Abstract
INTRODUCTION
Pericaecal hernias are a rare subgroup of internal abdominal hernias that present with abdominal pain and occasionally with features of bowel obstruction.
PRESENTATION OF CASE
A 72 year old female presented with a 24-h history of sharp, localised right iliac fossa pain, and no other symptoms. Clinical examination confirmed localised peritonism in the right iliac fossa. A tentative diagnosis of acute appendicitis was considered but in view of age a CT scan was performed. An area of abnormality in the right iliac fossa region was noted. At laparoscopy a macroscopically normal appendix and caecum was found. A smooth non-indentable mass in the lateral right iliac fossa contained loops of distal ileum, passing through a retro-caecal mesenteric defect consistent with a paraceacal hernia, with entrapment of the right ovary and fallopian tube. A right salpingectomy as performed and subsequent histopathological examination confirmed infarction of the fallopian tube.
DISCUSSION
Internal abdominal hernias are reported to have a post mortem incidence ranging between 0.2 and 0.9% of which only 10–15% are accounted for by pericaecal hernias. Types of pericaecal hernias include: ileocolic, retrocaecal, ileocaecal and paracaecal. These hernias are predisposed by the embryological development of the caecum retracting to the posterior abdominal wall and forming potential fossae.
CONCLUSION
This case highlights the need to consider a pericaecal hernia as a differential cause of right iliac fossa peritonism, and an indication for radiological imaging such as CT scan when the history is atypical for acute appendicitis.
Keywords: Paracaecal hernia, Appendicitis, Salpingo-ovarian, Ileum entrapment
1. Introduction
Paracaecal hernias are a rare subgroup of internal abdominal hernias that can present with abdominal pain and features of bowel obstruction. Often the diagnosis is made at time of operation and is not apparent from the clinical history or examination. We describe the first reported case of a paracaecal hernia identified at laparoscopy within which entrapment of the right ovary, fallopian tube and distal ileum were present in a patient thought to have acute appendicitis.
2. Presentation of case
A 72 year old female presented with a 24-h history of sharp, localised right iliac fossa pain. The patient denied nausea and vomiting, altered bowel habit, anorexia, weight loss or urinary symptoms. There was no significant prior medical, gynaecological or surgical history of note. She was heamodynamically stable and apyrexial. Clinical examination confirmed localised peritonism in the right iliac fossa with no other evidence of abdominal distension, hernias, masses or organomegaly. Per rectal and urine examination were normal. Plain abdominal X-rays showed two small loops of mildly dilated small bowel but no overt obstruction (Fig. 1).
Fig. 1.
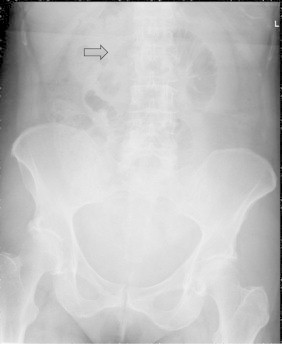
Plain abdominal radiograph. Two dilated loops of small bowel are seen (arrow).
Laboratory investigations including full electrolyte, haematological and coagulation profiles were within normal limits. However arterial blood gas revealed an elevated lactate of 4.1, with a pH of 7.435. On the basis of clinical history and examination findings acute appendicitis was considered but as the diagnosis was not clear a CT scan was performed. An area of abnormality in the region of the right iliac fossa was noted with a soft tissue density area inferior to the caecum with mesenteric thickening and calibre change in the small bowel (Fig. 2). There was no small or large bowel dilatation, groin hernia or abnormality within the rest of the intra-abdominal viscera.
Fig. 2.
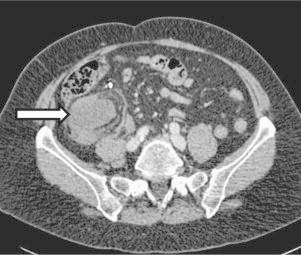
CT scan transverse view. A retrocaecal soft tissue mass is seen pushing the caecum anteriorly ( ).
).
Further ongoing pain on the second day of hospital admission mandated operative intervention. At laparoscopy a macroscopically normal appendix and caecum were found, in addition to a smooth non-indentable mass in the lateral right iliac fossa. Loops of distal ileum were observed to pass through a retrocaecal mesenteric defect consistent with a paracaecal hernia and further evaluation revealed entrapment of the right ovary and fallopian tube (Fig. 3). The fallopian tube appeared ischaemic and after evaluation by gynaecology colleagues was considered to be non-viable and a salpingectomy was performed. The ileum and ovary were not compromised. To prevent future recurrence of internal hernias in this area the entire paracolic attachment was divided. Postoperative recovery was uneventful and the patient discharged on day 4. At 2 months review she remained clinically well and pain free. Subsequent histopathological examination confirmed infarction of the fallopian tube.
Fig. 3.
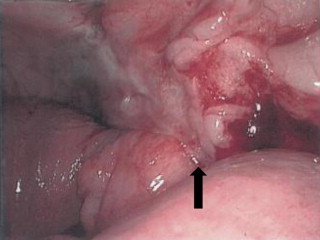
Laparoscopic view. The figure shows distal ileum passing through the paracaecal defect ( ) with the caecum displaced anteriorly.
) with the caecum displaced anteriorly.
3. Discussion
Internal abdominal hernias are reported to have a post mortem incidence ranging between 0.2 and 0.9% of which only 10–15% are accounted for by pericaecal hernias.1 Types of pericaecal hernias include ileocolic, retrocaecal, ileocaecal and paracaecal.2 These hernias are predisposed by the embryological development of the caecum retracting to the posterior abdominal wall and forming potential fossae.3 Meyer et al. proposed a classification for the boundaries of these as follows: paracaecal sulci, caecal fossa, caecal, superior ileocaecal, inferior ileocaecal and retrocaecal recesses.4 Paracaecal sulci are lateral depressions of peritoneum investing on the caecum with or without recesses. The caecal fossa is a groove formed by two peritoneal folds made up of a lateral fold from the continuation of the line of Toldt and a medial fold from the ileocaecal angle of the medial aspect of the caecum. The caecal recess is formed by the folds of the caecal fossa but the caecum is retroperitoneal. Both superior and inferior ileocaecal recesses are formed by the peritoneal folds from the terminal ileum to the caecum. Finally a retrocaecal recess is formed by the caecum anteriorly, the iliac fossa posteriorly, the right paracolic gutter and mesentery medially. In most cases of pericaecal hernia, the ileal loops herniate through the retrocaecal defect and occupy the right paracolic gutter as in our subject.5
While there have been a number of cases reported of pericaecal hernias6–9 only one has reported the appendix within a paracaecal hernia10 and from a review of the literature this is the first to document the concomitant entrapment of distal ileum, right ovary and fallopian tube. Clinical presentation of this rare entity can range from being non-specific to mimicking acute appendicitis as in our case, or even acute intestinal obstruction requiring resection.11
CT scanning has resulted in a paradigm shift in the ability to make a preoperative diagnosis of pericaecal hernias. Features on scan may reveal fluid filled small bowel loops located lateral to the caecum and posterior to the ascending colon 2. Furthermore a beaking appearance in the peritoneal recess, acute changes in calibre of small bowel and displacement of the mesenteric vascular pedicle in the hernia sac have all been described.2,7 In patients with milder clinical presentations a barium enema has been utilised to demonstrate ileal loops behind and lateral to the caecum and ascending colon.5 Although the diagnosis was not made preoperatively in our case, a retrospective analysis of images does show suggestive features (Figs. 4 and 5).
Fig. 4.
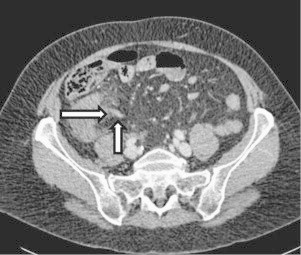
CT scan transverse view. The figure shows mushrooming of the soft tissue as it passes through the defect with beaking appearance ( ) in the peritoneal recess and displacement of the mesenteric vascular pedicle (
) in the peritoneal recess and displacement of the mesenteric vascular pedicle ( ). Unable to positively identify the appendix.
). Unable to positively identify the appendix.
Fig. 5.
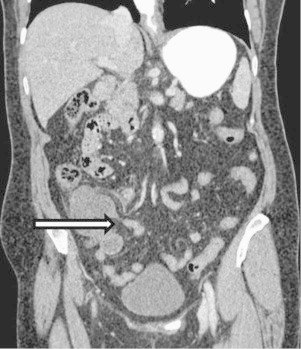
CT scan coronal view. The figure shows mushrooming of the soft tissue as it passes through the defect with beaking appearance ( ) in the peritoneal recess
) in the peritoneal recess
4. Conclusion
This is the first documented case of a paracaecal hernia with entrapment of the right ovary, fallopian tube and distal ileum presenting as a clinical acute appendicitis. The scenario highlights the requirement for ensuring a differential diagnosis which includes paracaecal hernia in patients presenting with right iliac fossa peritonism, even in the absence of obstructive symptoms and normal inflammatory markers. CT scanning provides an accurate ability to identify a paracaecal hernia preoperatively. Nevertheless in the absence of CT imaging the operating surgeon requires a high index of suspicion when a macroscopically normal appendix is encountered together with features of a mass in the region of the caecum. Often only loops of ileum are observed within the hernia but as our case illustrates, the ovary and fallopian tube can be also included.
Conflict of interest statement
None declared.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and case series and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
The manuscript was written by Ajit Dhillon and Shahid Farid. Radiology advice was given by Simon Dixon. John Evans is the consultant under whose care the patient was admitted. He also supervised the case report manuscript.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.Ghahremani G.G. Internal abdominal hernia. Surgical Clinics of North America. 1984;643:93–406. doi: 10.1016/s0039-6109(16)43293-7. [DOI] [PubMed] [Google Scholar]
- 2.Choh N.A., Rasheed M., Jehangir M. The computed tomography diagnosis of paracecal hernia. Hernia. 2010;14(5):527–529. doi: 10.1007/s10029-009-0572-4. [DOI] [PubMed] [Google Scholar]
- 3.Larson W.J. 3rd ed. Churchill Livingstone; Philadelphia, PA: 2001. Human embryology. [Google Scholar]
- 4.Meyers M. Internal abdominal hernias. In: Meyers M.A., editor. Dynamic radiology of the abdomen: normal and pathologic anatomy. 5th ed. Springer; New York: 2000. pp. 711–748. [Google Scholar]
- 5.Mathieu D., Luciano A. Internal abdominal herniations. American Journal of Roentology. 2004;183:397–404. doi: 10.2214/ajr.183.2.1830397. [DOI] [PubMed] [Google Scholar]
- 6.Jang E-J., Chi H., Kim D-D. A case of small bowel obstruction due to a paracecal hernia. Journal of Korean Society of Coloproctology. 2011;27(1):41–43. doi: 10.3393/jksc.2011.27.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu H-C., Wang J., Tsang Y-M., Tseng H-S., Li Y-W. Pericecal hernia: a report of two cases and survey of the literature. Clinical Radiology. 2002;57(9):855–858. [PubMed] [Google Scholar]
- 8.Blachar A., Federle M.P. Bowel obstruction following liver transplantation: clinical and CT findings in 48 cases with emphasis on internal hernia. Radiology. 2001;218:384–388. doi: 10.1148/radiology.218.2.r01ja22384. [DOI] [PubMed] [Google Scholar]
- 9.Bass J., Jr., Longley B.J. Paracecal hernia: case report and review of the literature. American Surgeon. 1976;42:285–288. [PubMed] [Google Scholar]
- 10.Birchley D. Ileal entrapment within a paracaecal hernia mimicking acute appendicitis. Annals of Royal College of Surgeons England. 2009;91(2):W1–W3. doi: 10.1308/147870809X400903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghiassi S., Nguyen S.Q., Divino C.M., Byrn J.C., Schlager A. Internal hernias: clinical findings, management, and outcomes in 49 nonbariatric cases. Journal of Gastrointestinal Surgery. 2007;11(3):291–295. doi: 10.1007/s11605-007-0086-2. [DOI] [PubMed] [Google Scholar]


