Abstract
In this prospective case series study, 20 patients with an implant-borne single crown following early implant placement with simultaneous contour augmentation were followed for 6 years. Clinical, radiologic, and esthetic parameters were assessed. In addition, cone beam computed tomography (CBCT) was used at 6 years to examine the facial bone wall. During the study period, all 20 implants were successfully integrated, and the clinical parameters remained stable over time. Pleasing esthetic outcomes were noted, as assessed by the pink esthetic scores. None of the implants developed mucosal recession of 1 mm or more. The periapical radiographs yielded stable peri-implant bone levels, with a mean DIB of 0.44 mm at 6 years. The CBCT scans showed that all 20 implants had a detectable facial bone wall at 6 years, with a mean thickness of around 1.9 mm. In summary, this prospective case series study demonstrated stable peri-implant hard and soft tissues for all 20 implants, and pleasing esthetic outcomes overall. The follow-up of 6 years confirmed that the risk for mucosal recession is low with early implant placement. In addition, contour augmentation with guided bone regeneration (GBR) was able to establish and maintain a facial bone wall in all 20 patients.
Keywords: post-extraction implant placement, guided bone regeneration, single-tooth replacement, esthetic outcome, esthetic complication, dental implant
Introduction
Today, the timing of implant placement post-extraction in the esthetic zone is considered an important factor which influences the esthetic treatment outcome (Chen and Buser, 2009). The clinician can choose from 4 different treatment options, as defined by 2 ITI Consensus Conferences in 2003 and 2008(Hämmerle et al., 2004; Chen et al., 2009). One of these options is early implant placement after 4 to 8 wks of soft-tissue healing (Buser et al., 2008). Implant placement is combined with simultaneous contour augmentation by guided bone regeneration (GBR) to compensate for ridge alterations post-extraction (Araújo and Lindhe, 2005). They are caused by bundle bone resorption and often result in a crater-like bone defect on the facial aspect of the extraction site, since, in most cases, this bone wall is either thin or missing at the time of extraction in the anterior maxilla (Braut et al., 2011; Januário et al., 2011).
The purpose of the present case series study was to analyze the stability of esthetic treatment outcomes in 20 patients following single-tooth replacement in the anterior maxilla using the concept of early implant placement with simultaneous contour augmentation. These 20 patients were followed for 6 yrs. The one- and three-year results have been previously reported (Buser et al., 2009, 2011). Special emphasis was placed on assessing the stability of the facial mucosa, since it directly depends on the stability of successful contour augmentation by GBR. For that, we obtained cone beam computed tomography (CBCT) scans to examine the facial bone wall.
Materials & Methods
In 2005 and 2006, 20 patients were consecutively enrolled in this study for examination of the concept of early implant placement in post-extraction single-tooth gaps in the anterior maxilla. The study protocol was approved by the standing ethical committee for clinical studies of the State of Bern (approval No. 30/05), and all patients gave their written informed consent. In addition, approval was obtained a second time from the same ethical committee (approval No.180/11) for the six-year examination, which included CBCT scans, and the patients signed a second informed consent. The study conformed to STROBE guidelines. Details of case selection and surgical and restorative procedures have been reported in 2 previous publications (Buser et al., 2009, 2011). The most important aspects of the surgical procedures included flapless tooth extraction, a soft-tissue healing period of 4 to 8 wks, and placement of a bone level implant with a chemically modified, sandblasted, and acid-etched surface (SLActive®, Straumann AG, Basel, Switzerland) in a correct 3-dimensional position. Simultaneous contour augmentation was performed with locally harvested autogenous bone chips to cover the exposed implant surface on the facial aspect, followed by a superficial layer of deproteinized bovine bone mineral (DBBM, Bio-Oss®, Geistlich Pharma, Wolhusen, Switzerland). The augmentation material was then covered with a non-crosslinked collagen membrane (Bio-Gide®, Geistlich Pharma), followed by tension-free primary wound closure. The reopening procedure with a flapless excision of the mucosa was performed after 8 to 12 wks of healing, and was followed by the prosthetic procedures for a screw-retained full-ceramic crown.
Follow-up Examinations
After completion of therapy, the 20 patients were recalled at various time-points. For the present report, the one-, three-, and six-year data for the following parameters are reported as outlined in detail in previous publications:
Clinical Parameters
Modified plaque index (mPLI) and modified sulcus bleeding index (mSBI; Buser et al., 1991)
Probing depth (PD, in mm; Buser et al., 1991)
Width of keratinized mucosa (KM, in mm; Buser et al., 1991)
DIM value (distance from the mucosal margin to the implant shoulder, in mm) on the facial aspect following the removal of the screw-retained crown (Buser et al., 1991)
Cast analysis. The mid-facial height of the implant crown (IC) and the corresponding height of the contralateral tooth crown (TC) were both measured on digitized images to identify potential changes in crown height (Buser et al., 2009).
Esthetic parameters. The respective casts and intra-oral pictures were critically analyzed by two examiners to assess the modified pink esthetic score (modPES; Belser et al., 2009).
Radiographic Parameters
DIB values (distance from the implant shoulder to the first bone-to-implant contact, in mm) measured on periapical radiographs as the average of the obtained mesial and distal values (Weber et al., 1992)
An additional 3D radiographic analysis was obtained at 6 yrs by CBCT with a 4 x 4-cm field of view (3D Accuitomo 170, Morita, Kyoto, Japan). For each implant, the thickness of the facial bone wall was measured (in mm) with specialized software (i-Dixel, Morita, Kyoto, Japan) at 3 different levels: 2 mm, 4 mm, and 6 mm apical to the implant shoulder.
Statistical Analysis
First, all data were analyzed with descriptive methods. To analyze possible differences over time in the gingival, esthetic, and radiographic parameters, we used exact Wilcoxon signed-rank tests, due to small sample size. The level of significance for all tests was p < .05. All statistical tests were calculated with the package exactRankTests (R 2.15.1 for Windows, Institute for Statistics and Mathematics, Vienna University of Economics and Business, Vienna, Austria; http://www.R-project.org). None of the p values was adjusted for multiple endpoints.
Results
Clinical Findings
Detailed results, including statistical analysis, are listed in Table 1. During the entire six-year study period, all implants were firmly integrated, demonstrating ankylotic stability. None of the patients presented with suppuration in the peri-implant sulcus. Overall, the patients exhibited good oral hygiene, documented by a mean mPLI of 0.40 at 6 yrs. Although one implant showed peri-implant mucositis, with reddening of the mucosal margin, the peri-implant soft tissues appeared healthy overall, as documented by a low mean mSBI of 0.16 at the six-year examination. The mean PD was 4.24 mm at 6 yrs. All implants showed a keratinized mucosa on the facial aspect, with a mean KM of more than 4 mm.
Table 1.
Clinical and Cast Parameters of the 20 Implants over Time (mean ± standard deviation)
| Parameters | Modified Plaque Index (modPlI) | Modified Sulcus Bleeding Index (modSBI) | Probing Depth (PD; mm) | Keratinized Mucosa (KM; mm) | Distance Implant Shoulder to Mucosal Margin* (DIM; mm) | Height of Implant Crown (IC; mm) | Height of Contralateral Tooth Crown (TC; mm) |
|---|---|---|---|---|---|---|---|
| 1 yr | 0.36 (± 0.33) | 0.21 (± 0.17) | 4.43 (± 0.57) | 4.50 (± 1.54) | −3.53 (± 1.16) | 10.03 (± 1.05) | 9.85 (± 1.23) |
| 3 yrs | 0.40 (± 0.27) | 0.20 (± 0.20) | 4.00 (± 0.56) | 4.10 (± 1.17) | −3.68 (± 0.97) | 9.94 (± 1.04) | 9.84 (± 1.21) |
| 6 yrs | 0.40 (± 0.41) | 0.16 (± 0.17) | 4.24 (± 0.49) | 4.20 (± 1.28) | −3.95 (± 1.14) | 9.99 (± 1.04) | 9.94 (± 1.23) |
There were no statistically significant differences between/among any investigated parameters over time. * The DIM value is limited to the facial aspect; n = 20 for all parameters measured except for DIM (n = 19).
Esthetic Outcomes
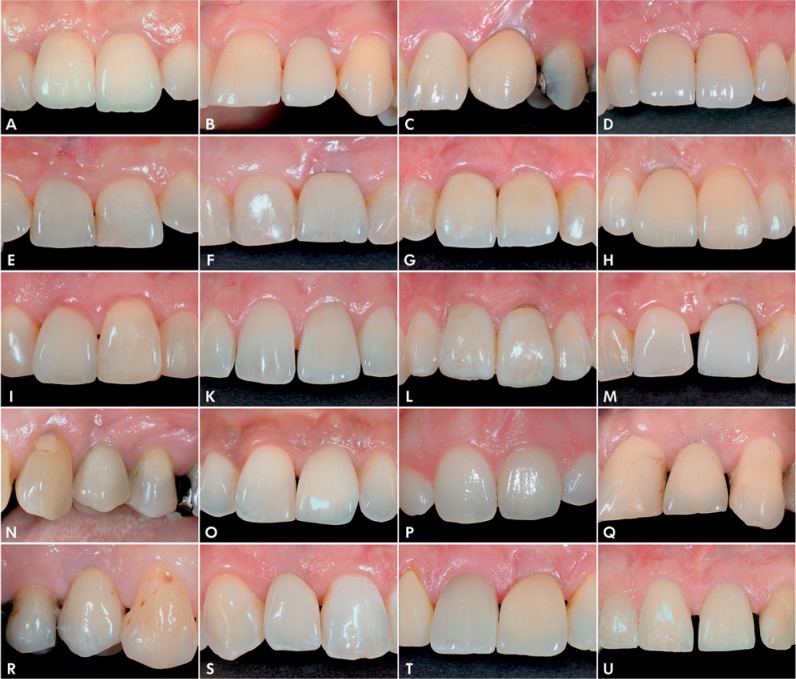
On the whole, the esthetic outcomes were pleasing throughout the study period. Fig. 1 shows the clinical status of all implant crowns at 6 yrs. The peri-implant soft tissues showed good stability, with only one implant demonstrating minor mucosal recession of 0.5 to 1 mm. This is documented by the facial DIM values, which remained stable over time, with a mean DIMfac of -3.95 mm at 6 yrs (Table 1), indicating a submucosal position of the implant platform. The stability of the soft tissue is also documented by the IC and TC values measured on the casts, which were similar at all 3 examinations (Table 1). The mean IC at the six-year examination was 9.99 mm (SD 1.04 mm), and the mean TC was 9.94 mm (SD 1.23 mm). The differences between IC and TC values at all 3 time-points were not statistically significant.
Figure 1.
Clinical pictures of all 20 implant-borne single crowns at 6 yrs. One implant (1M) showed minor recession of between 0.5 and 1 mm. Three implants yielded a step at the incisal edge (1A, 1D, 1L). Another implant (1I) demonstrated peri-implant mucositis.
The PES values at all 3 examinations also indicated stability over time. At the six-year examination, the analysis revealed a mean PES value of 8.25 (range, 5 to 10).The mean PES score was slightly higher compared with that at the first examination, with a mean PES value of 8.10, without reaching statistical significance (Appendix Table). Among the 5 parameters evaluated, the level of the mucosal margin showed the best mean value, with 1.9, whereas the mesial and distal papillae resulted in mean values of 1.5. It was also noted that three patients with an implant crown in the central incisor position developed a step at the incisal edge (Figs. 1A, 1D, 1L). These patients had an age of 24, 28, and 42 yrs, respectively, at the time of implant surgery.
Radiographic Findings
During the six-year period, none of the 20 implants demonstrated continuous peri-implant radiolucency. Overall, minimal crestal bone loss was observed, with a mean DIB of 0.44 mm at 6 yrs (range, 0.00 to 1.09 mm), compared with 0.18 mm at the one-year examination (Table 2). The difference reached statistical significance. Frequency analysis of the 20 DIB values at 6 yrs demonstrated 13 implants with a DIB value < 0.50 mm, 6 with a value between 0.50 and 1.00 mm, and 1 with a value > 1 mm.
Table 2.
Radiographic Data with DIB Values at Various Time Points, and the Thickness of the Facial Bone Wall at Various Levels
| DIB Values over Time (in mm) | Thickness of Facial Bone Wall (in mm) | |||||||
|---|---|---|---|---|---|---|---|---|
| Parameters | 0 mos | 12 mos | 36 mos | 72 mos | Platform Level | 2 mm | 4 mm | 6 mm |
| Mean | 0 | 0.18 | 0.18 | 0.44 | 1.05 | 1.75 | 1.96 | 1.93 |
| Median | 0 | 0.17 | 0.14 | 0.47 | 1.32 | 1.77 | 1.88 | 1.96 |
| Minimum | 0 | 0 | 0 | 0 | 0.00 | 0.22 | 0.14 | 0.19 |
| Maximum | 0 | 0.76 | 0.70 | 1.09 | 2.24 | 2.89 | 2.81 | 3.73 |
| STD | ± 0.00 | ± 0.20 | ± 0.23 | ± 0.24 | ± 0.79 | ± 0.57 | ± 0.63 | ± 0.72 |
| Significance | a, b, c | a, d | b, e | c, d, e | ||||
Statistically significant differences between the DIB values are marked with the same letters.
Examination of the facial bone wall with CBCT demonstrated that all 20 implants had a detectable facial bone wall (Fig. 2). The mean thickness ranged between 1.06 mm (SD 0.79 mm) at the platform level and 1.93 mm (SD 0.72 mm) at 6 mm apical to the platform (Table 2). At 14 implants, the facial bone wall extended coronal to the implant platform, with intact bone at the implant shoulder, whereas the remaining 6 implants showed minimal bone loss on the facial aspect. At 2, 4, and 6 mm apical to the platform, the facial wall was present on all CBCTs. However, one implant showed a rather thin facial bone wall, providing the minimal values at all levels of measurement (Fig. 2M). This implant also provided the least favorable PES value, with 5 at the six-year examination (Table 1), and mucosal recession between 0.5 and 1 mm during the study period (Fig. 1M).
Figure 2.
Oro-facial CBCT scans of all 20 implants. In 14 implants, the facial bone wall extended coronal to the platform, whereas 6 showed minor bone resorption at the platform level. One implant (1M) showed a very thin facial wall and was considered at risk.
Discussion
The six-year results of this prospective case series study with 20 consecutively treated patients confirm previously published favorable one- and three-year data (Buser et al., 2009, 2011). All 20 implants yielded successful tissue integration over 6 yrs, documented by clinical and radiographic parameters. The measured clinical parameters indicated healthy and stable peri-implant soft tissues. None of the parameters showed a significant change over time, and the mean values obtained were all in line with previous prospective studies utilizing identical parameters (Buser et al., 1999; Weber et al., 2000; Bornstein et al., 2005).
The DIB values obtained indicated overall minimal crestal bone loss, with a mean value of 0.44 mm. This is a low value for bone loss over 6 yrs and can be attributed to the platform-switching design of the bone level implants utilized. In recent years, several studies have demonstrated good crestal bone stability for such implants (Atieh et al., 2010). This assumption is supported by direct comparison with a recent publication including 41 implants and a follow-up of 5 to 9 yrs (Buser et al., 2013). In this study, with the same surgical protocol but non-platform-switching implants, the mean DIB value was 2.18 mm.
The main focus of this prospective six-year study was to determine the long-term stability of contour augmentation by the GBR technique. The goal of contour augmentation is the establishment of a facial bone wall of sufficient height and thickness to serve as support for esthetic soft tissues. The dimensions of this facial bone wall can be examined only by 3D radiographic imaging. Today, CBCT technology offers excellent image quality with a clearly reduced radiation dose risk for the patient when compared with dental CTs, in particular when a small 4 x 4-cm field of view is used (Loubele et al., 2009; Pauwels et al., 2012).
The CBCT images in the present study demonstrated a mean thickness of the facial bone wall between 1.05 and 1.96 mm at various levels. The CBCT findings of the facial bone, however, represent not only bone, but also the remaining DBBM particles. Only the histomorphometric analysis of human biopsies can show what percentage of this facial wall is bone vs. remaining graft material. Such data on human biopsies in a retrospective study with more than 10 patients will soon be available. In the present study, it is remarkable that 14 implants showed the peak of the facial bone wall coronal to the implant platform, whereas 6 implants had no facial bone directly at the shoulder level. The facial bone resorption, however, was minimal, since all 20 implants had an intact facial bone wall at 2 mm apical to the platform. This is in contrast to immediately placed implants that showed no detectable facial bone wall in 36% to 57% of cases in 2 retrospective CBCT studies (Miyamoto and Obama, 2011; Benic et al., 2012). Increased facial bone resorption has also been confirmed in 2 recent prospective one-year studies by consecutive CBCT images (Roe et al., 2012; Vera et al., 2012). One of these studies showed that 3 out of 7 immediately placed implants (43%) had no detectable facial bone wall at the one-year follow-up. These results clearly indicate that genetically driven ridge alterations take place following tooth extraction, even if an implant is placed on the day of extraction in combination with simultaneous bone augmentation.
An increased mucosal recession rate of between 20% and 40% was reported in 2 systematic reviews of esthetic complications with immediate implants, when primarily non-platform-switching implants were examined (Chen and Buser, 2009, 2013). In the present study, a much lower incidence of mucosal recession was observed, with only 1 implant (5%) showing minor recession of 0.5 and 1.0 mm. This is the same implant mentioned above, which showed a visible but rather thin bone wall in the CBCT. This implant must be considered at risk. The remaining 19 implants showed no mucosal recession, which was also confirmed by stable facial DIM values and the prospective cast analysis that measured IC values. The esthetic soft-tissue outcomes were also assessed with the modified PES index (Belser et al., 2009). The mean PES value was 8.25 at the six-year examination, slightly superior to values at 1 and 3 yrs. The observation of 3 incisal steps over time, in patients between 24 and 42 yrs of age at the time of implant surgery, confirms other reports of lifelong craniofacial growth causing esthetic complications (Bernard et al., 2004; Daftary et al., 2012)
The stability of the facial mucosa is mainly attributed to the stability of the underlying facial bone wall, which is built up during implant surgery with simultaneous contour augmentation by GBR. Here, 2 factors are decisive: the quality of the treatment applied by the involved surgeon, and the characteristics of the biomaterials utilized for contour augmentation.
The presented CBCT results indicate that a resorbable collagen membrane, in combination with autogenous bone chips and DBBM granules, is able to provide successful contour augmentation on the facial aspect of an implant, combined with primary wound closure and submerged healing for 8 wks. The combination of 2 bone fillers offers a synergistic effect which optimizes the regenerative outcome. The use of DBBM granules seems important for the long-term stability of the facial bone wall, since they have a low substitution rate (Jensen et al., 2005, 2006). They are combined with locally harvested autogenous bone chips. It is hypothesized that these bone chips not only accelerate new bone formation at the exposed implant surface, but also potentially enhance the ingrowth of newly formed bone into the superficial layer of DBBM particles. There is debate about the osteogenic potential of autografts. It is argued that non-collagenous proteins and/or osteocytes entrapped in the bone matrix may play an important role (Bosshardt and Schenk, 2009; Miron et al., 2011, 2013). The bony integration of DBBM particles seems important, since they are prone to resorption when they are located outside the bony envelope and come into contact with soft-tissue cells of the overlying mucosa (Busenlechner et al., 2012). These mechanisms are not well-understood and need further clarification.
The results of the present study confirm favorable data from a recent prospective cross-sectional study with 41 implants and 5 to 9 yrs of follow-up using the same surgical approach (Buser et al., 2013). This study reported a low risk of mucosal recession and the presence of an intact facial bone wall in 95% of the patients. Considering both prospective long-term studies, we can conclude that early implant placement with simultaneous contour augmentation offers high predictability for successful esthetic outcomes and good long-term stability of the established facial bone wall.
Acknowledgments
The authors thank Mrs. Olivia Bucher and Claudia Moser for the organization of all follow-up examinations.
Footnotes
The study was supported by departmental funds of the Universities of Bern and Geneva and by a research grant from Institut Straumann AG, Basel. J.-G. Wittneben serves on the advisory board and is a consultant of the cited companies, and owns related stocks or stock options.
The remaining authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
References
- Araújo MG, Lindhe J. (2005). Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol 32:212-218 [DOI] [PubMed] [Google Scholar]
- Atieh MA, Ibrahim HM, Atieh AH. (2010). Platform switching for marginal bone preservation around dental implants: a systematic review and meta-analysis. J Periodontol 81:1350-1366 [DOI] [PubMed] [Google Scholar]
- Belser UC, Grutter L, Vailati F, Bornstein MM, Weber HP, Buser D. (2009). Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria. A cross-sectional, retrospective study in 45 patients with a 2-4 year follow-up using pink and white esthetic scores (PES/WES). J Periodontol 80:140-151 [DOI] [PubMed] [Google Scholar]
- Benic GI, Mokti M, Chen CJ, Weber HP, Hämmerle CH, Gallucci GO. (2012). Dimensions of buccal bone and mucosa at immediately placed implants after 7 years: a clinical and cone beam computed tomography study. Clin Oral Implants Res 23:560-566 [DOI] [PubMed] [Google Scholar]
- Bernard JP, Schatz JP, Christou P, Belser U, Kiliaridis S. (2004). Long-term vertical changes of the anterior maxillary teeth adjacent to single implants in young and mature adults. A retrospective study. J Clin Periodontol 31:1024-1028 [DOI] [PubMed] [Google Scholar]
- Bornstein MM, Schmid B, Belser UC, Lussi A, Buser D. (2005). Early loading of non-submerged titanium implants with a sandblasted and acid-etched surface. 5-year results of a prospective study in partially edentulous patients. Clin Oral Implants Res 16:631-638 [DOI] [PubMed] [Google Scholar]
- Bosshardt DD, Schenk RK. (2009). Biologic basis of bone regeneration. In: 20 years of guided bone regeneration. Buser D, editor. Chicago, IL: Quintessence Publishing, pp. 15-45 [Google Scholar]
- Braut V, Bornstein MM, Belser U, Buser D. (2011). Thickness of the anterior maxillary facial bone wall: a retrospective radiographic study using cone beam computed tomography. Int J Periodontics Restorative Dent 31:125-131 [PubMed] [Google Scholar]
- Busenlechner D, Tangl S, Arnhart C, Redl H, Schuh C, Watzek G, et al. (2012). Resorption of deproteinized bovine bone mineral in a porcine calvaria augmentation model. Clin Oral Implants Res 23:95-99 [DOI] [PubMed] [Google Scholar]
- Buser D, Weber HP, Brägger U, Balsiger C. (1991). Tissue integration of one-stage ITI implants: 3-year results of a longitudinal study with hollow-cylinder and hollow-screw implants. Int J Oral Maxillofac Implants 6:405-412 [PubMed] [Google Scholar]
- Buser D, Mericske-Stern R, Dula K, Lang NP. (1999). Clinical experience with one-stage, non-submerged dental implants. Adv Dent Res 13:153-161 [DOI] [PubMed] [Google Scholar]
- Buser D, Chen ST, Weber HP, Belser UC. (2008). Early implant placement following single-tooth extraction in the esthetic zone: biologic rationale and surgical procedures. Int J Periodontics Restorative Dent 28:441-451 [PubMed] [Google Scholar]
- Buser D, Hart C, Bornstein M, Grütter L, Chappuis V, Belser UC. (2009). Early implant placement with simultaneous GBR following single-tooth extraction in the esthetic zone: 12-month results of a prospective study with 20 consecutive patients. J Periodontol 80:152-162 [DOI] [PubMed] [Google Scholar]
- Buser D, Wittneben J, Bornstein MM, Grütter L, Chappuis V, Belser UC. (2011). Stability of contour augmentation and esthetic outcomes of implant-supported single crowns in the esthetic zone: 3-year results of a prospective study with early implant placement postextraction. J Periodontol 82:342-349 [DOI] [PubMed] [Google Scholar]
- Buser D, Chappuis V, Bornstein MM, Wittneben JG, Frei M, Belser UC. (2013). Long-term stability of contour augmentation with early implant placement following single tooth extraction in the esthetic zone. A prospective, cross-sectional study in 41 patients with a 5- to 9-year follow-up. J Periodontol [Epub ahead of print 1/24/2013] (in press). [DOI] [PubMed] [Google Scholar]
- Chen ST, Buser D. (2009). Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants 24(Suppl):186-217 [PubMed] [Google Scholar]
- Chen S, Buser D. (2013). Esthetic outcomes following immediate and early implant placement in the anterior maxilla—a systematic review. Int J Oral Maxillofac Implants (accepted for publication, in press) [DOI] [PubMed] [Google Scholar]
- Chen ST, Beagle J, Jensen SS, Chiapasco M, Darby I. (2009). Consensus statements and recommended clinical procedures regarding surgical techniques. Int J Oral Maxillofac Implants 24(Suppl):272-278 [PubMed] [Google Scholar]
- Daftary F, Mahallati R, Bahat O, Sullivan RM. (2012). Lifelong craniofacial growth and the implications for osseointegrated implants. Int J Oral Maxillofac Implants 28:163-169 [DOI] [PubMed] [Google Scholar]
- Hämmerle CH, Chen ST, Wilson TG., Jr (2004). Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int J Oral Maxillofac Implants 19(Suppl):26-28 [PubMed] [Google Scholar]
- Januário AL, Duarte WR, Barriviera M, Mesti JC, Araújo MG, Lindhe J. (2011). Dimension of the facial bone wall in the anterior maxilla: a cone-beam computed tomography study. Clin Oral Implants Res 22:1168-1171 [DOI] [PubMed] [Google Scholar]
- Jensen SS, Broggini N, Weibrich G, Hjørting-Hansen E, Schenk R, Buser D. (2005). Bone regeneration in standardized bone defects with autografts or bone substitutes in combination with platelet concentrate: a histologic and histomorphometric study in the mandibles of minipigs. Int J Oral Maxillofac Implants 20:703-712 [PubMed] [Google Scholar]
- Jensen SS, Broggini N, Hjørting-Hansen E, Schenk R, Buser D. (2006). Bone healing and graft resorption of autograft, anorganic bovine bone and beta-tricalcium phosphate. A histologic and histomorphometric study in the mandibles of minipigs. Clin Oral Implants Res 17:237-243 [DOI] [PubMed] [Google Scholar]
- Loubele M, Bogaerts R, Van Dijck E, Pauwels R, Vanheusden S, Suetens P, et al. (2009). Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol 71:461-468 [DOI] [PubMed] [Google Scholar]
- Miron RJ, Hedbom E, Saulacic N, Zhang Y, Sculean A, Bosshardt DD, et al. (2011). Osteogenic potential of autogenous bone grafts harvested with four different surgical techniques. J Dent Res 90:1428-1433 [DOI] [PubMed] [Google Scholar]
- Miron RJ, Gruber R, Hedbom E, Saulacic N, Zhang Y, Sculean A, et al. (2013). Impact of bone harvesting techniques on cell viability and the release of growth factors of autografts. Clin Implant Dent Relat Res 14:481-489 [DOI] [PubMed] [Google Scholar]
- Miyamoto Y, Obama T. (2011). Dental cone beam computed tomography analyses of postoperative labial bone thickness in maxillary anterior implants: comparing immediate and delayed implant placement. Int J Periodontics Restorative Dent 31:215-225 [PubMed] [Google Scholar]
- Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, et al. (2012). Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol 81:267-271 [DOI] [PubMed] [Google Scholar]
- Roe P, Kan JY, Rungcharassaeng K, Caruso JM, Zimmerman G, Mesquida J. (2012). Horizontal and vertical dimensional changes of peri-implant facial bone following immediate placement and provisionalization of maxillary anterior single implants: a 1-year cone beam computed tomography study. Int J Oral Maxillofac Implants 27:393-400 [PubMed] [Google Scholar]
- Vera C, De Kok IJ, Chen W, Reside G, Tyndall D, Cooper LF. (2012). Evaluation of post-implant buccal bone resorption using cone beam computed tomography: a clinical pilot study. Int J Oral Maxillofac Implants 27:1249-1257 [PubMed] [Google Scholar]
- Weber HP, Buser D, Fiorellini JP, Williams RC. (1992). Radiographic evaluation of crestal bone levels adjacent to nonsubmerged titanium implants. Clin Oral Implants Res 3:181-188 [DOI] [PubMed] [Google Scholar]
- Weber HP, Crohin CC, Fiorellini JP. (2000). A 5-year prospective clinical and radiographic study of non-submerged dental implants. Clin Oral Implants Res 11:144-153 [PubMed] [Google Scholar]