Abstract
Objective
To describe patient satisfaction after Michigan four-wall sacrospinous ligament suspension for prolapse and identify factors associated with satisfaction.
Methods
Four hundred fifty-three patients were asked to rate their satisfaction with surgery and complete validated quality-of-life instruments. Postoperative support was extracted from the medical record and assessed when possible. Factors independently associated with patients who were “highly satisfied” were identified with multivariable logistic regression.
Results
Sixty-two percent (242/392) reported how satisfied they were 8.0±1.7 years later. Fifty-seven percent had failed prior prolapse surgery, and 56% had a preoperative prolapse ≥4 cm beyond the hymen. Ninety percent were satisfied; 76% were “completely” or “very” satisfied and they were considered “highly satisfied” for analysis. Fourteen percent reporting being “moderately” satisfied and they were considered among those “less satisfied.” Women with lower scores on the postoperative Pelvic Floor Distress Inventory-20 were more likely to be “highly satisfied.” Postoperative anatomic data was available for 67% (162/242) and vaginal support was observed at or above the hymen in 86%. Women with preoperative Baden Walker grade 3 or 4 prolapse were more likely than those with grade 2 prolapse to be “highly satisfied.” Women with advanced postoperative prolapse (Grade 3 or 4) were less likely and those with Grade 2 support were as likely to be “highly satisfied” as those with Grade 0 or 1 support.
Conclusion
The Michigan four-wall sacrospinous ligament suspension is an anatomically effective approach to vault suspension with a high rate of long-term patient satisfaction. Postoperative vaginal support at the hymen does not negatively affect patient’s satisfaction.
Introduction
One in every 10 women will have pelvic floor dysfunction so severe that she will undergo surgery. Native tissue vaginal prolapse repair is a minimally invasive approach free of complications related to abdominal or laparoscopic surgery and mesh placement (1).
There are several different operations that utilize the sacrospinous ligament for vaginal attachment. The Michigan four-wall sacrospinous ligament suspension uses an apical incision and attaches all four walls of the vaginal apex directly to the ligament. The apical incision heals to the ligament so that permanent suture is not needed (2). It differs from traditional sacrospinous suspension, which is approached through a posterior repair incision and attaches only the upper aspect of the right posterior vaginal wall to the ligament (3,4).
In a recent meta-analysis which included both posterior and apical approaches to the sacrospinous ligament, the procedure failed to satisfy 8-20% of patients. Rates of recurrence varied between 4-40% for objective outcomes and 5-25% for subjective outcomes. These data varied most importantly according to definitions of recurrence or failure (5). At present, longer term follow-up and specifically the relationship between patient satisfaction and operative outcome are poorly understood.
At our institution, we have had extensive experience with the Michigan four-wall sacrospinous ligament suspension for managing large and often recurrent prolapses. The primary objective of our study was to describe longer-term patient satisfaction with this procedure for prolapse. Secondary analysis sought to identify factors associated with patient satisfaction, including anatomic outcomes.
Materials and Methods
This IRB approved (IRB# HUM00024673) study involved a retrospective cohort of 453 patients who were identified by searching the electronic billing records for CPT code 57282. The study spanned the years between 1998, when electronic billing information was available, and 2003, the date 5 years prior to study initiation. All procedures were done by urogynecology faculty. Patients were excluded if they were deceased, if a family member advised that they were incapable of participating due to dementia, or if mailings were returned due to an “undeliverable address.”
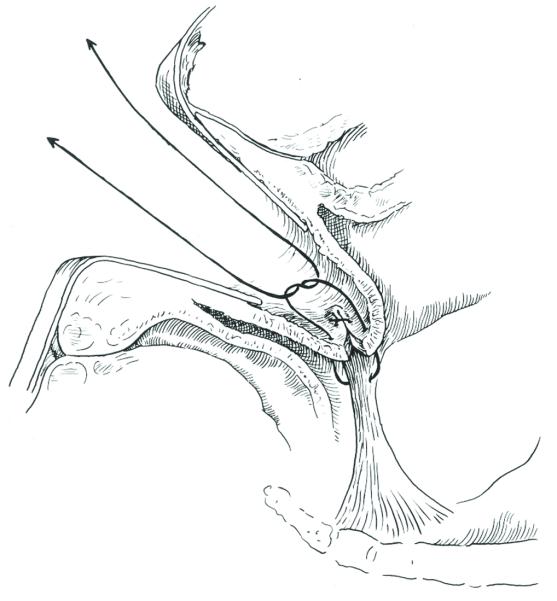
The operative technique of a Michigan four-wall sacrospinous ligament suspension has been described (6) and is available as a video at http://links.lww.com/xxx. In brief, the sacrospinous ligament is approached through an incision at the vaginal apex. In making this incision, excess vaginal length, when present, is excised so that the four walls of the vagina (anterior, posterior, lateral) each reach the ligament without redundancy. After pararectal dissection through the vaginal apex to the sacrospinous ligament, a Deschamps’ ligature carrier is passed through the ligament twice with a loop of 0 PDS suture to establish 4 strands in the ligament. After anterior colporrhaphy is performed (if indicated), the PDS sutures in the ligament are brought through the apical incision and tied to elevate the vagina (Figure 1).
Figure 1.
Sagittal image showing step in procedure where the new vaginal apex is both closed and tied down to the sacrospinous ligament with the second of 4 suspension sutures.(© DeLancey 2013)
Chart review of the electronic medical record was undertaken for all patients. The performance of a Michigan four-wall sacrospinous ligament suspension was confirmed by operative note review. Demographics, medical and surgical history, and the severity of patients’ prolapse were abstracted by study team members. Data regarding vaginal support was abstracted from the latest “clinic” visit, which was at least 15 weeks since the surgery and had either Baden Walker or pelvic organ prolapse quantification (POP-Q) data. After all data abstraction was complete, every fifth chart was reviewed to provide assurance regarding data accuracy.
Patient reported outcomes were assessed with a mailed questionnaire accompanied by a $2 incentive payment. Patients were also invited to return to clinic for an examination. Patients not willing to complete the questionnaire or return for an examination were encouraged to participate by answering a few items regarding their satisfaction with surgery, the primary outcome to be analyzed. Satisfaction was assessed by asking patients to place a mark along a horizontal line. The scale of the line was continuous, had limits of 0 and 100%, and had anchors at 0, 25, 50, 75, and 100 corresponding with “not at all,” “minimally,” “moderately,” “very,” and “completely” satisfied, respectively. If a response fell between anchors, a conservative value to the nearest increment below their rating was assigned. For the analysis, women were dichotomized into a “highly satisfied” group which included women who were “very” and “completely” satisfied (≥75%) and a “less satisfied” group who were “moderately,” “minimally,” or “not at all” satisfied (<75%). All patients were also asked to answer yes or no to the following question, “Would you make the decision to have surgery again?” The status of “responder” and “non-responder” was determined by whether or not patients answered these two questions. Those patients willing to complete the questionnaire went on to answer the Pelvic Floor Distress Inventory-20 (PFDI-20) and the Pelvic Floor Impact Questionnaire-7 (PFIQ-7) which provides subscales for pelvic organ prolapse (POPDI-6 and POPIQ), urogenital (UDI-6 and UIQ) and colorectal-anal symptoms (CRADI-8 and CRAIQ).
Patients returning a questionnaire and indicating a willingness to participate were contacted to have a “study” examination. A $25 participation incentive and parking reimbursement were given to defray travel expenses. Patients were examined by KL or DMM. POP-Q data were collected from each patient who returned to clinic for a “study examination.”
Analysis of anatomic support was done with the “most recent” data available. The most recent data regarding vaginal support was taken from either the “clinic” or the “study” examinations. POP-Q data, which became available during the course of the study, were converted to Baden Walker measurements to allow comparison of anatomical outcomes across all patients in each compartment of vaginal support (anterior, posterior, and apical). “Maximal” Baden Walker grade was determined by taking the highest grade of prolapse observed in any of the three compartments of support. Grades of vaginal support were categorized as follows: Baden Walker Grade 0, descent less than half way to the hymen; Baden Walker Grade 1, half way or more to the hymen; Baden Walker Grade 2, at the hymen; Baden Walker Grade 3 halfway past the hymen (<4 cm below the hymen); and Baden Walker Grade 4, (≥4 cm below the hymen). Data from the chart review, questionnaires, and examinations were double entered by a professional data service. STATA (College Station, Texas, v 9.2) was used for analyses. Outlier analysis was used to identify potential data errors. The responses to satisfaction were dichotomized. When only a verbal description of anatomy was provided, data were considered missing. Data management responsibilities were as follows: data extraction (KAL, MBB, MAS, SM, and DMM), cleaning (KAL, TS, DMM) and transformation and analysis (TS, DMM). T-tests were used for continuous measures and chi-squared analysis was performed for categorical variables. Parity which was not normally distributed was compared with the Wilcoxon Mann Whitney test. Comparisons with a p-value <0.05 were considered significant. Those factors which had a statistically significant relationship with the outcome of “highly satisfied” in bivariate analysis and/or had a clinically plausible relationship with patient satisfaction were included in a backward stepwise logistic regression to determine independent factors associated with satisfaction. Although concomitant hysterectomy was significant in the bivariate analysis, the number of women who underwent it was small and all were in the “highly satisfied” group. It therefore predicted satisfaction perfectly in this small group of women and could not be included in the multivariate analysis.
Results
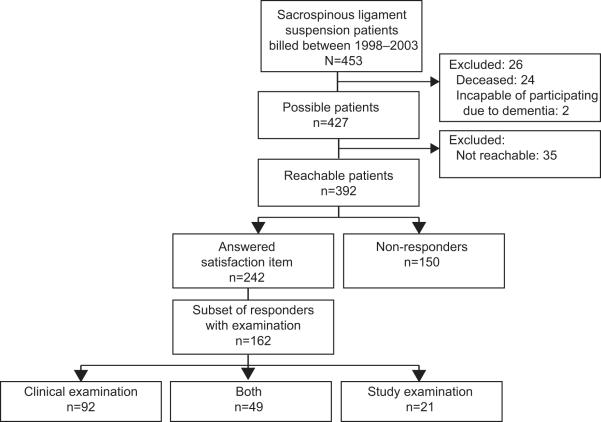
Of the original 453 patients operated on more than 5 years ago, 392 were identified for potential inclusion. 62% of patients who met inclusion criteria responded (242/392): 242 women completed the satisfaction questions, 187 women completed the entire validated questionnaires, and 70 were willing to return for the “study” examination (Figure 2). For all patients, mean age and weight were 64 ± 10 years and 162 ± 30 pounds, respectively. Median parity was three. A history of failed prolapse surgery was documented for 57%, and a prolapse ≥4 cm below the hymen was observed preoperatively for 56%. The average time since surgery was 8.0 ± 1.7 years.
Figure 2.
Patient flowchart.
The demographics and surgical histories of the responders and non-responders are compared in Table 1. The responders and non-responders differed in the percentage that had a hysterectomy before the Michigan four-wall sacrospinous ligament suspension and in the length of follow up. Age, parity, weight, a history of prior prolapse surgery, and preoperative severity of prolapse by Baden Walker grade, and postoperative vaginal support by Baden Walker at the “most recent” follow up did not differ between the groups.
Table 1.
Patient Demographics With Responder Compared With Nonresponder Comparison
| Responder (n=242) |
Nonresponder (n=150) |
P | |
|---|---|---|---|
| Age (years, mean ± sd) | 64.3 ± 9.9 | 65.1 ± 12.1 | 0.519 |
| Weight (lbs, mean ± sd) | 161.8 ± 29.5 | 161.5 ± 32.7 | 0.941 |
| Parity (median, range) | 3 (0-10) | 3 (0-9) | 0.082 |
| Caucasian (%) | 83 | 83.9 | 0.965 |
| Follow-up (years, mean ± sd) | 8.0 ± 1.7 | 8.4 ± 1.8 | 0.026 |
| History of prolapse surgery | 58.9% | 53.0% | 0.258 |
| History of hysterectomy | 92.2% | 84.6% | 0.018 |
| Preoperative maximum Baden Walker grade of prolapse Grade 2 Grade 3 Grade 4 |
4.9% 39.1% 56.0% |
4.1% 39.9% 56.1% |
0.918 |
| Maximum Baden Walker grade of prolapse At most recent follow-up |
0.119 | ||
| Grade 0/1 Grade 2 Grade 3 Grade 4 |
61.7% 24.1% 13.6% 0.6% |
50.0% 36.3% 11.3% 2.5% |
Among women who completed the satisfaction questionnaire (n=242), 89.7% were satisfied with the surgery. 75.6% indicated that they were “completely” or “very satisfied” with their surgical outcome and were classified as “highly satisfied.” There were 14.1% who reported being “moderately” satisfied, and this group was classified as “less satisfied” along with the 10.4% who reported being “somewhat” or “not at all” satisfied (Figure 3). 89% (202/227) reported they would make the decision to have surgery again.
Figure 3.
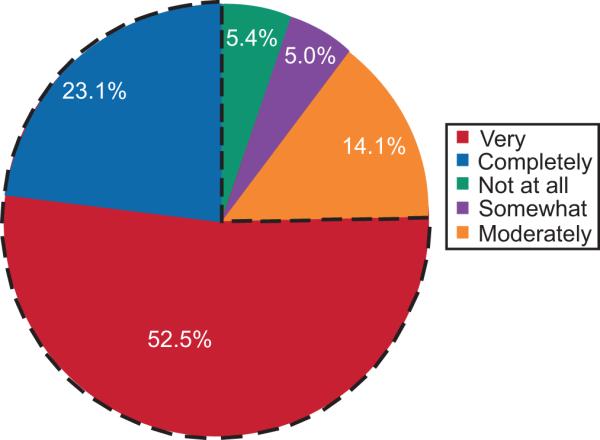
Patient reported satisfaction with “results of surgery.” The proportion of patients who were “very” or “completely” satisfied was 75.3% (n=183) compared to 24.5% (n=59) who were “moderately”, “somewhat” or “not at all” satisfied. Dashed line indicates the dichotomization of the satisfaction data for analysis into “highly satisfied” and “less satisfied.”
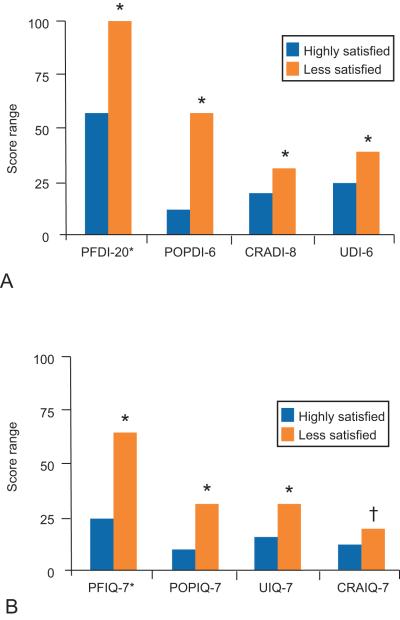
Mean responses of the 187 women who answered both the satisfaction items and the validated questionnaires were the following: PFDI-20 66.6 ± 54.9 (with prolapse, colorectal and urinary subscale means of 17.0 ± 19.6, 22.5 ± 21.8, and 27.4 ± 24.4 respectively) and PFIQ 32.8 ± 56.6 (with prolapse, colorectal and urinary subscale means of 8.4 ± 19.8, 10.7 ± 20.8, and 14.8 ± 23.0 respectively). The relationship between these findings and levels of satisfaction are shown in Figure 4.
Figure 4.
Histogram of postoperative distress inventories (A) and (B) questionnaires: By satisfaction status (“highly” and “less” satisfied). Scale range 0-300, means and standard deviations are presented. *P≤.001. †P=.01. †PFDI-20, pelvic floor distress inventory-20; POPDI-6, pelvic organ prolapse distress inventory-6; CRADI-8, colorectal-anal symptoms distress inventory-8; UDI-6, urogenital distress inventory-6; †PFIQ-7, pelvic floor impact questionnaire-7; POPIQ-7, pelvic organ prolapse impact questionnaire; UIQ-7, urogenital impact questionnaire-7; CRAIQ-7, colorectal-anal symptoms impact questionnaire-7.
The 242 patients included in the analysis of satisfaction are characterized as follows. Prior to their Michigan four-wall sacrospinous ligament suspension, the majority of patients had advanced pelvic organ prolapse with Baden Walker Grade 3 and Grade 4 prolapse being found in 39% and 56%, respectively. In Table 2, site-specific and maximal Baden Walker Grades of vaginal support preoperatively and postoperatively are provided. Postoperative support is categorized by the “clinic” examination extracted from the electronic medical record with mean follow-up of 1.8 years and by the “study” examination for 70 individuals who returned for an examination with a mean follow-up of 8 years. The combined “most recent” examination extracts data from either the “clinic” or the “study” visit for the 242 individuals providing satisfaction data, with mean follow-up of 4.3 years. Anatomic data was available for 67% (162/242). The “study” examination provided more up-to-date data for 49 individuals who had a “clinic” examination and was the only data for 21 individuals who had not had a “clinic” examination (Figure 2).
Table 2.
Site-Specific and Maximal Vaginal Support Preoperatively and Postoperatively Classified by Baden Walker Grade of Prolapse
| Site | Baden Walker Grade |
Preoperative (n=242) |
Clinic Examination* (n=141) |
Study Examination† (n=70) |
Most Recent Examination (n=162) |
|---|---|---|---|---|---|
| Maximal prolapse |
0/1 | 0 (0%) | 77 (54.6%) | 47 (67.1%) | 100 (61.7%) |
| 2 | 12 (5.0%) | 50 (35.5%) | 10 (14.3%) | 39 (24.1%) | |
| 3 | 95 (39.3%) | 14 (9.9%) | 12 (17.1%) | 22 (13.6%) | |
| 4 | 135 (55.8%) | 0 (0%) | 1 (1.4%) | 1 (0.6%) | |
| Anterior | 0/1 | 69 (28.8%) | 82 (59.0%) | 49 (70.0%) | 107 (66.5%) |
| 2 | 27 (11.3%) | 43 (31.0%) | 9 (12.9%) | 32 (19.9%) | |
| 3 | 70 (29.1%) | 14 (10.1%) | 11 (15.7%) | 21 (13.0%) | |
| 4 | 74 (30.8%) | 0 (0%) | 1 (1.4%) | 1 (0.6%) | |
| Posterior | 0/1 | 48 (20.3%) | 128 (92.8%) | 67 (95.7%) | 151 (93.8%) |
| 2 | 26 (11.0%) | 9 (6.5%) | 1 (1.4%) | 8 (5.0%) | |
| 3 | 83 (35.0%) | 1 (0.7%) | 1 (1.4%) | 1 (0.6%) | |
| 4 | 80 (33.8%) | 0 (0%) | 1 (1.4%) | 1 (0.6%) | |
| Apex | 0/1 | 54 (22.8%) | 132 (98.5%) | 69 (98.6%) | 156 (98.7%) |
| 2 | 42 (17.7%) | 1 (0.8%) | 0 (0%) | 1 (0.6%) | |
| 3 | 72 (30.4%) | 1 (0.8%) | 0 (0%) | 0 (0%) | |
| 4 | 69 (29.1%) | 0 (0%) | 1 (1.4%) | 1 (0.6%) |
Data are n(%) unless otherwise specified.
Clinic examination, mean follow-up (± standard deviation): 1.8 ± 1.8 years.
Study examination, mean follow-up (± standard deviation): 8.0 ± 1.7 years.
The percentages of women who developed support beyond the hymen over the period of follow up were modest (Table 2). By the “clinic” examination at a mean of 1.8 years, Baden Walker Grade 0, 1 or 2 support was observed in 90.1% (127/141). With a mean follow up of 8.0 years at the “study” examination, Baden Walker Grade 0, 1, or 2 support was observed in 81.4% (57/70). Anatomic failures were found predominantly in the anterior compartment at both points in follow up. The anterior vaginal wall was below the hymen in 10.1% at the “clinic” examination and in 17.1% in the group presenting for the “study” examination. Apical and posterior vaginal wall support was more stable. Loss of support below the hymen in these compartments was observed in less than 1% at the “clinic” examination and this increased to 2.8% at the “study” examination. We considered but decided against performing a survival analysis because we do not have data regarding anatomical support at multiple time points over an extended follow up period.
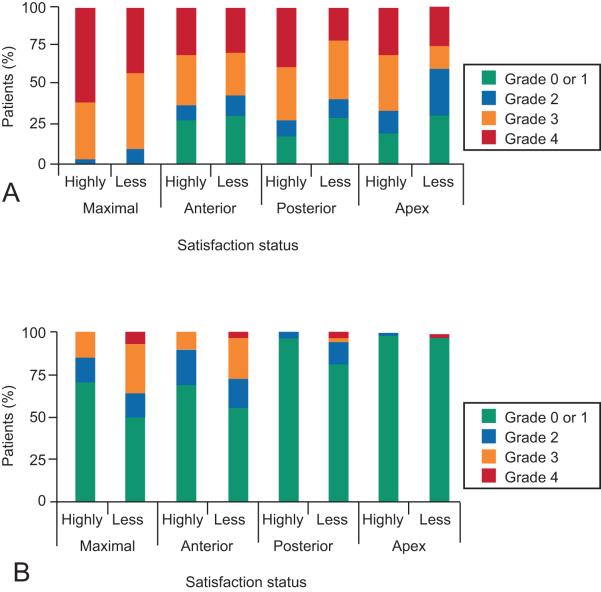
Factors associated with being “highly satisfied” were analyzed. Age, parity, weight, length of follow up, and failed prior prolapse surgery did not differ between the two groups. The scores for the PFDI-20 and PFIQ-7 (Figure 4) of the “highly satisfied” were lower, suggesting less symptom distress and less impact on quality of life. In addition, the subscales for prolapse, urinary incontinence and bowel dysfunction of the PFDI-20 and PFIQ-7 were each significantly lower among women who were “highly satisfied,” suggesting that each type of pelvic floor dysfunction contributes to satisfaction. Those women who had larger preoperative prolapses, predominantly in the apical compartment (data illustrated in Figure 5, provided in the Appendix), who had a concomitant vaginal hysterectomy (9% vs 0%, p=0.015), and who did not have a pubovaginal sling (4% vs 19%, p=0.001) were also more likely to be “highly satisfied.” Postoperatively, “highly satisfied” women had better pelvic organ support in the anterior and posterior compartments (data illustrated in Figure 5, provided in the Appendix). Although the one woman with postoperative apical failure was in the less satisfied group, the rarity of this outcome did not allow meaningful comparison.
Figure 5.
Stacked histogram of preoperative and postoperative Baden Walker Grade by compartment: By satisfaction status (“highly” and “less” satisfied). “Maximal” refers to the highest Baden Walker Grade that occurred in any compartment.
Multivariable logistic regression was used to identify factors independently associated with patients who were “highly satisfied” (Table 3). Women with a maximal preoperative Baden Walker Grade 3 or 4 prolapse were more likely to be “highly satisfied” than those with Baden Walker Grade 2 prolapse. Women with lower scores on the PFDI-20 and with Baden Walker Grade 0, 1, or support (compared with those having Grade 3 or 4 support) were also significantly more likely to be “highly satisfied.” It is noteworthy that women with postoperative maximal compartment at the hymen (Baden Walker Grade 2) were as likely to be “highly satisfied” as those with support above the hymen. Pubovaginal sling and PFIQ-7 scores were included but they were neither significant nor did their inclusion change the direction of the associations.
Table 3.
Logistic Regression Model Identifying Factors Independently Associated With the Outcome of Highly (“Completely” and “Very”) Satisfied
| Odds Ratio |
P | 95% Confidence Interval |
|
|---|---|---|---|
| Preoperative Baden Walker grade 3 prolapse* | 13.0 | 0.006 | 2.1 - 79.8 |
| Preoperative Baden Walker grade 4 prolapse* | 7.9 | 0.017 | 1.5 - 42.4 |
| Pelvic floor distress inventory – 20 | 0.99 | 0.001 | 0.98 - 0.99 |
| Postoperative Baden Walker grade 2 prolapse at “most recent” examination† |
0.50 | 0.266 | 0.15 - 1.7 |
| Postoperative Baden Walker grade 3/4 prolapse at “most recent” examination† |
0.12 | 0.001 | 0.04 - 0.42 |
Referent group is Preoperative Baden Walker Grade 2.
Referent group is Baden Walker Grade 0/1.
Discussion
With 8 years of follow-up, 90% of women indicated satisfaction with results of the Michigan four-wall sacrospinous ligament suspension and would decide to have the surgery again. These results were obtained with native tissue in patients where more than half had failed prior surgery and had a prolapse 4 cm or more below the hymen. Women who had prior operations for prolapse were as likely to be satisfied as those having primary repairs. Patients with the largest prolapses were more likely to be highly satisfied. Several authors report short-term satisfaction with sacrospinous suspension in of 80-93% of patients (7-10). Our similar long-term results are evidence of continued success over time.
We identified several factors that independently predict being “highly satisfied.” Since women with preoperative Baden Walker Grade 3 and 4 prolapses were more likely than those with Grade 2 prolapse to be “highly satisfied,” we hypothesize they had more to gain and were happier with the results. The postoperative occurrence of bladder, bowel and prolapse symptoms, reflected by the PFDI, negatively affected patient satisfaction. This is logical, since all are known to cause distress and impact quality of life.
Our data confirm that symptom severity affects patient satisfaction. This study extends the literature by quantifying the contribution of postoperative symptoms (as reflected by validated questionnaires) to overall satisfaction. We found significant differences in overall postoperative PFDI-20 and PFIQ-7 scores, in each of their subscales when comparing the “highly satisfied” and “less satisfied” groups. These differences all approach or exceed 0.5 SD, reported as estimates for clinically important differences (11). Multivariate logistic regression confirms that these findings are independent of postoperative anatomy and preoperative prolapse severity. Compared with data from Maher, et al. (8) our patients report similar postoperative IIQ-7 scores, but significantly higher scores on the UDI-6. A higher proportion of our patients underwent concomitant incontinence procedures, known to be associated with de novo urinary symptoms. We hypothesize that distress from these symptoms affected our patients’ satisfaction.
In assessing anatomical outcomes, prolapse was noted in between 14 and 17% of patients, depending on the subset available for analysis. This is similar to anatomic findings in abdominal sacral colpopexy (12). The level of postoperative vaginal support chosen as a criterion for operative failure has been discussed in the urogynecologic literature (13). Several studies have demonstrated that strict anatomic definitions result in lower reported success rates than the use of subjective satisfaction (5, 8, 14-15). Our findings demonstrate that prolapse below the hymen indeed affects patient satisfaction, whereas women with vaginal walls at the hymen are equally satisfied as those with higher vaginal walls. This supports the growing consensus for setting the anatomic threshold for failure below the hymen (13). Although surgeons would prefer to have the vaginal walls higher than this, the possibility of increased complications may not be warranted.
Several factors must be considered in interpreting the results of this study. Assessing the outcome of this cohort is limited by a response rate of 62% (242/390) and by a subgroup analysis of the 67% of responders who had anatomic data. The percentage of individuals who have responded and provided data is respectable (>60%) and similar to that reported in other surgical outcome studies (16). Nonetheless, a higher response rate might provide a more accurate assessment. There is the potential for responder bias in a retrospective cohort study. Comparison of the responders and non-responders suggests they have similar follow-up periods and are reasonably similar (with the exception of previous hysterectomy). With an absence of other long term data regarding these operations, we believe there is a role for such studies, keeping in mind the limitations of this type of research. The VAS is a conventional means of analyzing satisfaction, albeit not validated specifically for this use with prolapse. The Patient Global Impression of Improvement would be preferable, but it was not validated for prolapse surgery when the study was developed. Ultimately, satisfaction ratings were consistent with validated questionnaire scores. Strengths of the study include the large percentage of women with Stage III and IV prolapse and/or recurrent prolapse, the focus on outcomes from one surgical technique, and a follow up period of eight years.
The study provides information helpful for counseling patients regarding prolapse repair with a native-tissue Michigan four-wall sacrospinous ligament suspension. It reveals high long-term satisfaction for advanced apical prolapse without the use of graft material. Postoperative vaginal wall laxity at the hymen, historically described as a shortcoming of the procedure, did not affect patients’ satisfaction.
Supplementary Material
Acknowledgments
Support for investigator effort received from ORWH SCOR for Sex Differences Research P50 HD 44406 and R01 HD 38665.
The University of Michigan has received research funds in partial support of Dr. John O.L. DeLancey’s salary from the following companies: American Medical Systems, Johnson and Johnson Personal Products, Proctor and Gamble, and Kimberly Clark. Dr. Dee Fenner has received research support from American Medical Systems.
Appendix.
Appendix.
Preoperative and Postoperative Anatomic Outcomes at “Most Recent” Follow-up Analyzed by Satisfaction Status (Data for Figure 5)
| Preoperative | Postoperative | ||||||
|---|---|---|---|---|---|---|---|
| Site | Baden Walker Grade |
Highly | Less | P | Highly | Less | P |
| Maximum prolapse |
0/1 | 0% | 0% | 0.02 | 71.4% | 50% | 0.01 |
| 2 | 3.3% | 10.2% | 14.3% | 14.3% | |||
| 3 | 36.6% | 47.5% | 14.3% | 28.6% | |||
| 4 | 60.1% | 42.4% | 0% | 7.1% | |||
| Anterior | 0/1 | 28% | 31% | 0.82 | 69.5% | 54.6% | 0.03 |
| 2 | 10.4% | 13.8% | 20.3% | 18.2% | |||
| 3 | 30.2% | 25.9% | 10.2% | 24.2% | |||
| 4 | 31.3% | 29.3% | 0% | 3% | |||
| Posterior | 0/1 | 17.3% | 29.3% | 0.06 | 96.9% | 82.4% | 0.01 |
| 2 | 10.6% | 12.1% | 3.2% | 11.8% | |||
| 3 | 34.1% | 37.9% | 0% | 2.9% | |||
| 4 | 38% | 20.7% | 0% | 2.9% | |||
| Apex | 0/1 | 20% | 31.6% | 0.01 | 99.2% | 96.8% | 0.13 |
| 2 | 14.4% | 28.1% | 0.8% | 0% | |||
| 3 | 35% | 15.8% | 0% | 0% | |||
| 4 | 30.6% | 24.6% | 0% | 3% | |||
Data are percentages unless otherwise specified.
Footnotes
Financial Disclsoure: The other authors did not report any potential conflicts of interest.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Boyles SH, Weber A, Meyn L. Procedures for pelvic organ prolapse in the United States, 1979-1997. AJOG. 2003;188:108–115. doi: 10.1067/mob.2003.101. [DOI] [PubMed] [Google Scholar]
- 2.Kearney R, DeLancey JO. Selecting suspension points and excising the vagina during Michigan four-wall sacrospinous suspension. Obstet Gynecol. 2003 Feb;101(2):325–30. doi: 10.1016/s0029-7844(02)02464-x. [DOI] [PubMed] [Google Scholar]
- 3.Richter K, Albrich W. Long-term results following fixation of the vagina on the sacrospinal ligament by the vaginal route (vaginaefixatio sacrospinalis vaginalis) AJOG. 1981;141(7):811–816. doi: 10.1016/0002-9378(81)90709-2. [DOI] [PubMed] [Google Scholar]
- 4.Nichols DH. Sacrospinous fixation for massive eversion of the vagina. AJOG. 1982;142(7):901–4. doi: 10.1016/s0002-9378(16)32539-x. [DOI] [PubMed] [Google Scholar]
- 5.Morgan DM, Rogers MA, Huebner M, Wei JT, DeLancey JO. Heterogeneity in anatomic outcome of sacrospinous ligament fixation for prolapsed; a systematic review. J Obstet Gynecol. 2007;109(6):1424–33. doi: 10.1097/01.AOG.0000264066.89094.21. [DOI] [PubMed] [Google Scholar]
- 6.Morgan DM, Larson K. Uterosacral and sacrospinous ligament suspension for restoration of apical vaginal support. Clin Obstet Gynecol. 2010;53(1):72–85. doi: 10.1097/GRF.0b013e3181cf2d51. [DOI] [PubMed] [Google Scholar]
- 7.Marcickiewicz J, Kjöllesdal M, Brännström M. Perioperative course and long term outcome after vaginal sacrospinous colpopexy for vaginal vault prolapsed post hysterectomy: comparison of three different suture methods. J Obstet Gynaecol Res. 2008;34(6):1026–1031. doi: 10.1111/j.1447-0756.2008.00809.x. [DOI] [PubMed] [Google Scholar]
- 8.Maher C, et al. Abdominal sacral colpopexy or vaginal sacrospinous colpopexy for vagina vault prolapse: a prospective, randomized study. AJOG. 2004;190:20–6. doi: 10.1016/j.ajog.2003.08.031. [DOI] [PubMed] [Google Scholar]
- 9.David-Montefiore E, Barranger E, Dubernard G, Nizard V, Antoine JM, Darai E. Functional results and quality-of-life after bilateral sacrospinous ligament fixation for genital prolapse. Eur J Obstet Gynecol Reprod Biol. 2007;132:209–13. doi: 10.1016/j.ejogrb.2006.04.031. [DOI] [PubMed] [Google Scholar]
- 10.Feiner B, Gietelink L, Maher C. Anterior vaginal mesh sacrospinous hysteropexy and posterior fasical placation for anterior compartment dominated uterovaginal prolapsed. IUJ. 2010;21:203–208. doi: 10.1007/s00192-009-1012-9. [DOI] [PubMed] [Google Scholar]
- 11.Barber M, Spino C, Janz N, et al. The minimum important differences for the urinary scales of the pelvic floor distress inventory and the pelvic floor impact questionnaire. AJOG. 2009;200:580e1–580. e7. doi: 10.1016/j.ajog.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nygaard I, Brubaker L, Zyczynski HM, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–24. doi: 10.1001/jama.2013.4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barber M, Brubaker L, Nygaard I, et al. Defining Success After surgery for Pelvic Organ Prolapse. Obstet Gynecol. 2009;114(3) doi: 10.1097/AOG.0b013e3181b2b1ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paraiso MF, Ballard L, Walters M, et al. Pelvic support defects and visceral and sexual function in women treated with sacrospinous ligament suspension and pelvic reconstruction. AJOG. 1996;175(6) doi: 10.1016/s0002-9378(96)70085-6. [DOI] [PubMed] [Google Scholar]
- 15.Aigmueller T, Riss P, Dungl A, Bauer H. Long-term follow-up after vaginal sacrospinous fixation: patient satisfaction, anatomical results and quality of life. Int Urogynecol J Pelvic Floor Dysfunct. 2008 Jul;19(7):965–9. doi: 10.1007/s00192-008-0563-5. [DOI] [PubMed] [Google Scholar]
- 16.Parden AM, Gleason JL, Jauk V, Garner R, Ballard A, Richter HE. Incontinence outcomes in women undergoing primary and repeat midurethral sling procedures. Obstet Gynecol. 2013 Feb;121(2 Pt 1):273–8. doi: 10.1097/aog.0b013e31827c5de7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.