Abstract
The aim of the study was to assess the efficacy of Kinesiology Taping (KT) for treating breast cancer-related lymphedema. Sixty-five women with unilateral stage II and III lymphedema were randomly grouped into the KT group (K-tapes, n = 20), the Quasi KT group (quasi K-tapes, n = 22), or the MCT group (multilayered compression therapy group, n = 23). Skin care, 45 min pneumatic compression therapy, 1 h manual lymphatic drainage, and application of K-tape/Quasi K-tapes/multilayered short-stretch bandages were given every treatment session, 3 times per week for 1 month. Patient evaluation items included limb size and percentage edema. Comparing the changes in K-tapes with quasi K-tapes changes, there were no significant differences (P > 0.05). The edema reduction of multilayered bandages was much better than in results observed in taping groups. The KT appeared to be ineffective at secondary lymphedema after breast cancer treatment. The single-blind, controlled pilot study results suggest that K-tape could not replace the bandage, and at this moment it must not be an alternative choice for the breast cancer-related lymphedema patient. The trial is registered with ACTRN12613001173785.
1. Introduction
Lymphedema is a chronic and progressive condition resulting from an abnormality or damage to the lymphatic system. It is marked by an abnormal increase of tissue proteins, edema, chronic inflammation, and fibrosis. Secondary lymphedema is caused by multiple factors related with lymphatic stasis, such as tumor lymph node infiltration, lymph node dissection, radiotherapy, trauma, and infection. Upper limb lymphedema occurs in 24–49% of the cases with total mastectomy and in 2.4–49% of the cases with axillary lymph node dissection [1, 2].
In Western Europe [3], upper limb secondary lymphedema has been reported in 22% of patients after breast cancer therapy. Lymphedema occurs when there is an imbalance due to reduced lymph transport capacity which leads to interstitial fluid and protein accumulation. It further leads to chronic inflammation and fibrosis caused by the secondary proliferation of neutrophils, macrophages, and fibroblasts and accumulation of collagen.
Physical therapy is a common management for lymphedema. A program combining skin care, manual lymphatic drainage, exercise, and compression therapy (multilayered bandage, intermittent pneumatic compression) is recognized as the best practice in lymphedema management. There have been numerous prospective investigations with different treatment frequency and duration showing the effect of physical therapy, which has been accepted as a standard “gold” therapy for many years [4–8].
However, standard care and management can have significant economic consequences. Bandage changes and expensive compression hosiery drain the available resources. Well-documented, promising, and inexpensive methods from alternative medicine are still needed [9–13].
Kinesiology Taping (KT) for lymphatic drainage is a new choice in the field of physical and alternative therapy. The material used for the Kinesio tape and the original concept of the taping technique were introduced by Dr. Kenso Kase in 1973. K-tape had been designed to allow 30–40% longitudinal stretch. It is composed of 100% cotton fibers and acrylic heat sensitive glue. Development of the technique for its administration is still ongoing. Dr. Kase claimed that applying K-tape would have physiological effects including decreasing pain or abnormal sensation, supporting the movement of muscles, removing congestion of lymphatic fluid or hemorrhages under the skin, and correcting misalignment of joints. After applying K-tape, the taped area will form convolutions to increase the space between the skin and muscles. Once the skin is lifted, the flow of blood and lymphatic fluid is promoted. Other advantages are that a patient can take a shower without taking the tape off since it is waterproof. Patients can wear it from 1 to 4 days and even longer if it is applied on the back or buttock area [14, 15].
Many practitioners use it in clinical practice in European countries, and it has a beneficial effect. However, there is insufficient evidence for its clinical effects on lymphedematous limbs. The aim of the study was to assess the efficacy of Kinesiology Taping (KT) for treating breast cancer-related lymphedema. The endpoints were the reduction of limb volume and percentage edema size after a month's therapy.
2. Materials and Methods
The Research Ethics Committee from the Academy of Physical Education in Katowice, Poland, approved this study (national registration number 1605/12/2012). The trial is registered in the Australian New Zealand Clinical Trials Registry with ID number ACTRN12613001173785.
2.1. Settings and Participants
The study was performed at the Provita Clinic in Zory and Limf-Med Hospital in Chorzow, Poland, from December 2012 to August 2013. Participating women met the following inclusion criteria: (1) unilateral breast cancer-related lymphedema for at least one year, (2) moderate-to-severe lymphedema (stages II and III of upper limb edema, the volume difference between affected and healthy extremity with being more than 20%), (3) lack of chemo- or radiation therapy for at least 6 months, and (4) good compliance and willingness to sign the written consent form. Subjects with the following conditions were not allowed to participate or were excluded from the study: (1) active cancer or disease that might lead to swelling and presently taking diuretic therapy or other lymphedema-influencing drugs, (2) skin disease, (3) irremovable bracelet or ring, (4) marked restriction of active range of motion in the affected upper extremity, (5) the presence of a pacemaker, heart disease, pregnancy, metallic devices in the limb to be treated, infectious disease, epilepsy, cartilage growth, thrombophlebitis, arterial hypertension, or metastases, which are the treatment contraindications, and (6) the presence of mental, sensorial, or language problems, which could make cooperation difficult (more details in Figure 1).
Figure 1.
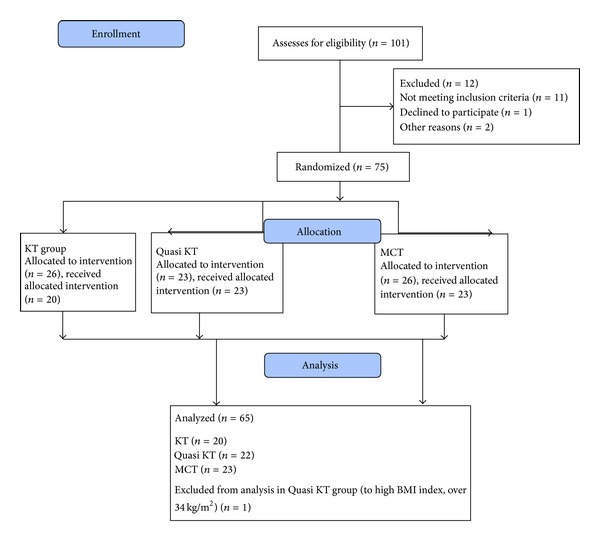
Flow diagram of the study.
2.2. Randomization and Intervention
Participants were randomly allocated to the groups. Computer-generated random numbers were sealed in sequentially numbered envelopes, and the group allocation was independent of the time and person delivering the treatment. The physician (main coordinator) who allocated the patients to groups had 75 envelopes, each containing a piece of paper marked with either group KT, Quasi KT, or MCT. The physician would select and open an envelope in the presence of a physiotherapist to see the symbol and would then direct the patient to the corresponding group. A clinical nurse collected the data and coded them into an Excel database. The “blinded” results were transferred to a STATISTICA version 10.0 (StatSoft Inc., Poland) database by a technician. The research coordinators had no contact with and could not identify the patients.
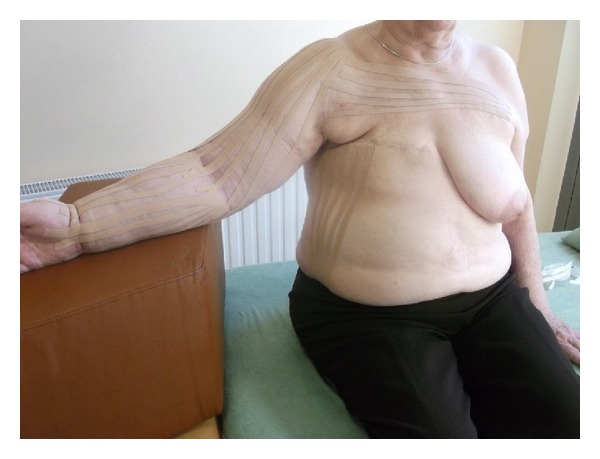
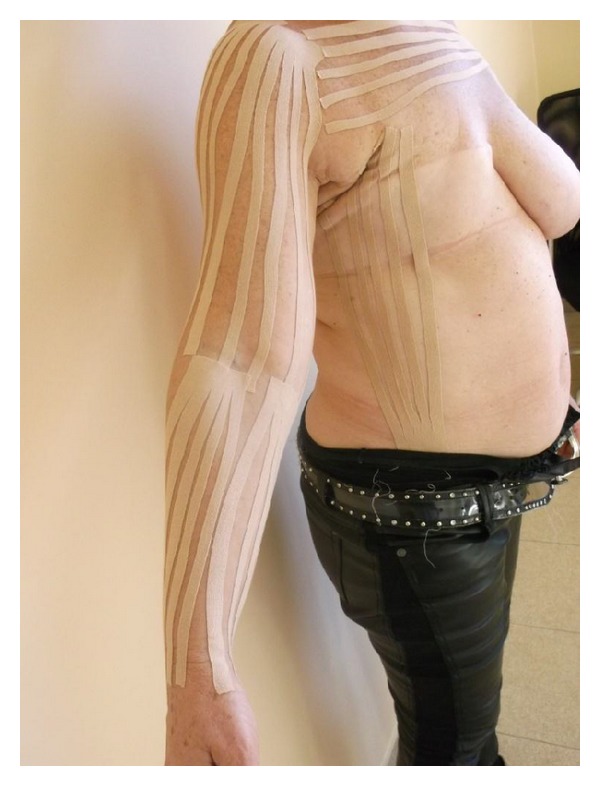
Subjects from all groups received a routine treatment, including skin care, 45 min pneumatic compression therapy in use of the DL1200 device (at pressure 90 mmHg, 12 chambers arm overlapping cuff, hold time 3 seconds with no interval), 1 h manual lymphatic drainage, and application of multilayered short-stretch bandages (50–60 mmHg). The tape groups (KT and Quasi KT groups also received standard therapy, but K-tapes were used instead of bandages). Each of the groups was treated 3 times weekly (bandages or K-tapes were applied and changed on Mondays, Wednesdays, and Fridays) for in the 4-week intervention period. One physical therapist (PT) provided treatment. The program was standardized, following the same protocol for lymphatic drainage to the anterior trunk, posterior trunk, and affected arm, always mowing fluid from the affected side toward the unimpaired side, after lymphatic drainage and before either the short-stretch bandages (Figure 2) or the Kinesiology Taping application (Figure 3). Both bandages and K-tapes (Figure 4) were applied by the by the physical therapist.
Figure 2.

Multilayered compression bandaging.
Figure 3.
Kinesiology Taping application.
Figure 4.
K-tapes technique.
In KT group, the fan tape anchor started at the anterior aspect of the hand with no tension. The tails of the tape were applied to the anterior, medial, and posterior aspects of the forearm and arm with 5–15% tension and then on anterior part of chest. The tapes were left on the patient's skin for the next three days. In Quasi KT group, we used tapes without therapeutic effects-common surgical plasters stuck using the same methodology as in KT group.
In MCT group, we used 4-layered compression bandaging. The first layer was applied to the skin directly with Tubula orthopedic sleeve. Then a supporting bandage Matoplast was applied to the fingers and on hand. Another layer was cotton Rolta-Soft covering the whole limb. The external layer consisted of short-stretch Hartmann bandages.
The following research was a single-blind, controlled, randomized clinical study. The experiment design, methodology, and treatment parameters were programmed by coordinators (physiotherapist, general surgeon, oncologist, and an internist). Standard care, optoelectronic measurements, and data collection were provided by a nurse. The KT/Quasi KT was performed by a physiotherapist. The final statistical analysis was performed by a technician.
2.3. Outcomes Assessment
To assess the volume of limb, we used an optoelectronic Perometer 40 T, cooperating with a personal computer. This method allowed us to estimate the volume of the measuring error for only 0.5%. The assessment technique was based on a special ring, equipped with a system of 378 LED diodes (emitting the infrared radiation). Within the ring were also the optical sensors that receive electromagnetic stimuli. In the course of measuring the limb was located inside the ring on the diode-sensor lines. The registered light pulses on the detectors were turned into electronic signals. The ring was moved during measurement to cover the entire limb (Figure 5). Measurements of the limb volume (both affected and healthy upper limb) were made for all three groups of patients before and after therapy (Figure 6).
Figure 5.

Optoelectronic limb volume measurement.
Figure 6.
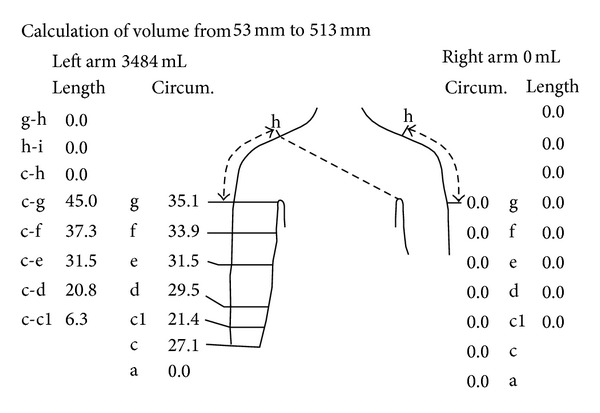
Graphical presentation of optoelectronic measurement.
2.4. Statistical Analysis
To compare the individual parameters that characterized the study groups, the nonparametric Kruskal-Wallis test for countable variables and the chi-squared test (χ 2) for categorical variables were used. The nonparametric matched pair Wilcoxon test was used to compare the within-group results before and after therapy. The Kruskal-Wallis analysis of variance (post hoc Tukey's test) was used to evaluate differences in the changes between the groups in the limb volume and edema values. Two-sided results (P < 0.05) were considered to be statistically significant.
3. Results
In total, 75 individuals were qualified to participate in the treatment. Six patients dropped out from the study during therapy in the KT group (one patient chose to discontinue treatment and withdrew from the study for personal reasons—taking care in the home of her daughter suffering from scarlet fever—four women had skin allergy after K-tapes, and one woman had a heart attack). Three patients from MCT group had complications unrelated to the treatment and were directed to other hospitals (one patient died of brain stroke) before the final observation. One patient in the Quasi KT (placebo group) was excluded from the analysis (BMI over 34 kg/m2, which was too high and significantly increased the SD; this increase could have seriously affected the reliability of both the nonparametric Kruskal-Wallis analysis of variance and the final conclusions).
Of the 65 patients who completed the study protocol (and were analyzed) and had stage II and stage III of secondary lymphedema of upper limb (Table 1), the average volume of the affected extremities in women from group KT was 9414.01 cm3 and decreased after treatment to 8051.15 cm3 (P = 0.002). The average volume of affected limb in women from Quasi KT group was 9621.33 cm3 and decreased after treatment to 8041.02 cm3 (P = 0.002).
Table 1.
Characteristics of patients.
| Group KT | Group Quasi KT | Group MCT | P | |
|---|---|---|---|---|
| Number of women** | 20 | 22 | 23 | 0.784 |
| Age (years)** | ||||
| Range | 44–80 | 39–81 | 42–81 | 0.835 |
| Average | 67.34 | 65.43 | 66.45 | |
| Median | 66.11 | 63.89 | 67.81 | |
| SD | 12.03 | 13.13 | 11.99 | |
| Total mastectomy* | 20 | 22 | 23 | 0.784 |
| Number of patients with adipositas* (BMI > 30 kg/m2) | 7 | 7 | 6 | 0.812 |
| Smokers* | 7 | 8 | 7 | 0.812 |
| Chemotherapy* | 12 | 10 | 11 | 0.812 |
| Radiation therapy* | 15 | 13 | 13 | 0.788 |
| Side of lymphedema* | ||||
| Right | 8 | 10 | 10 | 0.679 |
| Left | 12 | 12 | 13 | |
| Duration of lymphedema (months)** | ||||
| Range | 12.2–63.6 | 12.3–46.6 | 15.3–33.8 | 0.621 |
| Average | 22.12 | 22.78 | 20.03 | |
| Median | 22.02 | 22.52 | 21.67 | |
| SD | 12.56 | 13.01 | 13.02 | |
| Lymphedema severity** (% compared to healthy limb) | ||||
| II stage (20–40%) | 15 | 16 | 16 | 0.788 |
| III stage (40–60%) | 5 | 6 | 7 |
*χ 2 test.
**Kruskal-Wallis test.
In turn, the average volume of the affected limbs in women from MCT group was 10089.41 cm3 and after treatment it was 5021.22 cm3 (P = 0.000001).
In the following study, we observed that the most significant decrease of edema was in patients undergoing multilayered compression bandaging. Results in patients undergoing K-tapes were similar to those obtained in the single-blind placebo (Quasi KT) group (Table 2 and Figure 7).
Table 2.
Results in percentage edema (affected upper limb compared to healthy limb volume and expressed in percent).
| Group | Average ± SD | P | ||
|---|---|---|---|---|
| Before therapy | After therapy | |||
| Decrease of edema (%) | KT | 31.03 ± 28.17 | 25.03 ± 23.08 | 0.005 |
| Quasi KT | 30.28 ± 30.12 | 24.47 ± 23.55 | 0.005 | |
| MCT | 31.07 ± 29.30 | 14.02 ± 10.03 | 0.000003 | |
Wilcoxon test.
Figure 7.
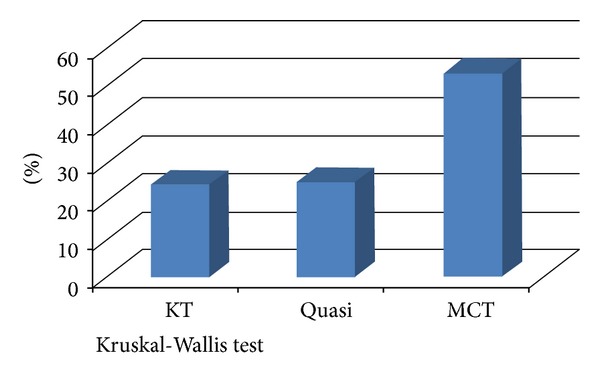
Comparing percentage edema reduction between groups. KT versus MCT group (24.45% versus 53.21%, P = 0.02). Quasi KT versus MCT group (24.78% versus 53.21%, P = 0.02). KT versus Quasi KT group (24.45% versus 24.78%, P = 0.455).
4. Discussion
The KT has been suggested as a promising treatment option for acute sport injuries [16], musculoskeletal disorders [17, 18], and also edema like venous and lymphedema [19–21], but there are still many controversies connected with methodology, application technique, and pressure values.
For example, Olszewski [22] maintains that lymphatics contract rhythmically with a frequency depending on the volume of inflowing tissue fluid. In regions with high capillary filtration rate and tissue fluid formation the frequency is high. The recorded pressures at rest, irrespective of whether in the lying or upright position, with free proximal flow (lateral pressure) range between 7 and 30 mmHg and during finger flexing between 10 and 30 mmHg. The pulse amplitude is from 3 to 20 mmHg and 5–17 mmHg, respectively. The pulse frequency is from 0.6 to 6/min and from 2 to 8/min, respectively. The resting end pressures with obstructed flow (e.g., corresponding to lymphatic obstruction in postsurgical lymphedema) range between 15 and 55 mmHg and during foot flexing from 15 to 50 mmHg. The pulse amplitude is from 3 to 35 mmHg and from 3 to 14 mmHg, respectively. The pulse frequency is from 2.5 to 10/min and from 3 to 12/min, respectively.
It means that external low pressure value during compression procedures (under 50 mmHg) has no effect on lymph pressures. In obstructive lymphedema only few lymphatic collectors remain patent. The recorded pressures during rest range from 5 to 45 mmHg depending on the remaining contractility force of the damaged lymphatic musculature. During calf muscular contractions pressures are generally low ranging from 10 to 25 mmHg, although well-conducted compression may in some cases generate pressures of above 60 mmHg. The author [22] recommends only high pressure range: 50–60 mmHg. In his opinion, lower values are useless, which is similar to our view of the results arising from the study, because K-tapes cannot induce higher external pressure than 15–20 mmHg.
We could find only one reliable meta-analysis presented by researchers from Israel [20], whose systematic review article tried to assessed the effects of therapeutic Kinesiology Taping on pain and disability in participants suffering from musculoskeletal, neurological, and lymphatic pathologies. Four online databases (CINAHL, Cochrane Library, MEDLINE, and PEDro) were comprehensively searched from their inception through March 2012. The initial literature search found 91 controlled trials. Following elimination procedures, 26 studies were fully screened. Subsequently, 12 met our inclusion criteria. The final 12 articles were subdivided according to the basic pathological disorders of the participants' musculoskeletal (n = 9), neurological (n = 1), and lymphatic (n = 2) systems. As to the effect on musculoskeletal disorders, moderate evidence was found supporting an immediate reduction in pain while wearing the KT. In 3 out of 6 studies, reduction of pain was superior to that of the comparison group. However, there is no support indicating any long-term effect. Additionally, no evidence was found connecting the KT application to elevated muscle strength or long-term improved range of movement. No evidence was found to support the effectiveness of KT for neurological conditions. As to lymphatic disorders, inconclusive evidence was reported. Although KT has been shown to be effective in aiding short-term pain, there is no firm evidence-based conclusion of the effectiveness of this application on the majority of movement disorders within a wide range of pathologic disabilities. In the authors' opinion, more research is clearly needed.
However (in only one found clinical trial in Pubmed and MEDLINE), Tsai et al. [21] presented a study about the positive effects of KT. The purpose of this experiment was to compare the treatment and retention effects between standard physical therapy combined with pneumatic compression and modified physical activity, in which the use of a short-stretch bandage was replaced by the use of Kinesiology Taping combined with pneumatic compression. The study results suggest that K-tapes could replace the bandage in therapy and could be a good alternative for patients with poor short-stretch bandage compliance. In our opinion, the mean weakness of this cited study are as follows: the Korean authors applied only single-layered compression therapy (15–20 mmHg, which is not enough to treat any kind of lymphedema) and there was a lack of estimation of the placebo effect in this article.
In the literature, there is a lack of well-conducted, randomized, controlled studies with KT and breast cancer-related lymphedema. It means that we will have to conduct our study. To this moment, we analyzed only a pilot group of women with secondary lymphedema after breast cancer treatment; further studies will be provided.
5. Conclusion
The KT appeared to be ineffective at secondary lymphedema after breast cancer treatment. The single blind, controlled pilot study results suggest that K-tape could not replace the bandage, and at this moment it must not be an alternative choice for the breast cancer-related lymphedema patient.
Ethical Approval
The Research Ethics Committee from the Academy of Physical Education in Katowice, Poland, approved this study (national registration no. 1605/12/2012).
Conflict of Interests
The authors would like to certify that they have no commercial associations with the manufacturers of the equipment described in the paper and other conflict of interests.
References
- 1.Demark-Wahnefried W, Campbell KL, Hayes SC. Weight management and its role in breast cancer rehabilitation. Cancer. 2012;118(8):2277–2287. doi: 10.1002/cncr.27466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shah C, Arthur D, Riutta J, Whitworth P, Vicini FA. Breast-cancer related lymphedema: a review of procedure-specific incidence rates, clinical assessment AIDS, treatment paradigms, and risk reduction. Breast Journal. 2012;18(4):357–361. doi: 10.1111/j.1524-4741.2012.01252.x. [DOI] [PubMed] [Google Scholar]
- 3.Todd M. Chronic oedema: impact and management. British Journal of Nursing. 2013;22(11):623–627. doi: 10.12968/bjon.2013.22.11.623. [DOI] [PubMed] [Google Scholar]
- 4.Moattari M, Jaafari B, Talei A. The effect of combined decongestive therapy and pneumatic compression pump on lymphedema indicators in patients with lymphedema secondary to breast cancer treatment: a randomized clinical control trial. Breast Journal. 2013;19(1):114–115. doi: 10.1111/tbj.12060. [DOI] [PubMed] [Google Scholar]
- 5.Chang CJ, Cormier JN. Lymphedema interventions: exercise, surgery, and compression devices. Seminars in Oncology Nursing. 2013;29(1):28–40. doi: 10.1016/j.soncn.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Lasinski BB, Thrift KM, Squire D, et al. A systematic review of the evidence for complete decongestive therapy in the treatment of lymphedema from 2004 to 2011. PM&R. 2012;4(8):580–601. doi: 10.1016/j.pmrj.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Fife CE, Davey S, Maus EA, Guilliod R, Mayrovitz HN. A randomized controlled trial comparing two types of pneumatic compression for breast cancer-related lymphedema treatment in the home. Supportive Care in Cancer. 2012;20(12):3279–3286. doi: 10.1007/s00520-012-1455-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feldman JL, Stout NL, Wanchai A, Stewart BR, Cormier JN, Armer JM. Intermittent pneumatic compression therapy: a systematic review. Lymphology. 2012;45(1):13–25. [PubMed] [Google Scholar]
- 9.Belmonte R, Tejero M, Ferrer M, et al. Efficacy of low-frequency low-intensity electrotherapy in the treatment of breast cancer-related lymphoedema: a cross-over randomized trial. Clinical Rehabilitation. 2012;26(7):607–618. doi: 10.1177/0269215511427414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cassileth BR, van Zee KJ, Yeung KS, et al. Acupuncture in the treatment of upper-limb lymphedema: results of a pilot study. Cancer. 2013;119(13):2455–2461. doi: 10.1002/cncr.28093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamakawa J, Motoo Y, Moriya Y, et al. Role of Kampo medicine in integrative cancer therapy. Evidence-Based Complementary and Alternative Medicine. 2013;2013:6 pages. doi: 10.1155/2013/570848.570848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Price S, Long AF, Godfrey M. Exploring the needs and concerns of women with early breast cancer during chemotherapy: valued outcomes during a course of traditional acupuncture. Evidence-Based Complementary and Alternative Medicine. 2013;2013:8 pages. doi: 10.1155/2013/165891.165891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nagai A, Shibamoto Y, Ogawa K. Therapeutic effects of saireito (Chai-Ling-Tang), a traditional Japanese herbal medicine, on lymphedema caused by radiotherapy: a case series study. Evidence-Based Complementary and Alternative Medicine. 2013;2013:6 pages. doi: 10.1155/2013/241629.241629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kase K, Hashimoto T, Okane T. Kinesio Taping Perfect Manual. Tokyo, Japan: Kinesio Taping Association; 1998. [Google Scholar]
- 15.Kase K, Wallis J, Kase T. Clinical Therapeutic Applications of the Kinesio Taping Methods. Tokyo, Japan: Kinesio Taping Association; 2003. [Google Scholar]
- 16.Campolo M, Babu J, Dmochowska K, Scariah S, Varughese J. A comparison of two taping techniques (kinesio and mcconnell) and their effect on anterior knee pain during functional activities. International Journal of Sports Physical Therapy. 2013;8(2):105–110. [PMC free article] [PubMed] [Google Scholar]
- 17.Simsek HH, Balki S, Keklik SS, Öztürk H, Elden H. Does Kinesio taping in addition to exercise therapy improve the outcomes in subacromial impingement syndrome? A randomized, double-blind, controlled clinical trial. Acta Orthopaedica et Traumatologica Turcica. 2013;47(2):104–110. doi: 10.3944/aott.2013.2782. [DOI] [PubMed] [Google Scholar]
- 18.Costa CS, Rodrigues FS, Leal FM, Rocha NA. Pilot study: investigating the effects of Kinesio Taping on functional activities in children with cerebral palsy. Developmental Neurorehabilitation. 2013;16(2):121–128. doi: 10.3109/17518423.2012.727106. [DOI] [PubMed] [Google Scholar]
- 19.Aguilar-Ferrándiz ME, Castro-Sánchez AM, Matarán-Peñarrocha GA, Guisado-Barrilao R, García-Ríos MC, Moreno-Lorenzo C. A randomized controlled trial of a mixed Kinesio taping-compression technique on venous symptoms, pain, peripheral venous flow, clinical severity and overall health status in postmenopausal women with chronic venous insufficiency. Clinical Rehabilitation. 2013 doi: 10.1177/0269215512469120. [DOI] [PubMed] [Google Scholar]
- 20.Kalron A, Bar-Sela S. A systematic review of the effectiveness of Kinesio Taping—fact or fashion? European Journal of Physical and Rehabilitation Medicine. 2013;49(5):1–11. [PubMed] [Google Scholar]
- 21.Tsai H-J, Hung H-C, Yang J-L, Huang C-S, Tsauo J-Y. Could Kinesio tape replace the bandage in decongestive lymphatic therapy for breast-cancer-related lymphedema? A pilot study. Supportive Care in Cancer. 2009;17(11):1353–1360. doi: 10.1007/s00520-009-0592-8. [DOI] [PubMed] [Google Scholar]
- 22.Olszewski WL. The third circulation in human limbs-tissue fluid, lymph and lymphatics. Phlebologie. 2012;41(6):297–303. [Google Scholar]


