Abstract
Background
A discipline- and sector-specific analysis of health-care utilization by persons with mental illness in Germany is an indispensable aid to planning for the provision of adequate basic care.
Methods
Secondary data from three statutory health insurers and the German Statutory Pension Insurance Scheme for the period 2005–2007 were evaluated to identify insurees with mental illness (ICD-10 diagnosis groups F0–F5).
Results
In the period 2005–2007, 3.28 million (33%) of 9.92 million insurees had at least one contact with the health-care system in which a mental disorder was diagnosed. 50.4% (1 651 367) of these insurees had at least two mental disorders. Nearly all (98.8%) of the insurees with a psychiatric index diagnosis had at least one somatic diagnosis coded as well. 95.7% of treatments were provided in the outpatient setting. Somatic medical specialties provided the majority of treatments both in ambulatory care and in the hospital. For example, 77.5% of persons with severe depression were treated with five kinds of treatment that were provided exclusively by primary care physicians and other specialists in somatic medicine in private practice, sometimes in combination with psychiatric treatment or psychotherapy.
Conclusion
There was a high degree of comorbidity of mental and somatic illness. The fact that the vast majority of treatment was provided in the outpatient setting implies that cooperation across health-care sectors and disciplines should be reinforced, and that measures should be taken to ensure the adequate delivery of basic psychiatric care by primary care physicians.
Facing the current challenges in the care of patients with mental illness requires reliable data on their health care. The problems to be addressed include not only increased use of health care services, incapacity for work, and early retirement due to mental disorders (1, 2), but also the lack of specialized physicians with associated long waiting times, the further development required in intersectoral and interdisciplinary care, and the implementation of new care structures and new compensation systems. Germany’s health care system is very complex. Studies of care provided often include only individual sectors such as outpatient care (3). There are essentially two representative research works available on the prevalence and care of mental illness in Germany: the 1998 German National Health Interview and Examination Survey (4) and a European study (5).
The research presented here was the first to bring together secondary data from three insurers (DAK-Gesundheit, KKH-Kaufmännische Krankenkasse [formerly KKH-Allianz], and hkk-erste Gesundheit) and the German statutory pension insurance scheme over a three-year study period (2005 to 2007), forming a dataset that includes almost 3.3 million insurance holders with mental illness. This dataset differs from the German National Health Interview and Examination Survey (1998) in its use of routine data, sample size, and longitudinal design. This makes it possible to assess health care service use objectively and representatively on the basis of rehabilitation and benefit payments.
This article presents the prevalence of use of outpatient, inpatient, and rehabilitational care services by those with mental illnesses (ICD-10, F0 to F5) during the study period of 2005 to 2007. For example, for serious depressive illnesses analysis examined the specialties and sectors of care used.
This study aims to identify any shortcomings, such as problems at the interface of different sectors of care, and areas in which the care of mental illness might be optimized, through interdisciplinary and intersectoral analyses of the care pathway.
Methods
The project involved secondary, mainly descriptive analysis of the care of patients with mental illness. The study was financed by the German Medical Association (Bundesärztekammer) and funds provided by the German Association of Psychiatry, Psychotherapy and Psychosomatics (DGPPN, Deutsche Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde) and the LVR-Klinikum Düsseldorf. The involved insurers searched the secondary data (6) of a total of 9 921 363 insurance holders for coding of a mental illness in ICD-10-GM groups F0 to F5 (Figure 1) between 2005 and 2007 and made available for analysis the datasets for the insurance holders who met this selection criterion (according to the standard in use for secondary data analysis, cf. [7]).
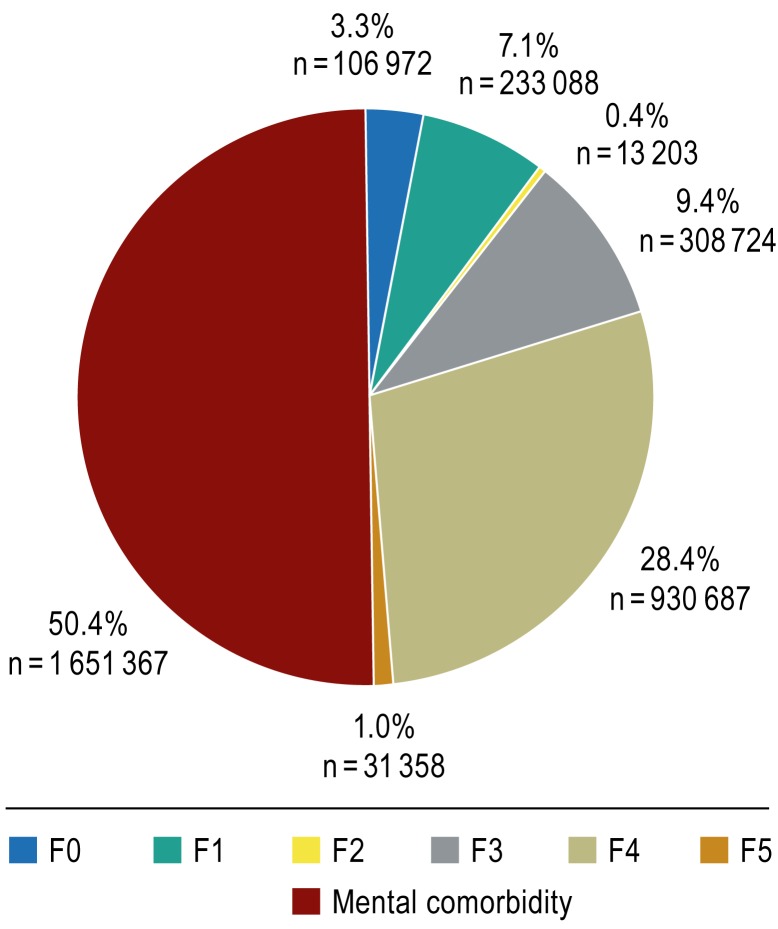
Figure 1.
Distribution of diagnoses 2005 to 2007: Insurance holders per diagnosis group. All insurance holders diagnosed with a mental disorder (F0 to F5) during the study period, 2005 to 2007 (n = 3 275 399).
F0: Organic, including symptomatic mental illnesses
F1: Mental and behavioral disorders caused by psychotropic substances
F2: Schizophrenia, schizotypal, and delusional disorders
F3: Affective disorders
F4: Neurotic, stress, and somatoform disorders
F5: Behavioral abnormalities with physical disorders and factors.
Mental comorbidity: multiple simultaneous or consecutive psychiatric diagnoses
The Institute for Health and Social Research (IGES Institut, Institut für Gesundheits- und Sozialforschung) assumed trusteeship of the data and performed data analysis. See the eBox for a detailed description of the methods used.
eBox. Detailed description of methods.
The project included essentially descriptive secondary data analysis on the care of mental illness.
Data sources
The secondary data (e1) of a total of 9 921 363 people insured with the insurers involved in the study, with coding of a mental illness in ICD-10-GM groups F0 to F5 between 2005 and 2007, were selected; the datasets were made available for analysis. Dataset selection, analysis, and measures taken to observe data protection legislation comply with the standard for secondary data analysis (Good Practice for Secondary Data Analysis [7]). The underlying data are those stipulated in clause 295 of Germany’s Social Security Code V (outpatient treatment), clause 301 of Social Security Code V (inpatient treatment) [e2]) and the German Database on Rehabilitation Statistics (e3).
Sample of insurance holders
The sample included in the research consisted of insurance holders who had had contact with the health care system as a result of a diagnosis of mental illness (according to ICD-10-GM) at least once during the study period. Selection was based on the following outpatient treatment diagnoses, main and secondary inpatient diagnoses, and diagnoses of incapacity to work:
Organic, including symptomatic mental illnesses (F0)
Mental and behavioral disorders caused by psychotropic substances (F1)
Schizophrenia, schizotypal, and delusional disorders (F2)
Affective disorders (F3)
Neurotic, stress and somatoform disorders (F4)
Behavioral abnormalities with physical disorders and factors (F5)
The Institute for Health and Social Research (IGES, Institut für Gesundheits- und Sozialforschung) assumed trusteeship of the data and performed data plausibility testing and data analysis.
Use of the health care system
Use of the health care system was analyzed on the basis of treatment cases. In insurers’ billing data, one treatment case does not correspond to one person, as a single patient may generate multiple treatment cases. In insurers’ billing data, a treatment case corresponds to a hospital stay in inpatient or day-patient care, or in outpatient care to “a treatment undertaken in whole by the same contractual physician in private practice in his/her practice, during a single quarter, for a single patient, on an outpatient basis and at the expense of a single insurance provider” (Federal Master Agreement of Physicians [as of 1 October 2006]). The treatment cases included were those for which a corresponding mental illness had been recorded (for inpatient care, only treatment cases in which the main diagnosis was a mental disorder were included). In rehabilitation, a treatment case included the period from the beginning to the end of rehabilitation measures. This included only cases for which a mental disorder was recorded. Distinctions between specialties were made on the basis of physicians’ specialization for outpatient treatment and departments’ specialization for inpatient treatment. Physicians or departments specializing in somatic medicine were considered to be all specialized physicians or departments that did not fall under the heading of specialized psychiatric/psychosomatic/psychotherapeutic care (internal medicine, gynecology, ophthalmology, etc.).
Analysis of care pathways
As an example, care pathways for severe depression (index diagnoses according to ICD-10-GM: F32.2 severe depressive episode with no psychotic symptoms; F32.3 severe depressive episode with psychotic symptoms; F33.2 recurring depressive disorder, currently severe episode with no psychotic symptoms; F33.3: recurrent depressive disorder, currently severe episode with psychotic symptoms) were analyzed, as ICD-10-GM provides information on disease severity only for depression. To facilitate representation and analysis of so many different individual care pathways, for every insurance holder the various specialties the individual had used during the care pathway and the basis on which care had been provided (inpatient/outpatient) were recorded. Each referral from one specialty to another (regardless of the duration of care in individual sectors) was recorded according to the date of treatment. Outpatient referrals within a quarterly treatment period were also placed in chronological order by treatment date. Inpatient treatment cases with an admission date during the study period and a date of discharge from outpatient treatment after the end of the study period were also included in the study. Stratification was performed according to the following care sectors and specialties: outpatient: physician specializing in psychiatry and psychotherapy/neurology; outpatient: physician specializing in psychosomatic medicine and psychotherapy; outpatient: psychotherapist; outpatient: primary care physician/other specialist in somatic medicine; inpatient: psychiatric department; inpatient: department of psychosomatic medicine/psychotherapy; inpatient: department of somatic medicine; rehabilitation. Cases were allocated pseudonyms for the purpose of care pathway analysis.
The five most common care pathways were identified and analyzed according to the following events: doctor’s note for depression, benefit claim due to depression, and mortality during the study period. For referrals between the commonest initial sectors of care and specialties and the next sectors of care and specialties, conditional probabilities of referral to another physician (p; [e4]) and confidence intervals (CI; [e5]) were estimated on the basis of the relative frequency of the referrals in question. Care pathway analyses included insurance holders with an index diagnosis assigned in the first quarter of the study (the first quarter of 2005) and uninterrupted insurance coverage until the end of the study period (31 December 2007), and those with an index diagnosis assigned in the first quarter of the study who died during the study period (1 January 2005 to 31 December 2007) (n = 1495; 5.6% of all insurance holders with severe depression in the first quarter of 2005). Naturally, in the latter case continuous observation until 31 December 2007 was not provided, as the individuals died during the study period. In these cases care data up to the date of death were evaluated. The data of all living insurance holders were analyzed up to the end of the study period (31 December 2007). The first quarter of 2005 was chosen as the period for index diagnosis, in order to ensure the longest possible study period.
Further analyses were also performed for insurance holders with an index diagnosis of severe depression during the first quarter of 2006, in order to rule out incomplete presentation of these care pathways due to left-censoring of the data resulting from the lack of a preobservation period (left-censoring would occur if a patient had already had contact with the health care system before the beginning of the study period [1 January 2005] and this was not included in the analysis). This provided a preobservation period, making it possible to distinguish between insurance holders who had already had contact with the health care system in the year before the index diagnosis of severe depression for mild (F32.0/F33.0) or moderate depression (F32.1/F33.1), those who had already had contact with the health care system as a result of another mental illness (F0 to F9, excluding depression), and those who had had no contact with the health care system during the preobservation period as a result of depression or any other mental illness.
For inpatient treatment, only service use due to severe depression (main diagnosis) was treated as an index diagnosis. For outpatient treatment, service use was only treated as an index diagnosis if severe depression was recorded in the routine data in the diagnosis category (possibly in addition to other diagnoses). Analysis of contact with the health care system following index service use included all service use associated with depression, regardless of the severity of depression.
Limitations of the data set
The secondary data do not include information on causes of death, and illness groups F6 to F9 were not included in this analysis. Data from outpatient psychiatric clinics and special forms of care (e.g. integrated care agreements) were not available. In outpatient care there are no main or secondary diagnoses, so for multiple diagnoses during outpatient care it is impossible to determine which illness is the most important. The study period was of limited duration, and the data do not reveal how much service use during this period was due to patients’ new onset disorders. Discipline-specific analysis of rehabilitation treatment was only possible on the basis of data from the German statutory pension insurance scheme, as insurance providers had no information on the facilities at which treatment was provided. The extent to which the population of people insured by substitute health insurance funds is representative of all those with statutory health insurance in Germany is limited: for example, on a sample day, 1 July 2006, 23.5 million people were insured by substitute funds (including co-insured relatives). This figure corresponded to 33.4% of all of the 70.3 million holders of statutory health insurance. Of all those insured by substitute funds, 57.2% were women. By comparison, the percentage of women among the total of 70.3 million holders of statutory health insurance in Germany on the same day was 53.1%. The percentage of pensioners insured by blue-collar and white-collar workers’ insurance funds was 23.5%; the corresponding figure for all those with statutory health insurance was 26.0%. Thus on the sample day, 1 July 2006, women were somewhat overrepresented and pensioners somewhat underrepresented among those insured by blue-collar and white-collar workers’ insurance funds when compared to the total population of those with statutory health insurance in Germany (e6). The average monthly percentages of people classified as sick among those insured by blue-collar workers’ insurance funds (3.20% in 2006) and those insured by white-collar workers’ insurance funds (3.30%) were comparable to the percentages for all those with statutory health insurance (3.31%) (e7).
The limitations associated with secondary data analysis are described in detail in the Discussion section and the further description of the methods used (eBox).
Results
Distribution of coded diagnoses
3 275 399 people insured with the insurers involved in this study met the criterion of an index diagnosis F0 to F5 during the study period (1 January 2005 to 31 December 2007). Figure 1 shows the distribution of diagnoses. Of the insurance holders with an index diagnosis, 50.4% presented mental comorbidity in the form of multiple diagnoses from different mental illness diagnosis groups, either simultaneously or longitudinally. The distribution of diagnoses has already been presented elsewhere (8). The differences between the distribution of diagnoses recorded here and that reported previously are the result of different groupings of the people in question: in the findings presented here all insurance holders with more than one diagnosis of mental illness were placed in the group “mental comorbidity” (Figure 1), while in the previous analysis they were counted multiple times.
For patients with mental comorbidity, the most common diagnosis combinations came from groups F3 (affective disorders) and F4 (neurotic, stress, and somatoform disorders). A code for at least one additional somatic diagnosis had also been recorded for nearly all insurance holders with a diagnosis of mental illness (inpatient or outpatient) (F0: 96.4%, F1: 96.5%, F2: 88.3%, F3: 98.2%, F4: 99%, F5: 99.1%; total for somatic comorbidity: 98.8%). In order to obtain the most comprehensive overview possible, analysis included all somatic diagnoses (at least one coded outpatient diagnosis or main/secondary inpatient diagnosis according to ICD-10, Chapter A to E, G to T [except G30]) during the study period.
Use of the health care system
Case-based analysis (eBox) for the three-year study period yielded almost 22 million cases treated for a diagnosis of mental illness (multiple cases for a single individual were possible. Of all treatments, 95.7% were provided on an outpatient basis, 4.2% on an inpatient basis, and 0.1% on a day-patient basis.
Of the insurance holders with an index diagnosis, 98% had received at least one outpatient treatment, 6% one inpatient treatment, and 0.2% one day-patient treatment (multiple treatments for a single individual permitted). Outpatient or inpatient rehabilitation care with a main diagnosis of a mental disorder was received by 2.6% of those insured.
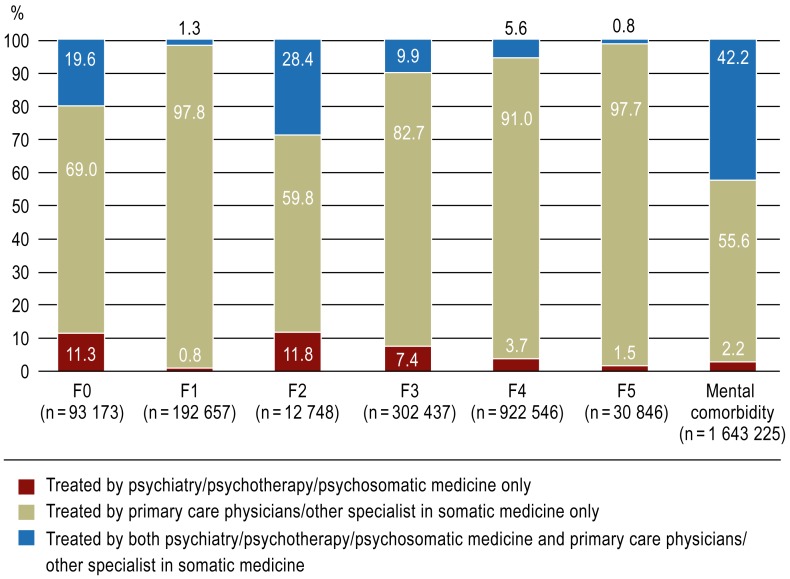
Almost three-quarters of insurance holders who received outpatient treatment for a psychiatric diagnosis were cared for only by primary care physicians or other specialists in somatic medicine (Figure 2).
Figure 2.
Outpatient care (2005 to 2007) by discipline and diagnosis (F0 to F5). All insurance holders receiving outpatient treatment and diagnosed with a mental illness (N = 3 197 632, corresponding to 97.6% of all patients diagnosed with a mental illness).
F0: Organic, including symptomatic mental illnesses
F1: Mental and behavioral disorders caused by psychotropic substances
F2: Schizophrenia, schizotypal, and delusional disorders
F3: Affective disorders
F4: Neurotic, stress, and somatoform disorders
F5: Behavioral abnormalities with physical disorders and factors.
Mental comorbidity: multiple simultaneous or consecutive psychiatric diagnoses
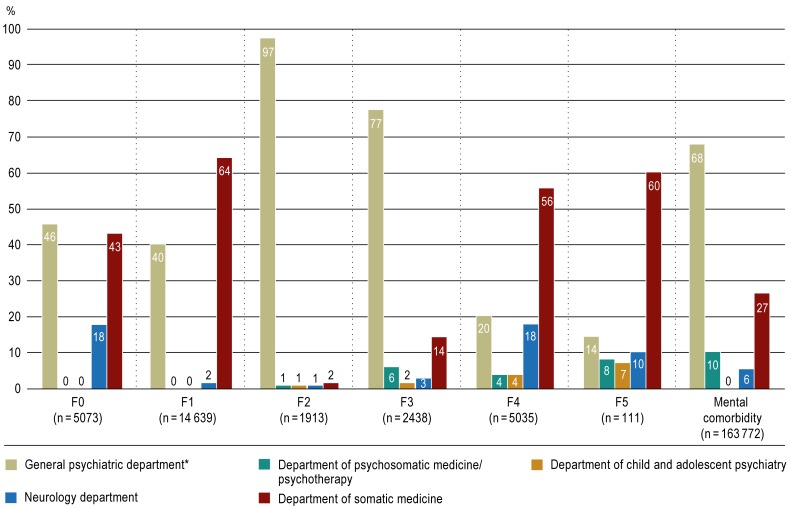
In inpatient care too, a relatively high percentage (27% to 64%) of patients with a psychiatric main diagnosis received care in departments specializing in somatic medicine (Figure 3).
Figure 3.
Percentages of care provided in inpatient and day-patient facilities for patients with a main diagnosis of mental illness during the study period, 2005 to 2007, by department type. All insurance holders receiving inpatient treatment for a main diagnosis of a mental illness F0 to F5 (N = 192 981). Multiple cases for a single individual permitted (individuals with multiple inpatient stays, possibly in multiple departments).
F0: Organic, including symptomatic mental illnesses
F1: Mental and behavioral disorders caused by psychotropic substances
F2: Schizophrenia, schizotypal, and delusional disorders
F3: Affective disorders
F4: Neurotic, stress, and somatoform disorders
F5: Behavioral abnormalities with physical disorders and factors.
Mental comorbidity: multiple simultaneous or consecutive psychiatric diagnoses.
*Treatment in addiction/geriatric psychiatry is included in general psychiatric departments
The greatest amount of outpatient rehabilitation care for treatment cases with a psychiatric main diagnosis was provided by departments specializing in psychosomatic care (n = 25 136, approximately 67% of all cases of rehabilitation treatment in 2005 to 2007). This was followed by departments specializing in addiction medicine (n = 5674, 15%), and general psychiatric departments (n = 3509, 9%). In 6% (n = 2392) of cases of rehabilitation with a psychiatric main diagnosis, patients were treated in departments specializing in somatic medicine, 0.1% (n = 3077) on an outpatient basis.
Care for severe depression
During the observation period, 110 462 insurance holders were diagnosed with severe depression (ICD-10-GM: F32.2, F32.3, F33.2, F33.3). In 23.9% of these cases (n = 26 412) the patient was diagnosed with severe depression as early as the first quarter of 2005. These individuals formed the index population for sample analysis of the care pathway. Sociodemographically, this core group differed little from the total population of all insurance holders diagnosed with severe depression (Table 1). A total of 524 different care pathways were found; they differed in terms of the type, number, or chronological sequence of the sectors of care or specialties. The most common pathways were those involving primary care and specialties within somatic medicine, and physicians specializing in psychiatry and psychotherapy (eTable 1).
Table 1. Distribution of sociodemographic characteristics of total population of patients with severe depression, index population, and selected subpopulations by care pathway (five most common care pathways).
| Population | N/n | Age on 01/01/2006, mean in years (standard deviation) | Male/female % (99% CI) | Former East or West Germany*1 % (99% CI) | Urban/rural*2*1 % (99% CI) | Mental comorbidity*3 % (99% CI) | Somatic comorbidity*4 % (99% CI) | |
|---|---|---|---|---|---|---|---|---|
| Total population of patients with severe depression (index diagnosis 1 January 2005 to 31 December 2007) | 110462 |
53.2 (±16.5) |
23.2/76.8 (22.9 to 23.5)/ (76.5 to 77.1) |
11.4/88.6 (11.2 to 11.7)/ (88.3 to 88.8) |
87.0/12.8 (86.7 to 87.3)/ (12.5 to 13.1) |
88.5 (88.3 to 88.8) |
99.8 (99.7 to 99.8) |
|
| Index population of patients with severe depression (index diagnosis 1st quarter of 2005) | 26412 |
57.5 (±15.2) |
22.4*5/77.6 (21.8 to 23.1)/ (76.9 to 78.2) |
12.3*5/87.7*5 (11.8 to 12.8)/ (87.1 to 88.2) |
88.9*5/10.9*5 (88.4 to 89.4)/ (10.4 to 11.4) |
86.3 (85.7 to 86.8) |
99.8 (99.8 to 100) |
|
| Number of care pathway*6 | Subpopulations by care pathway | |||||||
| 1 | Primary care physician/other specialist in somatic medicine (no onward referral) | 10354 |
59.5 (±15.6) |
22.5/77.5 (21.5 to 23.6)/ (76.4 to 78.5) |
11.1/88.9 (10.3 to 11.9)/ (88.1 to 89.7) |
88.3/11.5 (87.5 to 89.1)/ (10.7 to 12.3) |
78.0 (77.0 to 79.1) |
99.9 (99.9 to 100.0) |
| 2 | Primary care physician/other specialist in somatic medicine, referral to physician specializing in psychiatry and psychotherapy | 5466 |
60.5 (±13.9) |
22.0/78.0 (20.6 to 23.5)/ (76.5 to 79.4) |
15.6/84.3 (14.4 to 16.9)/ (83.0 to 85.6) |
88.7/11.1 (87.6 to 89.9)/ (10.0 to 12.1) |
89.4 (88.4 to 90.5) |
99.9 (99.9 to 100.0) |
| 3 | Physician specializing in psychiatry and psychotherapy, referral to primary care physician/other specialist in somatic medicine | 2679 |
57.2 (±14.0) |
22.1/77.9 (20.0 to 24.2)/ (75.8 to 80.0) |
12.0/88.0 (10.4 to 13.6)/ (86.4 to 89.6) |
89.5/10.5 (88.0 to 91.1)/ (8.9 to 12.0) |
90.6 (89.1 to 92.0) |
99.9 (99.9 to 100) |
| 4 | Physician specializing in psychiatry and psychotherapy (no onward referral) | 1380 |
59.7 (±15.5) |
30.1/69.9 (26.9 to 33.3)/ (66.7 to 73.1) |
11.4/88.6 (9.2 to 13.6)/ (86.4 to 90.8) |
90.5/9.4 (88.5 to 92.5)/ (7.3 to 11.4) |
85.8 (83.4 to 88.2) |
98.8 (98.1 to 99.6) |
| 5 | Primary care physician/other specialist in somatic medicine, referral to physician specializing in psychiatry and psychotherapy, further referral to psychiatric department | 609 |
59.8 (±13.8) |
22.2/77.8 (17.8 to 26.5)/ (73.5 to 82.2) |
19.4/80.6 (15.2 to 23.5)/ (76.5 to 84.8) |
86.2/13.5 (82.6 to 89.8)/ (9.9 to 17.0) |
95.1 (92.8 to 97.3) |
99.8 (99.4 to 100) |
*1Percentages may not total 100%, as for a small number of included insurance holders (<1%) there is no information on place of residence
*2Urban: conglomerations (regions with center of population >300 000 inhabitants or population density ≥300 inhabitants/km 2) and urban areas (regions with center of population >100000 in≥habitants or population density >150 inhabitants/km 2, minimum density 100 inhabitants/km 2); rural: regions with population density <150 inhabitants/km 2 and no center of population >100≥000 inhabitants, regions with center of population >100 000 inhabitants and population density ≤100 inhabitants/km 2 (definitions according to the German Federal Institute for Research on Building, Urban Affairs and Spatial Development, [BBSR, Bundesinstitut für Bau-, Stadt- und Raumforschung]).
*3At least one coded outpatient diagnosis or main or secondary inpatient diagnosis of a further mental illness excluding depression according to ICD-10-GM, Chapter F during the study period, 1 January 2005 to 31 December 2007.
*4At least one coded outpatient diagnosis or main or secondary inpatient diagnosis according to ICD-10-GM, Chapter A to E, G to T (excluding G30) during the study period, 1 January 2005 to 31 December 2007.
*5According to the 99% CI there is a significant difference (no overlap of confidence interval) between the figure for the total population with severe depression (index diagnosis 1 January 2005 to 31 December 2007).
*6In decreasing order of frequency of care pathway (cf. Figure 4). 99% CI: 99% confidence interval
eTable 1. Percentages of insurance holders in the index population using sectors of care/specialties during care, 2005 to 2007.
| Sector of care/specialty | Percentage of insurance holders in index population* (%) |
|---|---|
| Primary care physician/specialist in somatic medicine in private practice | 93.1 |
| Psychiatrist/psychotherapist/neurologist in private practice | 52.7 |
| Specialist in psychosomatic medicine and psychotherapy in private practice | 10.5 |
| Psychotherapist in private practice | 3.7 |
| Inpatient psychiatric department | 12.4 |
| Inpatient psychosomatic department | 1.4 |
| Department of somatic medicine | 0.7 |
*Multiple cases for a single insurance holder permissible
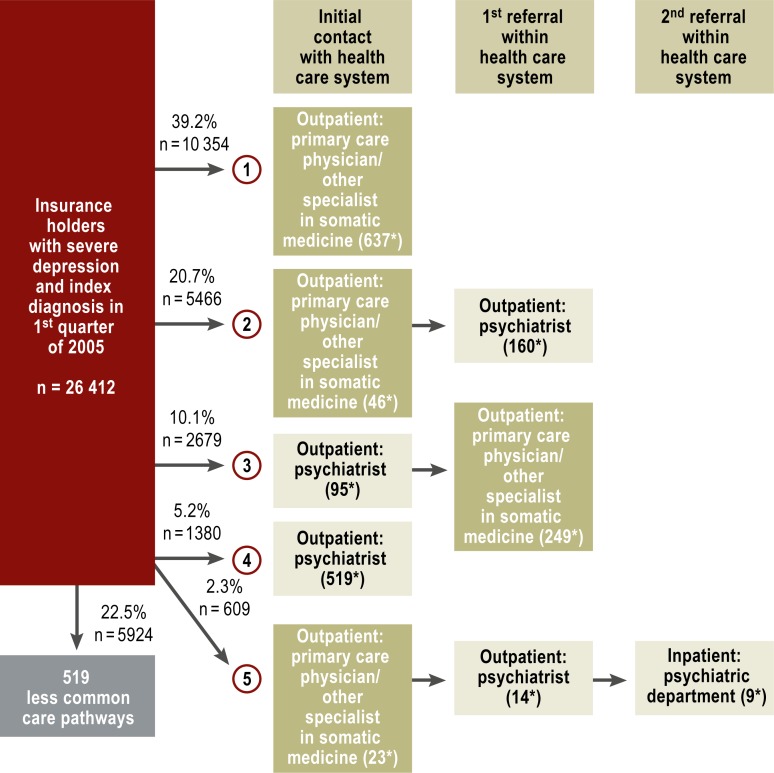
Most (74%) of the initial care provided at the beginning of the observation period (index care) was provided on an outpatient basis by a primary care physician or an other specialist in somatic medicine. In these cases, the probability of not being referred to another sector of care or another specialty during the time period studied was 53%. The probability of being referred on to another physician specializing in psychiatry and psychotherapy was 36%; and the probability of being transferred to another sector of care or another specialty was 11%.
For index care provided on an outpatient basis by a physician specializing in psychiatry and psychotherapy or neurology, which accounted for 20% of all index cases, the probability of not being referred to another sector of care or another specialty was 26%. The probability of being referred to a primary care physician or an other specialist in somatic medicine was 63%; the probability of being referred to another sector of care or another specialty was 11%.
For 2.5% of the index population, outpatient treatment was initially provided by a physician specializing in psychosomatic medicine and psychotherapy; for 0.7% it was initially provided by a psychotherapist (Psychologischer Psychotherapeut). Inpatient index care was very rare (department of somatic medicine: 0.1%; psychiatric department: 2.2%; department of psychosomatic medicine: 0.2%; rehabilitation: 0.2%). For these rarer types of index care, the probability of not being referred on to another sector of care was lower than for primary or psychiatric index care (primary care physician/other specialist in somatic medicine: 53%; physician specializing in psychiatry and psychotherapy/neurology: 26%; physician specializing in psychosomatic medicine and psychotherapy: 14%; psychotherapist: 13%; department of somatic medicine: 12%; psychiatric department: 12%; psychosomatic department: 4%; rehabilitation: 0.4%).
The five most common care pathways in this research, which together accounted for more than three-quarters (77.5%) of the index population, are shown in Figure 4.
Figure 4.
Pathways of health care during the study period 2005 to 2007 for those with an index diagnosis of severe depression in the first quarter of 2005 (ICD-10-GM: F32.2/F32.3/F33.2/F33.3) (n = 26 412). There were 524 different care pathways. The five most common pathway types are described in greater detail in decreasing order of frequency.
*Median time in sector of care, days (with no treatment in another sector of care in the intervening period; time from first to last day of treatment)
The study investigated significant events during these five most common care pathways (Table 2). The rates of incapacity for work and retirement were significantly lower for the two care pathways that included no referral to another sector of care than for any others. These care pathways also had the highest mortality rates.
Table 2. Events during care pathway in severe depression, stratified according to the five most common care pathways.
| Number of care pathway*1 | Care pathway | Number/percentage of insurance holders with care pathway n (%) | Percentage of patients unable to work due to mental illness*2 % (99% CI) | Percentage of patients retiring early due to mental illness*3 % (99% CI) | Mortality % (99% CI) |
|---|---|---|---|---|---|
| 1 | Primary care physician/other specialist in somatic medicine (no onward referral) |
10354 (39.2) |
5.7 (5.1 to 6.3) |
0.2 (0.06 to 0.27) |
7.6 (6.9 to 8.2) |
| 2 | Primary care physician/other specialist insomatic medicine, referral to physician specializing in psychiatry and psychotherapy |
5466 (20.7 ) |
10.6 (9.5 to 11.7) |
0.8 (0.05 to 1.1) |
5.4 (4.6 to 6.2) |
| 3 | Physician specializing in psychiatry and psychotherapy, referral to primary care physician/other specialist in somatic medicine |
2679 (10.1) |
13.5 (11.8 to 15.2) |
1.0 (0.5 to 1.5) |
3.1 (2.2 to 3.9) |
| 4 | Physician specializing in psychiatry and psychotherapy (no onward referral) |
1380 (5.2) |
8.2 (6.3 to 10.1) |
0.3 (0 to 0.7) |
7.3 (5.5 to 9.1) |
| 5 | Primary care physician/other specialist in somatic medicine, referral to physician specializing in psychiatry and psychotherapy, further referral to psychiatric department |
609 (2.3) |
16.7 (12.8 to 20.7) |
3.1 (1.3 to 4.9) |
5.7 (3.3 to 8.2) |
*1In decreasing order of frequency of care pathway (cf. Figure 4).
*2When interpreting incapacity for work and early retirement , it should be remembered that the index population also includes insurance holders who were not of working age (<15 years or >65 years). The corresponding percentages may therefore be underestimates. These age limits are generally chosen in order to give the most complete possible overview of working age, even though its age boundaries are usually imprecisely defined. It should also be remembered that there is no causal relationship between mortality and the care pathway or the parameters incapacity for work and early retirement. 99% CI: 99% confidence interval
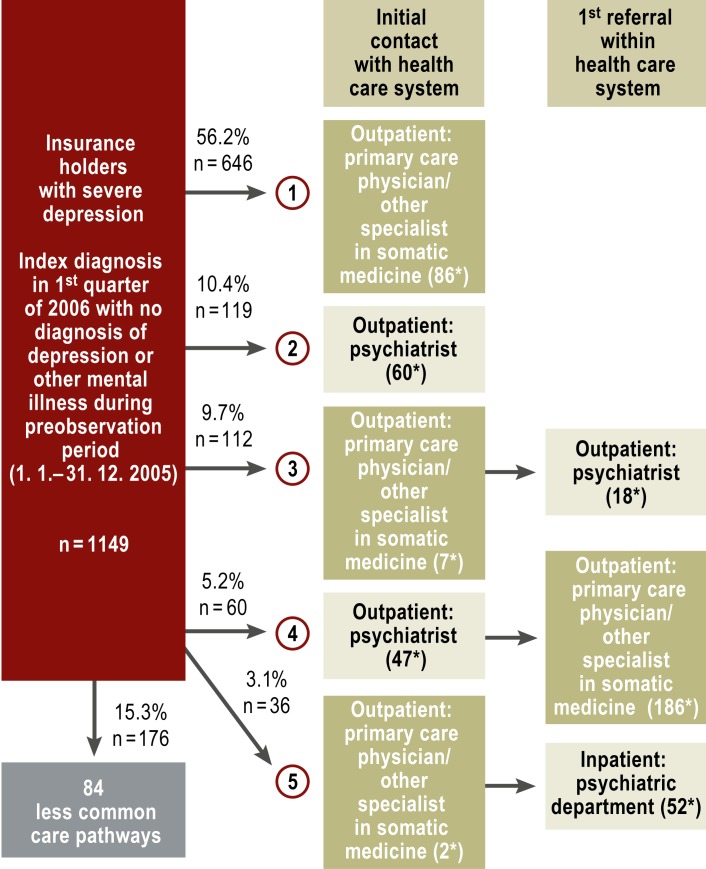
In addition, persons with an index diagnosis of severe depression in the first quarter of 2006 who had not used the health care system for a depressive or other psychiatric disorder in 2005 (n = 1149) were analyzed separately, in order to rule out incomplete presentation of these care pathways due to left-censoring of the data resulting from the lack of a preobservation period. These analyses showed certain shifts in order; the most common of these in this analysis too was “primary care physician/other specialist in somatic medicine, no onward referral” (eFigure, eTables 2 and 3).
eTable 2. Distribution of sociodemographic characteristics of total population of patients with severe depression, index population, and selected subpopulations by care pathway (five most common care pathways).
| Population | N/n | Age on 01/01/2006, mean in years (standard deviation) | Male/female % (95% CI) | Former East or West Germany*1 % (95% CI) | Urban/rural*2*1 % (95% CI) | Mental comorbidity*3 % (95% CI) | Somatic comorbidity*4 % (95% CI) | |
|---|---|---|---|---|---|---|---|---|
| Total population of patients with severe depression (index diagnosis 1 January 2005 to 31 December 2007) | 110462 |
53.2 (±16.5) |
23.2/76.8 (22.9 to 23.5)/ (76.5 to 77.1) |
11.4/88.6 (11.2 to 11.7)/ (88.3 to 88.8) |
87.0/12.8 (86.7 to 87.3)/ (12.5 to 13.1) |
88.5 (88.3 to 88.8) |
99.8 (99.7 to 99.8) |
|
| Index population of patients with severe depression (index diagnosis 1st quarter of 2006 with no diagnosis of depression or other mental illness [F0 to F5] in 2005) | 1149 |
50.9 (±17.9) |
27.9*5/72.1*5 (25.3 to 30.4)/ (69.6 to 74.7) |
11.5/88.3 (9.6 to 13.3)/ (86.5 to 90.2) |
88.3/11.3 (86.5 to 90.2)/ (9.5 to 13.1) |
68.4 (65.7 to 71.1) |
99.5 (99.1 to 99.9) |
|
| Number of care pathway*6 | Subpopulations by care pathway | |||||||
| 1 | Primary care physician/other specialist in somatic medicine (no onward referral) | 646 |
52.4 (±18.8) |
24.6/75.4 (21.2 to 27.9)/ (72.1 to 78.8) |
12.3/87.3 (10.3 to 15.5)/ (84.3 to 89.5) |
87.2/12.3 (84.7 to 89.8)/ (9.7 to 14.8) |
57.2 (53.4 to 61.1) |
99.8 (99.5 to 100) |
| 2 | Physician specializing in psychiatry and psychotherapy (no onward referral) | 119 |
54.4 (±18.3) |
35.8/64.2 (25.1 to 46.5)/ (53.5 to 74.9) |
8.6/91.4 (1.5 to 13.2)/ (86.8 to 98.4) |
91.4/8.6 (85.1 to 97.6)/ (2.3 to 14.9) |
70.4 (60.2 to 80.5) |
97.5 (94.1 to 100) |
| 3 | Primary care physician/other specialist in somatic medicine, referral to physician specializing in psychiatry and psychotherapy | 112 |
49.5 (±16.8) |
26.9/73.1 (18.3 to 35.6)/ (64.4 to 81.7) |
13.5/86.5 (3.2 to 14.1)/ (85.9 to 96.8) |
86.5/13.5 (79.9 to 93.2)/ (6.8 to 20.1) |
81.7 (74.2 to 89.3) |
100 (100 to 100) |
| 4 | Physician specializing in psychiatry and psychotherapy, referral to primary care physician/other specialist in somatic medicine | 60 |
49.8 (±14.2) |
28.3/71.7 (16.6 to 40.1)/ (59.9 to 83.4) |
13.3/86.7 (1.1 to 15.5)/ (84.5 to 98.9) |
86.7/13.3 (77.8 to 95.5)/ (4.5 to 22.2) |
90 (82.2 to 97.8) |
100 (100 to 100) |
| 5 | Primary care physician/other specialist in somatic medicine, referral to psychiatric department | 36 |
49.1 (±17.4) |
50/50 (27.3 to 72.6)/ (27.3 to 72.6) |
9.1/90.9 (0.7 to 35.7)/ (64.3 to 99.3) |
90.9/9.1 (77.9 to 100)/ (0 to 22.1) |
77.3 (58.3 to 96.3) |
100 (100 to 100) |
*1Percentages may not total 100%, as for a small number of included insurance holders (<1%) there is no information on place of residence
*2Urban: conglomerations (regions with center of population >300 000 inhabitants or population density ≥300 inhabitants/km 2) and urban areas (regions with center of population >100 000 inhabitants or population density >150 inhabitants/km 2, minimum density 100 inhabitants/km 2); rural: regions with population density <150 inhabitants/km 2 and no center of population >100 000 inhabitants, regions with center of population >100 000 inhabitants and population density ≤100 inhabitants/km 2 (definitions according to the German Federal Institute for Research on Building, Urban Affairs and Spatial Development, [BBSR, Bundesinstitut für Bau-, Stadt- und Raumforschung])
*3At least one coded outpatient diagnosis or main or secondary inpatient diagnosis of a further mental illness excluding depression according to ICD-10-GM, Chapter F during the study period, 1 January 2005 to 31 December 2007.
*4At least one coded outpatient diagnosis or main or secondary inpatient diagnosis according to ICD-10-GM, Chapter A to E, G to T (excluding G30) during the study period, 1 January 2005 to 31 December 2007.
*5According to the 95% CI there is a significant difference (no overlap of confidence interval) between the figure for the total population with severe depression (index diagnosis 1 January 2005 to 31 December 2007).
*6In decreasing order of frequency of care pathway.
For the total population, the confidence interval was calculated at a 99% significance level on the basis of the sample. For the index population and the subpopulations the confidence interval was calculated at only a 95% significance level, due to the relatively small sample size. 95% CI: 95% confidence interval
eTable 3. Events during care pathways in severe depression, stratified according to the five most common care pathways for insurance holders with no diagnosis of depression or any other mental illness during the preobservation period, 1 January to 31 December 2005; n = 1149.
| Number of care pathway*1 | Care pathway | Number/percentage of insurance holders with care pathway n (%) | Percentage of patients unable to work due to mental illness*2 % (95% CI) | Percentage of patients retiring early due to mental illness*2 % (95% CI) | Mortality % (95% CI) |
|---|---|---|---|---|---|
| 1 | Primary care physician/other specialist in somatic medicine (no onward referral) |
646 56.2 |
10.3 (7.9 to 12.6) |
0 (0 to 0) |
3.1 (1.8 to 4.5) |
| 2 | Physician specializing in psychiatry and psychotherapy (no onward referral) |
119 10.4 |
7.4 (1.6 to 13.2) |
0 (0 to 0) |
2.5 (0 to 5.9) |
| 3 | Primary care physician/other specialist in somatic medicine, referral to physician specializing in psychiatry and psychotherapy |
112 9.7 |
19.2 (11.5 to 26.9) |
1.0 (0 to 2.9) |
5.8 (1.2 to 10.3) |
| 4 | Physician specializing in psychiatry and psychotherapy, referral to primary care physician/other specialist in somatic medicine |
60 5.2 |
18.3 (8.3 to 28.4) |
1.7 (0 to 5.0) |
0 (0 to 0) |
| 5 | Primary care physician/other specialist in somatic medicine, referral to psychiatric department |
36 3.1 |
31.8 (10.7 to 53.0) |
0 (0 to 0) |
9.1 (0 to 22.1) |
*1 In decreasing order of frequency of care pathway.
*2When interpreting incapacity for work and early retirement , it should be remembered that the index population also includes insurance holders who were not of working age (<15 years or >65 years). The corresponding percentages may therefore be underestimates. These age limits are generally chosen in order to give the most complete possible overview of working age, even though its age boundaries are usually imprecisely defined. It should also be remembered that there is no causal relationship between mortality and the care pathway or the parameters incapacity for work and early retirement. 95% CI: 95% confidence interval
Discussion
Approximately 70 million people in Germany hold statuary health insurance (as of 2012, National Association of Statutory Health Insurance Funds [GKV Spitzenverband]). The number insured with the insurers involved in this study is 9 921 396, approximately one in seven holders of statutory health insurance.
Of all insurance holders, 33% had contact with the health care system during the three-year study period as a result of diagnosis of a mental illness. The most common types of service use resulted from mental comorbidity, followed by neurotic, stress, and somatoform disorders (F4), affective disorders (F3), and addictions (F1). In terms of their relative ranking, the service use prevalence rates shown here essentially reflect the prevalence rates already reported in the German National Health Interview and Examination Survey (4). These figures show the high demand for psychiatric/psychosomatic/psychotherapeutic care. This may pose a challenge for care planning in line with demand, as there is currently a lack of specialized physicians (9).
All those with mental illness showed high rates of mental and somatic comorbidity during the study period. The high rate of mental comorbidity (50.4%) is comparable with the rate reported in the 1998 German National Health Interview and Examination Survey (48% [4]). In addition to their psychiatric diagnosis, more than 90% of those insured were also diagnosed with a somatic disorder (excluding the group F2: 88.3%) during their care. The comparatively low somatic comorbidity rate in those with schizophrenia and other psychotic disorders (F2) may be evidence of underdiagnosis of somatic illnesses in this group of patients, as this is precisely where one would expect a comparatively high percentage of somatic comorbidity (10). Overall, our findings highlight the high rates of mental and somatic comorbidity in those with mental illness (11), just as those with somatic illness have an increased risk of somatic and mental comorbidity (12– 15). This means interdisciplinary care including psychiatric/psychosomatic/psychotherapeutic disciplines and primary care or other somatic specialties must be developed. Ungewitter et al. (16) found that treating physicians rarely collaborate in care of the mentally ill, and when they do this is usually only through flexible networks, not explicit collaboration.
Most care services were used by those with mental illness on an outpatient basis, as already shown in the 1998 German National Health Interview and Examination Survey (17). The current compensation structures mean that securing specialist care on an outpatient basis will become a particular challenge, as the funding structure does not provide a sufficient guarantee that guideline-compliant care or compensation for the necessary scope of treatment will be provided (9).
For both inpatients and outpatients, a considerable proportion of care for mental illnesses was provided by primary care physicians/other specialists in somatic medicine (18). Studies of the prevalence of the use of care by those with mental illness in Europe show that only 30% to 50% of the mentally ill have been treated by psychiatrists and psychotherapists (19). The relatively low proportion of psychiatric/psychosomatic/psychotherapeutic care may result from a lack of specialized physicians, together with barriers to access to specialized care. The German Federal Chamber of Psychotherapists reported very long waiting times for psychotherapy (20). Individual patients’ behavior when seeking help and their treatment preferences may also play a role. Primary care physicians remain the gateway for patients with mental complaints, and primary care carries little stigma (21). An insufficient rate of referral to specialized care may also be a possible cause. The reasons for there being less use of specialized psychiatric/psychosomatic/psychotherapeutic care than of primary care should be evaluated in the future.
Sample analyses of cases of severe depression reveal the low levels of collaboration between primary and specialized care. The results shown here for severe depression are taken from care analyses that bring together various disciplines and sectors of care for the first time; until now only individual aspects have been investigated, at the most (22, 23). The authors’ own cross-section analyses had already shown the high percentage of care provided by disciplines within primary care and somatic medicine (24).
There was a high number of care pathways (n = 524); the most common type of pathway was care by primary care physicians or other specialists in somatic medicine in private practice, sometimes in combination with psychiatric or neurological care. As shown by studies of the diagnosis of depression in primary care, depression in primary care practice is very common according to expert opinion, but only some are diagnosed as such (26– 28). In general, there are low rates of care for mental illnesses (19). Furthermore, Schneider et al. (25) found a higher rate of non-guideline-compliant treatment for depression in primary care compared to specialized psychiatric care. However, there are no systematic studies on the quality of outpatient care for depression in either primary or specialized care. In view of this situation, greater emphasis should be placed on measures to optimize the quality of outpatient care for depression (and other mental illnesses).
International studies show that depression is associated with an extremely heavy personal and societal burden, even more so than other widespread diseases such as diabetes and coronary heart disease (29, 30). The extent to which the care pathway is associated with unfavorable outcomes such as incapacity for work, early retirement, and mortality is not yet clear. Such questions take on particular significance given that, as discussed, there is room for improvement in the diagnosis and treatment of depression.
The analyses presented here do not show a systematic relationship between care pathways and these illness-associated events. The lowest rates of incapacity for work and early retirement as a result of depression occurred in the two care pathways without onward referral from the initial sector of care. This may indicate that cases of depressive disorders with more favorable prognoses are found with this type of care; this is also suggested by the fact that these cases show the significantly lowest rates of mental comorbidity. An argument against this idea is provided by the comparatively high mortality rate. The mortality rate cannot be interpreted as an age-related artefact, because the average age was almost identical for all care pathways. This may indicate that comprehensive, interdisciplinary care, possibly including inpatient care, has an effect in preventing mortality/suicide.
Limitations
The predictive power of the care analyses performed here was limited first of all by the fact that for index diagnoses made in the first quarter of 2005 no distinction could be made between insurance holders with and without a preexisting depressive or other mental illness, as there was no preobservation period. Additional analyses were therefore performed, including only insurance holders who had not had any contact with the health care system for a depressive or other preexisting mental illness for a one-year preobservation period. This essentially confirmed the results of the first analyses.
Because these analyses found no evidence of a systematic relationship between the characteristics of care pathways and illness-related events during care, detailed analysis should clarify whether other predicting factors, such as frequency of service use or length of treatments, have any influence. These analyses were not included in the evaluations presented here.
Further factors limiting the analyses of pathways of care are, on the one hand, lack of information on initial diagnoses, and, on the other hand, the fact that it was not possible to include contact with the health care system before and after the beginning of the observation period; this means the whole care pathway may not have been covered.
A further limitation to be taken into account when interpreting somatic comorbidity is the fact that the analysis included all somatic diagnoses, in order to provide as complete as possible a picture of health care service use for somatic illnesses. No distinction was made here between milder, short-term and severe, chronic illnesses.
One major methodological limitation in the analysis of secondary data is the unknown validity and reliability of the underlying information (31). The data used for this study were examined for plausibility and completeness at the IGES Institut. No external data validation such as checking against medical records was possible; as a result, the influence of mistaken diagnoses cannot be completely ruled out. For primary care, analysis did show that for various reasons primary care physicians often do not provide a psychiatric diagnosis of depression, although they are aware of the mental burden on those affected and take it into account in consultation (28). Further limitations of the evaluation of secondary data analyses are shown in detail in the eBox.
Conclusion, outlook
This project accomodates demands to use routine data for purposes of research into health care processes and for purposes of quality assurance (32). The results of the analysis show, on the one hand, an imbalance between health service use for mental illnesses and, on the other, the high levels of somatic and mental comorbidity in those with mental illness. In addition, we analyzed some of the more common care pathways for those with severe depression for the German health care system as an example; this yielded a high proportion of nonspecific psychiatric/psychosomatic/psychotherapeutic care.
Setting aside boundaries between different disciplines and sectors, the use of secondary data can, despite all its limitations, contribute to the detection of underdiagnosis, overdiagnosis, mistaken allocation, and intersectoral interface problems. This is revealed in the findings of this study, such as the detection of a high proportion of care provided by disciplines specializing in somatic medicine and somewhat low levels of interdisciplinary and intersectoral care. More importance should therefore be attached to secondary data as a routinely available source of data for further planning of care for mental illness.
Key Messages.
The high prevalence of health care service use as a result of mental illness (33% of all insurance holders included in this analysis) demonstrates a high level of demand for psychiatric/psychosomatic/psychotherapeutic care.
The high rates of mental and somatic comorbidity show the need for institutionalized interdisciplinary and intersectoral care, in order to provide adequate treatment for both mental and somatic illnesses.
The reasons for there being less use of specialized psychiatric/psychosomatic/psychotherapeutic care than of primary care for mental illness should be evaluated in the future. Efforts should be made to achieve greater involvement of psychiatric/psychosomatic/psychotherapeutic disciplines in care.
As outpatient primary care is by far the most common form of care for depression, greater emphasis should be placed on quality management in this sector
eFIGURE.
Care pathways during the study period 2006 to 2007 for those with an index diagnosis of severe depression (ICD-10-GM: F32.2/F32.3/F33.2/F33.3) in the first quarter of 2006 (with no diagnosis of depression of any severity or any other mental illness during the preobservation period, 1 January to 31 December 2005; n = 1149). There were 89 different care pathways. The five most common pathway types are described in greater detail in decreasing order of frequency.
*Median time in sector of care, days (with no treatment in another sector of care in the intervening period; time from first to last day of treatment)
Acknowledgments
Translated from the original German by Caroline Devitt, M.A.
Footnotes
Conflict of interest statement
Prof. Gaebel is a faculty member of the Lundbeck International Neuroscience Foundation (Scientific Advisory Board). He has received reimbursement of travel expenses from the DGPPN, the AQUA-Institut, and the Federal Working Group of Psychiatric Hospital Operators (Bundesarbeitsgemeinschaft der Träger psychiatrischer Krankenhäuser). He has received event sponsorship (symposium support) from Lilly, Servier, and Janssen Cilag.
M.A. Kowitz has received reimbursement of travel expenses from the DGPPN.
Prof. Fritze has received consultancy fees (Scientific Advisory Board) from Janssen Lundbeck, Lilly, Pfizer, Roche, Novartis, 3M, Eisai, AstraZeneca, the Private Health Insurance Association (Verband der Privaten Krankenversicherung), and the DGPPN.
PD Dr. Zielasek has received reimbursement of conference fees and travel expenses from the DGPPN.
References
- 1.DRAK- Unternehmen Leben. www.presse.dak.de/ps.nsf/Show/03AF73C39B7227B0C12576BF004C8490/$File/DAK_Gesundheitsreport_2010_2402.pdf. Hamburg: 2010. DAK-Gesundheitsreport 2010. last accessed 17. October 2013. [Google Scholar]
- 2.Dannenberg A, Hofmann J, Kaldybajewa K, Kruse E. Rentenzugang 2009: Weiterer Anstieg der Zugänge in Erwerbsminderungsrenten wegen psychischer Erkrankungen. RV aktuell. 2009;9:283–293. [Google Scholar]
- 3.Albrecht M, Fürstenberg T, Gottberg A. IGES Institut. Berlin: 2007. Strukturen und Finanzierung der neurologischen und psychiatrischen Versorgung. [Google Scholar]
- 4.Wittchen HU, Jacobi F. Die Versorgungssituation psychischer Störungen in Deutschland. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2001;44:993–1000. [Google Scholar]
- 5.Kovess-Masfety V, Alonso J, Brugha TS, Angermeyer MC, Haro JM, Sevilla-Dedieu C and the ESEMeD/MHEDEA 2000 Investigators. Differences in lifetime use of services for mental health problems in six European countries. Psychiat Serv. 2007;58:213–220. doi: 10.1176/ps.2007.58.2.213. [DOI] [PubMed] [Google Scholar]
- 6.Hoffmann F, Glaeske G. Neugebauer EAM. Analyse von Routinedaten. In: Pfaff H, Glaeske F, Schrappe M, editors. Lehrbuch Versorgungsforschung. Systematik - Methodik - Anwendung. Stuttgart: Schattauer Verlag; 2011. pp. 317–322. [Google Scholar]
- 7.Swart E, Ihle P, Klug S, Lampert T. Gute Praxis Sekundärdatenanalyse (GPS)-Revision nach grundlegender Überarbeitung. Das Gesundheitswesen. 2008;70 doi: 10.1055/s-2007-1022529. [DOI] [PubMed] [Google Scholar]
- 8.Gaebel W, Zielasek J, Kowitz S, Fritze J. Patienten mit Psychischen Störungen: Oft am Spezialisten vorbei. Dtsch Arztebl. 2011;108(26) [Google Scholar]
- 9.Hauth I, Bergmann F, Deuster A, et al. Positionspapier der DGPPN (Nr7). Psychisch erkrankt: gesundheitspolitische Anforderungen an eine bedarfsgerechte Behandlung im richtigen Umfeld. 24.6.2013. www.dgppn.de/publikationen/stellungnahmen/detailansicht/article/141/positionspap-4.html. (last accessed 26 July 2013) [Google Scholar]
- 10.Leucht S, Burkard T, Henderson J, et al. Physical illness and schizophrenia: a review of the literature. Acta Psychiatr Scand. 2007;116:317–333. doi: 10.1111/j.1600-0447.2007.01095.x. [DOI] [PubMed] [Google Scholar]
- 11.Laursen TM, Munk-Olsen T, Gasse C. Chronic somatic comorbidity and excess mortality due to natural courses in persons with schizophrenia or bipolar affective disorder. PlosONE. 2011;6 doi: 10.1371/journal.pone.0024597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Hert M, Detraux J, Vancampfort D, Yu W, Correll CU. Severe mental illness and diabetes mellitus Type 2. Die Psychiatrie. 2012;3:159–164. [Google Scholar]
- 13.Härter M, Baumeister H, Reuter K, et al. Increased 12-month prevalence rates of mental disorders in patients with chronic somatic diseases. Psychother Psychosom. 2007;76:354–360. doi: 10.1159/000107563. [DOI] [PubMed] [Google Scholar]
- 14.Hassan A, Wobrock T, Falkai P. Somatische Komorbidität bei Schizophrenie. Die Psychiatrie. 2012;3:152–158. [Google Scholar]
- 15.Millar HL. Physical health in the severely mentally ill population. Die Psychiatrie. 2012;3:137–142. [Google Scholar]
- 16.Ungewitter C, Böttger D, El-Jurdi J, et al. Struktur und Kooperation in der Versorgung psychisch Kranker. Nervenarzt. 2013;84:307–314. doi: 10.1007/s00115-011-3433-1. [DOI] [PubMed] [Google Scholar]
- 17.Jacobi F, Klose M, Wittchen HU. Psychische Störungen in der deutschen Allgemeinbevölkerung: Inanspruchnahme von Gesundheitsleistungen und Ausfalltage. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2004;47:736–744. doi: 10.1007/s00103-004-0885-5. [DOI] [PubMed] [Google Scholar]
- 18.Kruse J, Herzog W. Zwischenbericht zum Gutachten „Zur ambulanten psychosomatischen/psychotherapeutischen Versorgung in der kassenärztlichen Versorgung in Deutschland - Formen der Versorgung und ihre Effizienz“. Gießen. http://s255669059.online.de/pdf/Gutachten_Psychosomatik_Zwischenbericht.pdf. 2012 (last accessed 16. October 2013) [Google Scholar]
- 19.Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. European Neuropsychopharmacology. 2011;21:655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 20.Bundespsychotherapeutenkammer. www.bptk.de/fileadmin/user_upload/Publikationen/BPtK-Studien/belastung_moderne_arbeitswelt/Wartezeiten_in_der_Psychotherapie/20110622_BPtK-Studie_Langfassung_Wartezeiten-in-der-Psychotherapie.pdf. Berlin: 2011. BPtK-Studie zu Wartezeiten in der ambulanten psychotherapeutischen Versorgung. (last accessed: 26 July 2013) [Google Scholar]
- 21.Rogausch A, Kapmeyer A, Tenbieg A, Himmel W. Die Rolle des Hausarztes in der ambulanten Schizophreniebehandlung aus Sicht von Patienten. Psychiatr Prax. 2008;35:194–197. doi: 10.1055/s-2007-986286. [DOI] [PubMed] [Google Scholar]
- 22.Linden M, Gothe H, Ormel J. Pathways to care and psychological problems of general practice patients in a „gate keeper“ and an „open access“ health care system: a comparison of Germany and the Netherlands. Soc Psychiatry Psychiatr Epidemiol. 2003;38:690–697. doi: 10.1007/s00127-003-0684-6. [DOI] [PubMed] [Google Scholar]
- 23.Schaffner N, Schimmelmann BG, Niedersteberg A, Schultze-Lutter F. Versorgungswege von erstmanifesten psychotischen Patienten - eine Übersicht internationaler Studien. Fortschr Neurol Psychiatr. 2012;80:72–78. doi: 10.1055/s-0031-1273428. [DOI] [PubMed] [Google Scholar]
- 24.Gaebel W, Kowitz S, Zielasek J. The DGPPN research project on mental healthcare utilization in Germany: inpatient and outpatient treatment of persons with depression by different disciplines. Eur Arch Psychiatr Clin Neurosci. 2012;2:51–55. doi: 10.1007/s00406-012-0363-2. [DOI] [PubMed] [Google Scholar]
- 25.Schneider F, Kratz S, Bermejo I, et al. Insufficient depression treatment in outpatient settings. German Med Sci. 2004 [PMC free article] [PubMed] [Google Scholar]
- 26.Wittchen HU, Pittrow D. Prevalence, recognition and management of depression in primary care in Germany: the Depression 2000 study. Human Psychopharmacol. 2002;17(suppl 1):1–11. doi: 10.1002/hup.398. [DOI] [PubMed] [Google Scholar]
- 27.Jacobi F, Hofler W, Wittchen HU. Prävalenz, Erkennens- und Verschreibungsverhalten bei depressiven Syndromen. Eine bundesdeutsche Hausarztstudie. Nervenarzt. 2002;73:651–658. doi: 10.1007/s00115-002-1299-y. [DOI] [PubMed] [Google Scholar]
- 28.Sielk M, Altiner A, Janssen B, Becker N, de Pilars MP, Abholz HH. Prävalenz und Diagnostik depressiver Störungen in der Allgemeinarztpraxis. Ein kritischer Vergleich zwischen PHQ-D und hausärztlicher Einschätzung. Psychiatr Prax. 2009;36:169–174. doi: 10.1055/s-0028-1090150. [DOI] [PubMed] [Google Scholar]
- 29.Wittchen HU, Jacobi F. Size and burden of mental disorders in Europe—a critical review and appraisal of 27 studies. Eur Neuropsychopharmacol. 2005;15:357–376. doi: 10.1016/j.euroneuro.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 30.Murrey CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020. Global Burden of Disease Study. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 31.Bowles D, Damm O, Greiner W. Gesundheitsbezogene Versorgungsforschung mit GKV-Routinedaten - Grenzen am Beispiel der Prophylaxe venöser Thromboembolien in der Hüft- und Kniegelenkendoprothethik. Gesundh ökon Qual manag. 2011;16:96–107. [Google Scholar]
- 32.Mansky T, Robra BP, Schubert I. Vorhandene Daten besser nutzen. Dtsch Arztebl. 2012;109:A1082–A1085. [Google Scholar]
- e1.Hoffmann F, Glaeske G. Neugebauer EAM. Analyse von Routinedaten. In: Pfaff H, Glaeske F, Schrappe M, editors. Lehrbuch Versorgungsforschung. Systematik - Methodik - Anwendung. Stuttgart: Schattauer Verlag; 2011. pp. 317–322. [Google Scholar]
- e2.Gaebel W, Zielasek J, Kowitz S. Nutzung von Routinedaten für die psychiatrische und psychosomatische Versorgungsforschung. Die Psychiatrie. 2011;8:23–33. [Google Scholar]
- e3.Bestmann A. Datenquellen und Datenqualität der Reha-Statistik-Datenbasis. DRV-Schriften Band 55/2008 [Google Scholar]
- e4.Hartung J, Elpelt B, Klösener KH. Lehr- und Handbuch der angewandten Statistik. München: Oldenbourg Wissenschaftsverlag; 2005. Statistik. [Google Scholar]
- e5.Bortz J. Berlin: Springer Verlag; 1985. Lehrbuch der Statistik für Sozialwissenschaftler; 134 pp. [Google Scholar]
- e6.Bundesamt für Statistik. GKV-Versicherte nach Alter und Wohnort GKV-Statistik KM6 zum. www.bmg.bund.de/fileadmin/redaktion/pdf_statistiken/krankenversicherung/2006-km6-lang-pdf. 2006. Juli. (last accessed 17 October 2013)
- e7.Bundesministerium für Gesundheit. Gesetzliche Krankenversicherung. Mitglieder, mitversicherte Angehörige und Krankenstand. Jahresdurchschnitte. www.bmg.bund.de/fileadmin/redaktion/pdf_statistiken/krankenversicherung/KM1JD2004-pdf-5112.pdf. 1998 bis 2008. (last accessed 17 October 2013)