Abstract
The purpose of this study was (1) to investigate denture satisfaction following the conversion of existing mandibular complete dentures to implant overdentures (IOD) in very old edentulous patients who depend on help for activities of daily living and (2) to evaluate secondary end points, such as functional, structural, nutritional, and patient-centered aspects. For this randomized clinical trial, 2 interforaminal short implants were placed in the intervention group (n = 16, 85.0 ± 6.19 yrs) to retain mandibular IODs; the control group (n = 18, 84.1 ± 5.55 yrs) received conventional relines. During the first year, no implant was lost; however, 2 patients died. IODs proved more stable, and participants in the intervention group demonstrated significantly higher denture satisfaction as well as an increased oral health–related quality of life compared to the control group. Maximum voluntary bite force improved significantly with IODs, yet the chewing efficiency was not different between groups. Masseter muscle thickness increased with IODs, mainly on the preferred chewing side. Body mass index decreased in both groups, but the decline tended to be smaller in the intervention group; blood markers and the Mini Nutritional Assessment did not confirm this tendency. These results indicate that edentulous patients who depend on help for activities of daily living may benefit from IODs even late in life (ClinicalTrial.gov NCT01928004).
Keywords: geriatric dentistry, dental prostheses, dental implants, patient satisfaction, nutritional status, mastication
Introduction
Implant overdentures (IODs) proved clinically effective in numerous randomized controlled trials and present functional, structural, as well as psychosocial benefits (Awad et al., 2000; Müller et al., 2012). Despite the aging population, most studies enroll independently living patients younger than 70 yrs, so little is known about IODs in very old and institutionalized adults. Simple, fast, and minimally invasive treatment concepts are important to meet the needs of elderly adults with compromised physical health (Walton and MacEntee, 2005; Müller et al., 2011). A reduced chewing efficiency not only compromises the pleasures of dining but also affects food choice and nutritional intake (Sheiham et al., 2001). Yet, a body mass index over 28 seems to reduce morbidity and mortality in very old persons (Weiss et al., 2008). Consequently improving chewing efficiency might contribute toward an improved nutritional status. An increased chewing force might further stimulate salivary secretion from the parotid gland, which would facilitate mastication and alleviate discomfort caused by xerostomia. Last but not least, it remains unknown if IODs improve oral health–related quality of life and denture satisfaction in very old edentulous patients.
The present study aimed to test the following hypothesis: In very old edentulous patients who depend on help for activities of daily living, the conversion of existing complete lower dentures to IODs by means of 2 short interforaminal implants provides the same denture satisfaction than that of a conventional reline. Secondary end points were implant survival, maximum voluntary bite force, masseter muscle thickness, chewing efficiency, salivary flow, nutritional status, and oral health–related quality of life.
Materials & Methods
Randomization
Permission of the local ethics committee (Psy06-038) and written informed consent were obtained. The randomization sequence was established with http://www.randomizer.org with block sizes of 10 and an allocation ratio of 1:1. The sequence was established before recruitment of the study commenced and concealed in nontransparent consecutively numbered envelopes. After enrollment of a participant, the next randomization envelope was opened, according to the previously established sequence.
Inclusion and Exclusion Criteria
Inclusion criteria comprised an age of 75 yrs or older and living institutionalized or receiving help for activities of daily living as assessed with the Instrumental Activities of Daily Living Scale (Lawton and Brody, 1969). This scale covers the patient’s ability to dress and feed oneself, as well as continence, mobility, and toilette. Participants had to be edentulous and wear complete dentures. The lower denture had to cause discomfort to the degree that the patients were seeking treatment. Exclusion criteria comprised depression (evaluated with the Geriatric Depression Scale; Sheikh and Yesavange, 1986), dementia (according to the Mini-Mental State Examination; Folstein et al., 1975), poorly controlled diabetes, immunosuppression, or treatment with bisphosphonates.
Intervention
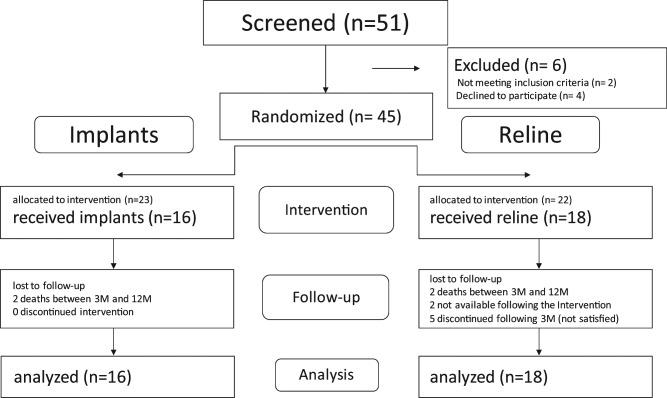
Between September 2007 and March 2011, 51 edentulous patients were screened to enter the study, and 45 were randomized (Figure). Anamnesis and examinations took place in the dental school, in the participant’s long-term care facility, or at his or her home. Different operators performed surgery (LV), the prosthetic procedures (FM, AL), and the endpoint evaluations (ED, MS). The patients obviously knew about the nature of their interventions. The trial was stopped in March 2011 because the funding expired. The treatment was free of charge.
Figure.
CONSORT flow diagram. Time points of assessment were baseline, intervention (implant loading/reline), and 3 and 12 months after the intervention (3M and 12M, respectively).
Twenty-three patients were allocated to the intervention group, but 7 withdrew after randomization. Thus, 16 participants received 2 Straumann Standard Implants (SLA surface, 8-mm length, RN, 4.1-mm diameter; Straumann, Basel, Switzerland) in the interforaminal region per the recommended surgical protocol. The implants were loaded using Locator attachments (Zest Anchors, Escondido, CA, USA) after 6 to 8 weeks of healing time by transforming the existing lower denture to an IOD.
Twenty-two patients were assigned to the control group, but 4 withdrew after randomization. Therefore, 18 patients received a conventional reline of their lower denture. Time points were baseline, intervention (implant loading/reline), 3 months, and 12 months.
Outcome Measures
Implant survival and success were assessed according to the Buser criteria, which refer to a successful osseointegration, the absence of local pathologies, and the possibility for restoration (Buser et al., 1990). The nutritional state was judged via body mass index (kg/m2) as well as the Mini Nutritional Assessment, a validated instrument covering 18 aspects of the patient’s general health, nutritional state, and nutritional habits (Guigoz et al., 1994). Blood markers (hemoglobin, albumin, folic acid, vitamin B12, and C-reactive protein) were collected and analyzed on whole blood and serum by Unilabs (Geneva) at baseline, 3 months, and 12 months.
Chewing efficiency was evaluated at all time points with a two-color mixing ability test; therefore, a two-colored chewing gum is masticated for 20 chewing cycles on the preferred chewing side (Schimmel et al., 2007). The optoelectronic analysis was performed with ViewGum software (http://www.dhal.com) using the reciprocal value of the standard deviation of hue (SDHue) of the scanned chewing gum wafer as a measure for chewing efficiency (Halazonetis et al., 2013).
Maximum voluntary bite force (N) was recorded at all time points with the Occlusal Force-Meter GM 10 (Nagano Keiki, Tokyo, Japan). The gauge has an 8.7-mm-thick bite element, which was placed unilaterally in the first molar region; dentures were stabilized with a contralateral bite element of the same thickness. The participants were asked to bite as hard as possible 6 times; for analysis, the right and left peak forces were averaged.
Denture satisfaction was evaluated with visual analog scale (DS-VAS) scores as described by Rashid et al. (2011); the patient is asked to respond to 24 predefined questions using 10-mm scales. High DS-VAS scores indicate elevated denture satisfaction. Oral health–related quality of life was assessed with the Oral Health Impact Profile–EDENT (Allen and Locker, 2002). This instrument contains 20 questions on functional limitations, pain, and physical and psychological disabilities; high scores indicate a low oral health–related quality of life.
Denture stability was judged clinically on a scale from 0 (no retention) to 3 (good retention). Masseter muscle thickness in contracted muscle condition was measured by means of linear ultrasound at baseline, 3 months and 12 months, and the preferred chewing side was noted (Schimmel et al., 2010). Stimulated saliva flow rate was assessed after chewing on paraffin (CRT, Ivoclar Vivadent) for 2 minutes and continuous collection of saliva.
Statistical Analysis
Because of the lack of available data in the literature, an interim power analysis was performed after the inclusion of the first 13 subjects on the main outcome variable: DS-VAS. According to this analysis, group sample sizes of 12 each would detect a significant difference (p < .05, 1 – β = 0.8). Normal distribution was tested using Shapiro-Francia W′ tests, and nonnormal distributed variables were successfully transformed (Appendix Table). The 2 groups were compared at baseline with t tests or Fisher’s exact test, as appropriate. Longitudinal data were analyzed according to the intention-to-treat concept (with data imputation) with linear mixed-effects regression models—STATA command xtmixed (p < .05); STATA 12.1 (STATA Corporation, College Station, TX, USA)—with time points, intervention, and the interaction term as exploratory variables.
Results
The intervention group comprised 9 women and 7 men (mean age, 85.0 ± 6.19 yrs, range 75-92 yrs), and the control group consisted of 14 women and 4 men (mean age, 84.1 ± 5.55 yrs, range 76-96 yrs). The groups were not different at baseline (Table 1).
Table 1.
Comparison of the Intervention and Control Groups at Baseline for Verification of Randomization Feasibility
| Intervention Group | Control Group | p | |
|---|---|---|---|
| Sex | 9 women, 7 men | 14 women, 4 men | .274 |
| Age, yrs | 85.0 ± 6.19 | 84.1 ± 5.55 | .6639 |
| Edentulous since, yrs | 11.1 ± 8.36 | 19.1 ± 14.19 | .0525 |
| Dentures’ time in function, yrs | 9.3 ± 9.64 | 11.2 ± 9.75 | .5793 |
| Geriatric Depression Scale | 3.9 ± 3.34 | 3.8 ± 3.15 | .9705 |
| Mini-Mental State Examination | 24.3 ± 4.25 | 23.5 ± 5.38 | .6317 |
| Instrumental Activities of Daily Living Scale | 10.8 ± 4.65 | 12.4 ± 5.93 | .3763 |
| Denture satisfaction–visual analog scale, Σmm | 749.4 ± 435.1 | 948.7 ± 497.53 | .2218 |
| Oral Health Impact Profile–EDENT, Σ | 41.1 ± 20.31 | 32.9 ± 20.84 | .2524 |
| Denture stability | 0.4 ± 0.65 | 0.4 ± 0.62 | .8191 |
| Chewing efficiency (SDHue) | 1.310 ± 0.265 | 1.157 ± 0.172 | .0845 |
| Maximum voluntary bite force, N | 18.0 ± 17.36 | 27.8 ± 28.41 | .2505 |
| Masseter muscle thickness–preferred chewing side, mm | 11.3 ± 1.92 | 10.7 ± 1.89 | .3571 |
| Masseter muscle thickness–nonpreferred chewing side, mm | 11.2 ± 1.955 | 10.7 ± 1.68 | .4772 |
| Stimulated saliva flow rate, mL | 2.2 ± 1.4 | 1.6 ± 1.1 | .1818 |
| Mini Nutritional Assessment | 17.0 ± 5.64 | 17.61 ± 4.51 | .7188 |
| Body mass index, kg/m2 | 24.9 ± 4.33 | 23.69 ± 3.37 | .3734 |
| Albumin, g/L | 40.4 ± 6.55 | 39.3 ± 5.40 | .5897 |
| Vitamin B12, pmol/L | 331.4 ± 329.08 | 331.44 ± 177.38 | .9994 |
| Folic acid, nmol/L | 13.4 ± 4.34 | 12.4 ± 4.79 | .5041 |
| Hemoglobin (blood markers), g/L | 135.8 ± 10.86 | 127.0 ± 15.24 | .0595 |
| C-reactive protein, mg/L | 5.9 ± 7.12 | 12.1 ± 18.31 | .2003 |
All implants were successful according to the applied criteria, and no implant was lost; however, 2 IOD patients were deceased after 3 months. The Locator attachments were difficult to handle for some patients and their caregivers, despite the extra-light retention insert (i.e., red, 230g retentive force); in fact, at insertion, sometimes the black laboratory insert was used. In 2 cases, they were replaced by ball attachments after 3 months.
IODs were significantly more stable (interaction term: p < .0001), and IOD patients were significantly more satisfied (DS-VAS, interaction term: p < .0001). Furthermore, they showed an improved oral health–related quality of life (Oral Health Impact Profile–EDENT, interaction term: p < .035) than patients who had received a conventional reline (Table 2, Appendix Table). Patients with IODs developed significantly higher maximum voluntary bite forces (interaction term: p < .0001), yet the chewing efficiency was not different between groups (standard deviation of hue, interaction term: p > .059). However, in the intervention group, masseter muscle thickness on the preferred chewing side increased but remained unchanged in the control group (interaction term: p = .028). The intervention had no influence on stimulated saliva flow rate.
Table 2.
Primary Outcome Measure (Denture Satisfaction–Visual Analog Scale) from the One-year Observation Period for the Intervention and Control Groups
| Intervention |
3 Months |
12 Months |
||||
|---|---|---|---|---|---|---|
| Intervention |
Control |
Intervention |
Control |
Intervention |
Control |
|
| n = 16 | n = 18 | n = 16 | n = 16 | n = 14 | n = 8 | |
| DS-VAS, Σmma,b | 749.4 ± 435.12c | 948.7 ± 497.53c | 1706.75 ± 565.35 | 1162.78 ± 482.88 | 1687.9 ± 596.39 | 1145.28 ± 519.62 |
| OHIP-EDENT, Σa,b | 41.1 ± 20.31c | 32.9 ± 20.84c | 20.9 ± 16.74 | 25.9 ± 13.46 | 21.9 ± 22.06 | 23.44 ± 13.82 |
| Denture stabilitya,b | 0.4 ± 0.65c | 0.37 ± 0.62c | 2.7 ± 0.70 | 1.2 ± 0.79 | 2.6 ± 0.81 | 1.1 ± 0.76 |
| SDHue | 1.490 ± 0.283 | 1.150 ± 0.139 | 1.521 ± 0.471 | 1.246 ± 0.269 | 1.328 ± 0.387 | 1.192 ± 0.221 |
| MBF, Nb | 44.3 ± 38.22 | 21.2 ± 26.95 | 62.8 ± 54.65 | 25.25 ± 29.25 | 73.0 ± 78.01 | 26.4 ± 28.39 |
| MMT-preferred, mmb | 11.3 ± 1.92c | 10.7 ± 1.89c | 11.7 ± 1.98 | 10.7 ± 1.82 | 11.7 ± 2.19 | 10.7 ± 1.87 |
| MMT-nonpreferred, mm | 11.2 ± 1.96c | 10.7 ± 1.68c | 11.6 ± 2.10 | 10.8 ± 1.52 | 11.5 ± 2.15 | 10.8 ± 1.55 |
| SSFR, mL | 1.9 ± 1.13 | 1.8 ± 1.20 | 2.0 ± 1.32 | 1.68 ± 1.17 | 1.88 ± 1.25 | 1.75 ± 1.35 |
| MNA | 17.0 ± 5.64c | 17.6 ± 4.51c | 16.4 ± 4.84 | 18.9 ± 4.68 | 16.3 ± 4.95 | 18.2 ± 4.80 |
| BMI, kg/m2a | 24.9 ± 4.33c | 23.69 ± 3.37c | 25.0 ± 4.39 | 23.7 ± 3.50 | 24.7 ± 4.14 ± | 23.3 ± 3.65 |
| Albumin, g/L | 40.4 ± 6.56c | 39.3 ± 5.40c | 39.3 ± 5.47 | 38.7 ± 4.04 | 38.9 ± 5.05 | 38.3 ± 4.78 |
| Vitamin B12, pmol/L | 331.4 ± 329.08c | 331.4 ± 177.39c | 265.6 ± 145.46 | 339.5 ± 212.32 | 356.5 ± 293.24 | 310.0 ± 159.16 |
| Folic acid, nmol/l | 13.4 ± 4.34c | 12.36 ± 4.79c | 11.9 ± 4.63 | 11.1 ± 5.55 | 14.9 ± 9.91 | 10.5 ± 5.23 |
| HB, g/Ld | 135.8 ± 10.86c | 127.0 ± 15.24c | 134.3 ± 10.34 | 128.2 ± 11.90 | 132.6 ± 12.18 | 126.6 ± 12.01 |
| CRP, mg/L | 5.9 ± 7.12c | 12.1 ± 18.31c | 20.6 ± 43.81 | 5.5 ± 6.01 | 7.8 ± 13.04 | 5.04 ± 5.34 |
In addition to the primary outcome measure (denture satisfaction–visual analog scale [DS-VAS]), further secondary outcome measures were the Oral Health Impact Profile–EDENT (OHIP-EDENT), denture stability, chewing efficiency (standard deviation of hue [SDHue]), maximum voluntary bite force (MBF), masseter muscle thickness (MMT; preferred/nonpreferred chewing side), stimulated saliva flow rate (SSFR), as well as nutritional parameters such as the Mini Nutritional Assessment (MNA), the body mass index (BMI), and various blood markers (Hb). Missing data were imputed according to the “last value carried forward” method; the intention-to-treat population was n = 16 (intervention group) and n = 18 (control group).
Significant time effect.
Significant interaction term (time × treatment).
Carried forward from BL.
Significant treatment effect.
The statistical model revealed a significant decrease in body mass index for both groups (time effect: p = .049), but the decline tended to be smaller in the intervention group. The Mini Nutritional Assessment and the blood markers did not confirm this tendency (all non-significant, Appendix Table).
Discussion
Numerous studies reported that IODs have a 5- to 10-year survival rate above 90%, are clinically successful, and offer a substantial benefit to the patient from a functional, structural, as well as psychosocial point of view (Thomason et al., 2009). However, most studies looked into “young old” patients with an average age younger than 70 yrs (Andreiotelli et al., 2010). The benefit of IODs may be even more evident in the “old old” than in the “young old,” where the functional shortcomings of complete dentures can be better compensated (Müller and Hasse-Sander, 1993).
High success and survival rates of IODs in patients older than 80 yrs were reported but mostly in independently living individuals (Grant and Kraut, 2007) or for fixed implant-supported prostheses (Kowar et al., 2013). The current study extends the evidence to very old patients who depend on help for the activities of daily living. Unexpectedly, the Locator attachments proved difficult to handle, as the inner part easily blocks with food debris, thus precluding the correct seating of the overdenture. Furthermore, the attachment often proved too tight, especially in patients with arthritis and/or age-related muscle weakness. The Locator attachment seems therefore not ideal for frail and dependent patients. Nevertheless, the proposed conversion of conventional lower complete dentures to IODs proved feasible and successful even in dependent elderly individuals.
It is noteworthy that 7 participants withdrew from the study after they had been randomized to receive dental implants free of charge. Elderly patients often object to implant treatment, mainly motivated by the fear of surgery and pain or an unperceived need for improvement (Müller and Hasse-Sander, 1993; Ellis et al., 2011). Risk factors for a negative attitude lie also in the lack of knowledge or the loss of autonomy (Müller et al., 2011). Walton and MacEntee (2005) reported a 35% refusal rate even if the implants were free of charge.
The investigated treatment concept implies a moderate surgical intervention with short implants. A recent literature review confirmed high survival rates even for very short implants (Srinivasan et al., 2013). By transforming the existing denture to an IOD, the involved cost and treatment sessions were kept at a minimum. The balanced benefit-risk ratio of the proposed treatment concept makes it particularly suitable for very old edentulous patients. Future treatment concepts may even use a single implant in the mandibular midline, but long-term survival data are still missing (Walton et al., 2009).
Considering the complexity of complete denture care for patients of advanced age, such patients present a considerable challenge to the practitioner. Although complete dentures can replace most lost tissues and thus satisfy aesthetic and phonetic demands, they fail to fully restore the lost function. Chewing capacity and bite force remain substantially impaired, yet enjoying food gains importance while other pleasures fade.
The current study has evident shortcomings due to the complexity of logistics, the patients’ health and motivation, as well as some caring institutions’ compliance. Thus, recruitment took longer than expected, and the study had to be terminated while still underpowered for some secondary outcome measures. Nevertheless, it provides evidence that even in very old patients, IODs offer substantial benefits: an effect that is well known for younger age cohorts (Feine et al., 1994). Although maximum voluntary bite force increased significantly in the intervention group, in contrast to younger patients, the chewing efficiency did not improve. Age-related decline of motor coordination and abraded denture teeth might have accounted for this finding. The proposed treatment concept intentionally used the existing dentures to keep the cost and intervention time at a minimum. However, renewing abraded occlusal surfaces would not require additional chairside time; only the cost of treatment would increase. In view of the results of this study, renewal of the occlusal surfaces of the denture teeth should be recommended when wear seems to limit the chewing efficiency.
The question arises whether improved denture stability induces a “training effect” for the chewing muscles. Physiologic aging leads to a 40% decrease of masseter muscle cross-sectional area from the age of 20 to 89 yrs (Newton et al., 1987). It was demonstrated that resistance training in elderly institutionalized persons is effective in regaining atrophied muscle bulk and force of the lower limb (Tokmakidis et al., 2009). The current study provides, for the first time, evidence that a similar effect exists for the chewing muscles after denture stabilization by means of dental implants.
Although subjectively often unnoticed, edentulism leads to adjusting the food choice to what is feasible to chew (Sheiham et al., 2001). Malnutrition has a prevalence of 5% to 8% of independently living persons but can increase up to 30% to 60% in the institutionalized population (Guigoz et al., 1994).
The meals, however, are of increasing importance late in life, not only from a nutritional but also from a social point of view. Twenty-nine percent of persons in a British survey claimed “eating” as important for their quality of life (McGrath and Bedi, 2002); the importance of oral health on the well-being and life satisfaction of residents in a long-term care facility was demonstrated (Locker and Allen, 2002).
Various attempts have been made by geriatricians to battle weight loss to reduce morbidity, but dental interventions have rarely been studied within this context. In independently living persons, improving chewing efficiency by dental restorative measures alone rarely changes the diet (Hamdan et al., 2013). The patients of the current study received help for their activities of daily living; thus, their nutritional intake was no longer a “free choice.” However, neither the patients nor the carers were invited to change or improve the diet following the intervention. Furthermore, chewing efficiency proved not significantly improved in the intervention group, indicating that food choice would have probably not been much different. Last but not least, the study may be underpowered to show a significant difference for this secondary outcome measure.
Conclusions
Stabilizing existing lower dentures by means of 2 short regular-diameter interforaminal implants in very old edentulous patients who are dependent for the activities of daily living provides significantly higher denture satisfaction than that of a conventional reline. Therefore, the hypothesis has to be rejected. High survival and success rates confirm the feasibility of the IOD treatment concept. However, the choice of attachments should be adapted to the patient’s manual force and dexterity, which should be monitored. The increased maximum voluntary bite force and masseter muscle bulk indicate a functional and morphologic benefit from this treatment, even for very old patients. However, the inconsistent findings in body mass index, Mini Nutritional Assessment, and blood markers reflect that nutritional intake is complex and not solely determined by the dental state.
Acknowledgments
The help of Dr. Manfred Imsand in developing the study protocol and placing implants is greatly acknowledged.
Footnotes
The study was supported by the ITI Foundation (grant 458_2006).
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
References
- Allen F, Locker D. (2002). A modified short version of the oral health impact profile for assessing health-related quality of life in edentulous adults. Int J Prosthodont 15:446-450 [PubMed] [Google Scholar]
- Andreiotelli M, Att W, Strub JR. (2010). Prosthodontic complications with implant overdentures: a systematic literature review. Int J Prosthodont 23:195-203 [PubMed] [Google Scholar]
- Awad MA, Locker D, Korner-Bitensky N, Feine JS. (2000). Measuring the effect of intra-oral implant rehabilitation on health-related quality of life in a randomized controlled clinical trial. J Dent Res 79:1659-1663 [DOI] [PubMed] [Google Scholar]
- Buser D, Weber HP, Lang NP. (1990). Tissue integration of non-submerged implants: 1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res 1:33-40 [DOI] [PubMed] [Google Scholar]
- Ellis JS, Levine A, Bedos C, Mojon P, Rosberger Z, Feine J, et al. (2011). Refusal of implant supported mandibular overdentures by elderly patients. Gerodontology 28:62-68 [DOI] [PubMed] [Google Scholar]
- Feine JS, Maskawi K, de Grandmont P, Donohue WB, Tanguay R, Lund JP. (1994). Within-subject comparisons of implant-supported mandibular prostheses: evaluation of masticatory function. J Dent Res 73:1646-1656 [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. (1975). “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189-198 [DOI] [PubMed] [Google Scholar]
- Grant BT, Kraut RA. (2007). Dental implants in geriatric patients: a retrospective study of 47 cases. Implant Dent 16:362-368 [DOI] [PubMed] [Google Scholar]
- Guigoz Y, Vellas B, Garry PJ. (1994). Mini Nutritional Assessment: a practical assessment tool for grading the nutritional state of elderly patients. In: The Mini Nutritional Assessment: Facts and Research in Gerontology (Suppl I). Paris, France: Serdi, pp. 15-60 [Google Scholar]
- Halazonetis DJ, Schimmel M, Antonarakis GS, Christou P. (2013). Novel software for quantitative evaluation and graphical representation of masticatory efficiency. J Oral Rehabil 40:329-335 [DOI] [PubMed] [Google Scholar]
- Hamdan N, Albuquerque R, Gray-Donald K, Feine J. (2013). A mandibular implant overdenture: is it a nutritionally significant choice? J Dent Res 92(Spec Iss A):0231 [Google Scholar]
- Kowar J, Eriksson A, Jemt T. (2013). Fixed implant-supported prostheses in elderly patients: a 5-year retrospective comparison between partially and completely edentulous patients aged 80 years or older at implant surgery. Clin Implant Dent Relat Res 15:37-46 [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody EM. (1969). Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179-186 [PubMed] [Google Scholar]
- Locker D, Allen PF. (2002). Developing short-form measures of oral health-related quality of life. J Public Health Dent 62:13-20 [DOI] [PubMed] [Google Scholar]
- McGrath C, Bedi R. (2002). Understanding the value of oral health to people in Britain: importance to life quality. Community Dent Health 19:211-214 [PubMed] [Google Scholar]
- Müller F, Hasse-Sander I. (1993). Experimental studies of adaptation to complete dentures related to ageing. Gerodontology 10:23-27 [DOI] [PubMed] [Google Scholar]
- Müller F, Salem K, Barbezat C, Herrmann FR, Schimmel M. (2011). Knowledge and attitude of elderly persons towards dental implants. Gerodontology 29:e914-e923 [DOI] [PubMed] [Google Scholar]
- Müller F, Hernandez M, Grütter L, Aracil-Kessler L, Weingart D, Schimmel M. (2012). Masseter muscle thickness, chewing efficiency and bite force in edentulous patients with fixed and removable implant-supported prostheses: a cross-sectional multicenter study. Clin Oral Implants Res 23:144-150 [DOI] [PubMed] [Google Scholar]
- Newton JP, Abel EW, Robertson EM, Yemm R. (1987). Changes in human masseter and medial pterygoid muscles with age: a study by computed tomography. Gerodontics 3:151-154 [PubMed] [Google Scholar]
- Rashid F, Awad MA, Thomason JM, Piovano A, Spielberg GP, Scilingo E, et al. (2011). The effectiveness of 2-implant overdentures: a pragmatic international multicentre study. J Oral Rehabil 38:176-184 [DOI] [PubMed] [Google Scholar]
- Schimmel M, Christou P, Herrmann FR, Müller F. (2007). A two-colour chewing gum test for masticatory efficiency: development of different assessment methods. J Oral Rehabil 34:671-678 [DOI] [PubMed] [Google Scholar]
- Schimmel M, Leemann B, Christou P, Schnider A, Müller F, Kiliaridis S. (2010). Masseter muscle thickness in hospitalised stroke patients. J Oral Rehabil 37:726-730 [DOI] [PubMed] [Google Scholar]
- Sheiham A, Steele JG, Marcenes W, Lowe C, Finch S, Bates CJ, et al. (2001). The relationship among dental status, nutrient intake, and nutritional status in older people. J Dent Res 80:408-413 [DOI] [PubMed] [Google Scholar]
- Sheikh J, Yesavange J. (1986). Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. In: Clinical Gerontology: A Guide to Assessment and Interventions; Bring TL, editor. New York, NY: Haworth Press, pp. 165-173 [Google Scholar]
- Srinivasan M, Vazquez L, Rieder P, Moraguez O, Bernard JP, Belser UC. (2013). Survival rates of short (6 mm) micro-rough surface implants: a review of literature and meta-analysis [published online February 18, 2013]. Clin Oral Implants Res. [DOI] [PubMed] [Google Scholar]
- Thomason JM, Feine J, Exley C, Moynihan P, Müller F, Naert I, et al. (2009). Mandibular two implant-supported overdentures as the first choice standard of care for edentulous patients: the York Consensus Statement. Br Dent J 207:185-186 [DOI] [PubMed] [Google Scholar]
- Tokmakidis SP, Kalapotharakos VI, Smilios I, Parlavantzas A. (2009). Effects of detraining on muscle strength and mass after high or moderate intensity of resistance training in older adults. Clin Physiol Funct Imaging 29:316-319 [DOI] [PubMed] [Google Scholar]
- Walton JN, MacEntee MI. (2005). Choosing or refusing oral implants: a prospective study of edentulous volunteers for a clinical trial. Int J Prosthodont 18:483-488 [PubMed] [Google Scholar]
- Walton JN, Glick N, Macentee MI. (2009). A randomized clinical trial comparing patient satisfaction and prosthetic outcomes with mandibular overdentures retained by one or two implants. Int J Prosthodont 22:331-339 [PubMed] [Google Scholar]
- Weiss A, Beloosesky Y, Boaz M, Yalov A, Kornowski R, Grossman E. (2008). Body mass index is inversely related to mortality in elderly subjects. J Gen Intern Med 23:19-24 [DOI] [PMC free article] [PubMed] [Google Scholar]