Abstract
Studies have shown that moderate alcohol use confers protection against some of the dominant predictors of long-term care placement, including diminished cognitive functioning, physical disability, and injury. But little is known about the association between alcohol use and the likelihood of placement in long-term care facilities. A nationally representative sample of 5,404 community-dwelling Canadians ages 50 years and older at baseline (1994/95) was obtained from the longitudinal National Population Health Survey. Alcohol use categories were developed based on the quantity and frequency of use in the 12 months before the interview. Cox proportional hazards models were used to estimate the association between alcohol use at baseline and subsequent placement in long-term care facilities after adjusting for covariates measured at baseline. During the 14-year follow-up period, 14% of lifetime abstainers, 10% of former drinkers, 7% of infrequent drinkers, 4% of moderate drinkers, and 3% of heavy drinkers were placed in long-term care facilities. Furthermore, the multivariate analysis revealed that abstainers, former drinkers, and infrequent drinkers were more than twice as likely to be placed in long-term care as moderate drinkers. Moderate drinking was protective against placement in long-term care facilities even after adjusting for an array of well-known confounders. The strong protective effect of moderate alcohol use on long-term care entry is likely due to a complex mix of physical, cognitive and psychosocial health factors.
Keywords: Alcohol, older adult, long-term care placement
1. INTRODUCTION
Epidemiological studies generally show that alcohol use starts to decline in middle through older age (Platt, Sloan, & Costanzo, 2010). Increasing morbidity with age may explain in part this decline (Shaper, 2011). However, lower alcohol use with age may not be evident in the entire population - a meta-analysis of longitudinal U.S. studies found that the average quantity of alcohol use significantly declined with age in older men, but not older women (Fillmore et al., 1991). Numerous studies show that alcohol in excess is harmful to health (Giesbrecht, Stockwell, Kendall, Strang, & Thomas, 2011; Latino-Martel et al., 2011); however, other studies demonstrate that alcohol use may be potentially beneficial in moderation (Kaplan et al., 2012; Ronksley, Brien, Turner, Mukamal, & Ghali, 2011). Complicating the picture, alcohol use in moderation may have beneficial effects regarding cardiovascular disease, but is associated with elevated risks for several cancers including those of the oral cavity, pharynx, larynx, esophagus, and liver (Latino-Martel et al., 2011).
Several studies using baseline alcohol use levels point to an association between moderate use and better health-related quality of life (HRQL) (Powers & Young, 2008), functional status (Chen & Hardy, 2009), cognitive health (Lang, Wallace, Huppert, & Melzer, 2007), subjective well-being (Lang et al., 2007), mental health (Lang et al., 2007), self-rated health (Turvey, Schultz, & Klein, 2006), absence of chronic illness (Mukamal et al., 2008), and lower mortality risk (Mukamal et al., 2008).
There is also some evidence that moderate alcohol use is associated with low rates of hospitalization and long-term care placement. Balsa et al. (2008) showed that older women consuming at least 12 drinks per year had reduced rates of hospitalization. In Australia, McCallum et al. (2005) found that any alcohol use reduced the risk of institutionalization by 45%. Similarly in China, Deng et al. (2006) found that moderate alcohol drinkers had a lower rate of nursing home placement. Many studies have shown that moderate alcohol use protects against some of the dominant predictors of long-term care placement such as diminished cognitive functioning (Chick, 1999; Lang et al., 2007; McGuire, Ajani, & Ford, 2007), physical disability (Cawthon et al., 2006), and injury (Peel, Bartlett, & McClure, 2007). In a review of the long-term effects of alcohol, Chick (1999) found that light drinking reduced cognitive decline. Other studies have found that problem drinking is associated with factors (e.g., disability, injury) leading to long-term care placement (Cawthon et al., 2007; Perreira & Sloan, 2002). A recent literature review found that cognitive and functional impairment were the most salient factors associated with long-term care placement (Luppa et al., 2010). However, none of the studies examined the role that alcohol use plays in the likelihood of long-term care placement in North America. Therefore, the present study assessed the association between alcohol use and placement in long-term care facilities in a large, representative sample of the Canadian population aged 50 years and older.
2. METHODS
2.1 Data Source
Data for this study derived from the 1994/95 to 2008/09 National Population Health Survey (NPHS). The longitudinal NPHS, conducted biennially by Statistics Canada, consisted of 17,276 noninstitutionalized members of private households in 1994/95 from all provinces, with the exclusion of individuals on Indian Reserves, Canadian Forces Bases and some remote areas in Québec and Ontario (Swain, Catlin, & Beaudet, 1999). In the initial cycle (i.e., baseline) of the NPHS (1994/95), the sample was created by first selecting households and then within each household choosing one member aged 12 and older to be the longitudinal respondent. The NPHS is based upon a complex design, with stratification and multiple stages of selection, and unequal probabilities of selection of respondents. The NPHS response rate at baseline was 83.6% and the average attrition rate across all the cycles for participants aged 50 years and older was 11.2%. The sample was representative of the Canadian population in 1994/95 (Swain et al., 1999). Panel members who died or who moved to long-term care facilities remain in the longitudinal sample. The present study focuses on 5,404 participants who were aged ≥ 50 years at baseline.
2.2 Dependent variable
Placement in a long-term care facility was operationalized using the longitudinal pattern variable, which was applied to respondents who had resided in long-term care facilities for 6 months or more. In the NPHS, a long-term care facility is defined as one that accommodates residents who need nursing and personal care on a continuing basis with medical supervision as required and that provides a minimum of 90 minutes of care per day to each resident. These facilities typically care for elderly residents but may also accommodate individuals with mental and physical disabilities as well as psychiatric patients. Specifically, long-term care facilities include nursing homes, residential care facilities, convalescent homes, seniors’ residences, and group homes (Statistics Canada, 2012).
2.3 Independent variables
The NPHS alcohol measures correspond to the Dawson and Room (2000) summary of recommendations and are compatible with suggestions in the World Health Organization (2000) report International Guide for Monitoring Alcohol Consumption and Related Harm. Respondents were categorized according to a classification scheme based on the baseline quantity and frequency of alcohol use in the 12 months prior to the interview.
Alcohol categories were chosen and adapted following Molander et al. (2010) and Powers et al. (2008). Many studies define moderate and heavy alcohol use with average daily consumption based on the weekly or monthly number of drinks (Powers & Young, 2008; Turvey et al., 2006). The NPHS provides a more precise set of questions regarding the number of drinks on each day of the week. Thus, we used the total number of drinks per week and the maximum number of drinks per day to define moderate and heavy drinkers. Using this scheme, moderate drinkers were defined as those having 1 to 14 drinks per week with ≤ 3 drinks per day for women or ≤ 4 drinks per day for men. Over 85% of moderate drinkers had ≤ 7 drinks per week. The other alcohol categories included life-long abstainers, former drinkers (no drinks in the past 12 months), infrequent drinkers (< 1 drink per week), and heavy drinkers (> 14 drinks per week or > 3 drinks per day for women or > 4 drinks per day for men).
2.4 Control variables
The control variables, identified in previous research, included baseline age, gender, marital status (married or not married), education (< 12, 12, or > 12 years), household income (< lower [< C$15,000] or ≥ middle to higher [≥C$15,000]), smoking (current or occasional, former, or never smoked), number of potentially life-threatening illnesses (high blood pressure, diabetes, heart disease, cancer, and/or stroke) (Ferraro & Farmer, 1999), number of other chronic illness (i.e., allergies, arthritis/rheumatism, chronic bronchitis, sinusitis, epilepsy, urinary incontinence, Alzheimer’s disease/dementia, glaucoma), body mass index, physical activity (measured with energy expenditure), HRQL, non-specific psychological distress (Kessler, Borges, & Walters, 1999), and past 12 months frequency of attending religious services (“not at all” to “once a week”). HRQL was assessed with the Health Utilities Index Mark 3 (HUI3) (Feeny, Furlong, Saigal, & Sun, 2004; Feeny et al., 2002). The HUI3 includes a functional status description system that is based on eight attributes: vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain/discomfort. There are five or six levels per attribute, ranging from no problem through severe disability. The overall HUI3 score ranges from −0.36 (highest possible level of disability across all attributes) to 1.00 (“perfect health”).
Physical activity was assessed with a continuous measure of energy expenditure (kcal/kg/day), which was based on the frequency and duration of 20 leisure-time activities (e.g., walking for exercise, yoga) over the previous three months (Statistics Canada, 2012). Nonspecific psychological distress was measured with six items on a 5-point Likert scale, ranging from “none of the time” (0) to “all of the time” (4). The participants indicated the frequency in the past month that they felt “so sad that nothing could cheer you up,” “nervous,” “restless or fidgety,” “hopeless,” “worthless,” or that “everything was an effort” (Kessler et al., 2002).
2.5 Statistical analysis
The association between alcohol use at baseline and subsequent placement in long-term care was examined using Cox proportional hazards models after adjusting for potential confounders. Individuals were censored at the time of their death, at the cycle for which they were lost to follow-up, or at the end of the follow-up period (December 2009). Three models were tested. The first (unadjusted) model assessed the effect of baseline alcohol levels on placement over the 14 years. The second model estimated the effect of the alcohol use categories on the likelihood of placement over 14 years, adjusting for age. The third model tested the effects of the alcohol use categories on the likelihood of placement over 14 years in a fully adjusted model. Moderate alcohol use was the reference group in all three models. Next, long-term care placement over 14 years was estimated for each statistically significant alcohol use category (relative to the referent group -- moderate alcohol use) using the Kaplan-Meier method. An analysis of Schoenfeld residuals was then used to assess the assumption of proportionality. Analyses were weighted to adjust for differential response rates and variation in probabilities of selection into the sample. The balanced repeated replication procedure using SAS-callable SUDAAN (Release 11.0; Research Triangle Institute, Research Triangle Park, N.C.) was used to adjust significance tests for the complex sample design. Replicated weights were provided by Statistics Canada.
3. RESULTS
Table 1 displays the baseline characteristics of the survey participants aged 50 years and older. Fifty-six percent of participants were women. The average age of the sample was 64 years. The majority of the sample was married (70%), in middle to higher income brackets (79%), and had at least a high school education (56%).
Table 1.
Characteristics of participants 50 years of age and older (n=5404)
| Baseline characteristics | All Percent (n) or Mean (SE) | Men Percent (n) or Mean (SE) | Women Percent (n) or Mean (SE) |
|---|---|---|---|
| Alcohol use | |||
| Lifetime abstainers | 11.9 (709) | 6.4 (140) | 16.5 (569) |
| Former | 18.8 (1123) | 15.7 (441) | 21.4 (682) |
| Infrequent | 30.1 (1577) | 29.1 (646) | 31.0 (931) |
| Moderate | 32.2 (1485) | 37.6 (753) | 27.6 (732) |
| Heavy | 7.0 (344) | 11.3 (251) | 3.5 (93) |
| Age in years | 64 (0.12) | 63 (0.16) | 65 (0.15) |
| Gender | |||
| Men | 45.9 (2322) | NA | NA |
| Women | 54.1 (3082) | NA | NA |
| Marital status | |||
| Married | 69.6 (3140) | 81.3 (1665) | 59.8 (1475) |
| Not married | 30.4 (2262) | 18.8 (655) | 40.2 (1607) |
| Educational attainment | |||
| <12 years | 44.2 (2585) | 43.6 (1118) | 44.8 (1467) |
| 12 years | 13.5 (658) | 11.8 (254) | 14.9 (404) |
| >12 years | 42.3 (2143) | 44.7 (940) | 40.3 (1203) |
| Household income | |||
| Lower | 20.2 (1415) | 16.2 (466) | 23.6 (949) |
| Middle/higher | 79.8 (3689) | 83.8 (1726) | 76.4 (1963) |
| Smoking status | |||
| Never | 37.4 (1960) | 21.6 (463) | 50.7 (1497) |
| Former | 41.1 (2147) | 53.6 (1212) | 30.6 (935) |
| Current/occasional | 21.5 (1152) | 24.9 (570) | 18.8 (582) |
| Body mass index (kg/m2) | 26.0 (0.08) | 26.4 (0.11) | 25.7 (0.11) |
| Physical activity (kcal/kg/day) | 1.4 (0.03) | 1.6 (0.05) | 1.3 (0.04) |
| HUI3 (range: −0.36 to 1.00) | 0.81 (0.00) | 0.83 (0.01) | 0.79 (0.01) |
| Non-specific psychological distress (range: 0 to 24) | 2.9 (0.06) | 2.4 (0.09) | 3.2 (0.09) |
| Perceived social support (range: 0 to 4) | 3.7 (0.01) | 3.6 (0.02) | 3.7 (0.02) |
| # medications (range: 0 to 11) | 1.9 (0.03) | 1.6 (0.04) | 2.1 (0.04) |
| # potentially life threatening chronic conditions (range: 0 to 5) | 0.5 (0.01) | 0.5 (0.02) | 0.5 (0.02) |
| # other chronic conditions (range: 0 to 9) | 1.0 (0.02) | 0.9 (0.03) | 1.1 (0.03) |
| Church attendance (range: 1 “not at all” to 5 “once a week”) | 3.0 (0.03) | 2.8 (0.05) | 3.2 (0.04) |
HUI3: Health Utilities Index Mark 3
Table 2 presents the baseline characteristics of participants aged 50 years and older for each alcohol use category. The results indicate that moderate drinkers were more likely to be younger, male, married, more physically active, have higher HUI3 scores, and lower levels of church attendance than the other categories. However, heavy drinkers were youngest of all groups and most likely to be male.
Table 2.
Characteristics of participants 50 years of age and older in each alcohol use category at baseline.
| Lifetime Abstainers Percent (n) or Mean (SE) | Former Drinkers Percent (n) or Mean (SE) | Infrequent Drinkers Percent (n) or Mean (SE) | Moderate Drinkers Percent (n) or Mean (SE) | Heavy Drinkers Percent (n) or Mean (SE) | |
|---|---|---|---|---|---|
| Age in years | 67 (0.61) | 67 (0.39) | 64 (0.28) | 62 (0.29)a,b,c,d | 60 (0.48) |
| Gender | |||||
| Men | 24.4 (140) | 38.0 (441) | 43.9 (646) | 53.3 (753)a,b,c,d | 72.8 (251) |
| Women | 75.6 (569) | 62.0 (682) | 56.1 (931) | 46.8 (732) | 27.2 (93) |
| Marital status | |||||
| Married | 60.1 (326) | 63.1 (573) | 66.9 (896) | 78.4 (1017)a,b,c | 73.9 (212) |
| Not married | 39.9 (383) | 36.9 (550) | 33.1 (681) | 21.6 (467) | 26.1 (132) |
| Educational attainment | |||||
| <12 years | 56.4 (429) | 54.7 (654) | 46.8 (764) | 31.2 (506) | 42.0 (151) |
| 12 years | 11.2 (64) | 12.5 (119) | 12.9 (194) | 15.1 (217) | 13.2 (44) |
| >12 years | 32.5 (211) | 32.9 (347) | 40.3 (617) | 53.6 (761) | 44.8 (149) |
| Household income | |||||
| Lower | 32.7 (279) | 29.5 (400) | 20.8 (420) | 10.8 (224)a,b,c | 17.6 (72) |
| Middle/higher | 67.4 (380) | 70.6 (667) | 79.2 (1081) | 89.2 (1187) | 82.4 (258) |
| Smoking status | |||||
| Never | 71.7 (499) | 38.9 (422) | 37.5 (567) | 29.3 (422)a,b | 11.7 (42) |
| Former | 17.0 (127) | 39.5 (463) | 42.2 (667) | 48.7 (722) | 48.5 (161) |
| Current/occasional | 11.3 (81) | 21.7 (238) | 20.3 (342) | 22.1 (341) | 39.8 (141) |
| Body mass index (kg/m2) | 25.9 (0.32) | 26.0 (0.18) | 26.2 (0.14) | 25.8 (0.12) | 26.3 (0.32) |
| Physical activity (kcal/kg/day) | 1.1 (0.08) | 1.2 (0.06) | 1.3 (0.05) | 1.7 (0.05)a,b,c | 1.5 (0.12) |
| HUI3 (range: −0.36 to 1.00) | 0.77 (0.01) | 0.73 (0.01) | 0.81 (0.01) | 0.85 (0.01)a,b,c | 0.84 (0.01) |
| Non-specific psychological distress (range: 0 to 24) | 3.1 (0.22) | 3.4 (0.16) | 2.8 (0.10) | 2.5 (0.09)b | 2.8 (0.26) |
| Perceived social support (range: 0 to 4) | 3.7 (0.04) | 3.6 (0.03) | 3.7 (0.03) | 3.7 (0.03) | 3.6 (0.07) |
| # medications (range: 0 to 11) | 1.9 (0.09) | 2.3 (0.08) | 1.9 (0.05) | 1.7 (0.05)b | 1.6 (0.09) |
| # potentially life threatening chronic conditions (range: 0 to 5) | 0.6 (0.05) | 0.6 (0.03) | 0.5 (0.02) | 0.4 (0.02)a,b | 0.4 (0.04) |
| # other chronic conditions (range: 0 to 9) | 1.0 (0.07) | 1.3 (0.05) | 1.0 (0.04) | 1.0 (0.03)b | 0.8 (0.07) |
| Church attendance (range: 1 “not at all” to 5 “once a week”) | 3.7 (0.08) | 3.1 (0.07) | 3.1 (0.06) | 2.8 (0.06)a,b,d | 2.2 (0.10) |
Mean and proportion differences for
lifetime abstainers,
former drinkers,
infrequent drinkers, and
heavy drinkers were compared to moderate drinkers using multinomial regression. Significance levels were adjusted for family-wise error using Bonferroni method. HUI3: Health Utilities Index Mark 3
Over the 14-year follow-up, 7% (n = 489) of the household population aged 50 or older at baseline was placed in long-term care. Fourteen percent of lifetime abstainers, 10% of former drinkers, 7% of infrequent drinkers, 4% of moderate drinkers, and 3% of heavy drinkers were placed in long-term care facilities.
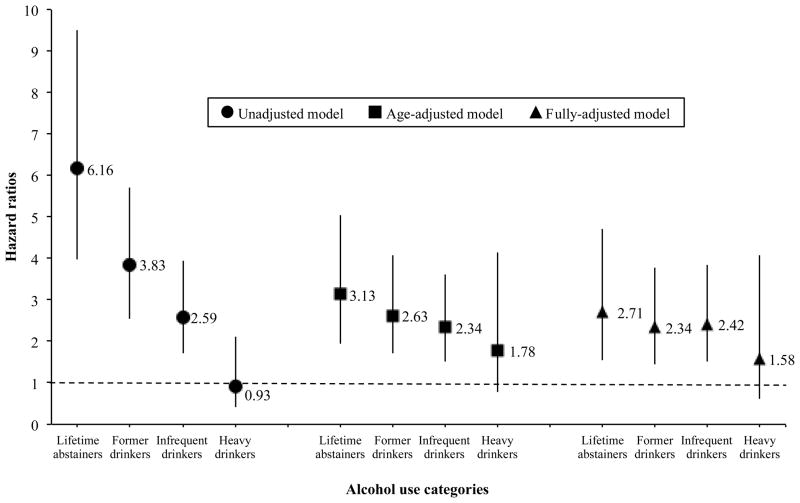
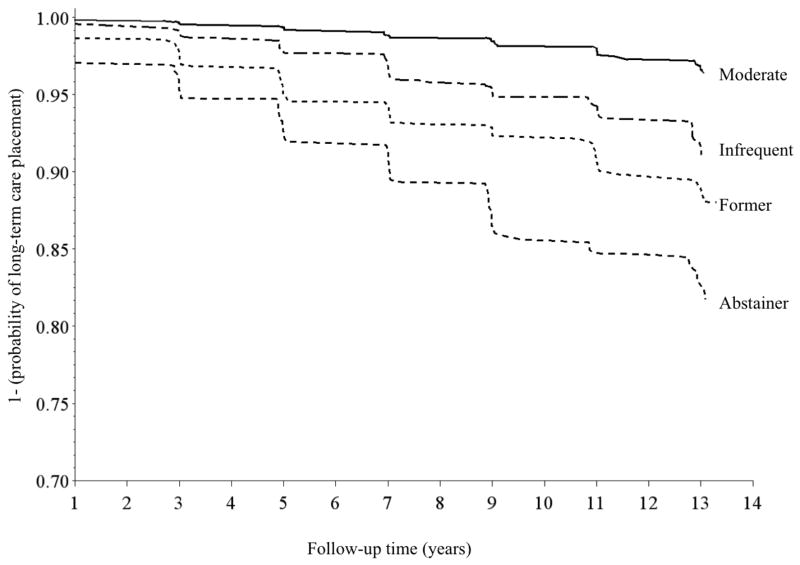
The effect of baseline alcohol use on long-term care placement was examined next. Figure 1 shows the unadjusted, age-adjusted, and fully-adjusted hazard ratios and 95% confidence intervals of being placed in long-term care facilities for lifetime abstainers, former drinkers, infrequent drinkers, and heavy drinkers relative to moderate drinkers. Results from the unadjusted Cox proportional hazards model show that abstainers, former drinkers, and infrequent drinkers were significantly more likely to be placed in long-term care than moderate drinkers. A related graphic depiction of the effects of baseline drinking status on long-term care placement over time appears in Figure 2. The Kaplan-Meier survival (free to long-term care placement) curves that represent infrequent drinkers, former drinkers, and abstainers show shorter time to long-term care placement compared to moderate drinkers. Because the heavy drinking category did not achieve statistical significance in the unadjusted Cox model, it was excluded from the Kaplan-Meier graph.
Figure 1.
Relative hazard of long-term care placement by alcohol use categories Moderate drinking was used as the reference category (dashed lines). The fully-adjusted model controlled for age, gender, marital status, educational attainment, household income, smoking status, body mass index, physical activity, Health Utilities Index Mark 3, non-specific psychological distress, perceived social support, number of medications, number of potentially life-threatening conditions, number of other chronic conditions, and church attendance. Error bars indicate 95% Confidence Interval.
Figure 2.
Kaplan-Meier estimates for survival free of long-term care placement by drinking status at baseline
Notice that the fully-adjusted Cox proportional hazards model (Figure 1) shows that abstainers were more than twice as likely to be placed in long-term care as moderate drinkers. Former and infrequent drinkers were also at higher risk for placement than moderate drinkers. Conversely, in all three Cox models, the heavy drinkers were not statistically significantly different from the moderates. This finding presumably reflects the modest sample size for heavy drinkers (n = 344) as well as the small numbers (n = 12) of heavy drinkers who were placed in long-term care. Of note, Schoenfeld residual analysis showed that the final model did not violate the proportionality assumption.
4. DISCUSSION
Overall, there is evidence that alcohol use measured at baseline in a representative sample of community-dwelling older adults is associated with long-term care placement. Specifically, lifetime abstainers, former drinkers, and infrequent drinkers were more likely to be placed over the 14-year study period. In contrast, moderate alcohol use at baseline appears to attenuate the risk of long-term care placement. The size of the effect of moderate alcohol use on the reduction of risk for entering long-term care in this population-based sample of Canadians is large even when compared to well-established risks for entry into long-term care like being older, female, and having poorer mental and physical health status (McCann, Donnelly, & O’Reilly, 2012). Further to this point, moderate drinkers maintained their favorable risk profile even with adjustment for an extensive number of confounding factors.
These findings appear to be consistent with previous studies. Asakawa and colleagues (2009) using the 1996/97 NPHS community and institutional samples found that HUI3 score, age, marital status, smoking, and alcohol (current versus not current drinker) were associated with the probability of being in an institution, with current drinkers less likely to reside in a long-term care facility than non-drinkers. This finding might in part be explained by research that has shown that moderate alcohol use lowers mortality risk and risk for declines in functional limitations in older adults (Lee et al., 2009). Although there may be unmeasured confounding related to lifetime alcohol abstention or being a former drinker (i.e., a “sick quitter”) that may elevate the risks of these factors for long-term care placement over moderate drinkers, our adjustments for health status (e.g., number of long-term chronic conditions) should diminish this problem. The alcohol use classification scheme also reduces this concern, as individuals who have quit drinking due to an illness that might put them at risk for long-term care placement should be in the former drinker category. Nonetheless, the highest risk for entry into long-term care is for the lifetime abstainers when compared with moderate drinkers.
The protective effect of moderate alcohol use on long-term care entry here could also operate through non-physical health-related traits of moderate drinkers compared to those who abstain. Rodgers et al. (2000) demonstrated higher depression and anxiety levels in non-drinkers and occasional drinkers compared with moderate drinkers. Our analysis also adjusted, to some degree, for mental health factors known to be associated with problem drinking. These same researchers (Rodgers et al., 2000) observed, however, that abstainers and occasional drinkers scored lower on psychological traits such as extraversion, fun seeking and drive. Other research has pointed to higher social inadequacy in abstainers compared to those who drink alcohol (Koppes, Twisk, Snel, De Vente, & Kemper, 2001). These latter unmeasured traits may be associated with willingness or desire to enter long-term care facilities and suggests that the strong protective effect of moderate alcohol use on long term care entry is likely due to a complex mix of physical, cognitive and psychosocial health factors.
The strengths of this study lie in the prospective population-based design, large sample, high participation rate, and long follow-up period of the NPHS. Furthermore, the study examined older people who are an important demographic sub-group that has often been overlooked when examining alcohol use throughout the life course. That being said, some limitations should be kept in mind when interpreting the results. First, the cumulative attrition rate over 8 cycles among those 50 and older was 44% (mostly due to mortality). Second, alcohol intake and health status measures were self-reported with potential reporting biases (e.g., underreporting alcohol intake due to social desirability response bias). There may also be recall bias if some participants were not able to remember accurately their alcohol intake (e.g., how many drinks on each day of the previous week). Third, the survey did not collect information on the size of or on the absolute alcohol level within each drink. Similarly, there were no data regarding the types of beverages consumed (i.e., beer, wine, or distilled spirits). Fourth, there were few older heavy drinkers placed in long-term care facilities. Consistent with other studies (see e.g., Hoeck & Van Hal, 2012; Karlamangla et al., 2009; Kirchner et al., 2007), the results might be subject to survival bias, particularly among older heavy drinkers. Finally, alcohol use may change over time, which may be associated with health problems and the increased likelihood of long-term care placement. However, most older drinkers do not change drinking category, but when they do change they do so to an adjacent category (Kaplan et al., 2012).
The finding that former drinkers are at elevated risk of placement in a long-term care facility is consistent with the “sick quitter” hypothesis, which says that declines in health and/or use of prescription drugs that interact with alcohol lead people to reduce or eliminate their use of alcohol. In other words, the decline in health causes discontinuation of alcohol use. However, given that the risk of placement is higher among lifetime abstainers than among former drinkers, the “sick quitter” hypothesis does not fully account for the associations reported herein.
It is important to note that this study did not use an experimental design and that observational data cannot fully disentangle the complex relationship between moderate drinking and long-term care placement. There may be residual confounders explaining this relationship. For example, moderate drinkers have been shown to have higher social engagement, socioeconomic status, well-being, and better physical and psychological health (Peele & Brodsky, 2000). Thus, we are not suggesting that prescribing alcohol would protect against placement in long-term care; however, health care professionals need to recognized the benefits of moderate drinking and should answer questions about alcohol use while keeping the potential beneficial effects of moderate use in mind.
Highlights.
We assessed the association between alcohol use and placement in long-term care facilities.
A nationally representative sample of 5,404 community-dwelling adults aged ≥50 years at baseline was followed for 14 years.
Compared to moderate users, lifetime abstainers, former drinkers, and infrequent drinkers were more likely to be placed in long-term care facilities over time.
Acknowledgments
Funding
The National Institute on Aging grant AG33796 supported preparation of this work and the research described herein. All analyses, interpretations, and conclusions based on the analysis of these data are solely the responsibility of the authors.
Abbreviations
- NPHS
National Population Health Survey
- HRQL
health-related quality of life
- HUI3
Health Utilities Index Mark 3
Footnotes
Contributors
MK originated the study, led the writing, and synthesized the analyses. BMcF, DF, and NH provided important intellectual content and helped draft the manuscript. NH, LO, PR-M conducted the data analysis. BMcF and JB provided statistical expertise. RC, NG and NR helped conceptualize ideas, interpret findings and review drafts of the manuscript. All the authors reviewed and approved the final draft.
Conflict of Interest
David Feeny, has a proprietary interest in Health Utilities Incorporated, Dundas, Ontario, Canada. HUInc. distributes copyrighted Health Utilities Index (HUI) materials and provides methodological advice on the use of HUI. None of the other authors have any interests that might be interpreted as influencing the research.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Asakawa K, Feeny D, Senthilselvan A, Johnson JA, Rolfson D. Do the determinants of health differ between people living in the community and in institutions? Social Science and Medicine. 2009;69(3):345–353. doi: 10.1016/j.socscimed.2009.05.007. [DOI] [PubMed] [Google Scholar]
- Balsa AI, Homer JF, Fleming MF, French MT. Alcohol consumption and health among elders. The Gerontologist. 2008;48(5):622–636. doi: 10.1093/geront/48.5.622. [DOI] [PubMed] [Google Scholar]
- Cawthon PM, Fink HA, Barrett-Connor E, Cauley JA, Dam TT, Lewis CE, Cummings SR. Alcohol use, physical performance, and functional limitations in older men. Journal of the American Geriatrics Society. 2007;55(2):212–220. doi: 10.1111/j.1532-5415.2007.01062.x. [DOI] [PubMed] [Google Scholar]
- Cawthon PM, Harrison SL, Barrett-Connor E, Fink HA, Cauley JA, Lewis CE, Cummings SR. Alcohol intake and its relationship with bone mineral density, falls, and fracture risk in older men. Journal of the American Geriatrics Society. 2006;54(11):1649–1657. doi: 10.1111/j.1532-5415.2006.00912.x. [DOI] [PubMed] [Google Scholar]
- Chen LY, Hardy CL. Alcohol consumption and health status in older adults: a longitudinal analysis. Journal of Aging and Health. 2009;21(6):824–847. doi: 10.1177/0898264309340688. [DOI] [PubMed] [Google Scholar]
- Chick J. Can light or moderate drinking benefit mental health? European Addiction Research. 1999;5(2):74–81. doi: 10.1159/000018969. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Room R. Towards agreement on ways to measure and report drinking patterns and alcohol-related problems in adult general population surveys: the Skarpo conference overview. Journal of Substance Abuse. 2000;12(1–2):1–21. doi: 10.1016/s0899-3289(00)00037-7. [DOI] [PubMed] [Google Scholar]
- Deng J, Zhou DH, Li J, Wang YJ, Gao C, Chen M. A 2-year follow-up study of alcohol consumption and risk of dementia. Clinical Neurology and Neurosurgery. 2006;108(4):378–383. doi: 10.1016/j.clineuro.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Feeny D, Furlong W, Saigal S, Sun J. Comparing directly measured standard gamble scores to HUI2 and HUI3 utility scores: group- and individual-level comparisons. Social Science and Medicine. 2004;58(4):799–809. doi: 10.1016/s0277-9536(03)00254-5. [DOI] [PubMed] [Google Scholar]
- Feeny D, Furlong W, Torrance GW, Goldsmith CH, Zhu Z, DePauw S, Boyle M. Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Medical Care. 2002;40(2):113–128. doi: 10.1097/00005650-200202000-00006. [DOI] [PubMed] [Google Scholar]
- Ferraro KF, Farmer MM. Utility of health data from social surveys: is there a gold standard for measuring morbidity? American Sociological Review. 1999;64:303–315. [Google Scholar]
- Fillmore KM, Hartka E, Johnstone BM, Leino EV, Motoyoshi M, Temple MT. A meta-analysis of life course variation in drinking. British Journal of Addiction. 1991;86(10):1221–1267. doi: 10.1111/j.1360-0443.1991.tb01702.x. [DOI] [PubMed] [Google Scholar]
- Giesbrecht N, Stockwell T, Kendall P, Strang R, Thomas G. Alcohol in Canada: reducing the toll through focused interventions and public health policies. Canadian Medical Association Journal = Journal de l’Association Medicale Canadienne. 2011;183(4):450–455. doi: 10.1503/cmaj.100825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, Feeny D, McFarland BH, Caetano R, Bernier J, Ross N. Alcohol use patterns and trajectories of health-related quality of life in middle-aged and older adults: a 14-year population-based study. Journal of Studies on Alcohol and Drugs. 2012;73(4):581–590. doi: 10.15288/jsad.2012.73.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56(7):617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Koppes LL, Twisk JW, Snel J, De Vente W, Kemper HC. Personality characteristics and alcohol consumption: longitudinal analyses in men and women followed from ages 13 to 32. Journal of Studies on Alcohol. 2001;62(4):494–500. doi: 10.15288/jsa.2001.62.494. [DOI] [PubMed] [Google Scholar]
- Lang I, Wallace RB, Huppert FA, Melzer D. Moderate alcohol consumption in older adults is associated with better cognition and well-being than abstinence. Age and Ageing. 2007;36(3):256–261. doi: 10.1093/ageing/afm001. [DOI] [PubMed] [Google Scholar]
- Latino-Martel P, Arwidson P, Ancellin R, Druesne-Pecollo N, Hercberg S, Le Quellec-Nathan M, Maraninchi D. Alcohol consumption and cancer risk: revisiting guidelines for sensible drinking. Canadian Medical Association Journal = Journal de l’Association Medicale Canadienne. 2011;183(16):1861–1865. doi: 10.1503/cmaj.110363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SJ, Sudore RL, Williams BA, Lindquist K, Chen HL, Covinsky KE. Functional limitations, socioeconomic status, and all-cause mortality in moderate alcohol drinkers. Journal of the American Geriatrics Society. 2009;57(6):955–962. doi: 10.1111/j.1532-5415.2009.02184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luppa M, Luck T, Weyerer S, Konig HH, Brahler E, Riedel-Heller SG. Prediction of institutionalization in the elderly. A systematic review. Age and Ageing. 2010;39(1):31–38. doi: 10.1093/ageing/afp202. [DOI] [PubMed] [Google Scholar]
- McCallum J, Simons LA, Simons J, Friedlander Y. Patterns and predictors of nursing home placement over 14 years: Dubbo study of elderly Australians. Australian Journal on Ageing. 2005;24(3):169–173. [Google Scholar]
- McCann M, Donnelly M, O’Reilly D. Gender differences in care home admission risk: partner’s age explains the higher risk for women. Age and Ageing. 2012;41(3):416–419. doi: 10.1093/ageing/afs022. [DOI] [PubMed] [Google Scholar]
- McGuire LC, Ajani UA, Ford ES. Cognitive functioning in late life: the impact of moderate alcohol consumption. Annals of Epidemiology. 2007;17(2):93–99. doi: 10.1016/j.annepidem.2006.06.005. [DOI] [PubMed] [Google Scholar]
- Molander RC, Yonker JA, Krahn DD. Age-related changes in drinking patterns from mid- to older age: results from the Wisconsin longitudinal study. Alcoholism: Clinical and Experimental Research. 2010;34(7):1182–1192. doi: 10.1111/j.1530-0277.2010.01195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamal KJ, Kennedy M, Cushman M, Kuller LH, Newman AB, Polak J, Siscovick DS. Alcohol consumption and lower extremity arterial disease among older adults: the cardiovascular health study. American Journal of Epidemiology. 2008;167(1):34–41. doi: 10.1093/aje/kwm274. [DOI] [PubMed] [Google Scholar]
- Peel NM, Bartlett HP, McClure RJ. Healthy aging as an intervention to minimize injury from falls among older people. Annals of the New York Academy of Sciences. 2007;1114:162–169. doi: 10.1196/annals.1396.026. [DOI] [PubMed] [Google Scholar]
- Peele S, Brodsky A. Exploring psychological benefits associated with moderate alcohol use: a necessary corrective to assessments of drinking outcomes? Drug and Alcohol Dependence. 2000;60(3):221–247. doi: 10.1016/s0376-8716(00)00112-5. [DOI] [PubMed] [Google Scholar]
- Perreira KM, Sloan FA. Excess alcohol consumption and health outcomes: a 6-year follow-up of men over age 50 from the health and retirement study. Addiction. 2002;97(3):301–310. doi: 10.1046/j.1360-0443.2002.00067.x. [DOI] [PubMed] [Google Scholar]
- Platt A, Sloan FA, Costanzo P. Alcohol-consumption trajectories and associated characteristics among adults older than age 50. Journal of Studies on Alcohol and Drugs. 2010;71(2):169–179. doi: 10.15288/jsad.2010.71.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers JR, Young AF. Longitudinal analysis of alcohol consumption and health of middle-aged women in Australia. Addiction. 2008;103(3):424–432. doi: 10.1111/j.1360-0443.2007.02101.x. [DOI] [PubMed] [Google Scholar]
- Rodgers B, Korten AE, Jorm AF, Christensen H, Henderson S, Jacomb PA. Risk factors for depression and anxiety in abstainers, moderate drinkers and heavy drinkers. Addiction. 2000;95(12):1833–1845. doi: 10.1046/j.1360-0443.2000.9512183312.x. [DOI] [PubMed] [Google Scholar]
- Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ: British Medical Journal. 2011;342:d671. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaper AG. Alcohol consumption decreases with the development of disease. Addiction. 2011;106(5):1023–1025. doi: 10.1111/j.1360-0443.2011.03372.x. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. National Population Health Survey. Household Component. Longitudinal - Cycle. 2012;9:2010–2011. Retrieved March, 22, 2013, from http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3225&Item_Id=1824&lang=en. [Google Scholar]
- Swain L, Catlin G, Beaudet MP. The National Population Health Survey--its longitudinal nature. Health reports. 1999;10(4):69–82. (ENG); 73–89(FRE) [PubMed] [Google Scholar]
- Turvey CL, Schultz SK, Klein DM. Alcohol use and health outcomes in the oldest old. Substance Abuse Treatment, Prevention and Policy. 2006;1:8. doi: 10.1186/1747-597X-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. International Guide for Monitoring Alcohol Consumption and Related Harm. Retrieved March. 2000;22:2013. from http://whqlibdoc.who.int/hq/2000/who_msd_msb_00.4.pdf. [Google Scholar]