Abstract
Objective
Weight loss programs are often conducted in a group format, but it is unclear whether weight losses or adherence cluster within treatment group and whether characteristics of the group (e.g. size or homogeneity) affect outcomes. We examined these questions within Look AHEAD, a multicenter study of the effects of an intensive lifestyle intervention (ILI) in overweight/obese individuals with type 2 diabetes.
Design and Methods
Weight losses and adherence (attendance, use of meal replacement products, and minutes of activity) were examined over one year of intervention in 2329 ILI participants in 209 treatment groups, which all received the same weight loss program.
Results
Weight losses did not cluster among members of a treatment group (intra-class correlation [ICC] of .007), whereas measures of adherence had small/moderate clustering (ICCs of .05–.11). The 209 groups varied in weight losses, with a mean of 8.64 % (SD=2.35 %, interquartile range=6.82%, 10.32%), but neither size nor baseline homogeneity of members affected the outcome.
Conclusions
Although these findings suggest that it may not be necessary to control for clustering in behavioral weight loss studies, they also indicate that merely treating individuals in groups is not sufficient to harness social influences on weight loss.
Keywords: behavioral weight loss, clustering of outcomes, treatment groups
Increasingly it is recognized that social factors play a role in the development of health problems and their resolution. For example, the incidence of obesity has been shown to occur in clusters, with the development of obesity in one person increasing the odds that obesity will develop in their close friends [1]. These social processes have been harnessed as a means to improve outcomes in several approaches to behavioral weight loss. For example, Wing and colleagues [2] recruited participants with several of their friends and/or family members and treated these participants as a team, with group activities utilized to stress intra-group cohesion and inter-group competition. This social intervention improved overall weight loss outcomes.
Moreover, as would be expected with a social intervention, the study by Wing and colleagues found that there was a clustering in the weight loss outcomes among the team members; weight losses of one member of the team were found to be strongly related to that of the other members [2]. Similarly, when patients’ friends or family members are included within the treatment program, the weight losses achieved by the patient and their social contacts are correlated with one another [3]. Such social contagion appears to extend even outside the program; the untreated spouses of patients in a behavioral weight loss program have been shown to achieve weight losses similar to the patients actually participating in the program [4]. Leahey and colleagues [5] recently reported that individual weight losses in a team-based weight loss program were influenced by the weight losses of others on the team, i.e. there was a clustering of outcomes; characteristics of the team at baseline influenced the results subsequently achieved[5].
It is less clear whether the characteristics of the other members of the group influence the weight losses achieved by the individual participants in standard group-based behavioral weight loss programs and whether these weight losses tend to cluster within the group. Typically, behavioral weight loss tested in research studies are conducted in a group format. Approximately 10–15 patients who do not know each other are treated together, with weekly meetings for 6 months, followed by less frequent meetings for extended periods of time [6]. These programs present a structured series of behavioral weight loss lessons and do not include emphasis on group cohesion or efforts to encourage group members to interact with each other outside of the group setting. Similarly, many other types of weight loss programs, such as Weight Watchers, Take Off Pounds Sensibly (TOPS), and lifestyle interventions to prevent diabetes that are offered through hospitals and YMCAs, utilize group approaches for the delivery of the program [7]. Weight losses achieved in group programs appear to surpass those seen with individual contact [8], and are clearly less costly to administer. However, to date there has been little research examining the group effects inherent in these programs.
A large number of studies have examined individual baseline characteristics that might predict treatment outcome (e.g., [9]) but few have examined whether the baseline characteristics of the group affect the outcome in behavioral weight loss studies. Studies of group performance suggest that characteristics such as the size of the group and the similarity of group members to each other might influence treatment outcomes [10, 11]. In the only study examining this within behavioral weight control interventions, Jeffery and colleagues [12] found no differences in the weight losses achieved by participants who were randomly assigned to groups that were homogeneous or heterogeneous with respect to gender and degree of overweight.
In addition, the extent to which performance (in terms of adherence or weight loss) clusters within groups has rarely been studied. Simon et al [13] analyzed the results of 13 different weight loss groups and observed that attendance during the 26 session program clustered within group (ICC=.14), but weight loss did not (ICC=.00). However, the relatively small number of weight loss groups and the fact that the mean weight losses in this trial were quite low (mean of 4.24 kg at12 months) may have limited the ability to see clustering.
Given that weight loss programs are often offered in group format, these issues have important clinical and methodological implications. Information about whether the size of the group or the characteristics of the group members, in terms of their diversity in age, gender, and BMI, affects the outcome could improve the results achieved in future programs. Evidence of significant clustering of outcomes within behavioral weight loss groups would have important methodological implications. Such clustering would need to be accounted for in estimating sample size and in data analysis [14]. Although clustering is often considered in sample size estimates for school-based and physician-based interventions, it is not typically considered in most clinical studies of weight loss interventions.
In this paper, we examine these questions using the Look AHEAD trial. Look AHEAD is a multicenter clinical trial comparing the effects of intensive lifestyle intervention (ILI) vs control on cardiovascular morbidity and mortality in over 5000 overweight/obese individuals with type 2 diabetes [15]. The fact that there were over 200 different ILI weight loss groups in this trial provides a unique opportunity to address two important questions: 1) Is there a clustering of outcomes within groups for adherence to treatment components and/or for the weight losses achieved?; 2) Do group characteristics (including size of the group and its composition) affect weight losses achieved? We focus primarily on weight losses at one year, because groups were meeting most frequently during this time.
Methods
Participants
As reported previously, to be included in Look AHEAD, participants had to have type 2 diabetes, be 45–76 years of age, have a BMI of >25 kg/m2 (>27 if taking insulin), with A1c <11%, systolic blood pressure <160 mmHg, diastolic blood pressure <100 mmHg, and triglycerides <600 mg/dl.[15] They were also required to complete a maximal fitness test. Look AHEAD recruited 5145 participants, with 59% females, and 37% from minority populations [16]. This analysis focused only on those individuals who were randomly assigned to the Intensive Lifestyle Intervention in the Look AHEAD trial.
Design/Procedures
Look AHEAD was conducted at 16 clinical sites within the United States. Participants were randomly assigned within clinical site to either the Intensive Lifestyle Intervention group (ILI) or to Diabetes Support and Education (DSE), the control group for this trial [15]. Participants in the ILI received a lifestyle intervention that has been described in detail [17]. This program was offered in a group format, with nutritionists, exercise physiologists, and behavioral psychologists serving as group leaders. Groups were formed according to participant availability. Our analyses focus primarily on clustering seen for outcomes achieved during the first year because the group contact was greatest during this time and participants typically remained in their assigned group throughout this period. During the first 6 months of the ILI program, participants attended one individual and 3 group meetings each month and during months 7–12 they attended one individual and two group meetings per month. Subsequently participants attended only one group meeting and had one individual contact per month. The goals of the intervention were to produce a mean weight loss of at least 7% of initial body weight (with participants each asked to try to lose 10% of their body weight) and to increase moderate intensity physical activity to 175 minutes per week. Participants were given a calorie and fat gram goal and were provided with liquid shakes and meal bars to help them adhere to this dietary regimen. The program focused on behavioral strategies, and emphasized self-monitoring, goal setting, and problem solving. Self-monitoring records were kept daily throughout the program and were reviewed each week by the lifestyle interventionists.
Measures
Demographic information was collected at baseline. Weight was assessed at baseline and annual assessments by clinic staff, who were masked to treatment assignment. Adherence metrics included attendance at treatment sessions (recorded by intervention staff), meal replacement use and minutes of moderate intensity physical activity (both obtained from participants’ weekly self-monitoring records).
Statistical Methods
Look AHEAD assigned 2570 participants to ILI at baseline. For inclusion in analyses, participants must have returned for their Year 1 weight to be measured: this eliminated 95 participants (3.7%). Those who gained more than 20% or lost more than 30% were dropped from the analyses to reduce the effect of atypical cases: this eliminated 15 more participants. Finally, we restricted analyses to intervention groups with at least 6 participants to provide reasonably stable group means and variances for group characteristics and excluded clinical sites that conducted fewer than 6 groups, which excluded 131 additional participants, for a final database of 2329 (90.6%) of the enrolled ILI participants. General linear models, with intervention groups as random effects nested within clinical sites, were used to estimate intraclass correlations (ICCs) with varying levels of covariate adjustment. The ICC is the ratio of the between group variance compared to the sum of the between and within group variance. These were estimated using Proc Mixed in SAS (SAS Institute. SAS/STAT, V.9.3., 2008) using a random effects model, i.e. group was considered to be a random effect. Given that our goal was descriptive, no significance tests were conducted. Linear models and correlation coefficients were used to describe associations between group characteristics (including baseline BMI, gender, insulin use and age) and group weight change. Since race/ethnicity tended to cluster within clinic site, it was not included as a separate variable among the group characteristics we considered.
Results
Analyses included data from 2329 participants, who were members of 209 intervention groups, across 15 clinics. Table 1 provides information on characteristics of the 209 groups. Group size averaged 11 members (range 6–21) and 58.9% of the group members were female (range 11.1–100%). The average group had 36.7% percent of its members with BMI of <30 kg/m2, 33.2% with BMI of 30 to 34 kg/m2, 18.4% with BMI of 35 to 39, and 11.7% with BMI of 40 kg/m2 or more. The average (standard deviation; interquartile range) percent loss of body weight across the 209 groups was 8.64% (2.35; 6.82 to 10.32%). Very similar results were seen using weight loss in kilograms: mean weight loss of 8.78 kg (2.48; 7.10 to 10.63 kg).
Table 1.
Characteristics of the 209 Look AHEAD intervention groups included in analyses at enrollment.
| Characteristic of Group | Mean [Range] |
|---|---|
| Group Size | 11.1 [6, 21] |
| Mean age, year | 58.8 [50.7, 67.1] |
| Percent female | 58.9 [11.1, 100.0] |
| Percent > HS education | 80.3 [0.0 100.0] |
| Percent race/ethnic groups | |
| African-American | 16.6 [0.0, 90.9] |
| Hispanic | 14.7 [0.0, 100.0] |
| Non-Hispanic white | 64.8 [0.0, 100.0] |
| Other/Multiple | 3.8 [0.0, 30.0] |
| Percent insulin use | 17.9 [0.0, 62.5] |
| Percent hypertensive | 84.6 [25.0, 100.0] |
| Percent prior CVD | 14.7 [0.0, 50.0] |
| Mean HbA1c (%) | 7.24 [6.17, 8.42] |
| BMI distribution | |
| % <30 kg/m2 | 36.7 [0.0, 85.7] |
| % 30–34 kg/m2 | 33.2 [0.0, 82.4] |
| % 35–39 kg/m2 | 18.4 [0.0, 66.7] |
| % ≥ 40 kg/m2 | 11.7 [0.0, 50.0] |
Clustering of weight loss outcomes and adherence within groups. Controlling for any systematic differences among clinics (i.e. including a marker for site as a covariate) with treatment groups nested within clinics, the overall ICC for change in percent body weight at one year was 0.008. As a comparison, the ICC for age and baseline BMI were 0.192 and 0.026, respectively. With additional adjustment for four baseline factors known to influence weight loss (gender, initial BMI, age, and insulin use), the overall ICC was 0.007 (Table 2). Table 2 also provides the adjusted ICCs for each clinic site. These were uniformly small, except for one site (“F”), for which the unadjusted and adjusted ICCs were 0.083 and 0.121, respectively. We also examined the ICC by year of enrollment in the trial, and found no consistent difference over time. The ICC for percent weight change at Year 4 was 0.000.
Table 2.
Estimated intra-class correlations for percentage change in weight and adherence to lifestyle intervention at one year.
| Intra-Class Correlation Among Intervention Groups1 |
|||||
|---|---|---|---|---|---|
| Clinic (N) | Number of ILI Groups |
% Weight Loss |
Session Attendance |
Use of Meal Replacements |
Minutes of Physical Activity |
| A (153) | 14 | 0.002 | 0.267 | 0.167 | 0.167 |
| B (165) | 13 | 0.034 | 0.133 | 0.081 | 0.011 |
| C (151) | 14 | 0.026 | 0.230 | 0.125 | 0.009 |
| D (143) | 14 | 0.000 | 0.150 | 0.096 | 0.000 |
| E (166) | 13 | 0.000 | 0.399 | 0.056 | 0.032 |
| F (157) | 14 | 0.121 | 0.000 | 0.061 | 0.149 |
| G (147) | 14 | 0.046 | 0.132 | 0.000 | 0.112 |
| H (150) | 14 | 0.000 | 0.146 | 0.109 | 0.021 |
| I (151) | 12 | 0.020 | 0.010 | 0.117 | 0.010 |
| J (138) | 13 | 0.016 | 0.079 | 0.121 | 0.017 |
| K (152) | 17 | 0.011 | 0.209 | 0.314 | 0.168 |
| L (166) | 12 | 0.000 | 0.028 | 0.079 | 0.000 |
| M (158) | 12 | 0.000 | 0.017 | 0.081 | 0.054 |
| N (160) | 17 | 0.000 | 0.000 | 0.056 | 0.057 |
| O (167) | 16 | 0.016 | 0.000 | 0.134 | 0.048 |
| Total (2342) | 209 | 0.007 | 0.118 | 0.116 | 0.054 |
Intraclass correlation coefficient for intervention group after adjusting for clinical site, gender, baseline insulin use, age group, and baseline BMI
Three process measures were used to monitor intervention adherence: attendance at treatment sessions, use of meal replacements, and self-reported minutes of physical activity. The overall means (standard deviations) for these measures over the first year of intervention were 35.2 (7.7) visits, 7.3 (4.1) meal replacements per week, and 143 (109) minutes of exercise per week. Each of these adherence measures was significantly correlated with one year weight loss (r=0.38, r=0.34, and r=0.41, respectively, all p<0.001). However, as seen in Table 2, these adherence measures, adjusted for clinic and baseline characteristics, each had much stronger within group ICCs than weight loss, and were substantial (e.g. >0.10) for several clinic sites.
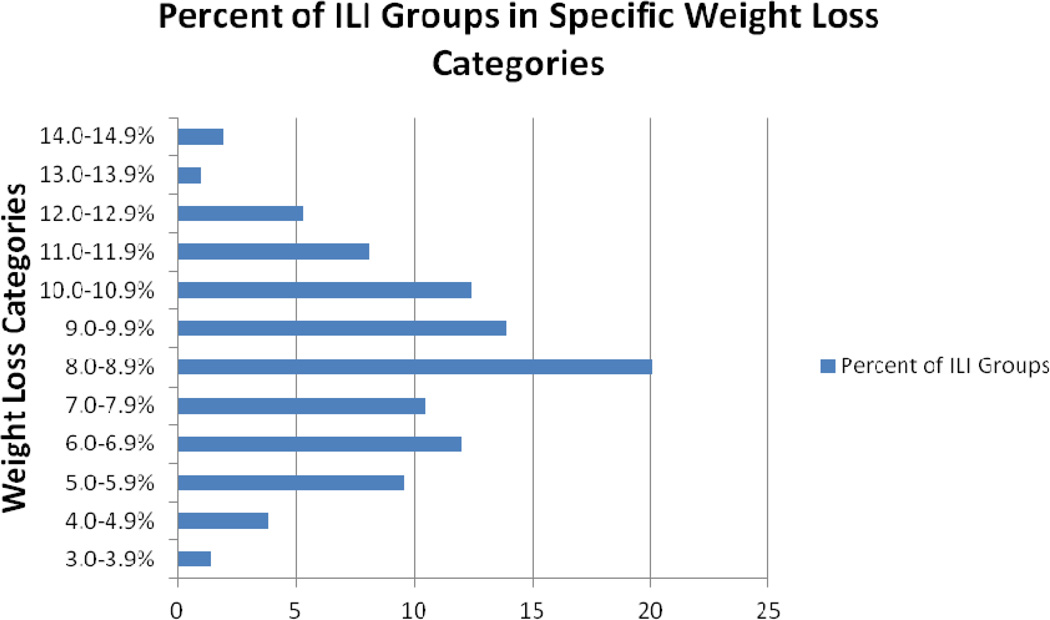
Between group effects for weight loss. As shown in Figure 1, there was a fair amount of variability in the outcomes that were achieved across the 209 groups. While 46.4% of the groups had average weight losses between 8 and 11%, 14.8% had a weight loss of <6%, and 8% had weight losses of >12%.
Figure 1.
Percent of ILI groups in specific weight loss categories
We examined whether the average weight losses across the 209 intervention groups were associated with baseline group characteristics. In analyses controlling for differences among clinic sites, group size was not associated with mean weight loss (r= −0.04, p=0.57). However, the percentage of women in the group (r=−0.16; p=0.02); the average age of the group (r=0.18; 0=0.01); and the average baseline BMI (r=−0.49; p<0.001) were all associated with the group’s average weight loss. Adjusting for clinic reduced the standard deviation among the intervention groups from 2.35% to 2.09% and further adjustment for covariates (age, sex, insulin use and BMI) reduced it to 1.83%. Thus less than 25% of the variance among intervention between groups was explained by these variables.
We also examined the relationship of weight loss with measures of group heterogeneity. For this, we looked at the gender distribution (absolute difference from 50% female) and the intra-group standard deviation of age and initial BMI. These measures had mean (interquartile range) of 15.9 (0.0, 22.7), 5.8 years (4.6, 7.0), and 5.5 kg/m2 (4.4, 6.7), respectively. Variability in age and gender were not related to the groups’ weight loss outcomes. Group mean weight losses tended to be lower among groups with greater heterogeneity in baseline BMI (r= −0.21, p=0.003), but this effect was removed after controlling for the group mean BMI (partial r = −0.08, p=0.27).
Discussion
Behavioral weight loss programs are typically offered in group formats [6]. Although these groups meet together over extended periods of time, the present data suggest that there is very little clustering of weight loss outcomes within standard behavioral weight loss groups. Thus, the outcome of the other group members appears to have little or no influence on the weight loss success of any one member. This finding, which replicates results reported by Simon and colleagues [13] across 13 therapy groups, has important methodological implications, as it suggests that weight loss studies need not account for clustering of outcomes in the power analyses or statistical approaches to the data analysis.
These findings also suggest that weight loss programs that seek to use social influence processes to improve outcome will need to provide more focused strategies, such as developing within-group activities or between group competitions, to accomplish this goal or alternatively, use existing relationships such as between friends or family members [3]. A recent study of weight loss in a team-based community intervention showed that individuals who reported greater social influence from their team achieved better weight losses[5]. Such social influence might be enhanced through group activities to develop shared norms or by increased social modeling of weight-related behaviors. In addition, individuals who are less successful at a task have been shown to perform better when doing a task with others, especially an interdependent task where every member of the group must succeed in order for the group to succeed [18]. This effect, referred to as the Kohler effect [19], has been shown to motivate higher levels of physical activity [20–22] and likely plays a role in the success of group-based contingencies in behavioral weight loss programs. Incorporating social influence strategies such as these may help improve weight loss outcomes. In contrast to the weight loss outcomes, adherence measures were more clustered within treatment group. Attendance, use of meal replacement products and minutes of physical activity all showed greater clustering within treatment group than did weight loss. Clustering of adherence outcomes may be stronger than clustering of weight loss due to the fact that weight loss is under more physiological control than behavioral outcomes. Alternatively, clustering may be seen more in self-report measures than in objective measures, because participants may bias the information they report to make them more similar to others in the group. Clustering of behavioral measures may also reflect group norms for adherence, social modeling of adherence behaviors, and/or diffusion of weight loss information among group members. For example, when some members of the group fail to attend treatment meetings, it may provide information, norms, and modeling of behavior, which then allows others to behave similarly, whereas success at weight loss remains more private.Another important finding is the heterogeneity in the outcomes seen across treatment groups, even after adjusting for participant characteristics expected to influence weight loss (such as gender and age). The mean weight loss across the 209 groups was 8.6%, exceeding the minimum study goal of 7%. Although participants in all groups were given the same weight and activity goals, and all groups had the same schedule and content of treatment lessons, there was a fair amount of variability in the outcomes achieved. This variability is of concern for smaller treatment development studies where the outcome observed in a limited number of groups is used to make decisions about the clinical efficacy of new treatment strategies. Some of this variability reflected the composition of the group and the same individual level variables (e.g. gender and age) that have been shown to influence initial weight loss [19]. However, much of the variability between groups was unaccounted for and may be largely a random phenomenon, consistent with the low intra-class correlations. Previous studies have documented marked variability among participants in the weight losses achieved [23], but this is the first study to show that group averages are also variable.
This study also suggests that the composition of the group has little effect on the outcomes achieved. Studies of group performance suggest that the homogeneity of the group, i.e. similarity among members of a group, may lead to greater cohesion and better outcomes [24, 25]. However, we found no evidence that the characteristics of the weight loss group, in terms of heterogeneity in age, weight, or gender distribution, affected the outcome, perhaps due to the restricted eligibility ranges used in this trial. Leahey likewise reported that group homogeneity did not affect weight loss outcomes[5]. Of particular interest was the finding that the size of the group did not affect the mean weight losses achieved; thus participants in smaller groups, who might be expected to receive more individual attention, did not achieve large weight losses. This is an interesting finding for clinicians who might want to consider the cost:effectiveness of delivering behavioral weight loss programs to groups of approximately 15–20 members.
There are several limitations of this study that need to be considered in interpreting the results. First, all Look AHEAD participants had diabetes, were between ages 45 and 76, and were willing to participate in a randomized clinical trial; these factors limited the heterogeneity of the sample and the generalizeability of the findings. In addition, efforts were made to maintain consistency of the intervention across sites and to maximize adherence in all participants; these efforts may have limited the effect of within-group variables. The treatment protocol involved both group and individual meetings, and the individual sessions, which are unusual to include in group-based programs, may have weakened the clustering of outcomes.
In summary, there appears to be little evidence that weight losses cluster among the members of a behavioral weight loss group, although somewhat greater effects were seen for adherence. Moreover, characteristics of the group in terms of size and homogeneity of the members have little effect on outcomes. Although treating participants in groups is clearly cost-effective, efforts to maximize the social aspects of group behavioral weight loss programs to improve treatment outcomes may be most successful if they utilize pre-existing relationships or extend beyond merely treating participants together in the same group and incorporate innovative strategies to affect group norms, group cohesion, and social influence processes.
What is known
Behavioral weight loss programs are typically conducted in small groups of about 15 participants.
In behavioral weight loss programs utilizing social interventions (e.g. team-based competitions), the weight loss of the team members are related to each other.
It is unclear whether there is a clustering of outcomes in standard behavioral weight loss programs and whether the characteristics of the group in terms of size or homogeneity affects the weight losses achieved. If clustering leads to moderate levels of intra-class correlation, the statistical power available for comparing interventions may be lowered.
What does this study add
This study found that weight losses do not cluster within behavioral weight loss groups, i.e. the weight loss of one member of the group is independent of the other members. Thus statistical power will likely not be lowered.
Neither group size nor group homogeneity affected the weight losses achieved by the group.
ACKNOWLEDGEMENTS
This report is based primarily on data collected during year 1 of the Look AHEAD study. All investigators and staff involved in the baseline and 1-year results of Look AHEAD are listed below.
Appendix
Clinical Sites
The Johns Hopkins Medical Institutions Frederick L. Brancati, MD, MHS1; Jeff Honas, MS2; Lawrence Cheskin, MD3; Jeanne M. Clark, MD, MPH3; Kerry Stewart, EdD3; Richard Rubin, PhD3; Jeanne Charleston, RN; Kathy Horak, RD
Pennington Biomedical Research Center George A. Bray, MD1; Kristi Rau2; Allison Strate, RN2; Brandi Armand, LPN2; Frank L. Greenway, MD3; Donna H. Ryan, MD3; Donald Williamson, PhD3; Amy Bachand; Michelle Begnaud; Betsy Berhard; Elizabeth Caderette; Barbara Cerniauskas; David Creel; Diane Crow; Helen Guay; Nancy Kora; Kelly LaFleur; Kim Landry; Missy Lingle; Jennifer Perault; Mandy Shipp, RD; Marisa Smith; Elizabeth Tucker
The University of Alabama at Birmingham Cora E. Lewis, MD, MSPH1; Sheikilya Thomas MPH2; Monika Safford, MD3; Vicki DiLillo, PhD; Charlotte Bragg, MS, RD, LD; Amy Dobelstein; Stacey Gilbert, MPH; Stephen Glasser, MD; Sara Hannum, MA; Anne Hubbell, MS; Jennifer Jones, MA; DeLavallade Lee; Ruth Luketic, MA, MBA, MPH; Karen Marshall; L. Christie Oden; Janet Raines, MS; Cathy Roche, RN, BSN; Janet Truman; Nita Webb, MA; Audrey Wrenn, MAEd
Harvard Center
Massachusetts General Hospital: David M. Nathan, MD1; Heather Turgeon, RN, BS, CDE2; Kristina Schumann, BA2; Enrico Cagliero, MD3; Linda Delahanty, MS, RD3; Kathryn Hayward, MD3; Ellen Anderson, MS, RD3; Laurie Bissett, MS, RD; Richard Ginsburg, PhD; Valerie Goldman, MS, RD; Virginia Harlan, MSW; Charles McKitrick, RN, BSN, CDE; Alan McNamara, BS; Theresa Michel, DPT, DSc CCS; Alexi Poulos, BA; Barbara Steiner, EdM; Joclyn Tosch, BA
Joslin Diabetes Center: Edward S. Horton, MD1; Sharon D. Jackson, MS, RD, CDE2; Osama Hamdy, MD, PhD3; A. Enrique Caballero, MD3; Sarah Bain, BS; Elizabeth Bovaird, BSN, RN; Ann Goebel-Fabbri, PhD; Lori Lambert, MS, RD; Sarah Ledbury, MEd, RD; Maureen Malloy, BS; Kerry Ovalle, MS, RCEP, CDE
Beth Israel Deaconess Medical Center: George Blackburn, MD, PhD1; Christos Mantzoros, MD, DSc3; Kristinia Day, RD; Ann McNamara, RN
University of Colorado Health Sciences Center James O. Hill, PhD1; Marsha Miller, MS, RD2; JoAnn Phillipp, MS2; Robert Schwartz, MD3; Brent Van Dorsten, PhD3; Judith Regensteiner, PhD3; Salma Benchekroun MS; Ligia Coelho, BS; Paulette Cohrs, RN, BSN; Elizabeth Daeninck, MS, RD; Amy Fields, MPH; Susan Green; April Hamilton, BS, CCRC; Jere Hamilton, BA; Eugene Leshchinskiy; Michael McDermott, MD; Lindsey Munkwitz, BS; Loretta Rome, TRS; Kristin Wallace, MPH; Terra Worley, BA
Baylor College of Medicine John P. Foreyt, PhD1; Rebecca S. Reeves, DrPH, RD2; Henry Pownall, PhD3; Ashok Balasubramanyam, MBBS3; Peter Jones, MD3; Michele Burrington, RD; Chu-Huang Chen, MD, PhD3; Allyson Clark, RD; Molly Gee, MEd, RD; Sharon Griggs; Michelle Hamilton; Veronica Holley; Jayne Joseph, RD; Patricia Pace, RD: Julieta Palencia, RN; Olga Satterwhite, RD; Jennifer Schmidt; Devin Volding, LMSW; Carolyn White
University of California at Los Angeles School of Medicine Mohammed F. Saad, MD1; Siran Ghazarian Sengardi, MD2; Ken C. Chiu, MD3; Medhat Botrous; Michelle Chan, BS; Kati Konersman, MA, RD, CDE; Magpuri Perpetua, RD
The University of Tennessee Health Science Center
University of Tennessee East. Karen C. Johnson, MD, MPH1; Carolyn Gresham, RN2; Stephanie Connelly, MD, MPH3; Amy Brewer, RD, MS; Mace Coday, PhD; Lisa Jones, RN; Lynne Lichtermann, RN, BSN; Shirley Vosburg, RD, MPH; and J. Lee Taylor, MEd, MBA
University of Tennessee Downtown. Abbas E. Kitabchi, PhD, MD1; Helen Lambeth, RN, BSN2; Debra Clark, LPN; Andrea Crisler, MT; Gracie Cunningham; Donna Green, RN; Debra Force, MS, RD, LDN; Robert Kores, PhD; Renate Rosenthal PhD; Elizabeth Smith, MS, RD, LDN; and Maria Sun, MS, RD, LDN; and Judith Soberman, MD3
University of Minnesota Robert W. Jeffery, PhD1; Carolyn Thorson, CCRP2; John P. Bantle, MD3; J. Bruce Redmon, MD3; Richard S. Crow, MD3; Scott Crow, MD3; Susan K Raatz, PhD, RD3; Kerrin Brelje, MPH, RD; Carolyne Campbell; Jeanne Carls, MEd; Tara Carmean-Mihm, BA; Emily Finch, MA; Anna Fox, MA; Elizabeth Hoelscher, MPH, RD, CHES; La Donna James; Vicki A. Maddy, BS, RD; Therese Ockenden, RN; Birgitta I. Rice, MS, RPh CHES; Tricia Skarphol, BS; Ann D. Tucker, BA; Mary Susan Voeller, BA; Cara Walcheck, BS, RD
St. Luke’s Roosevelt Hospital Center Xavier Pi-Sunyer, MD1; Jennifer Patricio, MS2; Stanley Heshka, PhD3; Carmen Pal, MD3; Lynn Allen, MD; Diane Hirsch, RNC, MS, CDE; Mary Anne Holowaty, MS, CN
University of Pennsylvania Thomas A. Wadden, PhD1; Barbara J. Maschak-Carey, MSN, CDE2; Stanley Schwartz, MD3; Gary D. Foster, PhD3; Robert I. Berkowitz, MD3; Henry Glick, PhD3; Shiriki K. Kumanyika, PhD, RD, MPH3; Johanna Brock; Helen Chomentowski; Vicki Clark; Canice Crerand, PhD; Renee Davenport; Andrea Diamond, MS, RD; Anthony Fabricatore, PhD; Louise Hesson, MSN; Stephanie Krauthamer-Ewing, MPH; Robert Kuehnel, PhD; Patricia Lipschutz, MSN; Monica Mullen, MS, RD; Leslie Womble, PhD, MS; Nayyar Iqbal, MD
University of Pittsburgh David E. Kelley, MD1; Jacqueline Wesche-Thobaben, RN, BSN, CDE2; Lewis Kuller, MD, DrPH3; Andrea Kriska, PhD3; Janet Bonk, RN, MPH; Rebecca Danchenko, BS; Daniel Edmundowicz, MD3; Mary L. Klem, PhD, MLIS3; Monica E. Yamamoto, DrPH, RD, FADA 3; Barb Elnyczky, MA; George A. Grove, MS; Pat Harper, MS, RD, LDN; Janet Krulia, RN, BSN, CDE; Juliet Mancino, MS, RD, CDE, LDN; Anne Mathews, MS, RD, LDN; Tracey Y. Murray, BS; Joan R. Ritchea; Jennifer Rush, MPH; Karen Vujevich, RN-BC, MSN, CRNP; Donna Wolf, MS
The Miriam Hospital/Brown Medical School Rena R. Wing, PhD1; Renee Bright, MS2; Vincent Pera, MD3; John Jakicic, PhD3; Deborah Tate, PhD3; Amy Gorin, PhD3; Kara Gallagher, PhD3; Amy Bach, PhD; Barbara Bancroft, RN, MS; Anna Bertorelli, MBA, RD; Richard Carey, BS; Tatum Charron, BS; Heather Chenot, MS; Kimberley Chula-Maguire, MS; Pamela Coward, MS, RD; Lisa Cronkite, BS; Julie Currin, MD; Maureen Daly, RN; Caitlin Egan, MS; Erica Ferguson, BS, RD; Linda Foss, MPH; Jennifer Gauvin, BS; Don Kieffer, PhD; Lauren Lessard, BS; Deborah Maier, MS; JP Massaro, BS; Tammy Monk, MS; Rob Nicholson, PhD; Erin Patterson, BS; Suzanne Phelan, PhD; Hollie Raynor, PhD, RD; Douglas Raynor, PhD; Natalie Robinson, MS, RD; Deborah Robles; Jane Tavares, BS
The University of Texas Health Science Center at San Antonio Steven M. Haffner, MD 1; Maria G. Montez, RN, MSHP, CDE 2; Carlos Lorenzo, MD 3
University of Washington / VA Puget Sound Health Care System Steven Kahn MB, ChB1; Brenda Montgomery, RN, MS, CDE2; Robert Knopp, MD3; Edward Lipkin, MD3; Matthew L. Maciejewski, PhD3; Dace Trence, MD3; Terry Barrett, BS; Joli Bartell, BA; Diane Greenberg, PhD; Anne Murillo, BS; Betty Ann Richmond, MEd; April Thomas, MPH, RD
Southwestern American Indian Center, Phoenix, Arizona and Shiprock, New Mexico William C. Knowler, MD, DrPH1; Paula Bolin, RN, MC2; Tina Killean, BS2; Cathy Manus, LPN3; Jonathan Krakoff, MD3; Jeffrey M. Curtis, MD, MPH3; Justin Glass, MD3; Sara Michaels, MD3; Peter H. Bennett, MB, FRCP3; Tina Morgan3; Shandiin Begay, MPH; Bernadita Fallis RN, RHIT, CCS; Jeanette Hermes, MS,RD; Diane F. Hollowbreast; Ruby Johnson; Maria Meacham, BSN, RN, CDE; Julie Nelson, RD; Carol Percy, RN; Patricia Poorthunder; Sandra Sangster; Nancy Scurlock, MSN, ANP-C, CDE; Leigh A. Shovestull, RD, CDE; Janelia Smiley; Katie Toledo, MS, LPC; Christina Tomchee, BA; Darryl Tonemah PhD
University of Southern California Anne Peters, MD1; Valerie Ruelas, MSW, LCSW2; Siran Ghazarian Sengardi, MD2; Kathryn Graves, MPH, RD, CDE; Kati Konersman, MA, RD, CDE; Sara Serafin-Dokhan
Coordinating Center Wake Forest University Mark A. Espeland, PhD1; Judy L. Bahnson, BA2; Lynne Wagenknecht, DrPH3; David Reboussin, PhD3; W. Jack Rejeski, PhD3; Alain Bertoni, MD, MPH3; Wei Lang, PhD3; Gary Miller, PhD3; David Lefkowitz, MD3; Patrick S. Reynolds, MD3; Paul Ribisl, PhD3; Mara Vitolins, DrPH3; Michael Booth, MBA2; Kathy M. Dotson, BA2; Amelia Hodges, BS2; Carrie C. Williams, MA2; Jerry M. Barnes, MA; Patricia A. Feeney, MS; Jason Griffin, BS; Lea Harvin, BS; William Herman, MD, MPH; Patricia Hogan, MS; Sarah Jaramillo, MS; Mark King, BS; Kathy Lane, BS; Rebecca Neiberg, MS; Andrea Ruggiero, MS; Christian Speas, BS; Michael P. Walkup, MS; Karen Wall, AAS; Michelle Ward; Delia S. West, PhD; Terri Windham
Central Resources Centers
DXA Reading Center, University of California at San Francisco Michael Nevitt, PhD1; Susan Ewing, MS; Cynthia Hayashi; Jason Maeda, MPH; Lisa Palermo, MS, MA; Michaela Rahorst; Ann Schwartz, PhD; John Shepherd, PhD
Central Laboratory, Northwest Lipid Research Laboratories Santica M. Marcovina, PhD, ScD1; Greg Strylewicz, MS
ECG Reading Center, EPICARE, Wake Forest University School of Medicine RonaldJ. Prineas, MD, PhD1; Teresa Alexander; Lisa Billings; Charles Campbell, AAS, BS; Sharon Hall; Susan Hensley; Yabing Li, MD; Zhu-Ming Zhang, MD
Diet Assessment Center, University of South Carolina, Arnold School of Public Health, Center for Research in Nutrition and Health Disparities Elizabeth J Mayer-Davis, PhD1; Robert Moran, PhD
Hall-Foushee Communications, Inc.
Richard Foushee, PhD; Nancy J. Hall, MA
Federal Sponsors
National Institute of Diabetes and Digestive and Kidney Diseases: Barbara Harrison, MS; Van S. Hubbard, MD PhD; Susan Z.Yanovski, MD
National Heart, Lung, and Blood Institute: Lawton S. Cooper, MD, MPH; Jeffrey Cutler, MD, MPH; Eva Obarzanek, PhD, MPH, RD
Centers for Disease Control and Prevention: Edward W. Gregg, PhD; David F. Williamson, PhD; Ping Zhang, PhD
Funding and Support
This study is supported by the Department of Health and Human Services through the following cooperative agreements from the National Institutes of Health: DK57136, DK57149, DK56990, DK57177, DK57171, DK57151, DK57182, DK57131, DK57002, DK57078, DK57154, DK57178, DK57219, DK57008, DK57135, and DK56992. The following federal agencies have contributed support: National Institute of Diabetes and Digestive and Kidney Diseases; National Heart, Lung, and Blood Institute; National Institute of Nursing Research; National Center on Minority Health and Health Disparities; NIH Office of Research on Women’s Health; and the Centers for Disease Control and Prevention. This research was supported in part by the Intramural Research Program of the National Institute of Diabetes and Digestive and Kidney Diseases. The Indian Health Service (I.H.S.) provided personnel, medical oversight, and use of facilities. The opinions expressed in this paper are those of the authors and do not necessarily reflect the views of the I.H.S. or other funding sources.
Additional support was received from The Johns Hopkins Medical Institutions Bayview General Clinical Research Center (M01RR02719); the Massachusetts General Hospital Mallinckrodt General Clinical Research Center (M01RR01066); the University of Colorado Health Sciences Center General Clinical Research Center (M01RR00051) and Clinical Nutrition Research Unit (P30 DK48520); the University of Tennessee at Memphis General Clinical Research Center (M01RR0021140); the University of Pittsburgh General Clinical Research Center (M01RR000056 44) and NIH grant (DK 046204); the VA Puget Sound Health Care System Medical Research Service, Department of Veterans Affairs; and the Frederic C. Bartter General Clinical Research Center (M01RR01346).
The following organizations have committed to make major contributions to Look AHEAD: Federal Express; Health Management Resources; Johnson & Johnson, LifeScan Inc.; Optifast-Novartis Nutrition; Roche Pharmaceuticals; Ross Product Division of Abbott Laboratories; Slim-Fast Foods Company; and Unilever.
1 Principal Investigator
2 Program Coordinator
3 Co-Investigator
All other Look AHEAD staffs are listed alphabetically by site.
Footnotes
Competing interests:
The authors have no competing interests
Contributor Information
Rena R. Wing, Email: rwing@lifespan.org.
Tricia Leahey, Email: tleahey@lifespan.org.
Robert Jeffery, Email: jefferw@gmail.com.
Karen C. Johnson, Email: kjohnson@uthsc.edu.
James O. Hill, Email: james.hill@ucdenver.edu.
Mace Coday, Email: mcoday@uthsc.edu.
Mark A. Espeland, Email: mespelan@wakehealth.edu.
References
- 1.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 2.Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol. 1999;67(1):132–138. doi: 10.1037//0022-006x.67.1.132. [DOI] [PubMed] [Google Scholar]
- 3.Gorin A, et al. Involving support partners in obesity treatment. J Consult Clin Psychol. 2005;73(2):341–343. doi: 10.1037/0022-006X.73.2.341. [DOI] [PubMed] [Google Scholar]
- 4.Gorin AA, et al. Weight loss treatment influences untreated spouses and the home environment: evidence of a ripple effect. Int J Obes (Lond) 2008;32(11):1678–1684. doi: 10.1038/ijo.2008.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leahey TM, et al. Temmates and social influence affect weight loss outcomes in a team-based weight loss competition. Obesity. 2012;20:1413–1418. doi: 10.1038/oby.2012.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wing RR. Behavioral approaches to the treatment of obesity. In: Bray GA, Bouchard C, editors. Handbook of obesity treatment. New York: Marcel Dekker; 2008. pp. 227–248. [Google Scholar]
- 7.Heshka S, et al. Weight loss with self-help compared with a structured commercial program: a randomized trial. Jama. 2003;289(14):1792–1798. doi: 10.1001/jama.289.14.1792. [DOI] [PubMed] [Google Scholar]
- 8.Renjilian DA, et al. Individual versus group therapy for obesity: effects of matching participants to their treatment preferences. J Consult Clin Psychol. 2001;69(4):717–721. [PubMed] [Google Scholar]
- 9.Fabricatore AN, et al. Predictors of attrition and weight loss success: Results from a randomized controlled trial. Behav Res Ther. 2009;47(8):685–691. doi: 10.1016/j.brat.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levine J, Moreland R. Small groups. In: Gilbert D, Fiske S, Lindzey G, editors. The Handbook of Social Psychology. New York, NY: Oxford University Press; 1998. pp. 415–469. [Google Scholar]
- 11.O'Dell JW. Group size and emotional interaction. J Pers Soc Psychol. 1968;8(1):75–78. doi: 10.1037/h0025326. [DOI] [PubMed] [Google Scholar]
- 12.Jeffery RW, Snell MK, Forster JL. Group composition in the treatment of obesity: does increasing group homogeneity improve treatment results? Behav Res Ther. 1985;23(3):371–373. doi: 10.1016/0005-7967(85)90016-6. [DOI] [PubMed] [Google Scholar]
- 13.Simon GE, et al. Is Success in Weight Loss Treatment Contagious (Do Attendance and Outcomes Cluster within Treatment Groups)? Obes Res Clin Pract. 4(4):283–291. doi: 10.1016/j.orcp.2010.09.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murray D. Design and analysis of group-randomized trials. New York: Oxford University Press; 1998. [Google Scholar]
- 15.Ryan DH, et al. Look AHEAD (Action for Health in Diabetes): design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Control Clin Trials. 2003;24(5):610–628. doi: 10.1016/s0197-2456(03)00064-3. [DOI] [PubMed] [Google Scholar]
- 16.Bray G, et al. Baseline characteristics of the randomised cohort from the Look AHEAD (Action for Health in Diabetes) study. Diab Vasc Dis Res. 2006;3(3):202–215. doi: 10.3132/dvdr.2006.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wadden TA, et al. The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring) 2006;14(5):737–752. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hertel G, Kerr NL, Messe LA. Motivation gains in performance groups: paradigmatic and theoretical developments on the Kohler effect. J Pers Soc Psychol. 2000;79(4):580–601. [PubMed] [Google Scholar]
- 19.Köhler O. Über den Gruppenwirkungsgrad der menschlichen Körperarbeit und die Bedingung optimaler Kollektivkraftreaktion [Human physical performance in groups and conditions for optimal collective performance] Industrielle Psychotechnik. 1927;4:209+–226. [Google Scholar]
- 20.Feltz DL, Kerr NL, Irwin BC. Buddy up: the Kohler effect applied to health games. J Sport Exerc Psychol. 33(4):506–526. doi: 10.1123/jsep.33.4.506. [DOI] [PubMed] [Google Scholar]
- 21.Irwin BC, et al. Aerobic exercise is promoted when individual performance affects the group: a test of the Kohler motivation gain effect. Ann Behav Med. 44(2):151–159. doi: 10.1007/s12160-012-9367-4. [DOI] [PubMed] [Google Scholar]
- 22.Osborn KA, et al. The Köhler effect: Motivation gains and losses in real sports groups. Sport, Exercise and Performance Psychology. 2012;1:242–253. [Google Scholar]
- 23.Foreyt JP, Goodrick GK, Gotto AM. Limitations of behavioral treatment of obesity: review and analysis. J Behav Med. 1981;4(2):159–174. doi: 10.1007/BF00844268. [DOI] [PubMed] [Google Scholar]
- 24.Evans C, KL D. Group cohesion and performance: A metaanalysis. Small Group Research. 1991;22:175–186. [Google Scholar]
- 25.Maznevski M. Understanding our differences: Performance in decision-making groups with diverse members. Human Relations. 1994;47:531–552. [Google Scholar]