Abstract
Poly(amido amine) (PAMAM) dendrimers have been evaluated for the influence of surface functionality and size on the epithelial barrier of the gut with the goal of identifying safe carriers that can be used for oral drug delivery. Limited studies are conducted to date however to assess the toxicity of PAMAM dendrimers in vivo when administered by the oral route. The goal of this research was to conduct an oral acute toxicity study of PAMAM dendrimers as a function of size and charge in immune competent CD-1 mice. Maximum tolerated doses (MTD) of PAMAM dendrimers as a function of size and surface functionality were established and clinical signs of toxicity monitored. Results demonstrate that positively charged dendrimers caused more toxicity whereas their anionic counterparts were tolerated at ten times higher doses. Severe signs of toxicity observed for large (G7) cationic amine- or hydroxyl-terminated dendrimers include hemobilia and spleenomegaly. The MTD for these dendrimers ranged from 30mg/kg to 200mg/kg. Anionic G6.5 or smaller molecular weight carboxyl-, amine- or hydroxyl-terminated dendrimers (G3.5-COOH, G4-NH2, G4-OH) on the other hand were tolerated at doses of upto 500mg/kg (300mg/kg in some cases) with minimal or no signs of toxicity. Establishing the MTD of orally delivered PAMAM dendrimers and the influence of surface functionality and size on toxicity, aids in the rational design of PAMAM-drug conjugates for oral drug delivery applications.
Keywords: Oral drug carriers, Acute toxicity, In vivo, Surface charge, PAMAM dendrimers, Drug delivery
INTRODUCTION
Dendrimers are branched polymeric architectures that have been used extensively for drug delivery applications [1-3]. One such branched polymer, i.e., poly(amido amine) dendrimers have been extensively investigated for oral drug delivery[4-9]. These studies, largely conducted in in vitro models of intestinal epithelial barrier, such as the everted sac and Caco-2 cell monolayers, have clearly shown the influence of size, surface functionality and charge on toxicity and transepithelial transport. A general trend has been observed that cationic PAMAM dendrimers are more toxic than their anionic counterparts, larger dendrimers are more toxic compared to smaller dendrimers of similar surface functionality, and that masking cationic residues with non charged groups improves tolerability of PAMAM dendrimers and their uptake by the epithelial cells[10, 11]. While the in vitro studies of PAMAM toxicity and transepithelial transport provide guidelines for the design of these carriers for oral drug delivery applications, much needs to be done to establish a size and charge window where oral administration of these constructs in an in vivo setting is safe. The present study is an initial attempt in this direction, and aims to understand the influence of size and surface charge on maximum tolerated dose and toxicity of PAMAM dendrimers in mice.
MATERIALS AND METHODS
Preparation and characterization of PAMAM dendrimers
PAMAM dendrimers (Table 1) were fractionated and characterized as previously described[12]. Briefly, PAMAM dendrimers (G3.5-COOH, G4-NH2, G4-OH, G6.5-COOH, G7-NH2 and G7-OH) with ethylene diamine core were purchased from Sigma (St. Louis, MO). Dendrimer samples were further fractionated by a preparative Sephadex Hiload 75 size exclusion column (GE Healthcare Biosciences, Piscataway, NJ) as necessary to remove small molecular weight impurities. All dendrimers were characterized at physiologically relevant pH by dynamic light scattering (DLS) on a DAWN HELEOS II (Wyatt Technologies, Santa Barbara, CA) at a concentration of 5 mg/ml and their zeta potential recorded on a Malvern Zetasizer (Malvern Instruments Inc., Westborough, MA) at a concentration of 10 mg/ml in triplicate. Zeta potential was measured in double distilled water (DDW) with pH adjusted to 7.4 using HCl and NaOH (not buffered). In addition, PAMAM dendrimers were characterized for absence of small molecular weight impurities by high performance liquid chromatography (HPLC) (Agilent Technologies, Santa Clara, CA) on a C18 (4.6 × 250 mm, 5 μm) column (Waters, Milford, MA) in an acetonitrile: water mixture (27:73) with 0.14% trifluoro acetic acid and size exclusion chromatography (SEC) on an analytical Superose 6 10/300 GL column (GE Healthcare Biosciences, Piscataway, NJ). Elution buffer was PBS: acetonitrile (80:20) with 0.1% sodium azide.
Table 1.
Physicochemical characterization of PAMAM dendrimers
| Dendrimer | # Of surface groups§ | Size (diameter) in nm | Zeta potential in mV (Conductivity in mS/cm)@ |
|---|---|---|---|
| G3.5-COOH | 64 | 3.2 ± 0 | * |
| G4-NH2 | 64 | 3.4 ± 0.22 | * |
| G4-OH | 64 | 2.6 ± 0 | * |
| G6.5-COOH | 512 | 8.5 ± 0.61 | −42.0 ± 1.2 (1.794)⌘ |
| G7-NH2 | 512 | 8.1 ± 0.42 | 64.8 ± 3.2 (0.264)⌘ |
| G7-OH | 512 | 6.4 ± 0 | 27.7 ± 1.1 (0.269)⌘ |
Provided by manufacturer
Dendrimers were below detection limit
Zeta potential was measured in double distilled water at pH 7.4 (not buffered)
Mean conductivity values
Oral acute toxicity studies
All oral acute toxicity studies were carried out in 4-6 weeks old female CD-1 mice weighing about 25 g purchased from Charles River Laboratories (Boston, MA) and used strictly according to the rules and guidelines of the University of Utah Institutional Animal Care and Use Committee. Animals were fed normal diet during the course of all studies. The dose escalation study started at 100mg/kg (except for cationic dendrimers which started at 50mg/kg). Detailed list of dose administered under each treatment group is provided in Table 2. Each dose of PAMAM dendrimer or saline control was prepared in a total volume of 0.2 ml/mice with physiological saline. Samples were filtered through 0.2 μm filters and administered by oral gavage using appropriately sized curved feeding needles. To exclude the presence of endotoxin in nanoparticle samples, an endpoint LAL assay (Lonza, Basel, Switzerland) was performed according to the manufacturer’s instructions. Immediately after the single dose administration, animals were observed for 30 min for post injection reaction. Body weight was recorded and systemic clinical observations for signs of toxicity such as unusual locomotion, bleeding in any orifice, ruffling of fur/skin, lacrimation/ redness of the eye, vasodialation, vasoconstriction, coldness of body, etc. [12] were carried out twice daily for a period of 10 days. Unless animals showed signs of toxicity (greater than 10% animal weight loss consistently for more than 2 days or other clinical signs of toxicity[12]), the acute toxicity study progressed to completion (10 day period). Ten days after administration, mice were individually euthanized using 70% CO2 in oxygen, with euthanasia confirmed by lack of breathing for 30s. Blood was taken via inferior vena cava (IVC) stick, and drawn into a heparinized syringe through a 23G needle and deposited into a blood tube. Blood samples were examined for clotting and/or hemolysis upon collection. Organs (heart, lungs, liver, spleen, kidney, and GI) were removed, weighed and % weight of organ to total body weight calculated to determine organ atrophy/hypertrophy in response to dendrimer administration. Complete blood counts (CBC) were performed within two hours of blood collection using a CBC-DIFF (Heska, Loveland, CO) blood count analyzer. Following CBC, samples were centrifuged at 10,000 rpm for 2.5 minutes. The collected serum samples were used to measure blood urea nitrogen (BUN), creatinine, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) using a DRI-CHEM (Heska, Loveland, CO) veterinary blood chemistry analyzer to examine kidney and liver toxicity. Maximum tolerated dose (MTD) was considered as the maximum dosage of a particular dendrimer that resulted in less than 10% animal weight loss over a period of 10 days or did not manifest any clinical signs of toxicity. At a given dose of a particular dendrimer when overt toxicity was observed the animal was euthanized by CO2 asphyxiation and the dosage of that particular dendrimer was reduced to midway between the current lethal dose and earlier determined maximum dose that was tolerated.
Table 2.
Acute toxicity doses administered orally to CD-1 mice
| Treatment group | No. of mice |
> 10% body weight loss |
Other signs of toxicity |
|---|---|---|---|
| G7 −NH2 | |||
|
| |||
| 50mg/kg | 5 | 1 | Hemobilia |
| 30mg/kg | 5 | 0 | No |
|
| |||
| G7-OH | |||
|
| |||
| 100mg/kg | 5 | 0 | No |
| 300mg/kg | 5 | 1 | Splenomegaly |
| 200mg/kg | 5 | 0 | No |
|
| |||
| G 6.5-COOH | |||
|
| |||
| 100mg/kg | 5 | 0 | No |
| 300mg/kg | 5 | 0 | No |
| 500 mg/kg | 5 | 0 | No |
|
| |||
| G4 −NH2 | |||
|
| |||
| 50mg/kg | 5 | 0 | No |
| 100mg/kg | 5 | 0 | No |
| 300mg/kg | 5 | 0 | No |
|
| |||
| G4-OH | |||
|
| |||
| 100mg/kg | 5 | 0 | No |
| 300 mg/kg | 5 | 0 | Elevated BUN level in 1 mice |
| 500 mg/kg | 5 | 0 | No |
|
| |||
| G3.5-COOH | |||
|
| |||
| 100mg/kg | 5 | 0 | No |
| 300mg/kg | 5 | 0 | No |
BUN - Blood Urea Nitrogen
RESULTS AND DISCUSSION
Physiochemical characterization of PAMAM dendrimers
PAMAM dendrimers were chosen in two different size ranges (~3nm and 8nm) and each of these groups in turn had three different surface groups (hydroxyl, carboxyl and amine) making it a total of six dendritic nanoconstructs (G3.5-COOH, G4-NH2, G4-OH, G6.5-COOH, G7-NH2 and G7-OH) that were studied. Dendrimers were characterized for hydrodynamic size and zeta potential, results of which are presented in Table 1. The absence of small molecular weight impurities was confirmed by size exclusion chromatography and high performance liquid chromatography which have been reported elsewhere[12].
In order to understand results from in vivo toxicity studies it was necessary to employ probes that were well characterized for their physiochemical properties. Interesting to note in the physicochemical characteristics was the fact that in both size ranges evaluated the hydroxyl-terminated dendrimers were smaller than their carboxyl or amine terminated counterparts (diameter measured by DLS) as shown in Table 1. This was probably due to the fact that the amine- or carboxyl-terminated surface groups on the respective dendrimers repel each other at the terminal ends contributing to the expanded conformation in solution whereas the hydroxyl terminated dendrimers being non-charged did not manifest this effect and hence had a collapsed structure. G7-NH2 had a positive zeta potential as expected but the neutral surface group containing G7-OH also had a slight positive charge at pH 7.4 (Table 1). This net positive charge can be attributed to the secondary and tertiary amines present in the structure of the dendrimers.
Acute oral toxicity and maximum tolerated doses of PAMAM dendrimers
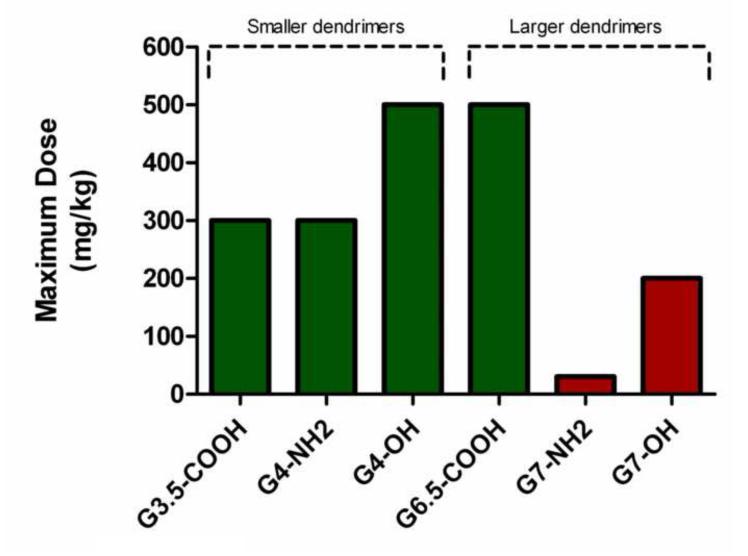
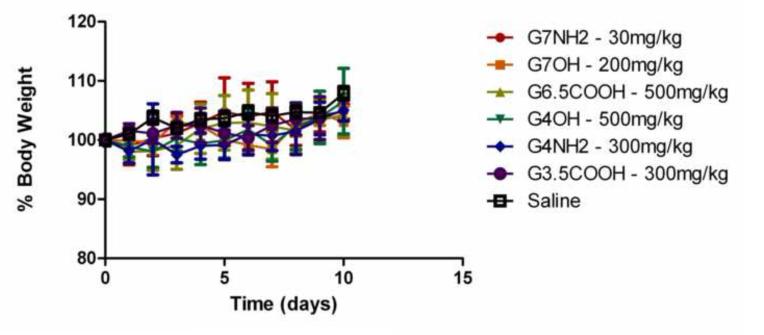
Maximum tolerated doses of the six different dendritic nanoconstructs were determined by a dose escalation study in immune competent CD-1 mice after oral administration. Half-log escalations of dendrimer doses are shown in Table 2. Starting doses were chosen based on earlier studies with systemic administration of dendrimers[12] and oral doses of other polymeric systems[13]. Results indicate that most dendrimers did not show any signs of toxicity after oral administration in CD-1 mice except for G7-NH2 and G7-OH. Maximum doses of the dendrimers with no observable signs of toxicity are reported in Figure 1. Animals in all treatment groups, other than G7-NH2 and G7-OH, did not exhibit any clinical signs of toxicity. Body weights observed over ten days of the study did not show any significant differences from the control group (Figure 2). Various blood parameters measured (RBC, WBC, platelet, ALT, AST, BUN and creatinine levels) also indicated no statistical differences from the control saline group (data not shown). The samples used in the study tested negative for endotoxin contamination (data not shown). Limitations in availability of dendrimer samples restricted the dose escalation study to terminate at a maximum dose of 500 mg/kg (300mg/kg in some cases).
Figure 1.
Maximum tolerated doses (MTD) (in mg/kg) of dendrimers determined by a dose escalation study in CD-1 mice. The acute oral toxicity study revealed that most dendrimers were safe to administer orally except for G7-NH2 and G7-OH, which exhibited signs of toxicity at relatively low dosage.
Figure 2.
Animal weight monitored over ten days as part of the oral acute toxicity study. Six different PAMAM dendrimers were administered orally to a group of five CD-1 mice and their percentage body weight is shown in the graph. Dosages shown here are the respective maximum tolerated doses for each treatment group. Each point in the graph represents Mean ±S.D.
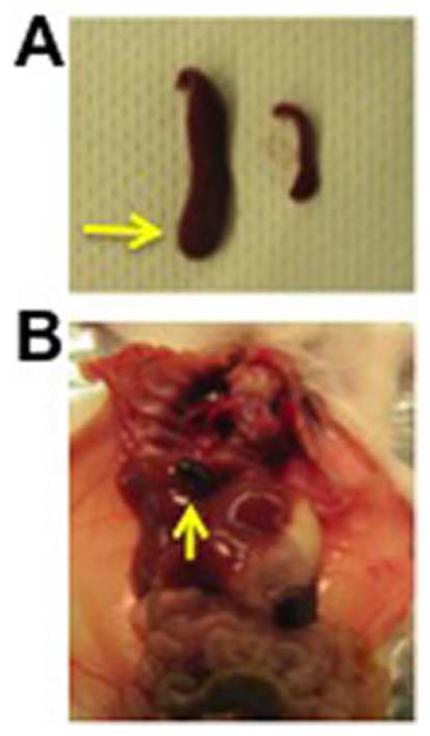
G7-OH dendrimers treated at doses greater than 200mg/kg (MTD) proved to be toxic. One animal from the group treated with G7-OH at 300mg/kg lost greater than 10% of its body weight over three days after administration of the dose. Further investigations at necropsy revealed that the animal had an abnormally enlarged spleen (Splenomegaly) as compared to controls (Figure 3A). Hence, the dosage had to be scaled down from 300mg/kg to 200mg/kg, which proved to be non-toxic. The important physiological function of the spleen, although a non-essential organ, is related to red blood cells (RBC) and the immune system[14]. Orally administered G7-OH dendrimers (positively charged) could induce RBC damage or cause inflammation by increased bacterial exposure rate in the GI tract, which could potentially be captured in the spleen leading to its enlargement.
Figure 3.
Evidence of toxicity with positively charged PAMAM dendrimers. A) Enlarged spleen observed in mice after oral administration of G7-OH at 300 mg/kg. Arrow indicates enlarged spleen as compared to a spleen from control mice. B) Hemobilia, accumulation of blood in gall bladder, observed in mice treated with G7-NH2 at 50 mg/kg. Arrow indicates gall bladder.
The G7-NH2 dendrimer was at least ten times less tolerated than their carboxyl terminated counterparts (G6.5-COOH) with an MTD of 30mg/kg. When administered at 50mg/kg, G7-NH2 dendrimers showed severe signs of hemobilia (Figure 3B) initially identified by greater than 10% weight loss in one mouse. The gall bladder was isolated and further investigation revealed accumulation of blood instead of bile fluid. Therefore, dosage of G7-NH2 was reduced to 30mg/kg (MTD reported) and no sign of toxicity were observed in the group of five mice. Our earlier studies on systemic administration of G7-NH2[12] revealed extensive coagulation and localization in the liver, which could possibily explain the hemobilia observed here. Other causes of hemobilia could include gallstones, injury and inflammation[15].
Other dendrimers (G3.5-COOH, G4-NH2, G4-OH and G6.5-COOH) administered as part of the study did not show any apparent signs of toxicity. The only other abnormality noticed was in the G4-OH (300mg/kg) treatment group where the blood urea nitrogen (BUN) level in one mouse (59.5 mg/dl) was elevated as compared to its co-mates (18.7±3.45 mg/dl) in the treatment group as well as in the control group (22.22±5.2 mg/dl). Outlier analysis revealed that this observation was an anomaly in just one animal. It is noteworthy to mention that no body weight loss or other signs of toxicity were noted in this particular animal. Hence, the next higher dose of G4-OH (500mg/kg) was administered which proved to be non-toxic (n=5).
Oral toxicity evaluations to determine maximum tolerated dose of dendrimers conformed to a general trend in that most dendrimers were safe to administer orally up to a maximum dose of 500 mg/kg (300 mg/kg in some cases) except for G7-OH and G7-NH2. It is interesting to note the correlation between surface charge and toxicity in this particular case. G7-OH (27.7 mV) and G7-NH2 (64.8 mV) were the only PAMAM dendrimers with a positive zeta potential (Table 1) and the only two dendrimers that showed signs of acute toxicity. G7-NH2 with a greater positive zeta potential was less tolerated at 30 mg/kg while G7-OH with a slightly lesser zeta potential was a little more tolerated, at 200 mg/kg. Nevertheless, both of these dendrimers were severely toxic at higher doses (Figure 1A). Although these effects were not uniformly observed in all five mice tested, they were considered substantial since they influenced 20% of the treated population. What is also interesting is the fact that the enlarged spleen observed in the case of G7-OH and hemobilia observed with G7-NH2 are systemic effects implying that these dendrimers needed to have permeated the epithelial barriers in order to cause such an effect systemically. However, since such severe signs of toxicity were observed after oral administration, and also because of other toxic effects reported previously with cationic dendrimers after intravenous administration[12], these dendrimers were not considered safe to be used at these doses. Interestingly G4-NH2 dendrimers, which also have cationic surface groups, exhibited no signs of toxicity (n=5) possibly because of the lower charge density as compared to the larger and denser generation 7 amine-terminated dendrimers. The net charge interacting with epithelial surfaces is weaker in the case of G4- NH2 when compared to G7-NH2.
To put these results into perspective with other orally administered polymeric systems a few examples are discussed below. Chitosan is a widely used positively charged polymer with reported LD50 (Lethal dose) of greater than 1.5 g/kg in rats after oral gavage[16]. Although this is not a head-to-head comparison, and different animal models were used in the two studies, these values are much higher than the MTDs reported for cationic G7 dendrimers after oral administration. This is probably in part due to potential absorption of dendritic systems into systemic circulation, which has been observed with other dendrimer systems[17]. The LD50 of acrylate polymers was reported to be greater than 2g/kg in rats[18]. Anionic G6.5 dendrimers demonstrated similar trends where we did not observe signs of toxicity as 500mg/kg after oral dosage in mice. A detailed comparative study of safety of polymeric carriers upon oral administration however is warranted.
Previously our research group and others have evaluated transepithelial transport of PAMAM dendrimers in vitro, and the influence of generation and surface functionality on toxicity[4, 5, 7, 10, 19]. It has been demonstrated that PAMAM dendrimers open the tight junctions of intestinal epithelial monolayers in cell culture systems, hence contributing to their enhanced transport[20]. In addition they have shown to be transported by endocytotic mechanisms[21, 22]. PAMAM-drug conjugates and complexes have also shown enhanced solubility of the drug and increased transepithelial transport in vitro[23]. These in vitro results bode well for the application of a subpopulation of dendrimers in oral drug delivery. However for a successful development of PAMAM-drug conjugates for oral drug delivery, their safety needs to be established in vivo. The findings of the present study shines light on potential toxic effects associated with PAMAM dendrimers as a function of size and surface charge, and their maximum doses in mice. It appears that anionic PAMAM dendrimers are safer for oral administration. Further expansion of these studies into more probes and understanding of the detailed mechanisms of toxicity are warranted.
ACKNOWLEDGEMENTS
Financial support was provided by the National Institutes of Health Grants (R01EB007470 and R01DE019050), Utah Science Technology and Research (USTAR) initiative and a University of Utah Graduate Research Fellowship.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Thiagarajan G, Ghandehari H. Dendrimers for Drug Delviery. In: Bronzino JD, Peterson DR, editors. The Biomedical Engineering Handbook. CRC Press; 2012. [Google Scholar]
- [2].Svenson S, Tomalia DA. Dendrimers in biomedical applications—reflections on the field. Adv Drug Deliv Rev. 2005;57:2106–2129. doi: 10.1016/j.addr.2005.09.018. [DOI] [PubMed] [Google Scholar]
- [3].Crampton HL, Simanek EE. Dendrimers as drug delivery vehicles: non-covalent interactions of bioactive compounds with dendrimers. Polymer International. 2007;56:489–496. doi: 10.1002/pi.2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].El-Sayed M, Ginski M, Rhodes C, Ghandehari H. Transepithelial transport of poly(amidoamine) dendrimers across Caco-2 cell monolayers. J Control Release. 2002;81:355–365. doi: 10.1016/s0168-3659(02)00087-1. [DOI] [PubMed] [Google Scholar]
- [5].Kitchens KM, Kolhatkar RB, Swaan PW, Eddington ND, Ghandehari H. Transport of poly(amidoamine) dendrimers across Caco-2 cell monolayers: Influence of size, charge and fluorescent labeling. Pharm Res. 2006;23:2818–2826. doi: 10.1007/s11095-006-9122-2. [DOI] [PubMed] [Google Scholar]
- [6].Kolhatkar RB, Swaan P, Ghandehari H. Potential oral delivery of 7-ethyl-10-hydroxy-camptothecin (SN-38) using poly(amidoamine) dendrimers. Pharm Res. 2008;25:1723–1729. doi: 10.1007/s11095-008-9572-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Wiwattanapatapee R, Carreno-Gomez B, Malik N, Duncan R. Anionic PAMAM dendrimers rapidly cross adult rat intestine in vitro: a potential oral delivery system? Pharm Res. 2000;17:991–998. doi: 10.1023/a:1007587523543. [DOI] [PubMed] [Google Scholar]
- [8].Najlah M, Freeman S, Attwood D, D’Emanuele A. In vitro evaluation of dendrimer prodrugs for oral drug delivery. Int J Pharm. 2007;336:183–190. doi: 10.1016/j.ijpharm.2006.11.047. [DOI] [PubMed] [Google Scholar]
- [9].Vijayalakshmi N, Ray A, Malugin A, Ghandehari H. Carboxyl-terminated PAMAM-SN38 conjugates: synthesis, characterization, and in vitro evaluation. Bioconjugate chemistry. 2010;21:1804–1810. doi: 10.1021/bc100094z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kolhatkar RB, Kitchens KM, Swaan PW, Ghandehari H. Surface acetylation of polyamidoamine (PAMAM) dendrimers decreases cytotoxicity while maintaining membrane permeability. Bioconjug Chem. 2007;18:2054–2060. doi: 10.1021/bc0603889. [DOI] [PubMed] [Google Scholar]
- [11].Sadekar S, Ghandehari H. Transepithelial transport and toxicity of PAMAM dendrimers: Implications for oral drug delivery. Adv Drug Deliv Rev. 2012;64:571–588. doi: 10.1016/j.addr.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Greish K, Thiagarajan G, Herd H, Price P, Bauer H, Hubbard D, Burckle A, Sadekar S, Yu T, Anwar A, Ray A, Ghandehari H. Size and surface charge significantly influence the toxicity of silica and dendritic nanoparticles. Nanotoxicology. 2011;6:718–728. doi: 10.3109/17435390.2011.604442. [DOI] [PubMed] [Google Scholar]
- [13].Jani P, Halbert GW, Langridge J, Florence AT. Nanoparticle uptake by the rat gastrointestinal mucosa: quantitation and particle size dependency. J Pharm Pharmacol. 1990;42:821–826. doi: 10.1111/j.2042-7158.1990.tb07033.x. [DOI] [PubMed] [Google Scholar]
- [14].Wilkins BS, Wright DH. Illustrated Pathology of the Spleen. Cambridge University Press; Cambridge, UK: 2000. [Google Scholar]
- [15].Green MHA, Duell RM, Johnson CD, Jamieson NV. Haemobilia. British Journal of Surgery. 2001;88:773–786. doi: 10.1046/j.1365-2168.2001.01756.x. [DOI] [PubMed] [Google Scholar]
- [16].Baldrick P. The safety of chitosan as a pharmaceutical excipient. Regulatory Toxicology and Pharmacology. 2010;56:290–299. doi: 10.1016/j.yrtph.2009.09.015. [DOI] [PubMed] [Google Scholar]
- [17].Thiagarajan G, Sadekar S, Greish K, Ray A, Ghandehari H. Evidence of oral translocation of anionic G6.5 dendrimers in mice. Mol Pharm(Accepted) 2013 doi: 10.1021/mp300436c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Zondlo Fiume M. Final report on the safety assessment of Acrylates Copolymer and 33 related cosmetic ingredients. International Journal of Toxicology. 2002;21(Suppl 3):1–50. doi: 10.1080/10915810290169800. [DOI] [PubMed] [Google Scholar]
- [19].Jevprasesphant R, Penny J, Jalal R, Attwood D, McKeown NB, D’Emanuele A. The influence of surface modification on the cytotoxicity of PAMAM dendrimers. Int J Pharm. 2003;252:263–266. doi: 10.1016/s0378-5173(02)00623-3. [DOI] [PubMed] [Google Scholar]
- [20].Goldberg DS, Ghandehari H, Swaan PW. Cellular entry of G3.5 poly (amido amine) dendrimers by clathrin- and dynamin-dependent endocytosis promotes tight junctional opening in intestinal epithelia. Pharm Res. 2010 doi: 10.1007/s11095-010-0153-3. [DOI] [PubMed] [Google Scholar]
- [21].Kitchens KM, Foraker AB, Kolhatkar RB, Swaan PW, Ghandehari H. Endocytosis and interaction of poly (amidoamine) dendrimers with Caco-2 cells. Pharm Res. 2007;24:2138–2145. doi: 10.1007/s11095-007-9415-0. [DOI] [PubMed] [Google Scholar]
- [22].Kitchens KM, Kolhatkar RB, Swaan PW, Ghandehari H. Endocytosis inhibitors prevent poly(amidoamine) dendrimer internalization and permeability across Caco-2 cells. Mol Pharm. 2008;5:364–369. doi: 10.1021/mp700089s. [DOI] [PubMed] [Google Scholar]
- [23].Goldberg DS, Vijayalakshmi N, Swaan PW, Ghandehari H. G3.5 PAMAM dendrimers enhance transepithelial transport of SN38 while minimizing gastrointestinal toxicity. J Control Release. 2011;150:318–325. doi: 10.1016/j.jconrel.2010.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]