Abstract
Background: Medical and nursing education lack adequate practical nutrition training to fit the clinical reality that health workers face in their practices. Such a deficit creates health workers with poor nutrition knowledge and child undernutrition management practices. In-service nutrition training can help to fill this gap. However, no systematic review has examined its collective effectiveness. We thus conducted this study to examine the effectiveness of in-service nutrition training on health workers’ nutrition knowledge, counseling skills, and child undernutrition management practices.
Methods: We conducted a literature search on nutrition interventions from PubMed/MEDLINE, CINAHL, EMBASE, ISI Web of Knowledge, and World Health Organization regional databases. The outcome variables were nutrition knowledge, nutrition-counseling skills, and undernutrition management practices of health workers. Due to heterogeneity, we conducted only descriptive analyses.
Results: Out of 3910 retrieved articles, 25 were selected as eligible for the final analysis. A total of 18 studies evaluated health workers’ nutrition knowledge and showed improvement after training. A total of 12 studies with nutrition counseling as the outcome variable also showed improvement among the trained health workers. Sixteen studies evaluated health workers’ child undernutrition management practices. In all such studies, child undernutrition management practices and competence of health workers improved after the nutrition training intervention.
Conclusion: In-service nutrition training improves quality of health workers by rendering them more knowledge and competence to manage nutrition-related conditions, especially child undernutrition. In-service nutrition training interventions can help to fill the gap created by the lack of adequate nutrition training in the existing medical and nursing education system. In this way, steps can be taken toward improving the overall nutritional status of the child population.
Keywords: in-service training, nutritional sciences, health knowledge, counseling, child undernutrition, health personnel
Background
Child undernutrition can be reduced if health workers with adequate nutrition knowledge provide correct, adequate, and frequent nutrition advise to caregivers (1, 2). Across the globe, the quality of health workers’ nutrition knowledge – and, by extension, their counseling skills – has been a concern (3–7). Historically, medical training has lacked adequate and updated nutrition training that is in keeping with the situation and needs on the ground (8–10). As a result, health workers produced from teaching institutions have lacked adequate nutrition knowledge (3, 6). Such health workers may also lack the competence and skills to provide basic nutrition advice to their clients (2, 11). This incompetence, in turn, may be a factor deterring health workers from providing nutrition advice and management to their clients (12).
In-service nutrition training can help to improve health workers’ nutrition knowledge (13–16). This may facilitate positive changes in their attitudes toward nutrition care (17, 18) and thus in their behavior (19–21). As a result, health workers’ skills in management of nutrition-related problems such as child undernutrition, including nutrition-counseling skills (13–15, 19, 22, 23), may improve (24–26).
In practical terms, the process by which the knowledge acquired through nutrition training is translated into management practices may not be linear. However, the outcome of nutrition training can be explained using the conceptual framework of general behavioral theories. Based on the Health Belief Model (27), for example, knowledge or education on a perceived threat or disease is likely to influence behavior change. Untrained health workers may feel incompetent to provide counseling to their clients even when they know or perceive the threat caused by a nutrition problem. When such health workers are trained to recognize threats posed by nutrition-related problems, they are likely to provide appropriate care. In an ideal situation, knowledge can impact practical skills; it can thus change health workers’ behaviors.
Changes in health workers’ nutrition-counseling behavior can be sustained even after training ends. This may be due to the rewards they may receive in the positive results of improving child feeding practices and nutritional status. According to Bandura’s social learning theory, a change can be influenced by being rewarded or punished as a result of one’s actions (27). Health workers’ counseling behavior is more likely to last or recur if the nutrition knowledge received is used to counsel or manage a child with undernutrition so as to yield obvious improvements in the child’s nutritional status.
Evidence is available for the impact of in-service nutrition training on health workers’ nutrition knowledge, nutrition-counseling skills, and management of child undernutrition. However, no systematic review has summarized such evidence toward effecting policy change. A few review articles have demonstrated the importance of nutrition training for health workers (7). Other reviews have shown the effect of health workers’ counseling of caregivers on feeding practices including dietary diversity, feeding frequency, and energy intake (28), complementary feeding, and children’s nutritional status (1, 29, 30). However, we could not find any systematic review on the impact of nutrition training for health workers on their own knowledge, attitudes, and child undernutrition management practices. Therefore the objective of this systematic review was to evaluate the impact of nutrition training interventions among health workers on their nutrition knowledge, nutrition counseling, and child undernutrition management practices.
Methods
The population, intervention, comparator, outcome (PICO) question to be addressed in this study was framed as follows: what is the effectiveness of nutrition training of health workers on their nutrition knowledge, nutrition counseling, and undernutrition management practices among children at risk of or suffering from undernutrition as compared to those who did not receive such training? For this review, we included studies with nutrition training interventions.
We defined nutrition training for health workers as any form of in-service training given to health workers and designed for continuing professional development (CPD), continuous medical education (CME), research purposes, or as part of a health project or program. We used a World Health Organization (WHO) and International Labor Organization (ILO) definitions of health worker to select health cadres as the population of interest (31, 32). Such health cadres included doctors, nurses, midwives, mid-level providers, dieticians, nutritionists, and pharmacists.
Three outcome variables were assessed in this review: health worker’s nutrition knowledge, nutrition counseling and/or general counseling skills, and management skills for child undernutrition. Health worker’s nutrition knowledge was measured using a standard scale or pre-made set of questions to test knowledge specific to the training given. We regarded nutrition counseling as any specific advice given by a health worker to caregivers on nutrition, feeding characteristics, dietary composition, or food intake. Such advice might have followed evaluation of the patient’s nutritional status, feeding behavior, dietary composition, or training on poor nutrition conditions. Depending on the availability of the data, we included assessment of quality and frequency of counseling to assess both skills and counseling acts of trained health workers.
We defined management practices for undernutrition as activities health workers perform toward management of poor nutritional status. Depending on data availability, this might include assessment of undernutrition using anthropometric scores, assessment of micronutrient deficiency, treatment of associated conditions, treatment of undernutrition by prescription of supplements, or monitoring by growth charts, among other methods.
The protocol for this systematic review was registered at PROSPERO http://www.crd.york.ac.uk/PROSPERO on February 6, 2013. The registration number for this review is CDR42013003800. It is available at http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42013003800.
Inclusion Criteria
Based on the nature of the intervention and the outcome of interest, we included studies with nutrition training interventions. As for the study design, we included studies conducted as RCTs, cluster RCTs, quasi-experimental studies, and pre–post-intervention longitudinal studies with or without comparison groups.
Exclusion Criteria
We excluded any study where in the structure and/or quality of the training intervention provided to health workers was unclear from the description provided. We also excluded studies involving cadres of health workers outside the scope of the WHO that included community health volunteers, medical and nursing students, medical interns, and peers trained to provide specified health services. Non-interventional studies were also excluded from this review. This included cross-sectional studies, case reports, and non-interventional qualitative studies.
Data Sources for Existing Reviews
We first searched for similar reviews or registered review protocols to avoid duplication and redundancy according to the standard review guidelines of the Center for Review and Dissemination (CRD) and Cochrane (33, 34). To this end, we searched such protocols listed in the Cochrane library and Cochrane Database of Systematic Reviews (CDSR). We used a similar approach to search other important databases for systematic reviews, including the Database of Abstracts of Reviews of Effects (DARE), the Educational Resources and Information Center (ERIC), the Campbell Library of Systematic Reviews, and the National Institute for Health and Clinical Excellence (NICE). Two independent researchers conducted the search for existing protocols and similar review articles.
Evidence Search Strategy
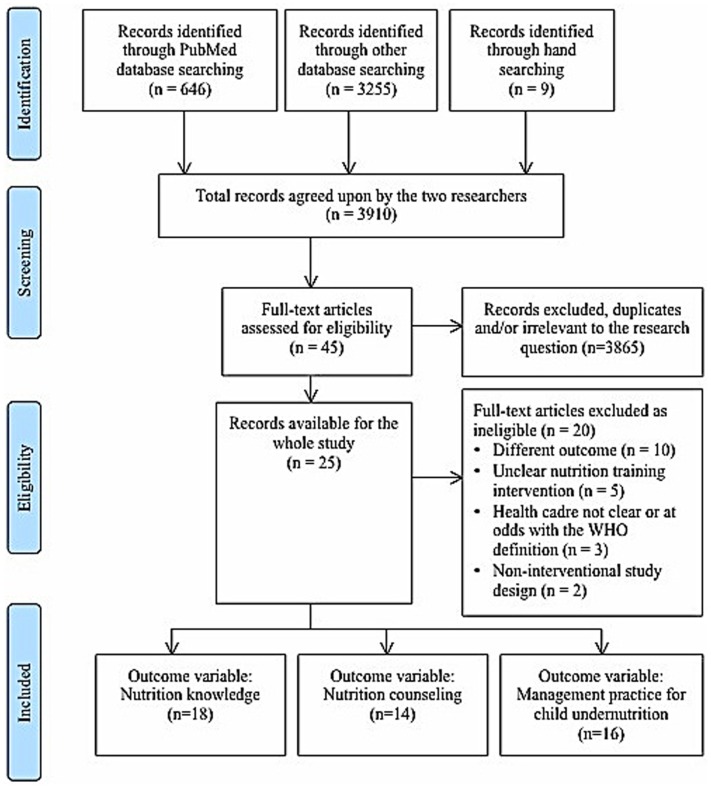
Two independent researchers conducted a literature search based on the published review protocol. The search was conducted in five medical databases: PubMed/Medline, CINAHL, EMBASE, ISI Web of Knowledge, and WHO regional databases. The search was limited to a 15-year-publication period (1997–2012), to ensure that we obtain enough evidence. Also, most of standard nutrition training interventions became more common after the publication of Integrated Management of Childhood Illnesses (IMCI) by WHO in 1997. For the PubMed/Medline database, we followed the search strategy outlined in the CDR register. Similar key words were then used to conduct searches in other selected databases. In order to ensure that we captured most of the relevant articles, we also conducted a hand search using references from key identified articles and archives of a journal with similar specialty – the Journal of Human Resources for Health. Figure 1 shows the results of searching and data management procedures according to the PRISMA check list (Table 1) (35).
Figure 1.
Diagram of information flow through phases of systematic review.
Table 1.
PRISMA 2009 checklist.
| Section/topic | No. | Checklist item | Reported on page No. |
|---|---|---|---|
| TITLE | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both | 1 |
| ABSTRACT | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number | 2 |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known | 3 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS) | 4 |
| METHODS | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g., Web address), and, if available, provide registration information including registration number | 4 |
| Eligibility criteria | 6 | Specify study characteristics (e.g., PICOS, length of follow-up) and report characteristics (e.g., years considered, language, publication status) used as criteria for eligibility, giving rationale | 4–5 |
| Information sources | 7 | Describe all information sources (e.g., databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched | 5–6 |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated | 6 |
| Study selection | 9 | State the process for selecting studies (i.e., screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis) | 4–6 |
| Data collection process | 10 | Describe method of data extraction from reports (e.g., piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators | 5 |
| Data items | 11 | List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made | 5–6 |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis | 6, Tables 2–3 |
| Summary measures | 13 | State the principal summary measures (e.g., risk ratio, difference in means) | 5–6 |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g., I2) for each meta-analysis | 5–6 |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g., publication bias, selective reporting within studies) | 6 |
| Additional analyses | 16 | Describe methods of additional analyses (e.g., sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified | NA |
| RESULTS | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram | 6, Figure 1 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g., study size, PICOS, follow-up period) and provide the citations | Table 4 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see item 12) | Tables 2–3 |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot | Tables 5–7 |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency | NA |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see item 15) | Tables 2–3 |
| Additional analysis | 23 | Give results of additional analyses, if done (e.g., sensitivity or subgroup analyses, meta-regression [see item 16]) | NA |
| DISCUSSION | |||
| Summary of evidence | 24 | Summarize the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g., healthcare providers, users, and policy makers) | 8–10 |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g., risk of bias), and at review-level (e.g., incomplete retrieval of identified research, reporting bias) | 9–10 |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research | 10 |
| FUNDING | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (e.g., supply of data); role of funders for the systematic review | 10 |
From Ref. (36).
A total of 3910 articles were retrieved from various sources. Of these, 646 studies were from PubMed/Medline. We retrieved a total of 3255 from other databases: 341 from CINAHL, 1543 from EMBASE, 1249 from ISI Web of Knowledge, and 122 from WHO Regional databases. A total of nine studies were additionally obtained based on hand searches and review of specific journal databases.
On an initial screening of articles, we excluded a total of 3865 abstracts and articles due to duplication between PubMed/Medline and other databases and those, which were irrelevant to the research question. Of the 45 studies remaining, we further excluded 20 studies following a full-text assessment of eligibility. The reasons for exclusion were as follows: different outcome variable to that of interest (n = 10), unclear or different intervention (n = 5), unclear or different population (n = 3), and different study design (n = 2).
Analysis Strategy
Also shown in Figure 1 is the distribution of the 25 studies included for final analysis according to outcome variables. A single study could incorporate more than one outcome variable of interest. A total of 18 studies had health workers’ nutrition knowledge as an outcome variable, 12 studies had health worker’s nutrition counseling or general counseling skills as an outcome variable, and 16 studies had health worker’s management practice as an outcome variable.
Of the 25 identified studies, six used a cluster RCT design (13–15, 19, 22, 23). One study had a controlled non-randomized trial design (16). A total of 18 studies, meanwhile, used a pre–post-intervention evaluation and quasi-experimental design with or without a control group (17, 20, 21, 24, 37–49).
The duration of the intervention, population characteristics, and measurement of outcome variables differed across each of the included studies. Study design also differed from one study to another though they all aimed generally at a nutrition training intervention for health workers (Table 4). To avoid the obvious risk of heterogeneity, we did not conduct a meta-analysis. Instead, we sought to write a narrative summary to describe our results and stratified such description according to the outcome of interest.
Table 4.
General description of studies included in the review.
| Author | Study design | Nutrition training intervention | Outcome of interest |
|---|---|---|---|
| Zaman et al. (22), Pakistan | Cluster RCT | Nutrition-counseling training using IMCI’s “counsel the mother” module for five and a half days. It included infant feeding knowledge and practice sessions for the development of communication and counseling skills | Communication skills |
| Nutrition counseling | |||
| Nutrition management/practice | |||
| Bassichetto and Réa (13), Brazil | Cluster RCT | WHO’s “infant and young child feeding counseling: an integrated course.” The training includes 8 h of practical sessions. Out of 34 sessions, 8 were dedicated to breastfeeding, 6 to HIV and infant and young child feeding, 7 to complementary feeding, 10 to counseling, and 4 to general themes, making a total of 40 h | Nutrition knowledge |
| Nutrition counseling | |||
| Undernutrition management/performance | |||
| Moore et al. (14), UK | Cluster RCT | A nutrition training program was delivered to six intervention practices (health facilities). Emphasis of the training was on increasing motivation to improve quality of dietary consultations and providing them with practical skills adapted from behavior models. Included components in the 7.5-h training were patients’ assessment, education, and goal setting in issues of public health importance including drinking | Nutrition knowledge Counseling |
| Pelto et al. (19), Brazil | Cluster RCT | Physicians from the intervention group received a 20-h training in a program derived from the IMCI nutrition-counseling module. After training, they provided care to caregiver/child pairs who attended their centers | Counseling |
| Practice: communication skills | |||
| Santos et al. (15), Brazil | Cluster RCT | Fourteen doctors received a 20-h nutrition-counseling training using IMCI’s “counsel the mother” and “management of the sick young infant” modules. Based on local adaptation of IMCI feeding guidelines, the key feeding recommendations identified were as follows: increase breast and complementary feeding frequency, provide animal protein and micronutrient-rich foods, add oil to the food, and increase dietary diversity. Of the 20 h of training, 40% was used for practical sessions in a health center | Nutrition knowledge Nutrition counseling: undernutrition management skills/practice |
| Penny et al. (23), Peru | Cluster RCT | Interventions aimed to raise the nutrition profile of the health facility and to integrate nutrition services into existing child health programs though training and provision of simple messages to caregivers. Training included demonstration of preparation of complementary foods and child’s age-specific group sessions for their caregivers. The intervention also included training for health care workers to improve anthropometry skills. An accreditation system was also introduced for institutional change | Nutrition counseling Others: health seeking behavior |
| Cattaneo and Buzzetti (16), Italy | Controlled non-randomized trial | An 18-h UNICEF “Breastfeeding, management, and health proportion in baby-friendly hospitals” course along with a 2-h counseling session from the WHO’s breast-feeding counseling course were implemented | Nutrition knowledge Hospital performance |
| Palermo et al. (37), Australia | Pre–post-intervention study | Thirty-two dieticians were allocated to three intervention groups: two face-to-face groups and one rural video-linked group. The intervention involved a mentoring circle of experienced nutritionists and community-based dieticians. Each participant attended six 2-h sessions every 6 weeks for a 7-month intervention period | Nutrition knowledge and competence |
| Lindorff-Larsen et al. (17), Denmark | Pre–post-intervention study | A follow-up study was conducted in 2004 and compared to a baseline study in 1997. Nutrition training and use of nutrition guidelines were being introduced and used between the two study intervals. Details of such training were not further elaborated | Nutrition knowledge |
| Puoane et al. (38), South Africa | Pre–post-intervention study (with a qualitative design) | A 5-day course developed by the University of West Cape involved practice sessions, group work, role-plays, action plan development, key messages, and question and answer sessions. The course followed the principle of care set out by WHO for managing severe malnutrition. A total of 66 nurses from 11 referral hospitals underwent this course | Health workers’ practice Attitudes |
| Hamer et al. (39), Gambia | Pre–post-intervention study | Nutrition training for nurses was conducted using the IMCI training manual, “assess and classify sick children aged 2 months to 5 years.” Training materials were provided to nurses a week prior to training. The training included both theoretical and practical components toward assessing children with and without wasting and/or edema admitted to the hospital | Nutrition knowledge Undernutrition management/practice |
| Edwards and Wyles (40), UK | Pre–post-intervention study | A total of 24 1-h training sessions were held, reaching 189 staff. Each session consisted of factual information, a brainstorming session about what a pregnant woman eat, and a nutrition game involving calculation of daily requirement for folic acid | Nutrition knowledge Health workers’ practice |
| O’Mahony et al. (41), UK | Pre–post-intervention study | Nutrition training was delivered to nurse participants. It also included the use of the Malnutrition Universal Screening Tool (MUST) | Nutrition knowledge Health workers’ practice |
| Hillenbrand and Larsen (20), US | Pre–post-intervention study | Forty-nine pediatric residents participated in a four-part education series about breastfeeding delivered over four consecutive days. The education intervention was internally designed using additional inputs from lactation experts and fellow pediatricians. The training included lectures, discussions, role-playing, and group exercises | Nutrition knowledge Nutrition counseling Counseling and practice |
| Olsson et al. (42), Sweden | Pre–post-intervention study | Nutrition education for nurses was conducted for 3 months. It was based on the use of nutrition assessments including energy intake, clinical complications of inadequate energy intake, hospital food energy content, patients energy requirements, weighing patients and its necessity, reasons for weight loss during illness, and fluid management | Nutrition knowledge Health workers’ practice |
| Pedersen et al. (43), Denmark | Pre–post-intervention study | Nutrition training was conducted for nurses. It included five modules of 3–4 days duration using the theory of planned change. The training incorporated basic nutrition education elements such as risk assessment, consequences of malnutrition, and assessment of needs and responsibility | Health workers’ practice |
| Gance-Cleverland et al. (21), US | Pre–post-intervention study | Thirty-five nurse practitioners received an intensive 4-h Healthy Eating and Activity Together Clinical Practice Guideline (HEAT CPG) training session | Nutrition knowledge Nutrition counseling |
| Bjerrum et al. (18), Denmark | Pre–post-intervention study | Sixteen nurses participated in a special training program on nutrition. It was based on experimental theories and included five modules spanning 3–4 days, combining theories of planned change and nutrition issues | Nutrition knowledge |
| Kennelly et al. (45), Ireland | Pre–post-intervention study | Seven general practitioners participated in the nutrition education program. A community dietician used a standardized presentation to conduct the program. The content of training included information on causes of malnutrition, effects of malnutrition, use of the MUST tool, practical dietary advice for patients with poor appetite, and evidence supporting the use of oral nutrition supplements (ONS) | Nutrition counseling Health workers’ practice |
| Kennelly et al. (44), Ireland | Pre–post-intervention study | An educational program incorporating the MUST training was implemented in 8 of 10 eligible primary practices, 7 private nursing homes, and 2 health centers. The training program was designed based on consultations with health professional groups, clinical guidelines from expert bodies, and current evidence for ONS use in community settings | Nutrition knowledge Nutrition counseling |
| Simoes et al. (46), Ethiopia | Pre–post-intervention study | A 9-day course using the pre-tested version of the IMCI course was provided to six clinic nurses. The training modules included assessment and classification of the sick child, treatment of the child, counseling the mother, and follow-up. Other modules included practical sessions in the clinic | Nutrition knowledge Nutrition counseling Health workers’ practice |
| Davies-Adetugbo and Adebawa (47), Nigeria | Pre–post-intervention study | A 1-day community mobilization with 6 h of training on breastfeeding and child survival was conducted for health workers and mothers. The training was designed to include the importance of breast-feeding, exclusive breastfeeding, lactation maintenance, expressed breast milk, practical demonstration of attachment, suckling, expression of milk, and cup feeding. An intensive 2-day training was then conducted for health workers using a WHO/UNICEF 18-h breastfeeding course manual. Training included practical, role-playing, and theory sessions | Nutrition and breastfeeding knowledge |
| Newes-Adeyi et al. (48), US | Pre–post-intervention study | A total of 35 women, infants, and children (WIC) staff underwent a 1-day intensive training program to improve their growth monitoring counseling and management of nutrition-related problems. The training included lectures, case studies, discussions, small group work, and role-plays | Nutrition counseling |
| Stark et al. (49), US | Quasi-experimental design | A 6-week online professional development program for nutrition and health practitioners course was delivered to the intervention group. It was based on the PRECEDE-PROCEED health program planning framework involving assessment of underlying factors for a health problem and strategizing the intervention | Nutrition knowledge and skills |
| Charlton et al. (24), Zambia | Pre–post-intervention study | Eight out of 16 health care workers received the Growth Monitoring and Promotion (GMP) training. Details of the training including duration and contents were not described | Nutrition knowledge Nutrition practice |
Risk of Bias
We assessed risk of bias (RoB) for each cluster RCT and non-randomized studies (Tables 2 and 3). We used the Cochrane RoB tool (34), to examine five types of RoB for randomized trials. These included selection, performance, attrition, detection, and reporting biases. Of the six cluster RCTs, only one study (13), had a high risk of selection and performance bias.
Table 2.
Risk of bias assessment cluster RCTs Cluster RCTs.
| Selection bias: allocation concealment | Performance bias: blinding of participants and personnel | Detection bias: blinding of outcome assessment | Attrition bias: incomplete outcome data | Reporting bias: selective reporting | |
|---|---|---|---|---|---|
| Zaman et al. (22) |  |
 |
 |
 |
 |
| Bassichetto and Réa (13) |  |
 |
 |
 |
 |
| Moore et al. (14) |  |
 |
 |
 |
 |
| Pelto et al. (19) |  |
 |
 |
 |
 |
| Santos et al. (15) |  |
 |
 |
 |
 |
| Penny et al. (23) |  |
 |
 |
 |
 |
+ Indicates low risk of bias, − indicates high risk of bias, and ? indicate unclear risk of bias.
Table 3.
Risk of Bias (ROB) and methodological quality for non-randomized studies.
| Author | Reporting (10) | External validity (3) | Internal validity-bias (7) | Internal validity-(confounding) selection bias (6) | Power (1) |
|---|---|---|---|---|---|
| Palermo et al. (37) | 8 | 3 | 6 | 4 | No |
| Lindorff-Larsen et al. (17) | 8 | 3 | 6 | 4 | No |
| Puoane et al. (38) | 5 | 2 | 4 | 2 | No |
| Hamer et al. (39) | 8 | 1 | 6 | 3 | Yes |
| Edwards and Wyles (40) | 6 | 2 | 5 | 1 | Yes |
| O’Mahony et al. (41) | 8 | 2 | 6 | 4 | No |
| Hillenbrand and Larsen (20) | 9 | 2 | 6 | 4 | No |
| Olsson et al. (42) | 8 | 3 | 6 | 4 | Yes |
| Pedersen et al. (43) | 9 | 2 | 6 | 4 | No |
| Gance-Cleverland et al. (21) | 8 | 3 | 4 | 4 | No |
| Bjerrum et al. (18) | 5 | 2 | 4 | 2 | No |
| Kennelly et al. (45) | 9 | 3 | 6 | 4 | Yes |
| Kennelly et al. (44) | 9 | 3 | 6 | 4 | Yes |
| Simoes et al. (46) | 9 | 2 | 5 | 4 | No |
| Davies-Adetugbo and Adebawa (47) | 9 | 3 | 6 | 4 | Yes |
| Newes-Adeyi et al. (48) | 8 | 2 | 6 | 4 | No |
| Stark et al. (49) | 9 | 3 | 7 | 2 | Yes |
| Charlton et al. (24) | 9 | 3 | 6 | 4 | Yes |
To assess quality and RoB for non-randomized studies, we used the Downs and Black scoring system (50). This tool has 27 checklists and is used to examine RoB for observation studies. We used the tool to examine reporting bias, external validity, internal validity-bias, internal validity- (confounding) selection bias, and power of the study. Generally, the included non-randomized studies had good external validity and internal validity. However, 10 out of 18 of non-randomized studies included had low or unknown power to detect a clinical important effect of the intervention. This is due to the nature of the intervention and methods used to recruit their participants. Most of nutrition training used all available health workers, selected non-randomly, and without prior or unspecified sample size calculations.
Results
General description of the included studies
Out of 3910 retrieved studies, a total of 25 studies were included in this systematic review. These studies were conducted in countries from Africa, North and South America, Europe, Asia, and Australia (Table 4). The selected studies were also conducted in varied socio-economic levels, from least to most developed countries. Among the included studies, six were cluster RCTs, one was a controlled non-randomized trial, 17 were pre–post-intervention evaluations, and one was a quasi-experimental design study. The included health worker cadres ranged from specialists in pediatric care to general practitioners (GPs), nurses, midwives and obstetricians, nutritionists, dieticians, and mid-level providers.
Nutrition training spanned varying forms and duration. The most common standard used was the IMCI model, based on the “counsel the mother” and “nutrition-counseling” modules (15, 19, 22, 39, 46). Other training frameworks included the WHO standard counseling training modules (13, 16, 38, 47), tailored nutrition training using the Malnutrition Universal Screening Tool (MUST) (41, 44, 45), and nutrition training prepared specifically to suit the specific situation or context. Across training types, the lowest training duration was 4 h (21), while the longest training duration was 6 weeks of online training (49).
The main outcome of interest from the selected studies are presented in Table 4 according to our objectives. Health workers’ nutrition knowledge after the nutrition training intervention was reported in a total of 18 studies: 3 RCTs (13–15), 1 controlled non-randomized trial (16), and 14 pre–post-intervention studies (17, 18, 20, 21, 37, 39–42, 44, 46, 47). Counseling and communication skills of health workers who underwent the nutrition intervention were reported in 12 studies: 6 RCTs (13–15, 19, 22, 23) and 6 pre–post-intervention studies (20, 21, 44–46, 48). A total of 16 studies reported health workers’ management skills for child undernutrition after undergoing nutrition training. Among such studies, 3 were RCTs (13, 15, 22), 1 was a controlled non-randomized trial (16), and 14 were pre–post-intervention evaluation studies (24, 37–46, 49).
Effectiveness of the intervention to improve health workers’ nutrition knowledge (a narrative summary)
Table 5 summarizes the 18 reviewed studies that included nutrition knowledge as the outcome variable. Among these studies, three used a cluster RCT design and were conducted in Brazil (13, 15) and the UK (14). A higher proportion of doctors who received the nutrition training intervention in the Brazilian studies had high post-training nutrition knowledge compared to doctors in the control group. In the UK-based RCT among GPs, nutrition training did not significantly change health workers’ nutrition knowledge (14). However, GPs in the intervention group were 30% more likely to believe that their nutrition knowledge was up-to-date compared to their counterparts in the control group (P = 0.001).
Table 5.
The effectiveness of nutrition training to improve nutrition knowledge of health care workers.
| Author | Study design | Health cadre | Nutrition training intervention | Comparison | Outcome: nutrition knowledge |
|---|---|---|---|---|---|
| Bassichetto and Réa (13), Brazil | RCT: 31 professionals received intervention and 28 were the control | Pediatricians and nutritionists | WHO’s “infant and young child feeding counseling: an integrated course.” The training includes 8 h of practical sessions. Out of 34 sessions, 8 were dedicated to breastfeeding, 6 to HIV and infant and young child feeding, 7 to complementary feeding, 10 to counseling, and 4 to general themes | Doctors and nutritionists in control group did not receive the training intervention. | Proportion of knowledge increase was more among HCWs in IG [e.g., Breastfeeding – IG-79.3%, CG-37% (P = 0.004); HIV and IYCF – IG-48.3%, CG-18.5% (P = 0.049); Complementary feeding – IG-69.0%, CG-37.0% (P = 0.012)] |
| Moore et al. (14), UK | Cluster RCT-paired cluster randomized trial with pre- and post-intervention assessment | 12 General practitioners | A training program was delivered to six intervention practices. Emphasis was on increasing motivation to improve quality of dietary consultations and providing practical skills adapted from behavior models. A 7.5-h training included patients’ assessment, education, and goal setting in issues of public health importance including drinking | Six control practices did not receive nutrition training | IG-trained practitioners were 30% (95% CI 12–50, P = 0.001) more likely to believe that their knowledge was up-to-date than practitioners in IG. There was no statistical significance difference in actual knowledge between IG and CG |
| Santos et al. (15), Brazil | RCT of 28 government health centers | 28 Medical doctors | A total of 14 doctors in the intervention group received a 20-h nutrition-counseling training and practice using IMCI’s “counsel the mother” and “management of the sick young infant” modules. The key recommendations identified were as follows: increase breast and complementary feeding frequency, provide animal protein and micronutrient-rich foods, add oil to the food, and increase dietary diversity | 14 Doctors recruited for CG did not receive training | Doctors from IG correctly answered 83% (95% CI 65–100) of 77 questions on practical situations in the IMCI guidelines compared to 68% (95% CI 48–88) in the CG (P = 0.02) |
| Cattaneo and Buzzetti (16), Italy | Controlled non-randomized study | Nurses, midwives, obstetricians, and physicians | An 18-h UNICEF “breastfeeding, management, and health proportion in baby-friendly hospitals” course along with a 2-h counseling session from the WHO breast-feeding counseling course were implemented | Post-training evaluation | In Group 1, nutrition knowledge went up from a mean score of 0.41 to 0.66 to 0.72. In Group 2, nutrition knowledge went from 0.53 to 0.53 to 0.75 |
| Palermo et al. (37), Australia | Pre–post-intervention study | Nutritionists and dieticians | A total of 32 dieticians were allocated to three IGs: two face-to-face groups and one rural video-linked group. The intervention involved a mentoring circle of experienced nutritionists and community-based dieticians. Each participant attended six 2-h sessions every 6 weeks for a 7-month intervention period | Pre–post-intervention comparison (qualitative and quantitative) | Reported competency score increased post-training/mentoring. An increase in post-intervention measures was also reported: [69.1(13.8) to 79.3(12.1), P < 0.001] |
| Lindorff-Larsen et al. (17), Denmark | Pre–post-intervention study | Doctors and nurses | A follow-up study was conducted in 2004 and compared to a baseline study in 1997. Nutrition training and guidelines were being introduced and used between the two study intervals. Details of such training were not further elaborated | A cross-sectional study, post-trainings and post-guideline application | About two-thirds of doctors and nurses expressed that their education nutrition was sufficient at post-intervention. Significantly fewer health workers lacked methods to identify undernutrition (P < 0.001) and difficult-to-identify patients in need of nutrition support (P < 0.001) at post-intervention |
| Hamer et al. (39), Gambia | Pre–post-intervention study | Registered nurses and auxiliary nurses | Nutrition training for nurses was conducted using the IMCI training manual, “assess and classify sick children aged 2 months to 5 years.” It included both theoretical and practical components of assessing children with and without wasting and edema | Post-training evaluation | Nurses showed good knowledge and performance after the completion of training |
| Edwards and Wyles (40), UK | Pre–post-intervention study | Midwives, physicians, dieticians, and nurses | A total of 24 1-h training sessions were held for 189 staff. Each session consisted of factual and brainstorming sessions about what a pregnant woman eats, and a nutrition calculation of daily requirement for folic acid | Post-training evaluation | Health workers’ nutrition knowledge improved post-training |
| O’Mahony et al. (41), UK | Pre–post-intervention study | Nursing staff | Nutrition training was delivered to nurse participants on the use of the Malnutrition Universal Screening Tool (MUST) | Post-training evaluation | A non-significant difference in post-training nutrition knowledge was observed [Mean (SD) knowledge score 21(6.7) vs. 23(6.2)]. A significant difference was observed in sub-analyses by bands. Nurses were more aware that malnutrition was a significant problem for the National Health Service post-training (P < 0.027) |
| Hillenbrand and Larsen (20), US | Pre–post-intervention study | Pediatric residents | A total of 49 pediatric residents participated in a four-part education series about breastfeeding over 4 consecutive days. It included lectures, discussions, role-playing, and group exercises. The education intervention was internally designed by the authors using inputs from lactation experts and fellow pediatricians | Post-training evaluation | Mean composite knowledge score was 80% post intervention compared to 69% pre-intervention, representing an 11% increase (P < 0.01) |
| Olsson et al. (42), Sweden | Pre–post-intervention study | Nurses | Nutrition education for nurses was conducted for 3 months. It was based on the use of nutrition assessment including energy intake, clinical complications of inadequate energy intake, hospital food energy, patients’ energy requirements, weighing patients and its necessity, reasons for weight loss during illness, and fluid management | Post-training evaluation | 69% Of nurses could calculate a patient’s energy requirement post-training compared to 24% pre-training (P < 0.01). Compared to pre-training, more nurses knew the energy content of hospital food (61 vs. 45%, P < 0.05), knew how to handle enteral infusion equipment (55 vs. 6%, P < 0.01), and found it easy to assess patients’ energy needs (56 vs. 24%, P < 0.01) |
| Gance-Cleverland et al. (21), US | Pre–post-intervention study | Nurse practitioners | A total of 35 nurse practitioners received an intensive 4-h Healthy Eating and Activity Together Clinical Practice Guideline (HEAT CPG) training session | Post-training evaluation | Nutrition knowledge post training improved, including on assessment of growth (P < 0.001), assessment of family history (P < 0.001), and assessment of physical activity (P < 0.001). Practitioners’ nutrition recommendation knowledge also improved post-training compared to pre-training |
| Bjerrum et al. (18), Denmark | Pre–post-intervention study | Nurses | A total of 16 nurses participated in a special training program on nutrition. It was based on experimental theories. A total of five modules lasting 3–4 days were included. They combined theories of planned change and nutrition issues | Post-training evaluation | A short-duration training program enhanced nurses’ awareness of nutrition care, management through assessment and monitoring, their management roles, and approach to clinical nutrition |
| Kennelly et al. (44), Ireland | Pre–post-intervention study | General practitioners (GPs) and nurse practitioners | An educational program incorporating Malnutrition Universal Screening Tool (MUST) training was implemented in 8 of 10 eligible primary practices, seven private nursing homes, and two health centers. The training program was designed based on consultations with health professional groups, clinical guidelines from expert bodies, and current evidence for oral nutrition supplementation (ONS) use in community settings | Post-training evaluation | Nutrition knowledge improved across three evaluation points (P < 0.05). For specific groups, a significant improvement in knowledge score was also observed among general practitioners (P < 0.001) and nurses (P < 0.001) |
| Simoes et al. (46), Ethiopia | Pre–post-intervention study | Clinic nurses | Six clinic nurses received a 9-day course using the pre-tested version of the IMCI course. The training modules included assessment and classification of a sick child, treatment of the child, counseling the mother, and follow-up. Other modules included practical sessions in the clinic | Post-training evaluation | After training, nurses could recognize visible severe wasting with a 67% sensitivity and 99% specify; conjunctiva pallor for anemia at 45% sensitivity and 94% specificity; and bipedal edema with 69% sensitivity and 98% specificity |
| Davies-Adetugbo and Adebawa (47), Nigeria | Pre–post-intervention study | Community health extension workers | A 6-h training on breastfeeding and child survival was conducted for health workers and mothers. The training included the importance of breast-feeding, exclusive breastfeeding, lactation maintenance, expressed breast milk, practical demonstration of attachment, suckling, expression of milk, and cup feeding. An intensive 2-day training was then conducted for health workers using a WHO/UNICEF 18-h breastfeeding course manual. Training included practical, role-playing, and theory sessions | Post-training evaluation | Trained health workers had a significantly higher aggregate knowledge score compared to their untrained counterparts [9.4(9.1–9.7) vs. 7.6(6.6–8.6), P < 0.001] |
| Stark et al. (49), US | Quasi-experimental design using intervention and delayed intervention comparison group | Nutrition and health professionals | An online professional development program for nutrition and health practitioners course was given to the intervention group for 6 weeks. It was based on the PRECEDE-PROCEED health program planning framework involving assessment of underlying factors for a health problem and strategizing the intervention | Delayed intervention control group | Compared to the control group, the intervention group reported significant positive changes (P < 0.01) on knowledge and skills scores |
| Charlton et al. (24), Zambia | Pre–post-intervention study | Health workers for growth monitoring and promotion | Eight out of 16 HCWs received the growth monitoring and promotion training | Post-training evaluation | Compared to untrained HCWs, trained HCWs could correctly define growth monitoring and promotion (P < 0.001) |
IG, intervention group; CG, control group; HCWs, health care workers.
In an Italian controlled non-randomized trial with a comparison group (16), the mean nutrition knowledge score of nurses, midwives, and doctors increased from 0.41 to 0.72 in Group 1 and from 0.53 to 0.75 in Group 2 after the nutrition training. Compared to the delayed intervention control group, health workers in the intervention group registered a significant change in knowledge and skills (P < 0.01) in a quasi-experimental study conducted in the US.
Fourteen studies were conducted using a pre–post-intervention design in Australia (37), Denmark (17, 18), Gambia (39), UK (41), US (20, 21, 49), Sweden (42), Ireland (44), Ethiopia (46), Nigeria (47), and Zambia (24). In all of these studies, health workers’ nutrition knowledge increased after nutrition training.
Effectiveness of intervention to improve nutrition-counseling skills of health workers (a narrative summary)
Table 6 shows the result of the 12 reviewed studies with nutrition counseling as an outcome variable following nutrition training of health workers. Of these studies, six were cluster RCTs and three were conducted in Brazil among doctors and pediatricians (13, 15, 19). Across all three studies, a significantly higher proportion of doctors in the intervention group had better post-training counseling skills and performed more nutrition counseling compared to the respective control group. Physicians undergoing the training intervention also showed higher mean communication skill scores compared to untrained physicians (P < 0.01) (19). In a Pakistani cluster RCT among lady health visitors (LHVs) working at a health facility as mid-level providers, 82% of participants in the intervention group registered improved post-training communication skills compared to 51% in the control group (P = 0.015). In this study, a higher proportion of trained LHVs reported increased counseling skills compared to their counterparts. GPs with nutrition training in the UK study (14), meanwhile, were 30% more likely to provide dietary advice that was completely appropriate (P = 0.01). In Peru (23), twice as many mothers in the intervention group received post-partum nutrition advice compared to their control group counterparts following the nutrition training intervention for their health workers (P = 0.02).
Table 6.
Effectiveness of nutrition training to improve nutrition counseling and counseling skills of caregivers.
| Author | Study design | Health cadre | Intervention | Comparison | Outcome: nutrition counseling |
|---|---|---|---|---|---|
| Zaman et al. (22), Pakistan | Cluster RCT: 18 health centers were assigned to IG and a similar number to CG | Lady health visitors (MLVs) | Nutrition-counseling training using IMCI’s “counsel the mother” module for five and a half days. It included infant feeding knowledge and practice sessions to develop communication and counseling skills | Health centers of the control group without counseling training for health workers | Counseling: asking about feeding practices and paying attention to answers: IG-50%, CG-25%, P = 0.056; praising mothers for positive action: IG-37%, CG-8%, P = 0.006. Appropriate recommendations to specific changes with explanation: IG-29%, CG-4%, P = 0.01 |
| Communication skills: IG-82%, CG-51%, P = 0.015 | |||||
| Bassichetto and Réa (13), Brazil | RCT: 31 professionals received intervention and 28 were recruited as a control group | Pediatricians and nutritionists | WHO’s “Infant and young child feeding counseling: an integrated course” was administered. The training includes 8 h of practical sessions. Out of 34 sessions, 8 were dedicated to breastfeeding, 6 to HIV and infant and young child feeding, 7 to complementary feeding, 10 to counseling, and 4 to general themes | Participants recruited for the control group did not receive the training intervention | Counseling: IG-51.7%, CG-22.2% (P = 0.004) |
| Moore et al. (14), UK | Cluster RCT-paired cluster randomized trial with pre- and post-intervention evaluation | General practitioners | A training program was delivered to six intervention practices. Emphasis was on increasing motivation to improve quality of dietary consultations and providing practical skills adapted from behavior models. A 7.5-h training included patients’ assessment, education, and goal setting in issues of public health importance including drinking | A total of six control practices did not receive nutrition training | Counseling: trained practitioners were 30% (95% CI 7–53, P = 0.01) more likely to provide dietary advise that was completely appropriate |
| Pelto et al. (19), Brazil | Cluster RCT of 28 municipal health centers | Doctors | Physicians from the intervention group received a 20-h training in a program derived from the IMCI nutrition-counseling module. After training, they provided care to caregiver/child pairs attending their centers | Physicians in the control group received a clinical refresher course but not on nutrition counseling | Counseling: trained providers engaged more in nutrition counseling [only 9(24%) consultations of IG participants did not include advice compared to 14 (43%) among CG participants: P < 0.013]; gave 81 messages compared to 20 of untrained ones (P < 0.002); gave more message specific to foods, preparations, and feeding practices compared to untrained ones (P < 0.01) |
| Communication skills: mean communication skills score of trained physicians was 3.94 (SD 1.68) vs. 1.38 (SD 1.02) for untrained ones (P < 0.01) | |||||
| Santos et al. (15), Brazil | RCT of 28 government health centers | 28 Medical doctors | A total of 14 doctors of the IG received a 20-h nutrition-counseling training and practice using IMCI’s “counsel the mother” and “management of the sick young infant” modules. The key recommendations identified were as follows: increase breast and complementary feeding frequency, give animal protein and micronutrient-rich foods, add oil to the food, and increase dietary diversity | 14 doctors recruited for the control group did not receive the training | Counseling: 83% of mothers in IG compared to 49% of mothers in CG received nutrition counseling (P < 0.001) |
| Penny et al. (23), Peru | Cluster RCT of 12 health facilities serving periurban areas | Health workers in selected health facilities | The intervention included training for HCWs to improve anthropometry skills. An accreditation system was also introduced for institutional change. Also it included demonstration of preparation of complementary foods and child’s age-specific group sessions for caregivers | HCWs and caregivers of CG did not receive the training intervention | Counseling: twice as many mothers in IG received nutrition advice after birth compared to those in CG (52 vs. 24%, P = 0.02). Greater impacts on counseling were observed at 4 and 18 months post-intervention (P < 0.002) |
| Hillenbrand and Larsen (20), US | Pre–post-intervention study | Pediatric residents | A total of 49 pediatric residents participated in a four-part education series about breastfeeding over four consecutive days. The training included lectures, discussions, role-playing, and group exercises. The education intervention was designed using additional inputs from lactation experts and fellow pediatricians | Post-training evaluation | Counseling: residents showed an increased knowledge in advising mothers concerning low milk supply (P = 0.045), infections including mastitis (P = 0.002), or abscess (P < 0.001) |
| Counseling and practice: residents showed significant increases in counseling on signs of breast-feeding adequacy (P = 0.012) and managing lactation problems correctly (P = 0.004) | |||||
| Gance-Cleverland et al. (21), US | Pre–post-intervention study | Nurse practitioners | A total of 35 nurse practitioners received an intensive 4-h Healthy Eating and Activity Together Clinical Practice Guideline (HEAT CPG) training session | Post-training evaluation | Counseling: participants reported a significant improvement in behavior modification techniques (P < 0.001) and practitioners’ counseling (P < 0.001) |
| Kennelly et al. (45), Ireland | Pre–post-intervention study | General practitioners-doctors | Seven GPs participated in the nutrition education program. The content of training included causes of malnutrition, effects of malnutrition, the use of the Malnutrition Universal Screening Tool (MUST), practical dietary advice for patients with poor appetite, and evidence supporting the use of oral nutrition supplements (ONS) | Post-training evaluation | Counseling: basic dietary advice provided by a health professional increased significantly post-training (90 vs. 26%, P < 0.001) |
| Kennelly et al. (44), Ireland | Pre–post-intervention study | General practitioners (GP) and nurse practitioners | An educational program incorporating the MUST training was implemented in 8 of 10 eligible primary practices, seven private nursing homes, and two health centers. The training program was designed based on consultations with health professional groups, clinical guidelines from expert bodies, and current evidence for ONS use | Post-training evaluation | Counseling: about 80% of HCWs reported always providing nutrition advice to patients |
| Simoes et al. (46), Ethiopia | Pre–post-intervention study | Clinic nurses | A 9-day course using the pre-tested version of the IMCI course was provided to six clinic nurses. The training modules included assessment and classification of sick child, treatment of the child, counseling the mother, and follow-up. Other modules included practical sessions in the clinic | Post-training evaluation | Counseling: trained health workers provided feeding advice rated as “good” by 78%, “fair” at 18% and “poor” at 4% |
| Newes-Adeyi et al. (48), US | Pre–post-intervention study | Health workers of a special nutrition program | A total of 35 health workers underwent a 1-day intensive training program to improve their growth monitoring counseling and management of nutrition-related problems. The training included lectures, case studies, discussions, small group work, and role-plays | Post-training evaluation | Counseling: compared to pre-training, there was a significant change in elicitation (P < 0.001) and negotiation proficiency (P = 0.07). The level of engagement in discussing provider suggestions for follow-up strategies increased from 1.8 to 2.3 (P < 0.01) and the overall responsiveness level increased from a mean of 2.4–2.8 (P < 0.07) |
IG, intervention group; CG, control group; HCWs, health care workers.
A total of six studies using pre–post-intervention evaluation of nutrition training of health workers reported nutrition-counseling skills as an outcome variable. These studies were conducted in the US (20, 21, 48), Ireland (44, 45), and Ethiopia (46). In all six studies, nutrition and general counseling skills of health workers improved after nutrition training.
Effectiveness of intervention to improve health workers’ management practices for child undernutrition (a narrative summary)
Table 7 summarizes the results of the 16 reviewed studies reporting management of undernutrition and management practices as an outcome variables following the nutrition training intervention. Within these studies, two of the three cluster RCTs were conducted in Brazil among medical doctors, pediatricians, and nutritionists (13, 15). Doctors in the intervention group were more likely to report improved post-intervention practices in managing child undernutrition compared to their counterparts. In the Pakistani study, trained LHVs were more likely to plot children’s weights, discuss appropriate foods with caregivers, and check mothers’ understanding of imparted nutrition knowledge compared to their counterparts in the control group. In an Italian controlled non-randomized trial (16), all hospitals improved their compliance with WHO’s “Ten Steps to Successful Breastfeeding” after undergoing the WHO baby-friendly hospital and counseling course.
Table 7.
Effectiveness of nutrition training to improve nutrition management practices and competence of health workers.
| Author | Study design | Health cadre | Intervention | Comparison | Outcome: nutrition management or practice |
|---|---|---|---|---|---|
| Zaman et al. (22), Pakistan | Cluster RCT: 18 health centers were assigned IG and a similar number were assigned to CG | Lady health visitors | Nutrition-counseling training using IMCI’s “counsel the mother” module for five and a half days. It included infant feeding knowledge and practice sessions for development of communication and counseling skills | HCWs of the CG received no counseling training | Practice: HCWs in the intervention group were more likely to plot the weight of a child, discuss foods appropriate to the child, and check if mothers understood information provided |
| Bassichetto and Réa (13), Brazil | RCT: 31 professionals recruited to IG and 28 for CG | Pediatricians and nutritionists | WHO’s “infant and young child feeding counseling: an integrated course” was implemented. The training includes 8 h of practical sessions. Out of 34 sessions, 8 were dedicated to breastfeeding, 6 to HIV and infant and young child feeding, 7 to complementary feeding, 10 to counseling, and 4 to general themes | HCWs in the CG did not receive the training intervention | Performance: IG participants improved their dietary anamnesis during consultations after intervention (P < 0.001) |
| Santos et al. (15), Brazil | RCT of 28 government health centers assigned to either IG or CG | 28 Medical doctors | A total of 14 doctors of IG received a 20-h nutrition-counseling training and practice using IMCI’s “counsel the mother” and “management of the sick young infant” modules. The key recommendations identified were as follows: increase breast and complementary feeding frequency, provide animal protein and micronutrient-rich foods, add oil to the food, and increase dietary diversity | Doctors in the CG did not receive counseling training | Practice: doctors from IG were more likely to assess child’s complementary feeding, assess breast-feeding, use good communication skills, and use and provide mothers with a card compared to CG |
| Cattaneo and Buzzetti (16), Italy | Controlled non-randomized | Nurses, midwives, obstetricians, and physicians | An 18-h UNICEF “breastfeeding, management, and health proportion in baby-friendly hospitals” course along with a 2-h counseling session from the WHO breast-feeding counseling course was implemented | Post-training evaluation | Performance: all hospitals improved their compliance with the WHO 10 steps to successful breastfeeding |
| Palermo et al. (37), Australia | Pre–post-intervention study | Nutritionists and dieticians | A total of 32 dieticians were allocated to three intervention groups: two face-to-face groups and one rural video-linked group. The intervention involved a mentoring circle of experienced nutritionists and community-based dieticians. Each participant attended six 2-h sessions every 6 weeks for a 7-month intervention period | Pre–post-intervention comparison (qualitative and quantitative) | Nutrition competence: reported competency scores increased post training/mentoring. An increase in post-intervention measures was also observed: [69.1(13.8) to 79.3(12.1), P < 0.001] |
| Puoane et al. (38), South Africa | Pre–post-intervention study (with a qualitative design) | Nurses | A 5-days course developed by the University of West Cape was administered. It involved practice sessions, group work, role-plays, development of an action plan, key messages, and question and answer sessions. The course followed the principle of care set out by WHO for managing severe malnutrition | Post-intervention (training) | Practice: in-patient care for malnutrition management improved after the training. This included adequate follow-up on the 10 steps to management of malnutrition |
| Hamer et al. (39), Gambia | Pre–post-intervention study | Registered and auxiliary nurses | Nutrition training for nurses was conducted using the IMCI training manual, “Assess and classify sick children aged 2 months to 5 years.” It included both theoretical and practical components of assessing children with and without wasting and/or edema admitted to the hospital | Post-training evaluation | Practice: in assessing undernutrition, nurses showed a 56% sensitivity, 95% specificity, and 56% positive predictive value (PPV) |
| Edwards and Wyles (40), UK | Pre–post-intervention study | Midwives, physicians, dieticians, and nurses | A total of 24 1-h training sessions were held, reaching 189 staff. Each session consisted of factual information, a brainstorming session about what a pregnant woman eats, and a nutrition game involving calculation of daily requirement for folic acid | Post-training evaluation | Practice: in a nutrition game, a high average intake of folic acid was observed in the chosen food items. It ranged from 244 to 500 μg compared to only 219 μg shown in average in census data on the same population |
| O’Mahony et al. (41), UK | Pre–post-intervention study | Nursing staff | Nutrition training was conducted with nurse participants. It also included the use of the Malnutrition Universal Screening Tool (MUST) | Post-training evaluation | Practice: 94% of nurses weighed patients on admission post-training compared to 74% before (P < 0.001) |
| Olsson et al. (42), Sweden | Pre–post-intervention study | Nurses | Nutrition education for nurses was conducted for 3 months. Training was based on the use of nutrition assessments including energy intake, clinical complication of inadequate energy intake, hospital food energy content, patients’ energy requirements, weighing patients and its necessity, reasons for weight loss during illness, and fluid management | Post-training evaluation | Practice: compared to pre-training, during post-training, nurses were more likely to use food forms to document food intake (P < 0.01) |
| Pedersen et al. (43), Denmark | Pre–post-intervention study | Nurses | Nutrition training was conducted for nurses. It included five modules spanning 3–4 days using the theory of planned change. The intervention involved basic nutrition education elements such as risk assessment, consequences of malnutrition, and assessment of needs and responsibility | Post-training evaluation | Practice: after the training, more patients reported eating difficulties to staff (P = 0.01), none reported not receiving help in cutting their food (P = 0.014), fewer had difficulty in chewing (P = 0.01), and fewer reported not receiving food they did not order (P = 0.01) |
| Kennelly et al. (45), Ireland | Pre–post-intervention study | General practitioners-doctors | Seven general practitioners participated in the nutrition education program. A community dietician used a standardized presentation to conduct the program. The content of training included information on causes of malnutrition, effects of malnutrition, the use of MUST, practical dietary advise to patients with poor appetite, and evidence supporting the use of oral nutrition supplements (ONS) | Post-training evaluation | Practice: about 62% completed a nutrition screening tool (MUST) on referral to a community dietician compared to 0% pre-intervention (P < 0.001). A greater proportion of patients with high risk of malnutrition were prescribed ONS post-training compared to pre-training (88% vs. 37%, P < 0.001) |
| Kennelly et al. (44), Ireland | Pre–post-intervention study | General practitioners (GP) and nurse practitioners | An educational program incorporating MUST training was implemented in 8 of 10 eligible primary practices, 7 private nursing homes, and 2 health centers. The training program was designed based on consultations with health professional groups, clinical guidelines from expert bodies, and current evidence for ONS use in community settings | Post-training evaluation | Practice: management of malnutrition improved post training. About 69% of HCWs weighed patients more frequently and 80% reported on the usefulness of MUST |
| Simoes et al. (46), Ethiopia | Pre–post-intervention study | Clinic nurses | A 9-day course using the pre-tested version of the IMCI course was provided to six clinic nurses. The training modules included assessment and classification of a sick child, treatment of the child, counseling the mother, and follow-up. Other modules included practical sessions in the clinic | Post-training evaluation | Practice: compared to pediatricians, the trained nurses could diagnose malnutrition and anemia classified as severe or some malnutrition at a sensitivity of 85% and specificity of 96% |
| Stark et al. (49), US | Quasi-experimental design | Nutrition and health professionals | An online professional development program for nutrition and health practitioners course was given to the intervention group for 6 weeks. It was based on the PRECEDE-PROCEED health program planning framework involving assessing underlying factors for a health problem and strategizing the intervention | Delayed intervention control group | Nutrition management skills: compared to the control group, the intervention group reported positive changes (P < 0.01) on knowledge and skills scores |
| Charlton et al. (24), Zambia | Pre–post-intervention study | Health workers of growth monitoring and promotion | Eight out of 16 HCWs received the Growth Monitoring and Promotion (GMP) training. Details of the training including duration and contents were not explained | Post-training evaluation | Practice: trained HCWs could correctly interpret growth cards and complete the under-five card compared to their untrained counterparts (P < 0.05) |
IG, intervention group; CG, control group; HCWs, health care workers.
Nutrition and health professionals in the quasi-experimental design study in the US exhibited better nutrition management skills after the 6-week online nutrition training (49). Compared to health workers in the delayed intervention control group, those in the intervention group registered significant positive changes on knowledge and skills scores (P < 0.01).
Eleven pre–post-intervention studies on nutrition training of health workers were conducted in Australia (37), South Africa (38), Gambia (39), UK (40, 41), Sweden (42), Denmark (43), Ireland (44, 45), Ethiopia (46), US, and Zambia (24). In all these studies, management practices and competence of health workers improved after the intervention compared to pre-nutrition training intervention levels.
Discussion
This is the first systematic review to examine the effectiveness of in-service nutrition training to improve health workers’ nutrition knowledge, nutrition counseling, and undernutrition management practices. In this review, we reviewed a total of 25 studies reporting on nutrition training interventions. Across all three of our outcome variables, significant post-intervention improvements were reported. First, in-service nutrition training improved health workers’ nutrition knowledge. Second, the counseling skills and competence of health workers were also improved after in-service nutrition training. Third, the training intervention improved child undernutrition management practices of participating health workers.
A total of 18 studies, including five with a cluster RCT design, showed significant post-nutrition training improvements in health workers’ nutrition knowledge. These studies were conducted in areas of varying social and economic levels and geographic characteristics. Health workers might also have been exposed to nutrition education during their college training (8). However, previous studies have indicated that such training is inadequate or not in keeping with the clinical reality encountered in practice (9, 10). Lack of such knowledge might also cause them to refrain from providing nutrition counseling and care to their clients (8). Sometimes, due to lack of adequate nutrition knowledge, doctors feel that it is the duty of nurses or other cadres below them to provide nutrition counseling and care. To improve knowledge of such health workers, it is important to expose them to in-service nutrition training tailored to their environment, context, and health cadre (9). This will help to boost their competence and confidence in management of nutrition-related conditions including undernutrition.
In this systematic review, a total of 12 studies, including six cluster RCTs, showed a significant improvement in counseling skills among health workers with in-service nutrition training. Nutrition training would thus seem to be effective in improving health workers’ nutrition knowledge. Nutritionally informed health workers may be more confident to address nutrition-related conditions in their patients (51). Such health workers may be better equipped to provide appropriate advice and counseling to their clients. The prevailing attitude toward nutrition counseling among medical doctors and pediatricians that such functions are not within their job description might also change after nutrition training. In this way, such trained health workers would be more likely to provide nutrition counseling (52). In line with the health belief model, nutrition knowledge provided to the health workers through nutrition training is more likely to influence counseling behavior (27). Further, according to Bandura’s social learning theory, such behavior or attitude change is mediated through cognitive processes and thus is learned through imitating and observing the actions of others (27). Accordingly, the reward that health workers can gain from their nutrition-counseling actions, such as better nutritional status or feeding practices in those they treat, may reinforce their counseling actions, thus making it a permanent habit. In this way, the quality of health workers with regard to nutrition counseling might be expected to improve.
Our review showed that health workers’ undernutrition management practices improved when they received in-service nutrition training. A total of 16 intervention studies, including three cluster RCTs, showed a significant improvement in management practices for child undernutrition after nutrition training. Barriers to effective management of child undernutrition include lack of nutrition knowledge and counseling skills among health providers (12). Such barriers can be ameliorated when health workers receive appropriate and tailored in-service nutrition training suited to their context and cadre.
Findings from this review should be carefully considered in the context of two primary limitations. First, the results are not based on meta-analysis to calculate the overall effect size of the intervention for each outcome variables. This was due to variations in the study designs and measurements used for outcome variables, and to differences in the competence, experience, and cadres of participating health workers. Such variations could have resulted in high heterogeneity. Hence, instead of meta-analyses, we explained each study separately in a narrative summary stratified by outcome variable. Although we did not pool our results, individual studies showed a significant effect of nutrition interventions on outcome variables.
Second, the included studies differed in the intervention’s length and content. This might have caused differences in the measured outcome variables. However, most of the studies used standard nutrition training frameworks for health workers including the IMCI nutrition-counseling training module, breast-feeding counseling training modules by both WHO and UNICEF, MUST training modules, and other comparable training based on formative research. Despite such differences, each study showed a significant improvement in one or more of the outcome variables.
Despite its limitation, findings thus presented may help decision makers to plan and conduct in-service nutrition training for health workers, an important building block toward building a strong foundation for any health system. This review is the continuation of series papers on the effectiveness of nutrition training of health workers. It is the first systematic review on the effectiveness of nutrition training for health workers on their nutrition knowledge, nutrition counseling, and undernutrition management skills. The other paper in the series found that, nutrition training of health workers improved feeding frequency, energy intake, and dietary diversity of children aged 6 months to 2 years (28).
In conclusion, in-service nutrition training of health workers improves their nutrition knowledge, nutrition and general counseling skills, and undernutrition management skills. Such nutrition training within the context of their practice is of paramount importance due to inadequate nutrition training in the health workers’ mainstream medical and nursing education. In-service nutrition training can take different forms such as compulsory CME, nutrition seminars, workshops, or non-compulsory continuing professional education CPD. Whatever form it takes, nutrition training has the potential to improve the quality of health workers, making them more confident and competent in this key area and thus contributing to positive changes in population nutrition.
Authors’ Contributions
Bruno F. Sunguya conceived the research questions, designed the study, participated in the literature review and analyses, and prepared the first draft. Krishna C. Poudel refined the research question and the first draft. Linda B. Mlunde contributed to the study design, participated in the literature review, and helped to prepare the first draft. David P. Urassa revised the protocol. Junko Yasuoka participated in the preparation of the first draft and revisions. Masamine Jimba reviewed the study protocol and manuscript, and approved the submission. All authors read and approved the final version of the manuscript for submission.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This study was funded by the Ministry of Health, Labor, and Welfare of Japan (Research Grant No. H24-chikyukibo-Ippan-008). The funders did not influence the review process or interpretation of findings.
References
- 1.Imdad A, Yakoob MY, Bhutta ZA. Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health (2011) 11(Suppl 3):S25. 10.1186/1471-2458-11-S3-S25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williams A, Pinnington LL. Nurses’ knowledge of current guidelines for infant feeding and weaning. J Hum Nutr Diet (2003) 16(2):73–80 10.1046/j.1365-277X.2003.00430.x [DOI] [PubMed] [Google Scholar]
- 3.Mowe M, Bosaeus I, Rasmussen H, Kondrup J, Unosson M, Rothenberg E, et al. Insufficient nutritional knowledge among health care workers? Clin Nutr (2008) 27(2):196–202 10.1016/j.clnu.2007.10.014 [DOI] [PubMed] [Google Scholar]
- 4.Ryan VC, Rao LO, Rekers G. Nutritional practices, knowledge, and attitudes of psychiatric healthcare professionals: unexpected results. Psychiatr Hosp (1990) 21(3):125–7 [PubMed] [Google Scholar]
- 5.Hu SP, Wu MY, Liu JF. Nutrition knowledge, attitude and practice among primary care physicians in Taiwan. J Am Coll Nutr (1997) 16(5):439–42 10.1080/07315724.1997.10718711 [DOI] [PubMed] [Google Scholar]
- 6.Kgaphola M, Wodarski L, Garrison M. Nutrition knowledge of clinic nurses in Lebowa, South Africa: implications for nutrition services delivery. J Hum Nutr Diet (1997) 10(5):295–303 10.1046/j.1365-277X.1997.00063.x [DOI] [Google Scholar]
- 7.Calderon TA. Nutrition education training of health workers and other field staff to support chronically deprived communities. Public Health Nutr (2001) 4(6A):1421–4 10.1079/PHN2001231 [DOI] [PubMed] [Google Scholar]
- 8.Adams K, Lindell K, Kohlmeier M, Zeisel S. Status of nutrition education in medical schools. Am J Clin Nutr (2006) 83(4):941S–4S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zimmerman M, Kretchmer N. Isn’t time to teach medical students nutrition. Am J Clin Nutr (1993) 58(6):828–9 [DOI] [PubMed] [Google Scholar]
- 10.Pearson TA, Stone EJ, Grundy SM, McBride PE, Van Horn L, Tobin BW, et al. Translation of nutritional sciences into medical education: the Nutrition Academic Award Program. Am J Clin Nutr (2001) 74(2):164–70 [DOI] [PubMed] [Google Scholar]
- 11.Fletcher A, Carey E. Knowledge, attitudes and practices in the provision of nutritional care. Br J Nurs (2011) 20(10):615–6 [DOI] [PubMed] [Google Scholar]
- 12.Leslie FC, Thomas S. Competent to care. Are all doctors competent in nutrition? Proc Nutr Soc (2009) 68(3):296–9 10.1017/S0029665109001293 [DOI] [PubMed] [Google Scholar]
- 13.Bassichetto KC, Réa MF. Infant and young child feeding counseling: an intervention study. J Pediatr (Rio J) (2008) 84(1):75–82 10.2223/JPED.1750 [DOI] [PubMed] [Google Scholar]
- 14.Moore H, Greenwood D, Gill T, Waine C, Soutter J, Adamson A. A cluster randomised trial to evaluate a nutrition training programme. Br J Gen Pract (2003) 53(489):271–7 [PMC free article] [PubMed] [Google Scholar]
- 15.Santos I, Victora CG, Martines J, Gonçalves H, Gigante DP, Valle NJ, et al. Nutrition counseling increases weight gain among Brazilian children. J Nutr (2001) 131(11):2866–73 [DOI] [PubMed] [Google Scholar]
- 16.Cattaneo A, Buzzetti R. Effect on rates of breast feeding of training for the baby friendly hospital initiative. BMJ (2001) 323(7325):1358–62 10.1136/bmj.323.7325.1358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lindorff-Larsen K, Højgaard Rasmussen H, Kondrup J, Staun M, Ladefoged K, Group SN. Management and perception of hospital undernutrition-a positive change among Danish doctors and nurses. Clin Nutr (2007) 26(3):371–8 10.1016/j.clnu.2007.01.006 [DOI] [PubMed] [Google Scholar]
- 18.Bjerrum M, Tewes M, Pedersen P. Nurses’ self-reported knowledge about and attitude to nutrition – before and after a training programme. Scand J Caring Sci (2012) 26(1):81–9 10.1111/j.1471-6712.2011.00906.x [DOI] [PubMed] [Google Scholar]
- 19.Pelto GH, Santos I, Gonçalves H, Victora C, Martines J, Habicht JP. Nutrition counseling training changes physician behavior and improves caregiver knowledge acquisition. J Nutr (2004) 134(2):357–62 [DOI] [PubMed] [Google Scholar]
- 20.Hillenbrand KM, Larsen PG. Effect of an educational intervention about breastfeeding on the knowledge, confidence, and behaviors of pediatric resident physicians. Pediatrics (2002) 110(5):e59. 10.1542/peds.110.5.e59 [DOI] [PubMed] [Google Scholar]
- 21.Gance-Cleveland B, Sidora-Arcoleo K, Keesing H, Gottesman MM, Brady M. Changes in nurse practitioners’ knowledge and behaviors following brief training on the healthy eating and activity together (HEAT) guidelines. J Pediatr Health Care (2009) 23(4):222–30 10.1016/j.pedhc.2008.03.002 [DOI] [PubMed] [Google Scholar]
- 22.Zaman S, Ashraf RN, Martines J. Training in complementary feeding counselling of healthcare workers and its influence on maternal behaviours and child growth: a cluster-randomized controlled trial in Lahore, Pakistan. J Health Popul Nutr (2008) 26(2):210–22 [PMC free article] [PubMed] [Google Scholar]
- 23.Penny ME, Creed-Kanashiro HM, Robert RC, Narro MR, Caulfield LE, Black RE. Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: a cluster-randomised controlled trial. Lancet (2005) 365(9474):1863–72 10.1016/S0140-6736(05)66426-4 [DOI] [PubMed] [Google Scholar]
- 24.Charlton KE, Kawana BM, Hendricks MK. An assessment of the effectiveness of growth monitoring and promotion practices in the Lusaka district of Zambia. Nutrition (2009) 25(10):1035–46 10.1016/j.nut.2009.03.008 [DOI] [PubMed] [Google Scholar]
- 25.Robert RC, Gittelsohn J, Creed-Kanashiro HM, Penny ME, Caulfield LE, Narro MR, et al. Process evaluation determines the pathway of success for a health center-delivered, nutrition education intervention for infants in Trujillo, Peru. J Nutr (2006) 136(3):634–41 [DOI] [PubMed] [Google Scholar]
- 26.Robert RC, Gittelsohn J, Creed-Kanashiro HM, Penny ME, Caulfield LE, Narro MR, et al. Implementation examined in a health center-delivered, educational intervention that improved infant growth in Trujillo, Peru: successes and challenges. Health Educ Res (2007) 22(3):318–31 10.1093/her/cyl078 [DOI] [PubMed] [Google Scholar]
- 27.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q (1988) 15(2):175–83 10.1177/109019818801500203 [DOI] [PubMed] [Google Scholar]
- 28.Sunguya BF, Poudel KC, Mlunde LB, Shakya P, Urassa DP, Jimba M, et al. Effectiveness of nutrition training of health workers toward improving caregivers’ feeding practices for children aged six months to two years: a systematic review. Nutr J (2013) 12:66. 10.1186/1475-2891-12-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shi L, Zhang J. Recent evidence of the effectiveness of educational interventions for improving complementary feeding practices in developing countries. J Trop Pediatr (2011) 57(2):91–8 10.1093/tropej/fmq053 [DOI] [PubMed] [Google Scholar]
- 30.Dewey KG, Adu-Afarwuah S. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Matern Child Nutr (2008) 4(Suppl 1):24–85 10.1111/j.1740-8709.2007.00124.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gupta N, Maliqi B, França A, Nyonator F, Pate MA, Sanders D, et al. Human resources for maternal, newborn and child health: from measurement and planning to performance for improved health outcomes. Hum Resour Health (2011) 9(1):16. 10.1186/1478-4491-9-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.ILO International Standard Classification of Occupations: ISCO-08. Geneva: International Labour Organization; (2010). [Google Scholar]
- 33.Akers J, Aguiar-Ibanez R, Sari A, Beynon S, Booth A, Burch J, et al. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. New York: CRD, University of York; (2009). [Google Scholar]
- 34.Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.6 [Updated September 2006]. Chichester: John Wiley & Sons LTD; (2009). [Google Scholar]
- 35.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol (2009) 62(10):1006–12 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 36.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group, X Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med (2009) 6:e1000097. 10.1371/journal.pmed1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palermo C, Hughes R, McCall L. An evaluation of a public health nutrition workforce development intervention for the nutrition and dietetics workforce. J Hum Nutr Diet (2010) 23(3):244–53 10.1111/j.1365-277X.2010.01069.x [DOI] [PubMed] [Google Scholar]
- 38.Puoane T, Sanders D, Ashworth A, Ngumbela M. Training nurses to save lives of malnourished children. Curationis (2006) 29(1):73–8 10.4102/curationis.v29i1.1055 [DOI] [PubMed] [Google Scholar]
- 39.Hamer C, Kvatum K, Jeffries D, Allen S. Detection of severe protein-energy malnutrition by nurses in The Gambia. Arch Dis Child (2004) 89(2):181–4 10.1136/adc.2002.022715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Edwards L, Wyles D. The folic acid message – can training make a difference? J Hum Nutr Diet (1999) 12(4):317–26 10.1046/j.1365-277x.1999.00170.x [DOI] [Google Scholar]
- 41.O’Mahony S, Hutchinson J, McConnell A, Mathieson H, McCarthy H. A pilot study of the effect of a nutrition education programme on the nutrition knowledge and practice of nurses. J Hum Nutr Diet (2011) 24:300. 10.1111/j.1365-277X.2011.01175_30.x [DOI] [Google Scholar]
- 42.Olsson U, Bergbom-Engberg I, Ahs M. Evaluating nurses’ knowledge and patients energy intake after intervention. Clin Nurse Spec (1998) 12(6):217–25 10.1097/00002800-199811000-00005 [DOI] [PubMed] [Google Scholar]
- 43.Pedersen PU, Tewes M, Bjerrum M. Implementing nutritional guidelines – the effect of systematic training for nurse nutrition practitioners. Scand J Caring Sci (2012) 26(1):178–85 10.1111/j.1471-6712.2011.00912.x [DOI] [PubMed] [Google Scholar]
- 44.Kennelly S, Kennedy NP, Rughoobur GF, Slattery CG, Sugrue S. An evaluation of a community dietetics intervention on the management of malnutrition for healthcare professionals. J Hum Nutr Diet (2010) 23(6):567–74 10.1111/j.1365-277X.2010.01111.x [DOI] [PubMed] [Google Scholar]
- 45.Kennelly S, Kennedy NP, Corish CA, Flanagan-Rughoobur G, Glennon-Slattery C, Sugrue S. Sustained benefits of a community dietetics intervention designed to improve oral nutritional supplement prescribing practices. J Hum Nutr Diet (2011) 24(5):496–504 10.1111/j.1365-277X.2011.01197.x [DOI] [PubMed] [Google Scholar]
- 46.Simoes EA, Desta T, Tessema T, Gerbresellassie T, Dagnew M, Gove S. Performance of health workers after training in integrated management of childhood illness in Gondar, Ethiopia. Bull World Health Organ (1997) 75(Suppl 1):43–53 [PMC free article] [PubMed] [Google Scholar]
- 47.Davies-Adetugbo AA, Adebawa HA. The Ife South Breastfeeding Project: training community health extension workers to promote and manage breastfeeding in rural communities. Bull World Health Organ (1997) 75(4):323–32 [PMC free article] [PubMed] [Google Scholar]
- 48.Newes-Adeyi G, Helitzer DL, Roter D, Caulfield LE. Improving client-provider communication: evaluation of a training program for women, infants and children (WIC) professionals in New York state. Patient Educ Couns (2004) 55(2):210–7 10.1016/j.pec.2003.05.001 [DOI] [PubMed] [Google Scholar]
- 49.Stark CM, Graham-Kiefer ML, Devine CM, Dollahite JS, Olson CM. Online course increases nutrition professionals’ knowledge, skills, and self-efficacy in using an ecological approach to prevent childhood obesity. J Nutr Educ Behav (2011) 43(5):316–22 10.1016/j.jneb.2011.01.010 [DOI] [PubMed] [Google Scholar]
- 50.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health (1998) 52(6):377–84 10.1136/jech.52.6.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Moore H, Adamson AJ, Gill T, Waine C. Nutrition and the health care agenda: a primary care perspective. Fam Pract (2000) 17(2):197–202 10.1093/fampra/17.2.197 [DOI] [PubMed] [Google Scholar]
- 52.Mihalynuk TV, Scott CS, Coombs JB. Self-reported nutrition proficiency is positively correlated with the perceived quality of nutrition training of family physicians in Washington State. Am J Clin Nutr (2003) 77(5):1330–6 [DOI] [PubMed] [Google Scholar]