Abstract
Background
Prior studies have found that students with overweight and obesity have impairments in performance IQ and executive function, and worse school functioning in comparison to normal weight peers.
Objectives
The current study assessed school and cognitive functioning in a sample of adolescents with severe obesity being evaluated for laparoscopic adjustable gastric banding. Setting: Psychiatry Department, University Medical Center, United States.
Methods
Eligible candidates for bariatric surgery were referred for psychiatric evaluation which included a semi-structured clinical interview measuring school functioning and the vocabulary and matrix reasoning subtests of the Wechsler Abbreviated Scale of Intelligence (WASI).
Results
Self-reported school problems were common, with 55.5% of adolescents failing a grade or subject, 38.7% attending summer school, and 17.8% failing a citywide exam. A significant relationship was observed between body mass index (BMI),estimated WASI IQ(r= −0.250, p=0.005), and the vocabulary subtest (r= −0.241, p=0.006), but not matrix reasoning (r= −0.126, p=NS).
Conclusions
Even among a sample of adolescents with severe obesity, increased BMI was associated with lower WASI IQ and vocabulary subtest scores. Increasing awareness of potential cognitive and school problems in bariatric candidates among teachers, school counselors, and other mental health providers is an important first step to improving academic support and educational systems deficiencies for students with overweight and obesity.
Keywords: Obesity, Adolescent, Cognitive Function, School performance, Bariatric Surgery
Introduction
With the alarmingly high rates of pediatric obesity, the need to identify effective treatment strategies for obesity and its related health and psychosocial comorbidities has also intensified. The National Health and Nutrition Examination Survey (NHANES) of 2007–2008 found 16.9% of children and adolescents in the U.S. were obese, as defined by sex-specific body mass index (BMI) for age growth charts. In addition to the substantial rates of obesity among youth, rates of extreme obesity are also growing rapidly with the prevalence of children and adolescents with a BMI greater than the 99th percentile increasing by more than 300% since 1976 (0.8% in 1976–1980 to 3.8% in 1999–2004)(1). Children and adolescents with obesity face significant stress, prejudice, and weight bias in multiple domains, including school, relationships, and healthcare(2). In childhood and adolescence school plays a critical role as a stage for development of academic ability, peer relationships, and of emotional maturity. School functioning and cognitive ability have been assessed using academic achievement in the classroom, academic achievement on nationalized tests, school attendance, and assessments of cognitive performance including IQ tests and measures of executive functioning.
Students with overweight demonstrate worse functioning in school in comparison to normal-weight peers. In a study of suburban 6th and 7th graders, Shore et al(3) found that students with overweight had a significantly lower grade point average and increased number of detentions, absences, and tardiness. Girls with obesity were 1.51 times more likely to report having been held back a year(4), and Tershakovecand colleagues(5)found that the proportion black inner-city children with obesity placed in special education or remedial class settings was twice that for non-obese children. Further, obesity is associated with 1.9 more days absent from school among inner-city 4th–6th graders when controlling for age, gender, race/ethnicity and school(6).
Children and adolescents with obesity also demonstrate impaired cognitive functioning, including lower performance IQ and other measures of cognitive function. Li(7) administered the Wechsler Intelligence Scale for Children (WISC) in China and observed that children with severe obesity had a significantly lower performance IQ score in comparison to controls. Moreover, adolescents with obesity with IQs in the average range performed significantly worse than normative data (mean z-score 0) on cognitive tests of digit span, verbal interference, switching of attention and a maze task demonstrating that neurocognitive deficits were confined to tests measuring executive functions (e.g. complex attention, mental flexibility, and disinhibition)(8). Phan et al(9) also showed that adolescents with obesity seeking bariatric surgery had a mean IQ in the average range; however, 21% of the sample had IQ scores that were borderline or extremely low (double what would be expected in a normative population).
The aforementioned studies, evaluated both academic and cognitive functioning, but did not examine both of these domains in the same population. The extant literature examines a range of variables across a number of samples, with different definitions of severe obesity, which limits comparisons with other research. Furthermore, the majority of these studies evaluate school function in the general population children and adolescents with obesity, and little is known about treatment-seeking youth with obesity.
Because there are no studies assessing both academic performance and cognitive function in the same sample, a more comprehensive examination of school functioning in adolescents with extreme obesity is needed to begin to explore the extent of problems in this group and reasons for impairments. The purpose of the current study was to assess school and cognitive functioning in a sample of adolescents with severe obesity being evaluated for bariatric surgery. We hypothesized that, even within this sample of adolescents with extreme obesity, increased BMI would be predictive of poorer academic and cognitive functioning.
Materials and Methods
Participants
Details of this study have been previously reported(10). Participants were adolescent surgical candidates with severe obesity enrolled in a university hospital bariatric surgery program. The 141 participants in the study were evaluated for Laparoscopic Adjustable Gastric Banding (LAGB; NCT01045499) and were required to meet eligibility criteria including: age between 14 and 17 years of age when enrolled, BMI > 40 kg/m2 or BMI > 35 kg/m2 with serious comorbid conditions, and a history of obesity of at least five years, including failed attempts at weight loss treatment.
Procedures
The surgical team described the LAGB procedure, potential risk and benefits, and obtained written informed consent from parents and assent from adolescents. Following initial screening, all eligible candidates were referred for psychiatric evaluation which includeda clinical interview with adolescent and parent. The Institutional Review Board reviewed and approved the research protocol.
Adolescents also completed the vocabulary and matrix reasoning subtests of the Wechsler Abbreviated Scale of Intelligence (WASI)(11), which provide an estimate of full scale intelligence quotient (product summary of vocabulary and matrix reasoning subtests). These subtests were intended to serve as a brief clinical screening tool and estimate of general cognitive functioning (Wechsler), as completing the full WASI in addition to other components of the initial psychiatric evaluation process was considered to be burdensome. Students with higher intelligence test scores show better scholastic achievement than students with lower intelligence test scores(12). Using the WASI allows us to examine this association in the current sample and assess school function controlling for IQ. Candidates were also given the Beck Depression Inventory (BDI)(13), as increased scores on the BDI are associated with poor academic achievement(14).
Clinical interviews were conducted by a psychologist or psychiatrist using a semi-structured interview template(15). School functioning questions included: history of evaluation by committee for special education, of special education placement and of neuropsychiatric or educational evaluation; school refusal; repeated grades; summer school attendance; failure of a grade or subjects or citywide exam; current grades; and, whether on schedule for high school graduation.
Statistical Analyses
Means are reported + standard deviations. Pearson’s correlation coefficients (r) were calculated to evaluate relationships between WASI scores, BMI, and measures of psychiatric symptoms. Independent samples t-tests were used to compare differences between measures of school performance and continuous demographic variables (age, BMI) and WASI IQ. Chi-square tests (Χ2) compared dichotomous demographic variables (gender) and school performance. Data for the t-tests assumed equal variances unless otherwise indicated. Given the expected relationship between WASI IQ and school performance, follow-up logistic regression analyses were conducted for significant relationships between BMI, psychiatric treatment, and school functioning to control for the relationship between WASI IQ and school functioning. Statistical calculations were performed by using SPSS for WINDOWS software (version 18; SPSS Inc, Chicago, IL).
Results
On average, participants were 15.79 + 1.13 years old (range 13–18) with a BMI of 48.19 + 8.22 kg/m2 (range 35.40–83.30 kg/m2). Adolescents and parents reported an age of onset of overweight of 5.9 + 3.9 years of age. Of the 141 adolescents, 70.9% of participants were female ((n=100), 36.9% were Caucasian (n=52), 36.9% were Hispanic/Latino (n=52), 19.9% were African American (n=28), and 6.4% were of another race (n=9).
Information about current and past psychiatric treatment and medical history was obtained during the clinical interview. A total of 30.0% adolescents were receiving psychotherapy at the time of the evaluation, 32.9% reported past psychotherapy, and 37.1% never received psychotherapy. A smaller percentage of adolescents indicated that they were prescribed psychiatric medications either currently (12.9%) or in the past (10.7%). Significant relationships were noted for school refusal and psychotherapy (Χ2(2)=14.61, p=0.001) and psychiatric medication (Χ2(2)=14.35, p=0.001), and failing a citywide exam and psychotherapy (Χ2(2)=6.22, p=0.05). Logistic regression was used to control for WASI IQ in these relationships, and only psychotherapy was still significantly related to school refusal, and it conferred a 3.2 greater likelihood of school refusal (pseudo r2 Cox and Snell=0.138, p < 0.001). Of those adolescents with school refusal, 14.3% had never received psychotherapy, 34.3% reported past psychotherapy, and 51.4% reported currently receiving psychotherapy.
Obesity-related medical conditions were reported in 27% of the sample, including type 2 diabetes, hypertension, sleep apnea, hypercholesterolemia and polycystic ovarian syndrome. The presence of an obesity-related medical condition was not significantly associated with any of the school functioning variables or WASI IQ score.
On the abbreviated WASI, the mean Full Scale IQ estimate among adolescents was 97.50 + 12.25 (range 62–124), which approximates a normal distribution for this measure. A total of 79.5% of participants had estimated IQs in the normal range (85–115), 7.9% had IQ estimates in the above average range (above 115), 10.2% had estimated IQs in the borderline intellectual functioning range (70–85) and 2.4% had IQ estimate consistent with the mild mental retardation (50–70). A significant inverse correlation was observed between BMI and WASI score (r= −0.250, p= 0.005) (see Figure 1). When examining individual subtests, scores on the vocabulary subtest were significantly related to BMI (r= −0.241, p=0.006); however, a significant relationship was not observed between the matrix reasoning subtest scores and BMI. Significant relationships were also not foundfor BMI and median household income or total BDI scores, and WASI IQ was not significantly related to total BDI scores.
Figure 1.
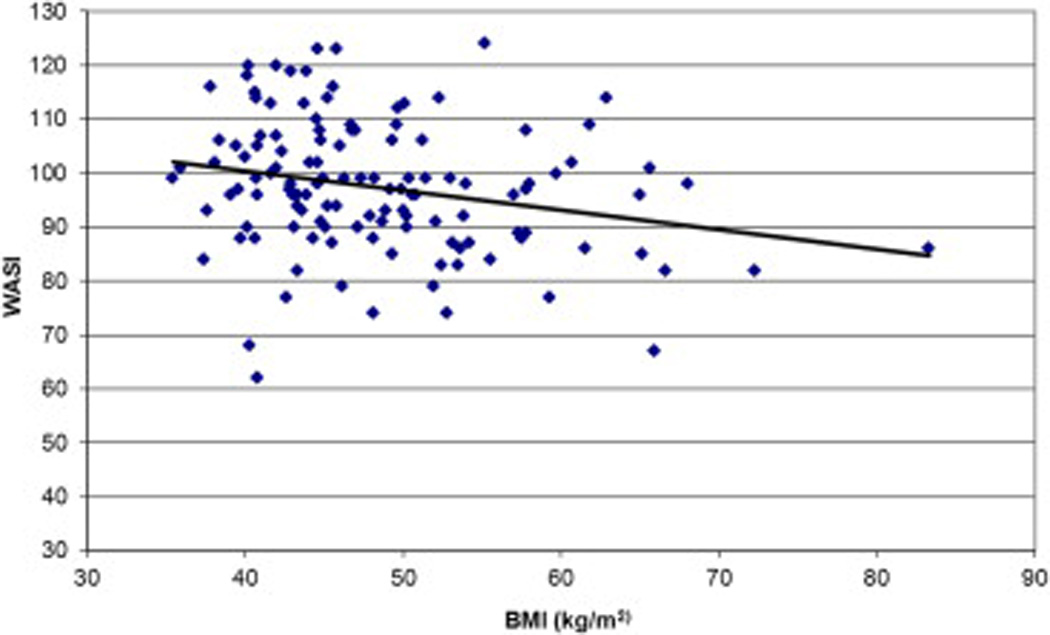
Relationship between Body Mass Index (BMI: kg/m2) and approximate IQ measured by Wechsler Abbreviated Scale of Intelligence (WASI)in 141 Bariatric Surgery Candidates on Initial Pre-Surgical Psychiatric Evaluation
Table 1 summarizes the proportion of adolescents reporting problems with school functioning. Age was not significantly related to any measure of school functioning. Among the sample, 2.8% reported that they were home schooled. A total of 68.2% of the sample reported the onset of overweight prior to first failing a grade, 22.7% reported failing a grade prior to the onset of overweight, and 9.1% reported the onset of overweight and obesity and failing a grade at the same age. A significant difference was found in the proportion of females refusing to attend school (30.6%) in comparison to males (12.5%; Χ2(1)=4.92, p=0.03) and in the proportion of males repeating a grade (27.5%) in comparison to females (9.2%; Χ2(1)=7.69, p=0.006).
Table 1.
Proportion of 141 Bariatric Surgery Candidates Reporting Problems with School Functioning on Initial Pre-Surgical Psychiatric Evaluation
| Female (%) |
Male (%) | Total (%) | |
|---|---|---|---|
| CSE Evaluation | 24 | 25 | 24.3 |
| School Refusal | 30.6* | 12.5 | 25.4 |
| Repeated Grades | 9.2* | 27.5 | 14.5 |
| Summer School | 37.8 | 41 | 38.7 |
| Failed a grade or subject | 4.1 | 59 | 55.5 |
| Failed a citywide exam | 15.6 | 23.1 | 17.8 |
| Neuropsychiatric/educational evaluation | 11.2 | 5 | 9.4 |
| Not “on schedule” for high school graduation | 13.5 | 7.9 | 11.9 |
Note: CSE= Committee on Special Education.
P< 0.05 male vs female
Significant relationships between median household income and several school functioning variables were observed: adolescents repeating a grade (t(135)=2.95, p=0.004), who failed a grade or subject (t(134)=2.52, p=0.013), and were not on schedule to graduate (t(131)=−3.13 p=0.002) had significantly lower median household income. No significant relationships were found between median household income and history of Committee on Special Education (CSE) evaluation, school refusal, summer school failing a citywide exam, or neuropsychiatric or education evaluation.
Adolescents repeating a grade or not on schedule to graduate from high school had significantly higher BMIs in comparison to those who had not repeated a grade and expected to graduate on time (repeating grade:t(136)=−2.63, p= 0.009; on schedule: t(132)=2.56, p= 0.012). When logistic regression was used to control for WASI IQ, repeating a grade and being on schedule to graduate were no longer significantly associated with BMI. Participants who did not experience problems with repeating a grade or failing a grade or were not required to attend summer school had higher WASI scores in comparison to adolescents who repeated a grade, failed a grade or attended summer school (repeating a grade: t(122)=2.45 p=0.016; failing a grade: t(121)=2.01, p= 0.046; attended summer school t(121)=2.63, p=0.010).
Discussion
The results of the current study indicate that, even among a sample of adolescents with severe obesity increased BMI was associated with lower WASI scores and poor school outcomes. A high frequency of self-reported school problems was observed among adolescents presenting to a bariatric surgery program, with nearly all of the sample reporting some school problems (e.g., greater than 50% of the sample had failed a grade during their academic career). Retrospectively evaluating the time course of problems in school and the development of overweight limits our ability to evaluate the chronology of these events. However, adolescents and parents reported the candidates were, on average, first overweight at an age that corresponds to kindergarten, suggesting that most of this sample had weight problems prior to experiencing school problems. The identification of school problems among bariatric candidates is consistent with previous research documenting problems in school functioning for students with obesity(3–8)and extends the extant literature by demonstrating that deficits in school functioning are also related to performance on a cognitive task.
Associations were observed between higher BMI and worse school performance and lower WASI scores. Consistent with a previous study by Phanand colleagues evaluating adolescent bariatric surgery candidates, the mean IQ is in the average range(9). Phanand colleagues failed to show a relationship between BMI and IQ, but examined this association in a much smaller sample(9). When the two WASI subtests administered in this study were examined independently, only the vocabulary subtest scores were significantly associated with BMI. Additionally, when correcting for WASI IQ, relationships between school variables and BMI were no longer significant. These findings suggest that in this clinical population, full scale IQ estimates and vocabulary subtest scores are predictive of academic performance, which is consistent with the predictive value of IQ in the general population(16). The causal relationships among BMI, school performance, and WASI IQ are unknown. It is possible that lower WASI scores may lead to increased BMI by affecting food and health choices. The converse may also be true, in that increased BMI may affect cognitive processes resulting in a lower WASI scores. In addition, these factors may play independent roles in school performance. Other researchers have similarly raised questions about directionality and posited that structural brain deficits may lead to disinhibited eating, or that brain structural deficits may result from injury related to obesity and its associated insulin resistance or that these effects may be bidirectional(17). Further research, including longitudinal studies, is necessary to learn more about these relationships.
Further, socioeconomic status (SES), as measured by median household income by zip code, was also associated with school problems for adolescents enrolled in a bariatric surgery program; however, a significant relationship was not observed between BMI and SES. Many studies show an inverse relationship between overweight/obesity and SES, such that SES accounts for differences between school performance of students with obesity and their normal weight peers(18). The current study suggests that it may be possible to consider lower SES and increased BMI, among this sample of adolescents with severe obesity, as independent risk factors for school dysfunction. Both lower SES and increased BMI likely confer increased psychosocial stress, but by different mechanisms. For example, in lower SES homes, it is more likely for adolescents to be in a single parent home, have parents with lower educational achievement and have increased levels of family conflict,(19) all of which may interfere with a student’s ability to meet academic demands. Therefore, these factors may be additive stressors related to BMI, such as health related problems, as well as cognitive and performance deficits potentially related to BMI. Furthermore, depressive symptoms as measured by the BDI were not correlated with school functioning or WASI, which suggests that, although some studies have shown increased rates of depression in adolescents with obesity(20,21)or associations between decreased school performance and depression(14), depression does not appear to account for the poor school functioning or lower WASI scores observed in this sample.
Increasing awareness of the deficits identified in this study is important for teachers, school counselors, and other mental health providers. Some studies have suggested that school performance of adolescents with overweight and obesity is significantly impacted by stigma that includes negative treatment by peers and teachers(22). Both impaired school performance and negative treatment likely contribute to school refusal and the choice for home schooling. Also, evidence suggests that students with obesity have more school absences(3)which may be related to stigma, the need to attend doctor’s appointments, which may be particularly relevant for bariatric surgery patients, or psychiatric symptoms, as in our sample adolescents reporting current or past participation in psychotherapy had a significantly greater likelihood of school refusal. Because this group has multiple additive risk factors for difficulty in school, there should be a low threshold for referral to school counselors to identify any problems with academic advancement, school attendance and need for further supports in classroom and at home. Additionally, schools should work to identify systems solutions to create a more educationally conducive environment for students with obesity including anti-bullying policies, classroom furniture to accommodate larger students and other modifiable factors.
There are several limitations in our study. First, all of the information about school performance was obtained during a clinical interview with potential surgical candidates and their parents. As these interviews were part of a required pre-operative evaluation to determine eligibility for surgery, it is possible that subjects (or their parents) may have distorted school performance positively or negatively in order to be viewed as appropriate surgical candidates. Collateral information from schools would have provided more objective data. In addition, the assessment of cognitive function was limited to the abbreviated WASI, which includes only verbal and performance subtests. The abbreviated WASI served as a clinical screening tool in the pre-surgical psychiatric evaluation because the vocabulary and matrix reasoning subtests can be administered quickly and provide a general summary of an individual’s cognitive functioning(11), but utilizing the full WASI would have provided a more comprehensive understanding of cognitive functioning in this sample Sensori-motor, attention, executive function or language deficits were not assessed with sensitive measures. Finally, this study did not include a control group, and it is therefore not possible to determine whether the problems with school functioning generalize to adolescents with severe obesity who are not pursuing weight loss surgery.
These data highlight the importance of future studies examining cognitive and academic deficits associated with obesity. For adults seeking bariatric surgery, some cognitive impairment may be reversible with weight loss, as patients showed improvements on memory indexes at a 12 weeks post-operative evaluation(23). In that study improvement in cognitive function was largely unrelated to presence or absence of obesity-related illnesses, suggesting similar or greater cognitive improvement may occur in a younger population that is less medically burdened(24).Additional studies to better characterize the relationship between school performance, intellectual functioning, and severe obesity in youth are needed. Critically, it is not clear whether school performance improves following successful bariatric surgery.
Acknowledgements
Dr. Freidl is supported by the National Institute of Mental Health Grant T32-MH015144 and received grant funding from American Academy of Child and Adolescent Psychiatry (AACAP) and Pilot Research Award for Junior Faculty and Child and Adolescent Psychiatry Residents, supported by Lilly, USA LLC. Dr. Sysko is supported by the National Institute of Diabetes and Digestive and Kidney Diseases Grant DK088532-01A1 and holds stock in Pfizer Pharmaceuticals. Dr. Walsh received research support from AstraZeneca.
Sumati Gupta, Ph.D.
Columbia University
Jennifer Bush, MSEd
Fordham University
Stephanie Brewer
Loyola University of Chicago
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009;9:322–329. doi: 10.1016/j.acap.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaidya V. Psychosocial aspects of obesity. Adv Psychosom Med. 2006;27:73–85. doi: 10.1159/000090965. [DOI] [PubMed] [Google Scholar]
- 3.Shore SM, Sachs ML, Lidicker JR, Brett SN, Wright AR, Libonati JR. Decreased scholastic achievement in overweight middle school students. Obesity. 2008;16:1535–1538. doi: 10.1038/oby.2008.254. [DOI] [PubMed] [Google Scholar]
- 4.Falkner NH, Neumark-Sztainer D, Story M, Jeffery RW, Beuhring T, Resnick MD. Social, educational, and psychological correlates of weight status in adolescents. Obes Res. 2001;9:32–42. doi: 10.1038/oby.2001.5. [DOI] [PubMed] [Google Scholar]
- 5.Tershakovec AM, Weller SC, Gallagher PR. Obesity, school performance and behaviour of black, urban elementary school children. Int J Obes Relat Metab Disord. 1994;18:323–327. [PubMed] [Google Scholar]
- 6.Geier AB, Foster GD, Womble LG, et al. The relationship between relative weight and school attendance among elementary schoolchildren. Obesity. 2007;15:2157–2161. doi: 10.1038/oby.2007.256. [DOI] [PubMed] [Google Scholar]
- 7.Li X. A study of intelligence and personality in children with simple obesity. Int J Obes Relat Metab Disord. 1995;19:355–357. [PubMed] [Google Scholar]
- 8.Lokken KL, Boeka AG, Austin HM, Gunstad J, Harmon CM. Evidence of executive dysfunction in extremely obese adolescents: a pilot study. Surg Obes Relat Dis. 2009;5:547–552. doi: 10.1016/j.soard.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Phan TL, Curran JL, Datto GA. Evaluation of intelligence in an adolescent bariatric population. Surg Obes Relat Dis. 2012 doi: 10.1016/j.soard.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 10.Sysko R, Zakarin EB, Devlin MJ, Bush J, Walsh BT. A latent class analysis of psychiatric symptoms among 125 adolescents in a bariatric surgery program. Int J Pediatr Obes. 2011;6:289–297. doi: 10.3109/17477166.2010.545411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wechsler, David . Wechsler abbreviated scale of intelligence. Psychological Corporation; 1999. [Google Scholar]
- 12.Colom R, Flores-Mendoza CE. Intelligence predicts scholastic achievement irrespective of SES factors: Evidence from Brazil. Intelligence. 2007;35:243–251. [Google Scholar]
- 13.Beck AT, Ward CH, Mendelson M, et al. Beck Depression Inventory. In: Rush Ja, Frist MB, Balcker D., editors. Handbook of Psychiatric Measure. second edition. Washington DC: American Psychiatric Publishing, Inc; 2008. pp. 504–506. [Google Scholar]
- 14.Frojd SA, Nissinen ES, Pelkonen MUI, Marttunen MJ, Koivisto AM, Kaltiala-Heino R. Depression and school performance in middle adolescent boys and girls. J Adolesc. 2008;31:485–498. doi: 10.1016/j.adolescence.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 15.Sysko R, Devlin MJ. Special issues in the assessment and treatment of adolescent bariatric surgery patients. In: Mitchell JE, de Zwaan M, editors. Psychological Assessment and treatment of Bariatric Surgery Patients. New York: Routledge Taylor & Francis Group; 2012. pp. 185–197. [Google Scholar]
- 16.Mayes SD, Calhoun SL, Bixler EO, Zimmerman DN. IQ and neuropsychological predictors of academic achievement. Learn Ind Differ. 2009;19:238–241. [Google Scholar]
- 17.Maayan L, Hoogendoorn C, Sweat V, Convit A. Disinhibited eating in obese adolescents is associated with orbitofrontal volume reductions and executive dysfunction. Obesity. 2011;19:1382–1387. doi: 10.1038/oby.2011.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Datar A, Sturm R, Magnabosco JL. Childhood overweight and academic performance: national study of kindergartners and first-graders. Obes Res. 2004;12:58–68. doi: 10.1038/oby.2004.9. [DOI] [PubMed] [Google Scholar]
- 19.Bradley RH, Corwyn RF. Socioeconomic status and child development. Annu Rev Psychol. 2002;53:371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- 20.Erermis S, Cetin N, Tamar M, Bukusoglu N, Akdeniz F, Goksen D. Is obesity a risk factor for psychopathology among adolescents? Pediatr Int. 2004;46:296–301. doi: 10.1111/j.1442-200x.2004.01882.x. [DOI] [PubMed] [Google Scholar]
- 21.Kim JR, Langer JM, Baker AW, Filter DE, Williams NN, Sarwer DB. Psychosocial Status in Adolescent Undergoing Bariatric Surgery. Obes Surg. 2008;18:27–33. doi: 10.1007/s11695-007-9285-x. [DOI] [PubMed] [Google Scholar]
- 22.Crosnoe R, Muller C. Body mass index, academic achievement, and school context: examining the educational experiences of adolescents at risk of obesity. J Health Soc Behav. 2004;45:393–407. doi: 10.1177/002214650404500403. [DOI] [PubMed] [Google Scholar]
- 23.Gunstad J, Strain G, Devlin MJ, et al. Improved memory function 12 weeks after bariatric surgery. Surg Obes Rel Dis. 2011;7:465–472. doi: 10.1016/j.soard.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zitsman JL, Digiorgi MF, Marr JR, Witt MA, Bessler M. Comparative outcomes of laparoscopic adjustable gastric banding in adolescents and adults. Surg Obes Rel Dis. 2011;7:720–726. doi: 10.1016/j.soard.2011.01.042. [DOI] [PubMed] [Google Scholar]


