Abstract
For the restoration of an anterior missing tooth, implant-supported single crowns (ISCs) or fixed dental prostheses (FDPs) are indicated, but it is not clear which type of restoration is more cost-effective. A self-selected trial was performed with 15 patients with ISCs and 11 with FDPs. Patient preferences were recorded with visual analog scales before treatment, 1 month following restoration, and then annually. Quality-adjusted tooth years (QATYs) were estimated by considering the type of reconstruction for replacing the missing tooth and its effect on the adjacent teeth. A stochastic cost-effectiveness model was developed using Monte Carlo simulation. The expected costs and QATYs were summarized in cost-effectiveness acceptability curves. ISC was the dominant strategy, with a QATY increase of 0.01 over 3 years and 0.04 over 10 years with a higher probability of being cost-effective. While both treatment options provided satisfactory long-term results from the patient’s perspective, the lower initial costs, particularly laboratory fees, were responsible for the dominance of ISCs over FDPs.
Keywords: dental economics, cost effectiveness, single-tooth implants, fixed partial denture, dental restoration, patient satisfaction
Introduction
For restoring a single missing tooth, dental implants have been established as an alternative to the conventional 3-unit fixed dental prostheses (FDPs) or adhesive bridges. The FDP is retained by the prepared neighboring abutment teeth, while the implant-supported single crown (ISC) stands on its own. The decisive clinical factors for the treatment selection are the conditions of the adjacent teeth, the soft and hard tissue situation (including potential needs for tissue augmentation), the preservation of adjacent anatomical structures, and the available space (Zitzmann et al., 2010). Aesthetic concerns play a major role, particularly in the maxillary anterior region, and the effects of the treatment on the soft tissue contour in patients with a high lip line exposing this region must be considered. Additional decisive factors are the patients’ desires and preferences, as well as their general compliance in further pretreatment efforts if required. The final decision is made by the patient, who has to be thoroughly informed about the pros and cons of the different treatment options in the particular situation. Objective criteria include longevity and prognosis of the treatment planned, costs, and expected maintenance efforts. A recent willingness-to-pay study found that the majority of subjects would prefer implant treatment if they were missing any anterior teeth (Leung and McGrath, 2010).
In general, the annual failure rates of both treatment modalities, ISC and FDP, are approximately 1%, which corresponds to a 5- and 10-year survival of 93.8% and 89.2% for FDP and 94.5% and 89.4% for ISC, respectively (Pjetursson et al., 2012). During maintenance, biological complications dominated in both types of restorations, with caries or loss of pulp vitality being most frequent among FDPs, while peri-implantitis or soft tissue complications affected ISCs (Pjetursson et al., 2012). The incidence of technical complications was significantly higher for implant-supported, rather than for tooth-supported, reconstructions. For ISC, the most frequent complications comprised chipping or fracture of the veneering material, abutment or occlusal screw loosening, and loss of retention, whereas for FDPs, chipping or fracture of the veneering and framework fractures dominated (Pjetursson et al., 2012). Furthermore, costs are, in most countries, slightly lower for implant treatment than for FDP but may vary depending on the pretreatment required. Because of these similarities, the treatment decision cannot be clearly based on longevity or financial aspects, and cost-effectiveness cannot be determined by simply comparing costs and long-term success. ISC and FDP have been compared in a preference trial, in which the direct costs recorded included initial and maintenance costs and the indirect costs included the number of visits and hours spent on treatment or maintenance issues during a 1- to 4-year observation period (Brägger et al., 2005). The authors demonstrated that FDP involved higher total costs mainly due to the laboratory work and concluded that ISC was preferable from an economic viewpoint.
The aim of the current study was to draw on previous research to compare the long-term cost-effectiveness of implant treatment to restore a single missing tooth with that of the conventional 3-unit FDP. A probabilistic model was used in the analysis, and patients’ preferences were taken into account.
Materials & Methods
The study was designed as a prospective preference trial (self-selected trial) in which the informed patient decided on the treatment selection. Treatment was performed within the combined surgical and restorative postgraduate program at the Department of Periodontology, Endodontology, and Cariology and the Department of Oral Surgery, Oral Radiology, and Oral Medicine at the University of Basel, Switzerland. Each patient was informed orally and in writing about the different treatment options and individual pretreatment needs and given a cost estimation. Inclusion criteria were the need for tooth replacement in the maxillary anterior region, including first premolars. Apart from general contraindications for implant surgery, no exclusion criteria were applied, and all patients who were willing to visit the clinics for at least a 3-year recall period were included. The study was approved by the local Ethics Research Committee (reference No. 173/05), and all patients signed a consent form. Patients were asked to fill out a questionnaire to evaluate how they perceived their missing teeth as well as their mesial and distal adjacent teeth. The 3 regions were then assessed on a visual analog scale (VAS; baseline). Patients received a written explanation of the endpoints of the VAS and instructions on the aesthetics, function, mucosal contour, and appearance of the clinical crown.
A total of 26 patients were included (October 2007 to May 2009), of whom 15 selected ISC (group 1) and 11 selected FDP (group 2). Depending on the soft and hard tissue contour, the implant design (8 × Standard Plus, 7 × Bone Level, Straumann, Basel, Switzerland) was selected, and implants were placed at least 6 weeks after tooth extraction. Simultaneous bone augmentation was used in 5 patients to cover exposed buccal implant surfaces. Restoration of the implant site was scheduled 2 to 4 months after implant insertion and comprised impression taking at implant level, abutment, and/or framework and bisque bake try-in. If feasible, screw-retained restorations were selected (8×), while individualized titanium (1×) or zirkoniumoxide abutments (6×) were used for cemented implant crowns. For FDP, egg-shell provisonals were preprepared by the dental technician and adjusted after abutment preparation. Impressions were taken at the earliest 2 weeks later. The metal framework and bisque bake were tried in, and the FDPs were designed with circular porcelain margins.
To investigate the treatment results, patients’ perception were further evaluated 1 month after completing the treatment and then annually. Initial total costs and maintenance costs for scheduled recall visits or unscheduled visits due to emergencies were recorded.
Statistical Analysis
All data were first analyzed descriptively. Between-group differences of continuous variables were assessed using the t test and Wilcoxon rank-sum test, while categorical variables were compared with the chi-square test. All descriptive and inferential statistical analyses were performed using Stata 11.0 (StatCorp, College Station, Texas).
Cost-effectiveness Analysis
To compare the costs and effects of ISC with those of 3-unit FDP, their cost-effectiveness was analyzed from a health care perspective. Treatment and maintenance costs were estimated in 2008 Swiss francs (CHF 100 = US$93). Effects were estimated as quality-adjusted tooth years (QATYs). One QATY corresponds to a sound tooth over a 1-year period (Sendi et al. 1997; Birch and Ismail, 2002). Cost-effectiveness was analyzed over a time horizon of 3, 5, and 10 years using an annual discount rate of 3%.
Modeling Effects
QATYs were estimated by considering the type of reconstruction used to replace the missing tooth and its effect on the adjacent teeth. A value of 0% indicated the worst situation (e.g., tooth missing, existing crown aesthetically unacceptable or functional use not feasible), while 100% represented the best possible situation with an intact, healthy natural tooth or a restoration with ideal color and form and fully satisfactory aesthetics and function. For the missing tooth, the VAS at baseline (before treatment) was defined as zero. At each observation time point, the 3 VAS scores of the replaced and adjacent teeth were averaged to estimate the overall effect of the treatment strategy. To account for possible differences in baseline utility for the adjacent teeth in the 2 groups, baseline VAS scores were adjusted using a generalized linear model with an inverse Gaussian identity link. The importance of adjusting for baseline utility to account for ex ante between-group differences in patient preferences is described in detail (Manca et al. 2005).
Modeling Costs
Treatment costs were estimated using microcosting based on the Swiss tariff for dental treatments (surgical and reconstructive) and laboratory fees. For the follow-up and maintenance costs, resource use was estimated, taking into account an annual recall examination with sensitivity testing, periodontal examination, periapical radiographs, occlusal control, professional cleaning, and oral hygiene instructions. A Swiss tariff tax point value of 3.7 was applied for costing procedures (SSO tariff list; i.e., Swiss Dental Association [Société Suisse d’Odonto-Stomatologie]).
Probabilistic Model
To capture any variability in costs and effects, a stochastic cost-effectiveness model was developed by defining distributions for the cost parameters and VAS scores used in our model. Variability in expected treatment costs was captured by using a normal distribution and the corresponding standard error for expected costs in each treatment group. Variability in maintenance costs was acquired by defining a triangular distribution with the likeliest value based on the actual Swiss tariff used for our patients, leading to an annual maintenance cost of CHF 140 and a range between CHF 117 and 188 by varying the Swiss tariff between 3.1 (social insurance tariff) and 4.9 (upper limit for cost estimation). Based on the complications found during the observation period in 2 out of 15 patients with ISC, which caused additional treatment costs of CHF 200 per patient, an estimated amount of CHF 27 was added to the maintenance costs (CHF 400/15) in the third and following years. The VAS scores and maintenance cost estimates for the third year were used for modeling outcomes in the subsequent years, taking into account that complications were also observed after 4 and 6 years. The cost-effectiveness analysis was projected over a time horizon of 5 and 10 years in a sensitivity analysis.
All the distributions defined in the model were sampled 10,000 times in a Monte Carlo simulation, and the expected costs and QATYs were calculated for each sample, yielding a distribution for costs and effects for each of the 3 time horizons modeled. These distributions were summarized in the form of cost-effectiveness acceptability curves, which describe the probability that the intervention is cost-effective given the ceiling ratio—that is, the decision maker’s maximum willingness to pay for a QATY (van Hout et al., 1994). The software package TreeAge Pro 2012 (TreeAge Software, Williamstown, Massachusetts) was used for the cost-effectiveness analysis.
Results
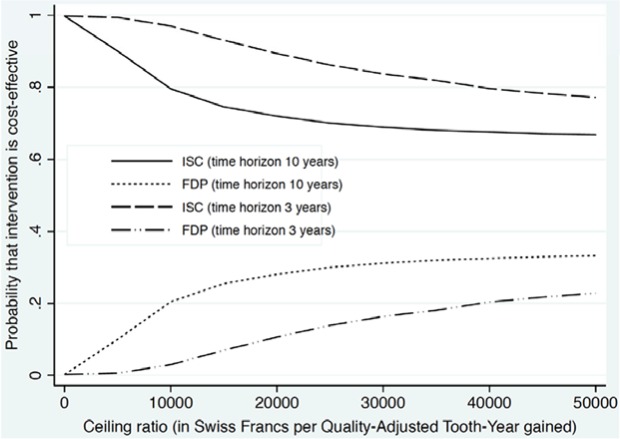
The site distributions in the 2 groups are shown in Figure 1. The total initial costs for ISC were CHF 4498 ± 632, including CHF 1582 ± 401 for the laboratory fees, while FDPs costs amounted to CHF 5082 ± 432, with CHF 2402 ± 283 for laboratory fees. Mean observation time was 50.6 months (range, 38-71) in group 1 and 48.9 months (range, 37-69) in group 2 (Table 1). In addition to the annual follow-up, 2 unscheduled visits were recorded due to a biological complication and a technical complication in group 1. In 1 patient, palatal soft tissue swelling occurred during the fourth year around the implant in the canine region and required professional cleaning. The technical complication with loss of the screw access filling occurred in a screw-retained canine implant during the 6th year. Both interventions caused additional costs of CHF 200 per patient.
Figure 1.
Site distribution (tooth number, American system) for implant-supported single crowns (ISCs) and 3-unit fixed dental prostheses (FDPs).
Table 1.
Baseline Characteristics and Cost-and-Effect Estimates for the 2 Treatment Groups
| Variable | Group 1: ISC n = 15 | Group 2: FDP n = 11 | p |
|---|---|---|---|
| Age, y | 49.8 (13.9) | 42.8 (18.9) | .39 |
| Males, % (n) | 40 (6) | 72.7 (8) | .09 |
| Mean observation time, mo | 50.6 (11.6) | 48.9 (9.8) | .69 |
| Treatment costs overall | 4498 (632) | 5082 (432) | .02 |
| Laboratory fees | 1581 (401) | 2402 (283) | < .001 |
| Dental health state preferencea | |||
| At baseline | |||
| Mesial tooth | 84.2 (15.1) | 66.4 (26.7) | .09 |
| Distal tooth | 87.3 (12.2) | 65.3 (35.0) | .13 |
| After 1 month | |||
| Mesial tooth | 91.8 (10.2) | 92.0 (11.16) | .96 |
| Distal tooth | 90.7 (12.9) | 88.8 (11.6) | .69 |
| Replaced tooth | 92.0 (10.2) | 93.8 (8.8) | .63 |
| After 1 year | |||
| Mesial tooth | 93.2 (7.8) | 91.9 (9.5) | .69 |
| Distal tooth | 93.8 (8.5) | 92.5 (9.0) | .73 |
| Replaced tooth | 94.2 (8.8) | 93.5 (7.6) | .82 |
| After 2 years | |||
| Mesial tooth | 93.3 (6.4) | 93.7 (9.6) | .88 |
| Distal tooth | 94.1 (6.1) | 93.2 (8.9) | .76 |
| Replaced tooth | 93.9 (4.9) | 95.0 (7.4) | .66 |
| After 3 years | |||
| Mesial tooth | 93.5 (6.4) | 92.8 (9.8) | .83 |
| Distal tooth | 94.2 (5.8) | 92.8 (9.8) | .65 |
| Replaced tooth | 94.9 (4.4) | 94.2 (7.9) | .78 |
| Total effects in QATYs, 1-3 y | 2.82 (0.16) | 2.80 (0.24) | .82 |
Mean (SD), unless noted otherwise.
ISC, implant-supported single crown; FDP, fixed dental prosthesis; QATY, quality-adjusted tooth year.
Visual analog scale.
Patient preferences for the 3 teeth at baseline and during recall are shown in Table 1. Baseline data before treatment revealed lower ratings of the adjacent teeth in group 2 (66.4 and 65.3) than in group 1 (84.2 and 87.3), but these differences were not statistically significant. One month after insertion of the restoration, patients’ estimations were improved for all sites with the highest scores for the replaced tooth site in both groups. The total effects in QATY over 3 years amounted to 2.82 ± 0.16 in group 1 and 2.80 ± 0.24 in group 2 (p = .82).
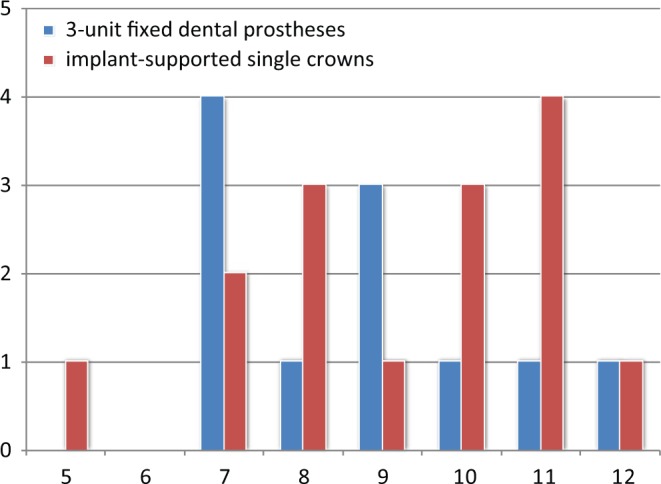
According to the cost-effectiveness analysis, implant treatment led to expected cost savings of CHF 584 (incremental costs), irrespective of the time horizon and discount rate used in the model (Table 2). Furthermore, implant treatment led to an increase in expected QATY of 0.01 over a time horizon of 3 years and 0.04 QATY over a time horizon of 10 years, indicating that implant treatment was the dominant strategy in the current analysis.
Table 2.
Incremental Cost-effectiveness Ratios of Implant Treatment versus Fixed Dental Prosthesis for Replacing a Single Missing Tooth
| Time Horizon: Discount Rate | Costsa | Effectsb | Incremental Costsa | Incremental Effectsb | Incremental Cost-effectiveness Ratioc |
|---|---|---|---|---|---|
| 3 y: 0% | 584 | −0.01 | Dominated | ||
| Group 1: ISC | 4795 | 2.81 | |||
| Group 2: FDP | 5379 | 2.80 | |||
| 3 y: 3% | 584 | −0.01 | Dominated | ||
| Group 1: ISC | 4782 | 2.73 | |||
| Group 2: FDP | 5366 | 2.72 | |||
| 5 y: 3% | 584 | −0.02 | Dominated | ||
| Group 1: ISC | 5099 | 4.43 | |||
| Group 2: FDP | 5683 | 4.41 | |||
| 10 y: 3% | 584 | −0.04 | Dominated | ||
| Group 1: ISC | 5814 | 8.25 | |||
| Group 2: FDP | 6398 | 8.21 |
Swiss francs.
Quality-adjusted tooth year.
Swiss francs per quality-adjusted tooth year.
ISC, implant-supported single crown; FDP, fixed dental prosthesis.
The cost-effectiveness acceptability curves for the 2 treatment strategies are shown in Figure 2. Under circumstances of uncertainty, implant treatment revealed a higher probability of being the preferred strategy, irrespective of the time horizon chosen (3 or 10 years).
Figure 2.
Cost-effectiveness acceptability curves for implant-supported single crowns (ISCs) versus fixed dental prostheses (FDPs).
Discussion
The current cost-effectiveness analysis indicated that ISCs have a higher probability of being cost-effective than FDPs over a 3- and 10-year time horizon. While both treatment options provided satisfactory long-term results from the patients’ perspective, with slightly higher QATYs and few complications in ISCs, the higher initial costs, particularly laboratory fees, were responsible for the disadvantageous economic outcome in FDPs.
The current study was designed as a preference trial where the patient selected the type of restoration after receiving detailed information and recommendations. For FDPs, possible adjustments of the abutment teeth in form and color are one advantage of this treatment option, particularly when the adjacent teeth are affected by some decay, when fillings are insufficient, or when the tooth color and/or shape changed. Treatment with ISCs is, however, not intended to affect the adjacent teeth but may accidentally result in changes in the soft tissue appearance, particularly in a loss of the papillary height. These aspects make it even more important to include the adjacent teeth in the assessment of the treatment outcomes and not to simply focus on the restoration in function as the only outcome parameter. Although the FDP option also allows the outcome of the adjacent teeth to be improved, this study did not find that the FDP is more cost-effective than the ISC. A recent cost-effectiveness analysis evaluated conventional denture treatments and implant overdentures in the edentulous mandible and found that implants led to greater improvements in dental health outcomes (quality-adjusted prosthesis years), but required substantially higher costs (Zitzmann et al., 2006). As in the present investigation, data were extrapolated over a 10-year time horizon with ceiling ratios per quality-adjusted prosthesis year gained becoming smaller with time.
Compared with edentulous patients, the situation of a single missing tooth in the aesthetic zone clearly requires more expensive fixed treatment solutions, with costs influenced by the national dental and laboratory tariff structures. Further costs may be involved in dealing with additional needs (e.g., provisional restorations in the ISC), although none were performed here in any group 1 patient. Leung and McGrath (2010) found that the willingness to pay for anterior tooth replacement was higher among subjects without missing teeth or restorative needs, women, and those with higher education. Since the starting point (with or without treatment needs) can greatly influence costs, median costs were used for willingness-to-pay analyses (Johannesson et al., 1996). In contrast, in the current cost-effectiveness analysis, real initial and maintenance costs were considered.
Our study has several limitations. First, the sample size may be considered rather small, which generally leads to higher variability in cost and effects, as can be seen from the shape of the cost-effectiveness acceptability curves in a probabilistic sensitivity analysis. Our results therefore show that, even under conditions of uncertainty, implant treatment has a higher probability of being cost-effective for all ceiling ratios. Second, the results of cost-effectiveness analyses are generally not transferable between countries, since cost estimates are usually country specific. For a between-country comparison, cost-effectiveness analyses would need to be conducted in different countries and settings. Third, one may argue that our clinical results only apply to a controlled academic setting and thus have low external validity. However, it seems reasonable to assume that patient satisfaction after treatment, as measured by VAS, may be similar to that in a general practice and that the analysis, performed from the patients’ perspective, coincides with the health care perspective in private dentistry.
Acknowledgments
We are grateful to Marina Naef for her help in collecting data as part of her undergraduate master thesis.
Footnotes
This study was supported in part by the International Team of Implantology, Switzerland (ITI Research Grant No. 440_2006).
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Birch S, Ismail AI. (2002). Patient preferences and the measurement of utilities in the evaluation of dental technologies. J Dent Res 81:446-450 [DOI] [PubMed] [Google Scholar]
- Brägger U, Krenander P, Lang NP. (2005). Economic aspects of single-tooth replacement. Clin Oral Implants Res 16:335-341 [DOI] [PubMed] [Google Scholar]
- Johannesson M, Jonsson B, Karlsson G. (1996). Outcome measurement in economic evaluation. Health Econ 5:279-296 [DOI] [PubMed] [Google Scholar]
- Leung KC, McGrath CP. (2010). Willingness to pay for implant therapy: a study of patient preference. Clin Oral Implants Res 21:789-793 [DOI] [PubMed] [Google Scholar]
- Manca A, Hawkins N, Sculpher MJ. (2005). Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 14:487-496 [DOI] [PubMed] [Google Scholar]
- Pjetursson BE, Zwahlen M, Lang NP. (2012). Quality of reporting of clinical studies to assess and compare performance of implant-supported restorations. J Clin Periodontol 39(suppl 12):139-159 [DOI] [PubMed] [Google Scholar]
- Sendi PP, Palmer AJ, Marinello CP. (1997). Health state utilities in dentistry: a review. Acta Med Dent Helv 2:243-248 [Google Scholar]
- van Hout BA, Al MJ, Gordon GS, Rutten FF. (1994). Costs, effects and C/E-ratios alongside a clinical trial. Health Econ 3:309-319 [DOI] [PubMed] [Google Scholar]
- Zitzmann NU, Marinello CP, Sendi P. (2006). A cost-effectiveness analysis of implant overdentures. J Dent Res 85:717-721 [DOI] [PubMed] [Google Scholar]
- Zitzmann NU, Krastl G, Hecker H, Walter C, Waltimo T, Weiger R. (2010). Strategic considerations in treatment planning: deciding when to treat, extract or replace a questionable tooth. J Prosthet Dent 104:80-91 [DOI] [PubMed] [Google Scholar]