinking versus none). Maclure1 showed that for the usual-frequency case-crossover analysis, the OR can be derived by dividing the total expected unexposed periods of the acutely exposed cases by the total expected exposed periods of the acutely unexposed cases. The expected exposed periods were obtained from subjects’ usual frequency of drinking during last 12 months. To be consistent with the acute drinking assessment, a 6-hour period was also used as the effect period for each occasion of any alcohol use in the control period. The expected unexposed periods were derived by subtracting the expected number of exposed periods from the total number of possible 6-hour periods each year, defined as 365•3, which excluded one six-hour sleeping period each day.22
The control-adjusted case-crossover estimates were obtained by dividing ORs from the case-crossover by those from the control-crossover analysis. In addition to study-specific estimates, we also estimated the pooled overall effect using a meta-analytic method23 of weighted average, taking into account the standard errors of the study-specific estimates. Only random-effect estimates are reported in Table 1, given that the homogeneity test yielded very small p-values.
Table 1.
Odds Ratios and 95% Confidence Intervals for Injury Related to Drinking from Case-control and Usual-Frequency Case-crossover Analysis, and ORs from Control-crossover Analysis, by Study Location and Pooled Estimates
| Studies | No. injured (No. exposeda) | No. not injured (No. exposeda) | Case-control ORs (95%CIs) | Case-crossover ORs (95%CIs) | Control-crossover ORs (95%CIs) | Case-crossover Adj ORsb (95%CIs) |
|---|---|---|---|---|---|---|
| San Francisco, CA, US | 550 (191) | 1,276 (199) | 2.6 (2.1–3.3) | 5.7 (4.6–7.0) | 1.8 (1.5–2.1) | 3.2 (2.4–4.1) |
| Contra Costa, CA, US | 1,001 (190) | 1,363 (194) | 1.1 (0.9–1.4) | 2.9 (2.4–3.4) | 3.2 (2.7–3.8) | 0.9 (0.7–1.1) |
| Kaiser hospital, CA, US | 410 (34) | 546 (39) | 1.0 (0.6–1.7) | 1.1 (0.8–1.6) | 1.6 (1.2–2.3) | 0.7 (0.4–1.1) |
| Jackson, MS, US | 275 (62) | 739 (48) | 3.0 (1.9–4.5) | 7.8 (5.4–11.1) | 2.2 (1.6–3.0) | 3.5 (2.2–5.6) |
| Santa Clara, CA, US | 288 (44) | 988 (62) | 2.3 (1.5–3.6) | 3.0 (2.1–4.4) | 2.0 (1.5–2.7) | 1.5 (0.9–2.4) |
| Mexico City, Mexico | 1,609 (434) | 533 (43) | 3.0 (2.2–4.3) | 24.0 (20.8–27.8) | 4.1 (2.8–5.9) | 5.9 (4.0–8.7) |
| Acapulco, Mexico | 342 (99) | 289 (30) | 3.0 (1.9–4.8) | 29.5 (21.8–39.9) | 4.4 (3.0–6.5) | 6.7 (4.1–10.9) |
| Pachuca, Mexico | 668 (96) | 727 (20) | 4.1 (2.5–6.9) | 18.1 (13.5–24.3) | 3.4 (2.1–5.6) | 5.3 (3.1–9.5) |
| Alberta, Canada | 335 (96) | 494 (44) | 3.6 (2.4–5.3) | 7.6 (5.7–10.0) | 2.3 (1.7–3.2) | 3.2 (2.1–5.0) |
| Quebec, Canada | 263 (41) | 387 (52) | 1.0 (0.6–1.6) | 3.6 (2.5–5.1) | 3.5 (2.6–4.7) | 1.0 (0.7–1.6) |
| Barcelona, Spain | 1,683 (262) | 679 (88) | 1.1 (0.9–1.5) | 1.1 (1.0–1.3) | 1.0 (0.8–1.3) | 1.1 (0.9–1.5) |
| Triste, Italy | 303 (118) | 157 (37) | 1.8 (1.1–2.8) | 2.9 (2.2–3.8) | 1.4 (0.9–2.0) | 2.1 (1.3–3.3) |
| Mar del Plata, Argentina | 378 (85) | 417 (44) | 1.9 (1.2–2.8) | 3.0 (2.3–3.8) | 1.5 (1.1–2.1) | 2.0 (1.3–3.0) |
| Warsaw, Poland | 507 (45) | 205 (6) | 2.8 (1.1–6.8) | 2.4 (1.7–3.3) | 1.5 (0.6–3.8) | 1.5 (0.6–4.0) |
| Sosnowiec, Poland | 421 (67) | 306 (19) | 2.4 (1.4–4.2) | 3.7 (2.8–4.9) | 2.8 (1.6–4.7) | 1.4 (0.7–2.5) |
| Pooled estimatec | 2.1 (1.6–2.7) | 4.7 (2.6–8.5) | 2.2 (1.8–2.8) | 2.1 (1.5–3.1) |
Injured and not injured patients are exposed to acute drink if they consumed alcohol 6-hour before their injury or illness events
Adjusted ratios are case-crossover ORs divided by control-crossover ORs
Pooled random effects from meta-analysis.
RESULTS
As shown in Table 1, the usual-frequency case-crossover method produced ORs at least 1.5 times as large as the corresponding estimates from case-control analyses for 11 out of the 15 emergency-room studies, and 2 times the case-control results in 8 studies. The pooled OR was 4.7 (95% CI= 2.6–8.5) from case-crossover analysis, compared with 2.1 (1.6–2.7) from case-control analysis. This trend with case-crossover estimates was also seen in the control-crossover analysis. ORs were greater than 1.5 for 13 studies and greater than 2 for 9 studies. The control-crossover pooled OR was 2.2 (1.8–2.8), substantially larger than the expected estimate of 1. After adjusting the case-crossover estimate, based on the control-crossover estimate, the pooled adjusted case-crossover OR was 2.1 (1.5–3.1) – very close to 2.1 (1.6–2.7) from case-control analysis. The across-study Pearson correlation between the case-control and the unadjusted and adjusted case-crossover estimates (logarithm of ORs) improved from 0.75 to 0.84.
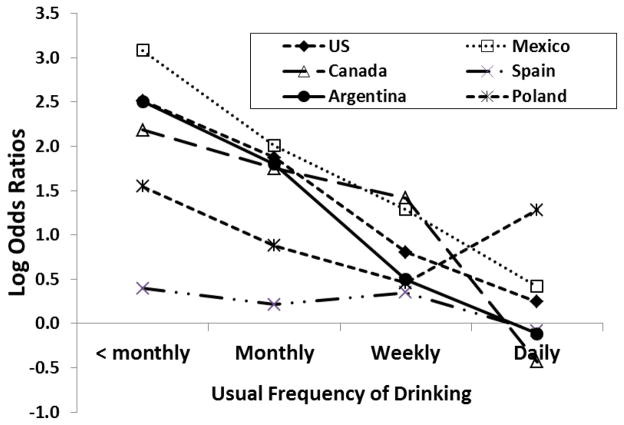
To examine the potential source of upward bias in the case-crossover estimates, we performed separate control-crossover analyses for subsamples at various drinking-frequency levels. For each frequency level, with all studies combined, the control-crossover ORs were quite similar to the ratio between the observed and expected exposure prevalence (Table 2). ORs generally decreased monotonically, from the lowest to the highest usual frequency level. The largest bias was found among those reporting the least frequent drinking (OR=15 for 1–5 times last year), while the estimate for “daily drinkers” was close to 1. Control-crossover analyses were also performed for each of the six countries separately, (Italy was dropped due to a small sample size) although with a slightly modified usual-frequency measure reduced to four categories. As shown in the Figure, clear monotonic relationships between the control-crossover estimates and usual frequency of drinking were observed for four of the six countries. One country exhibited no relationship (Spain, with log ORs close to zero for each usual-frequency level) and one appeared to be variable but with log ORs all above zero (Poland).
Table 2.
Odds Ratios from Control-crossover Analysis as well as Observed and Expected Exposure Prevalence Separately for Usual Frequency Levels, all Emergency Room Studies Combined
| Usual Frequency | No. | Observed Exposure prevalence before event (%) | Exposure prevalence expected from usual frequency (%) | Control-crossover ORs (95% CI) |
|---|---|---|---|---|
| 1 – 5 times last year | 1535 | 4.0 | 0.3 | 15.3 (11.9–19.8) |
| 6 – 11 times last year | 455 | 6.0 | 0.8 | 7.6 (5.2–11.2) |
| Once per month | 616 | 9.7 | 1.1 | 9.8 (7.5–12.7) |
| 2–3 times per month | 797 | 11.4 | 2.7 | 4.6 (3.7–5.7) |
| 1–2 times per week | 1012 | 18.3 | 7.1 | 2.9 (2.5–3.4) |
| 3–4 times per week | 485 | 26.0 | 16.6 | 1.8 (1.4–2.2) |
| (Nearly) every day | 1033 | 36.2 | 33.3 | 1.1 (1.0–1.3) |
Figure.
Control-crossover estimates by usual frequency of drinking for 6 counties.
DISCUSSION
Our comparisons between the case-control and case-crossover analysis and the control-crossover estimates show that the usual-frequency case-crossover method apparently overestimates the risk of injury related to drinking. In particular, the observed monotonic relationship between control-crossover estimates and usual frequency levels (where larger biases were associated with less-frequent drinking) may be most plausibly explained by recall bias. Survey estimates assessing annual alcohol volume, particularly estimates derived from usual-frequency and quantity measures, have consistently been found to account for only a fraction of per capita consumption from sales data.24 Our results suggest the bias is more likely among persons with a less consistent drinking pattern, who may thus have more difficulty recalling their drinking over time – particularly over an assessment period as long as 12 months.
One possible alternative explanation for the larger case-crossover estimates observed is that, among non-injury emergency room patients, some illnesses (e.g., myocardial infarction25) may be related to alcohol use prior to the event. To the extent this is true, estimates from the control-crossover analyses represent at least some elevated risk of non-injury illness associated with acute drinking, and case-control analyses may thus underestimate risk of injury to some extent. However, the clear monotonic relationship between usual frequency and control-crossover estimates are stronger evidence for recall bias than an effect of drinking on non-injury illness.
The cross-study pooled estimate from case-control analysis is virtually the same as that from case-crossover analysis after adjusting for potential bias suggested by control-crossover analysis (OR=2.1 for both). Not all study-specific results are similar, however. For example, case-crossover adjusted ORs in the three Mexican studies are all larger than case-control estimates, suggesting some inconsistencies not caused by random error. There has been debate regarding whether the two designs are comparable, with the case-control study asking “why is the event happening to me versus another person,” whereas the case-crossover analysis asks “why now versus another time.” 26 Conversely, both case-control and case-crossover designs can be linked to an underlying cohort study,21,27 and hypothetical examples have been constructed to show the equivalence of estimates from the two approaches if they follow the same assumed data-generating process.27 While the results from the two approaches might not necessarily converge, large discrepancies between their estimates suggest bias; here, recall bias seems a plausible candidate. This potential bias is not restricted to the usual-frequency case-crossover design for estimating the alcohol-injury relationship; it would potentially apply to any exposure based on self-reported data over a long retrospective window.
Acknowledgments
Source of Funding: Supported by grants from the U.S. National Institute on Alcohol Abuse and Alcoholism R01 AA013750 and P50 AA005595.
The paper is based on data collected by the following collaborators participating in the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP): Guilherme Borges (Mexico), Mariana Cremonte (Argentina), Norman Giesbrecht (Canada), Scott Macdonald (Canada), Jacek Moskalewicz (Poland), Flavio Poldrugo (Italy), Juan Rhodes (Spain), Grazyna Swiathiewicz (Poland), and Cheryl Cherpitel (U.S.)
Footnotes
Conflicts of Interest: There is no conflict of interest.
Contributor Information
Yu Ye, Alcohol Research Group, Public Health Institute, Emeryville, CA, USA.
Jason Bond, Alcohol Research Group, Public Health Institute, Emeryville, CA, USA.
Cheryl J. Cherpitel, Alcohol Research Group, Public Health Institute, Emeryville, CA, USA
Tim Stockwell, Center for Addictions Research of BC and, Department of Psychology, University of Victoria, Victoria, BC, Canada.
Scott Macdonald, Center for Addictions Research of BC and, School of Health Information Science, University of Victoria, Victoria, BC, Canada.
Jürgen Rehm, Centre for Addiction and Mental Health and, Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada. Epidemiological Research Unit, Technische Universität Dresden, Klinische Psychologie and Psychotherapie, Dresden, Germany.
References
- 1.Maclure M. The case-crossover design: a method for studying transient effect on the risk of acute events. American Journal of Epidemiology. 1991;133(2):144–53. doi: 10.1093/oxfordjournals.aje.a115853. [DOI] [PubMed] [Google Scholar]
- 2.Mittleman MA, Maclure M, Tofler GH, Sherwood JB, Goldberg RJ, Muller JE. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. The New England Journal of Medicine. 1993;329(23):1677–1683. doi: 10.1056/NEJM199312023292301. [DOI] [PubMed] [Google Scholar]
- 3.Cherpitel CJ. Alcohol and injuries: a review of international emergency room studies. Addiction. 1993;88(7):923–937. doi: 10.1111/j.1360-0443.1993.tb02110.x. [DOI] [PubMed] [Google Scholar]
- 4.Stockwell T, McLeod R, Stevens M, Phillips M, Webb M, Jelinek G. Alcohol consumption, setting, gender, and activity as predictors of injury: a population-based case-control study. Journal of Studies on Alcohol. 2002;63(3):372–379. doi: 10.15288/jsa.2002.63.372. [DOI] [PubMed] [Google Scholar]
- 5.Borges G, Cherpitel CJ, Mittleman M. The risk of injury after alcohol consumption: a case-crossover study in the emergency room. Social Science and Medicine. 2004;58(6):1191–1200. doi: 10.1016/s0277-9536(03)00290-9. [DOI] [PubMed] [Google Scholar]
- 6.Borges G, Cherpitel CJ, Mondragón L, Poznyak V, Peden M, Gutiérrez I. Episodic alcohol use and risk of nonfatal injury. American Journal of Epidemiology. 2004;159(6):565–571. doi: 10.1093/aje/kwh073. [DOI] [PubMed] [Google Scholar]
- 7.Borges G, Cherpitel CJ, Orozco R, Bond J, Ye Y, Macdonald S, Giesbrecht NA, Stockwell T, Cremonte M, Moskalewicz J, Swiatkiewicz G, Poznyak V. Acute alcohol use and the risk of non-fatal injury in sixteen countries. Addiction. 2006;101(7):993–1002. doi: 10.1111/j.1360-0443.2006.01462.x. [DOI] [PubMed] [Google Scholar]
- 8.Cherpitel CJ, Ye Y, Moskalewicz J, Swiatkiewicz G. Risk of injury: a case-crossover analysis of injured emergency service patients in Poland. Alcoholism: Clinical and Experimental Research. 2005;29(12):2181–2187. doi: 10.1097/01.alc.0000191771.44999.a1. [DOI] [PubMed] [Google Scholar]
- 9.Vinson DC, Mabe N, Leonard LL, Alexander J, Becker J, Boyer J, Moll J. Alcohol and injury. A case-crossover study. Archives of Family Medicine. 1995;4(6):505–511. doi: 10.1001/archfami.4.6.505. [DOI] [PubMed] [Google Scholar]
- 10.Vinson DC, MacLure M, Reidinger C, Smith GS. A population-based case-crossover and case-control study of alcohol and the risk of injury. Journal of Studies on Alcohol. 2003;64(3):358–366. doi: 10.15288/jsa.2003.64.358. [DOI] [PubMed] [Google Scholar]
- 11.Borges G, Cherpitel CJ, Orozco R, Bond J, Ye Y, Macdonald S, Rehm J, Poznyak V. Multicentre study of acute alcohol use and non-fatal injurie: data from the WHO collaborative study on alcohol and injuries. Bulletin of the World Health Organization. 2006;84(6):453–460. doi: 10.2471/blt.05.027466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cherpitel CJ, Bond J, Ye Y, Borges G, Macdonald S, Giesbrecht NA. A cross-national meta-analysis of alcohol and injury: data from the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) Addiction. 2003;98(9):1277–1286. doi: 10.1046/j.1360-0443.2003.00459.x. [DOI] [PubMed] [Google Scholar]
- 13.Marshall RJ, Wouters S, Jackson RT. A case-crossover analysis of a case-control study of alcohol consumption and coronary events: the effects of exposure definition and the use of control data. Journal of Epidemiology and Biostatistics. 2000;5(6):367–373. [PubMed] [Google Scholar]
- 14.Hallqvist J, Möller J, Ahlbom A, Diderichsen F, Reuterwall C, de Faire U. Does heavy physical exertion trigger myocardial infarction? A case-crossover analysis nested in a population-based case-referent study. American Journal of Epidemiology. 2000;151(5):459–467. doi: 10.1093/oxfordjournals.aje.a010231. [DOI] [PubMed] [Google Scholar]
- 15.Suissa S. The case-time-control design. Epidemiology. 1995;6(3):248–253. doi: 10.1097/00001648-199505000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Suissa S. The case-time-control design: further assumptions and conditions. Epidemiology. 1998;9(4):441–445. [PubMed] [Google Scholar]
- 17.Greenland S. A unified approach to the analysis of case-distribution (case-only) studies. Statistics in Medicine. 1999;18(1):1–15. doi: 10.1002/(sici)1097-0258(19990115)18:1<1::aid-sim961>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 18.Hernández-Díaz S, Hernán MA, Meyer K, Werler MM, Mitchell AA. Case-crossover and case-time-control designs in birth defects epidemiology. American Journal of Epidemiology. 2003;158(4):358–391. doi: 10.1093/aje/kwg144. [DOI] [PubMed] [Google Scholar]
- 19.Cherpitel CJ, Ye Y, Bond J. Alcohol and injury: multi-level analysis from the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) Alcohol and Alcoholism. 2004;39(6):552–558. doi: 10.1093/alcalc/agh091. [DOI] [PubMed] [Google Scholar]
- 20.Cherpitel CJS. A study of alcohol use and injuries among emergency room patients. In: Giesbrecht N, Gonzales R, Grant M, Österberg E, Room R, Rootman I, Towle L, editors. Drinking and Casualties: Accidents, poisonings and violence in an international perspective. New York: Tavistock/Routledge; 1989. pp. 288–299. [Google Scholar]
- 21.Rothman KJ, Greenland S. Modern epidemiology. 2. Philadelphia, PA: Lippincott-Raven Publishers; 1998. [Google Scholar]
- 22.Maclure M, Mittleman MA. Should we use a case-crossover design? Annual Review of Public Health. 2000;21:193–221. doi: 10.1146/annurev.publhealth.21.1.193. [DOI] [PubMed] [Google Scholar]
- 23.Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F. Methods for Meta-Analysis in Medical Research. Chichester, UK: John Wiley and Sons; 2000. [Google Scholar]
- 24.Rehm J. Measuring quantity, frequency, and volume of drinking. Alcoholism: Clinical and Experimental Research. 1998;22(Suppl 2):4S–14S. doi: 10.1097/00000374-199802001-00002. [DOI] [PubMed] [Google Scholar]
- 25.Gerlich MG, Krämer A, Gmel G, Maggiorini M, Lüscher TF, Rickli H, Kleger G-R, Rehm J. Patterns of alcohol consumption and acute myocardial infarction: a case-crossover analysis. European Addiction Research. 2009;15(3):143–149. doi: 10.1159/000213641. [DOI] [PubMed] [Google Scholar]
- 26.Maclure M. ‘Why me? ’ versus ‘why now’?–differences between operational hypotheses in case-control versus case-crossover studies. Pharmacoepidemiology and Drug Safety. 2007;16(850–853):8. doi: 10.1002/pds.1438. [DOI] [PubMed] [Google Scholar]
- 27.Greenland S. Confounding and exposure trends in case-crossover and case-time-control designs. Epidemiology. 1996;7(3):231–239. doi: 10.1097/00001648-199605000-00003. [DOI] [PubMed] [Google Scholar]