Sir,
We would like to thank Bibeau et al (2013) for their constructive comment on our article. We acknowledge that the question raised is of crucial interest and, as the evaluation of infarct-like necrosis (ILN) was not planned in our analyses, we went back to our samples in order to investigate it.
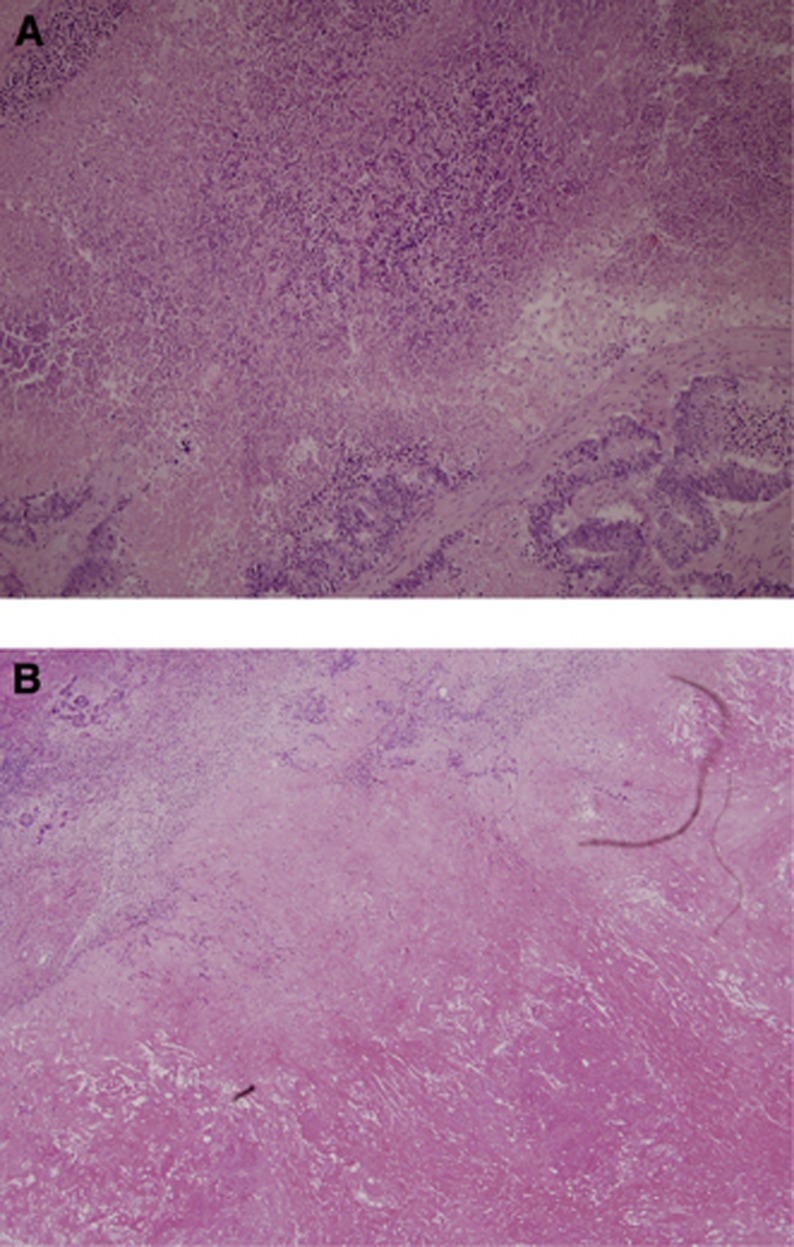
We adopted the definition of ILN previously proposed (Chang et al, 2012) and we found 24 (37%) out of 65 patients showing ILN, characterised by large confluent areas of eosinophilic cytoplasmic remnants, located centrally within a lesion and surrounded by a rim of fibrosis with foamy macrophages (Figure 1). Infarct-like necrosis was observed in 1 (5%) out of 28 patients in the control group, in 4 (27%) out of 18 in the chemotherapy group and in 19 (83%) out of 24 in the bevacizumab group (P<0.0001). The ‘bevacizumab-related effect' previously described was also confirmed in our study (bevacizumab group vs chemotherapy group, P=0.0009; Table 1).
Figure 1.
Examples of usual necrosis (A) and infarct-like necrosis (B).
Table 1. Frequency of infarct-like necrosis in colorectal liver metastases according to treatment.
| Bevacizumab group, N=24 | Chemotherapy group, N=18 | |
|---|---|---|
| Presence of ILN |
19 (83%)a |
4 (27%)b |
| Lack of ILN | 4 (17%)a | 11 (73%)b |
Abbreviation: ILN=infarct-like necrosis.
One patient not evaluable.
Three patients not evaluable; P=0.0009.
In our samples, patients showing a pathologic response according to the classification proposed by Blazer et al (2008) were more likely to present ILN in comparison to patients showing no pathologic response: ILN was present in 71% of patients showing tumour regression grade (TRG) 1-2-3 vs 29% of patients with TRG 4–5 (P=0.0008). These data strengthen the observation that ILN should be regarded as a particular feature of pathologic response induced by preoperative treatments.
Exploratory outcome analyses showed no differences in terms of progression-free survival according to the presence of ILN both among all treated patients (HR=0.59, 95% CI:0.25–1.36; P=0.21) and in the bevacizumab group (HR=0.42, 95% CI:0.06–1.77; P=0.19). Nevertheless, such analyses in our cohort are affected by the relatively small sample size.
In conclusion, we definitely agree with the proposal from Bibeau et al (2013) to include the evaluation of ILN in future studies assessing pathologic response of colorectal liver metastases to preoperative treatments.
References
- Bibeau F, Gil H, Castan F, Boissière-Michot F. Comment on ‘Histopathologic evaluation of liver metastases from colorectal cancer in patients treated with FOLFOXIRI plus bevacizumab'. Br J Cancer. 2013;109 (12:3129–3130. doi: 10.1038/bjc.2013.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blazer DG, 3rd, Kishi Y, Maru DM, Kopetz S, Chun YS, Overman MJ, Fogelman D, Eng C, Chang DZ, Wang H, Zorzi D, Ribero D, Ellis LM, Glover KY, Wolff RA, Curley SA, Abdalla EK, Vauthey JN. Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. J Clin Oncol. 2008;26:5344–5351. doi: 10.1200/JCO.2008.17.5299. [DOI] [PubMed] [Google Scholar]
- Chang HH, Leeper WR, Chan G, Quan D, Driman DK. Infarct-like necrosis: a distinct form of necrosis seen in colorectal carcinoma liver metastases treated with perioperative chemotherapy. Am J Surg Pathol. 2012;36:570–576. doi: 10.1097/PAS.0b013e31824057e7. [DOI] [PubMed] [Google Scholar]