Abstract
INTRODUCTION
Isolated endometriosis of the intestine causing large bowel obstruction is rare.
PRESENTATION OF CASE
We present a case of endometriosis presenting as large bowel obstruction in a woman of childbearing age. She had no previous symptoms to suggest endometriosis and on presentation urgent surgery was required. The diagnosis of endometriosis was made only after pathological evaluation of the specimen.
DISCUSSION
No cases of endometriosis confined to this sigmoid colon without pelvic involvement were noted in the literature.
CONCLUSION
The diagnosis of endometriosis should be entertained when women of childbearing age presents with large bowel obstruction, whether or not the patient has other evidence of the disease.
Keywords: Endometriosis, Sigmoid, Colon, Obstruction
1. Introduction
Endometriosis involving the intestines occurs in 5% of premenopausal women. Of these, 70% present with large bowel obstruction.1 We present a case of endometriosis presenting as large bowel obstruction in a woman of childbearing age. She had no previous symptoms to suggest endometriosis and on presentation urgent surgery was required. The diagnosis of endometriosis was made only after pathological evaluation of the specimen. No cases of endometriosis confined to this sigmoid colon without pelvic involvement were noted in the literature.
When women of childbearing age seek medical attention for signs and symptoms of intestinal obstruction, and there is no obvious etiology, intestinal endometriosis should be considered as a differential diagnosis.
2. Presentation of case
A 37 year-old housewife and mother of a 10 year-old by Caesarian section, presented with a history of generalized, colicky abdominal pain and constipation for 6 days, with bilious vomiting and distention for 2 days. She had normal, regular menses with no history of dyspareunia, dysmenorrhea, abdominal pain, constipation, diarrhea or rectal bleeding.
On examination, she was in painful distress, ill looking and mildly dehydrated, with a tachycardia of 108/min. Abdominal examination revealed a Pfannenstiel incision scar. The abdomen was distended and tympanitic with generalized mild tenderness but no peritonism or palpable mass. Bowel sounds were decreased and the rectum was empty.
CT-scan showed grossly distended large intestine from the caecum to the sigmoid colon, with no air in the rectum (see Fig. 1). The complete blood count, liver function test and carcino-embryonic antigen were all within normal limits.
Fig. 1.

CT topography showing dilated large intestine from the caecum to sigmoid colon.
At surgery, the large intestine was grossly distended from the caecum to sigmoid colon where there was a palpable solid tumor in the wall of the bowel. The sigmoid loop, with its tumor, was freely mobile with no adhesions. The pelvis, ovaries, tubes and uterus were grossly normal and there were no other intra-abdominal abnormalities. With an operative diagnosis of carcinoma, sigmoid colectomy with primary anastomosis was performed. Post-operatively, she had an uneventful hospital stay of 5 days. The cut specimen revealed an obstructing tumor on the mesenteric border, within the wall of the sigmoid colon without involvement of the mucosa (see Fig. 2). Microscopically, there was endometrial glandular tissue accompanied by endometrial stroma in the sigmoid ‘tumor’, with clear margins and no evidence of malignancy (see Fig. 3). At histology, the final diagnosis of intestinal endometriosis was made. She was subsequently referred to the gynecologist for treatment and remains asymptomatic 15 months later.
Fig. 2.
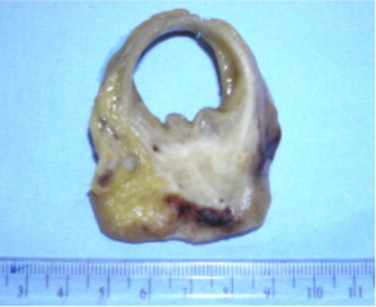
Photograph of the cut specimen (sigmoid tumor) showing diseased bowel wall with intact mucosa.
Fig. 3.
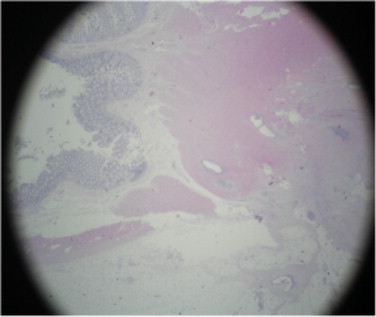
Microscopic photograph (magnification power 2×) showing normal large bowel mucosa and submucosa with endometrial glands within the muscularis propria. Stained with hematoxylin and eosin.
3. Discussion
Intestinal involvement by endometriosis occurs in 5% of premenopausal women. Of these, 70% present with large bowel obstruction.1 However, the vast majority of these patients reported are known cases of endometriosis, having complaints of pelvic pain, dyspareunia and/or dysmenorrhea.1–5 Many of them also have a history of infertility, for which they were subjected to investigation, such as laparoscopy, hence, presenting with a previous diagnosis of endometriosis.
Our patient had no history to suggest the condition with no visible endometrioma, ovarian or pelvic abnormality indicative of endometriosis. The pathophysiology of endometriosis has been explained by various theories; direct myometrial extension, coelomic metaplasia, lymphatic and hematogenous metastasis, reverse menstruation and implantation during salpingography or due to operative spillage.6 The mechanism by which our patient developed ‘isolated’ endometriosis within the muscular layer of the bowel with no involvement of mucosa or any pelvic organ remains unclear. Although seat belt trauma had, in one case, been suggested as an etiologic factor, no clear evidence was provided for this.7 In our patient, there was no history of trauma.
When the initial presentation of endometriosis is intestinal obstruction with no previous history and no suspicious findings at surgery, the diagnosis is unlikely to be made preoperatively. In most reported cases, the patients had a known history of endometriosis or the surgical findings were very suggestive of it.8 Both these observations were absent in our patient. In the non-obstructed case, colonoscopy, endoscopic ultrasonography and magnetic resonance imaging may assist in accurate preoperative diagnosis.9 We believe that one should always maintain a high level of suspicion of endometriosis, when a woman of childbearing age presents with intestinal obstruction and there is no other obvious cause. If the diagnosis is made preoperatively, surgery may be avoided in the non-obstructed case and only a limited resection done in the event of obstruction.10
4. Conclusion
When a woman of childbearing age presents with large bowel obstruction, one should always entertain a possible diagnosis of endometriosis whether or not the patient has other evidence of the disease.
Conflict of interest statement
The authors have no conflict of interest to disclose.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-chief of this journal on request.
Author contributions
All the authors of this article contributed to the study design, data collection, data analysis and writing.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.Lin Y.H., Kuo L.J., Chuang A.Y., Cheng T.I., Hung C.F. Extrapelvic endometriosis complicated with colonic obstruction. J Chin Med Assoc. 2006;69:47–50. doi: 10.1016/S1726-4901(09)70111-X. [DOI] [PubMed] [Google Scholar]
- 2.Jarmin R., Idris M.A., Shaharuddin S., Nadeson S., Rashid L.M., Mustaffa W.M. Intestinal obstruction due to rectal endometriosis: a surgical enigma. Asian J Surg. 2006;29(3):149–152. doi: 10.1016/S1015-9584(09)60075-0. [DOI] [PubMed] [Google Scholar]
- 3.Mourthe de Alvim Andrade M., Batista Pimenta M., De Freitas Belezia B., Durte T. Rectal obstruction due to endometriosis. Tech Coloproctol J. 2008;12(1):57–59. doi: 10.1007/s10151-008-0387-1. [DOI] [PubMed] [Google Scholar]
- 4.Paksoy M., Karabicak I., Ayan F., Aydogan F. Intestinal obstruction due to rectal endometriosis. Mt Sinai J Med. 2005;72(6):405–408. [PubMed] [Google Scholar]
- 5.Yildirim S., Nursal T., Tarim A., Tarim A., Torer N., Bal N. Colonic obstruction due to rectal endometriosis. Turk J Gastroenterol. 2005;16(1):48–51. [PubMed] [Google Scholar]
- 6.Nagar H.S., Tyagi A.K., Chouhan A., Mohanty S.K. Ileocaecal endometriosis with intestinal obstruction. Med J Armed Forces India (MJAFI) 2005;61(1):82–83. doi: 10.1016/S0377-1237(05)80129-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Haddad M., Bouras E.P., Cangemi J.R. Sigmoid endometriosis presenting with colonic obstruction after seat-belt trauma. Vis Huan J Endosc. 2006;5(2):2–3. [Google Scholar]
- 8.Bartkowiak R., Zieniewicz K., Kaminski P., Krawczyk M., Marianowski L., Szymanska K. Diagnosis and treatment of sigmoid endometriosis – a case report. Med Sci Monit. 2000;6(4):787–790. [PubMed] [Google Scholar]
- 9.Yoshida M., Watanabe Y., Horiuchi A., Yamamoto Y., Sugishita H., Kawachi K. Sigmoid colon endometriosis treated with laparoscopy-associated sigmoidectomy: significance of preoperative diagnosis. World J Gastroenterol. 2007;13(40):5400–5402. doi: 10.3748/wjg.v13.i40.5400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dimoulios P., Koutroubakis I.E., Tzardi M., Antoniou P., Matalliotakis I.M., Kouroumalis E.A. A case of sigmoid endometriosis difficult to differentiate from colon cancer. BMC Gastroenterol. 2003;3:18–21. doi: 10.1186/1471-230X-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]


