Abstract
This study applies life-course theories of latent (direct), pathway (indirect) and conditional effects in an analysis of childhood poverty on later-life depressive symptoms among older adults in Mexico. Data are from the 2001 Mexican Health and Aging Study (MHAS), a nationally representative sample of older adults born before 1951 (n=8696). Respondents had a mean of 3.6 past-week depressive symptoms and 71 % had no household sanitation facilities before age 10; this measure served as a proxy for childhood poverty. Childhood poverty is significantly related to scores on an adapted 9-item CES-D scale in the full model (b=0.27, p<0.001). This effect is partially mediated by four adult socio-economic status measures, although decomposition analysis reveals the mediation effect to be primarily driven by educational achievement. These findings have important implications for Mexico’s rapidly aging population as well as efforts for childhood poverty reduction and gains in education.
Keywords: Life-course, Childhood socio-economic status, Depressive symptoms, Mexico, Older adults
Introduction
Recent health research has turned its focus to childhood circumstances in order to explain later-life outcomes (Elo and Preston 1992; Hertzman and Boyce 2010; Kuh et al. 2003; Luo and Waite 2005). Studies of the “life-course origins” of later-life health find significant direct and indirect relationships between childhood socio-economic status (SES) and adult health (Haas 2008; Hertzman et al. 2001). However, these studies have historically been conducted in developed countries. Fewer life-course analyses have been completed in the developing country context. Even within life-course studies done in developing countries, mental health outcomes such as depression have rarely been examined. Depression is one of the leading causes of disability worldwide (Murray et al. 2012) and in Mexico (Stevens et al. 2008). The present analysis addresses this gap by looking at the relationship between childhood poverty and current depressive symptoms among a representative sample of older Mexican adults, with particular attention to the life-course mechanisms driving this relationship.
Childhood conditions and older adult health in Latin America and Mexico
Studies influenced by life-course epidemiology have illuminated the importance of considering childhood exposures, including childhood poverty, as a determinant of adult health status and health disparities (Haas 2008; Haas et al. 2012; Hertzman et al. 2001; Luo and Waite 2005). Childhood poverty refers to the deprivation of both material and psycho-social resources that place children at a disadvantage in terms of survival and development (UNICEF 2011). Such adverse conditions in childhood can have irreversible effects on health and development that operate both directly and through other mechanisms, including lower socio-economic attainment in adulthood (Hertzman and Boyce 2010). The effects of childhood exposures to lower relative socio-economic status or conditions of poverty on later-life health may persist regardless of upward socio-economic mobility in adulthood in some cases (Luo and Waite 2005; Poulton et al. 2002).
Research on the links between childhood and adult socio-economic status with later-life health outcomes in Latin America, and Mexico specifically, has grown in recent years (Beltrán-Sanchez et al. 2011; Huang et al. 2011; Kohler and Soldo 2005; Maurer 2010; Monteverde et al. 2009; Nguyen et al. 2008). These studies have been made possible by significant survey data collection efforts among older adults in Latin America (Wong et al. 2006). Collectively, these studies emphasize the importance of considering country and regional contexts in examining the relationship between socio-economic status (SES), including early childhood SES, and later-life health. For example, there is some evidence of a social gradient in health in some areas that is inverse of that observed in the United States, where higher SES is uniformly associated with better health (Smith and Goldman 2007). In addition, studies of older Latin American adults have found education to be more consistently associated with health outcomes relative to adult economic or occupation measures (Maurer 2011). It may be that older adults in Latin America receive significant support from their family members even in the absence of sufficient income or assets at the household level, which may reduce the salience of these later-life economic status indicators for health (Wong and Palloni 2009).
Despite the advances in the literature on early childhood conditions and later-life health in Latin America, there are several important gaps that this analysis seeks to address. One, there has been less attention paid to mental health outcomes of older adults. This is a significant omission, given the increasing global burden of mental health conditions, and depression in particular (Murray et al. 2012). Depression is the leading contributor to disease burden in Mexico (Berenzon et al. 2013), accounting for an estimated 6 % of disability-adjusted life years lost as of 2004 (Stevens et al. 2008). Depression is also strongly associated with other aspects of chronic disease and physical functioning that are of increasing concern for a growing older adult population in Mexico (Wagner et al. 1999).
Estimates of depression among older adults in Mexico vary based on the measure used. Findings from a national health study estimated a 9.6 % lifetime prevalence of major depression among 55–65 year olds using criteria based on the Diagnostic and Statistical Manual (DSM-IV) (Medina-Mora et al. 2007). In a survey that included older adults in rural and urban Mexico, Guerra et al. (2009) estimated a 1.3 % 12-month prevalence of major depression using the DSM-IV, which specifies that depression be unrelated to bereavement and be severe enough to cause ‘clinically significant distress or impairment’. The same study reported a 32 % prevalence of clinically significant depression, more broadly defined, with estimates ranging from about 16.7 % for urban and rural Mexican men between 65 and 69 years old to 44 % for rural Mexican women in the same age group.
Two, another deficit in the extant literature is the insufficient attention paid to the relationship between socio-economic and health conditions in childhood and later-life depression generally. Alvarado et al. (2007) reported a significant association between childhood hunger and the odds of severe depression for Latin Americans in older adulthood, although this study was limited to respondents in urban areas, including Mexico City, and not generalizable to all of Mexico. Other studies have limited their analysis of the link between life-course socio-economic and health conditions and later-life depression to measures of educational attainment or adult socio-economic and health status (Bojorquez-Chapela et al. 2012; Guerra et al. 2009), and not examined the long-term association between childhood conditions and later-life depressive symptoms.
Three and finally, even within the broader literature on early-life contributors to later-life health in Latin America, there has been limited conceptualization of the mediators or pathways linking childhood poverty to later life health. For example, Huang et al. (2011) identify a broad set of mediating variables, including adult health, health behaviors and socio-economic status, that might link early childhood health and socio-economic conditions to later-life physical functioning for older Mexican adults. However, the authors simultaneously add both educational attainment and lifetime occupation as a “set” of mediating variables. The inclusion of these two measures at once assumes that each intervenes simultaneously across the life-course, and that each equally explains the relationship between childhood conditions and later-life health, which may or may not be the case in the Mexican context. This paper aims to pay particular attention to the relative contribution of adult socio-economic mediators of the relationship between childhood poverty and later-life depressive symptoms by way of considering several theories related to the life-course perspective.
Conceptual Framework
Broadly, the life-course perspective acknowledges the contribution of earlier life conditions on adult health outcomes, including mental health (Kuh et al. 2003). Researchers using this perspective elaborate three key ways in which early childhood circumstances may influence later-life depressive symptoms and other health outcomes: latent mechanisms, pathway effects, and conditional effects (Hertzman and Boyce 2010).
Latent or direct effects refer to childhood exposures that affect later life-course health outcomes, regardless of adult conditions. Latency mechanisms are generally associated with the fetal origins hypothesis, whereby adverse fetal environment and birth outcomes have an irreversible, negative influence on health across the life-course (Barker 1993). However, there may be long-term consequences of conditions extending from the gestational period through childhood given the critical cognitive, psychological and social developments occurring during this period (Hertzman and Boyce 2010). These latency mechanisms may account for the direct association between childhood poverty and later-life depression, net of adult socio-economic attainment and other factors. The lasting, direct effects of material deprivation during childhood may be particularly important for older adults in Mexico. Current older adults in Mexico generally faced conditions of extreme poverty over their lifetime, even as their life expectancy rapidly increased due to improved medical technologies (Wong and Palloni 2009). Given the potential for direct effects of childhood conditions on adult health, we hypothesize that childhood poverty will be significantly associated with increased depressive symptoms later in life even when including a number of controls related to mid-life health and socio-economic status.
Pathway mechanisms suggest that childhood conditions might influence later-life health indirectly, by facilitating or constraining later-life opportunities such as educational attainment that in turn affect health outcomes. Under this perspective, early childhood conditions are important only to the extent that they predict educational, occupational and economic attainment. O’Rand (1996) describes the process of how childhood socio-economic status (SES) links to adult SES, suggesting that institutions like the educational system stratify socio-economic chances by “allocate[ing] value, protection and reward over time in ways that reinforce or ameliorate inequalities” (p.231). Children living in poverty may never receive the kinds of institutional protections that may enable them to later obtain formal education, and subsequently employment, income and wealth that might be protective of health. Education in turn contributes to health by leading to better economic and occupational standing as well as improved coping resources, social support and a greater sense of control over one’s life, which might be particularly important for depression outcomes (Pearlin et al. 2005; Ross and Wu 1995).
Pathway or indirect effects of childhood poverty on later-life health often occur alongside direct or latent mechanisms. We therefore hypothesize that the association between childhood poverty and depressive symptoms later in life will be partially mediated by measures of adult socio-economic status. That is, part of the effect of childhood poverty on depressive symptoms will be an indirect effect, through the influence of childhood poverty on educational attainment, lifetime occupation and adult income and wealth. Given observations from the Latin American literature emphasizing education as the primary socio-economic predictor of later-life health, we expect that education will account for most of the indirect or mediated effect of childhood poverty on depressive symptoms.
This analysis will also assess the possibility of conditional effects, testing the notion that the relationship between childhood poverty and later-life depressive symptoms depends on the levels of socio-economic attainment achieved in adulthood. For example, it may be that high levels of education act as a buffer in the relationship between childhood poverty and later-life depression by undoing some of the damage of early material and psycho-social deprivation—related to the construct of social mobility across the life-course (Luo and Waite 2005). Finally, it may be that education matters more for later-life depression outcomes for those who lived in poverty as a child. The same amount of educational attainment might have a more beneficial influence on mental health outcomes for those who experienced socio-economic deprivation early on as compared to those who started accruing material and social advantage.
Negative results for conditional effects would indicate the persistence of the adverse effects of childhood poverty on health regardless of upward or downward mobility during adulthood (Poulton et al. 2002). Given the possibility of conditional effects, we hypothesize that there will be a significant interaction between childhood poverty and education in the effect on later-life depressive symptoms whereby the association between childhood poverty and depressive symptoms will be weaker for those with greater educational attainment. A significant interaction between childhood poverty and education in the effect on depressive symptoms may be interpreted as a buffering effect of education on the relationship between adverse childhood conditions and adult health.
Methods
Data
Data for this analysis comes from the baseline (2001) wave of the Mexican Health and Aging Study (MHAS), a national survey of Mexican adults born before 1951. The MHAS used a multistage area probability sample, stratifying by two Mexican regions consisting of: 1) six states with high rates of out-migration to the United States and 2) the remaining 26 states and the Federal District of Mexico (Wong and Espinoza 2004). The MHAS selected households with adults 50 years and older included in the nationally representative 2000 Mexican Employment Survey (ENE-2000). Households in heavy out-migration states were oversampled and those in the remaining states were selected with probability proportionate-to-size.
At the household level, each adult 50 years or older had an equal probability of being selected, proportionate to the number of age-eligible adults in the household. Spouses or cohabitating partners were also interviewed. Proxy interviews were completed for respondents who could not answer due to health problems including cognitive impairment, or language difficulties. The MHAS collected data from a total of 15,156 respondents, spouses and proxies, with a non-response rate of 10.3 %. Of these interviews, spouse interviews (n=5609) and proxy interviews (n=715) are excluded. Another 136 cases missing data on demographic characteristics (2 %) were excluded, yielding a final analytic sample of 8696 respondents.
The exclusion of proxy interviews may bias the sample towards healthier individuals with more education, given that health and language difficulties were primary reasons for interviewing a proxy. In addition, this study excludes individuals in long-term care facilities, although this represents a small very small fraction of the total older adult population in Mexico (Wong et al. 2006). These parameters may skew the MHAS sample towards younger adults with better physical, mental and cognitive health indicators. While we cannot correct for this bias in our analysis, it is possible that we slightly underestimate the association between poor childhood conditions and later-life depressive symptoms with our relatively healthy sample. Finally, although the baseline version of the MHAS was completed nearly a decade ago, it is unique in its inclusion of a nationally representative sample of middle-aged and older Mexican adults, and its assessment of socio-economic status indicators across the life-course in addition to multiple health outcomes.
Measures
Dependent variable
We measured respondents’ past-week depressive symptoms with a nine item scale adapted from the Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff 1977). Respondents were asked to indicate if for the majority of the past week they felt the following: depressed, lonely, sad, tired, that everything they did was an effort, or that their sleep was restless. An additional three positively worded items were included: whether respondents felt happy, enjoyed life, or felt they had a lot of energy. Each item originally had a response code of 1 for a “yes” and 0 for a “no” answer. The three positively worded items were reverse coded and all of the items were summed such that higher scores indicated more depression-related feelings (range: 0–9).
We note that the adaptation of Radloff’s original 20-item CES-D scale for use in the MHAS follows changes made for studies of older adults in the US (Irwin et al. 1999), including the Health and Retirement Study (HRS). Aside from reducing the number of scale items, the MHAS version includes binary “yes”/“no” response categories rather than the original four-item response categories asking about frequency of depressive symptoms in the past week. In addition, the original CES-D scale did not include the question about having “a lot of energy”; this item was added as part of the abbreviated version of the scale included in the HRS. The CES-D scale, including the adapted version used in the MHAS, has been validated for use among older adult populations in Mexico (Aguilar-Navarro et al. 2007; Sánchez-García et al. 2008). The scale has a reliability coefficient of α=0.80 for our analytic sample.
Finally, in addition to using a continuous measure of past-week depressive symptoms, we consider a binary measure based on a cut-off score of five or more points (out of nine possible points). This cut-off score was selected based on the results of a validation study of the adapted CES-D scale used in the MHAS for a clinic-based sample of older Mexican adults which found that a five point cut-off maximized both sensitivity and specificity of the scale when compared to diagnoses of depressive disorder using the Diagnostic and Statistical Manual, Fourth Edition (80.7 % sensitivity, 68.7 % specificity) (Aguilar-Navarro et al. 2007).
Key independent variable
Child poverty is captured by whether or not respondents had sanitation facilities in their household before age 10. This measure is based on literature from international agencies that suggest that childhood poverty be measured with indicators related to nutrition, health, sanitation facilities, shelter and education rather than household income or consumption, given that earnings and expenditures are not evenly distributed within the household (UNICEF 2011).
Mediating variables
We test several measures of socio-economic status from childhood to adulthood. The measure of education includes three categories indicating respondents who have no formal education, those who completed some primary education (1–5 years), and those who completed a primary school education or more (6 or more years). Occupational status was based on respondents’ primary lifetime occupation based on the Mexican Classification of Occupations and grouped into six broad categories: professional/administrative, agricultural, service sector (including informal services), factory/industrial, domestic labor and no history of work (INEGI, 2010). We analyzed mean depressive symptoms across categories for men and women separately, given gendered differences in occupational patterns (e.g. women are more likely to have no work history). Given the relative disadvantage of those with a history of domestic or agricultural work in terms of current depressive symptoms, these two occupations were grouped together as indicating low occupational status, compared with the remaining four categories.
Net monthly income was calculated at the household level using a series of questions asking about the balance of respondents’ positive earnings (e.g. employment income and pensions) with debts and expenditures. Respondent wealth was calculated with information about their total assets, including property and savings, as well as debts. Missing data for these measures were imputed by the MHAS study team (Wong and Espinoza 2004). We categorize these variables into quintiles and present them in terms of US dollars based on the conversion in 2000 of roughly 10 Mexican pesos to $1 US dollar.
Covariates
The analysis accounts for measures of migration history and health status, given their potential importance in additionally mediating the effects of childhood poverty on later-life depression outcomes. Measures of personal ever-migration include no history of migration, internal migration, and international migration, which is primarily to the US. These are mutually exclusive categories; migrants who were both internal and international migrants are counted as international migrants.
Health measures at different life course stages are included in order to disentangle the effect of childhood living conditions on adult health from their effects on adult socio-economic attainment. To indicate childhood health status, respondents were asked if before age 10 they experienced an adverse health event that prevented them from carrying out normal activities for a month or more. Respondents were also asked whether or not they had ever been diagnosed with a number of chronic health conditions, including hypertension, diabetes, cancer, respiratory illness, or ever had a heart attack or stroke. These responses were collapsed to indicate if respondents had ever been diagnosed with any chronic condition (yes/no). Respondents who had never seen a doctor (n=211) were scored as “no”, although this may result in some error given the possibility of undiagnosed conditions. Finally, a measure of recent, relative health status was also included. Respondents were asked whether their health was better, the same or worse compared with two years ago and these categories were retained as such.
Socio-demographic measures
Additional covariates include gender and age. Age is a binary measure with categories of 50–59 years old compared to 60 years or older. Given the possibility that older respondents may have experienced higher levels of material deprivation in childhood than younger respondents, even with the same indicator of household sanitation facilities as a child, we consider an interaction term between age and the indicator of childhood sanitation facilities. Marital status is categorized as married or in a consensual union, never married, divorced or separated, and widowed. We additionally tested a measure of living arrangements (e.g. living alone, with spouse/partner, or other family members) in order to indicate family-level social and instrumental support, which may buffer the adverse impacts of socio-economic disadvantage on health. However, we found this measure to be highly collinear with marital status and preferred not to include it in the analysis given similar findings.
Respondents are also classified according to whether or not they live in an urban area, defined as having at least 100,000 residents. Finally, we included a measure of whether or not respondents resided in one of six states in Western Mexico with heavy out-migration to the US between 1990–1995, given that households were oversampled from these states (Wong and Espinoza 2004)
Analysis
We first obtained descriptive statistics, both with and without weights that reflect the unequal probability of selection into the MHAS sample based on age, gender and residence in both urban centers and high out-migration states. Our subsequent analysis followed the conceptual model presented in Fig. 1, whereby the bivariate relationship between childhood poverty and past-week depressive symptoms is first estimated using Ordinary Least Squares linear regression (Model 1). We then estimated a series of multiple regression models, first adding socio-demographic and health-related covariates (Model 2). We then added level of education (Model 3) and subsequently added variables of occupation, income and wealth (Model 4) to assess the additional mediating effect of adult socio-economic status beyond education.
Fig. 1.
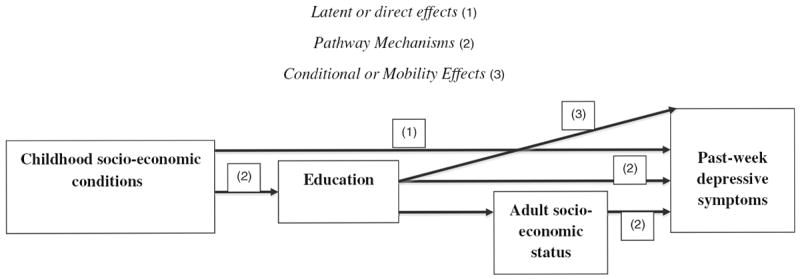
Conceptual framework of the relationship between childhood socio-economic and health conditions and past-week depressive symptoms for a sample of middle-aged and older Mexican adults, 2001
We conducted formal tests of mediation, including the Sobel-Goodman test (Goodman 1960) and the “khb” analysis, which decomposes the effects of multiple mediating variables in regression analyses (Kohler et al. 2011). This method permits the assessment of the relative contribution of each of the four socio-economic status mediating variables. We additionally tested interaction terms between the measure of sanitation facilities during childhood and educational attainment and other adult SES measures, respectively, to assess whether the relationship between childhood exposures and later-life depressive symptoms was conditional on intervening socio-economic achievement. We re-tested all results using negative binomial regression, although given similar findings we prefer OLS regression given the ease of assessing mediation effects with a linear model.
Finally, in order to approximate the relevance of our childhood poverty measure to clinical depressive disorder, we estimated a logistic regression model where the outcome was the log-odds of reporting five or more depressive symptoms. We include the full set of covariates in this model. All regression models are unweighted and instead include the variables used to construct the probability weights (i.e. age, gender, urban residence and high out-migration state residence). All analyses were done using STATA v.12.
Results
Sample description
Fewer than half of respondents are between 50 and 59 years of age, with the remaining respondents 60 years and older (Table 1). Forty-eight percent of respondents live in an urban area and about 18 % live in six high out-migration states. Furthermore, while nearly 40 % of respondents never migrated from their home communities, 8 % had migrated internationally in their lifetime. The remaining 53 % migrated internally to either rural or urban areas. Respondent health measures indicate that about 10 % had an adverse health event before age 10. Nearly half (46 %) had been diagnosed with a chronic health condition by the time of the survey and over a third of respondents reported a relative decline in their health compared to 2 years previous.
Table 1.
Descriptive statistics for socio-demographic, migration and health measures for a national sample of Mexican adults born before 1951 (n=8696)
| n | % | |
|---|---|---|
| 50–59 years old | 4110 | 46.0 |
| Female | 4781 | 53.6 |
| Marital status | ||
| Married/Consensual Union | 4990 | (55.7) |
| Never married | 481 | (6.2) |
| Divorced/separated | 1038 | (13.3) |
| Widowed | 2187 | (24.8) |
| Urban residencea | 5870 | (47.7) |
| Residence in high out-migration stateb | 2399 | (18.4) |
| Migration history | ||
| No migration | 3145 | (39.3) |
| Domestic migration | 4731 | (52.6) |
| US migration | 820 | (8.0) |
| Health status | ||
| Adverse childhood health event before age 10 | 956 | (9.9) |
| Any chronic health condition, current | 4290 | (45.8) |
| Relative health status, compared to 2 years ago | ||
| Better health | 1009 | (11.8) |
| Same health | 4816 | (54.0) |
| Worse health | 2871 | (34.2) |
| Past-Week depressive symptoms | ||
| Number of depressive symptoms (range: 0–9), mean (SD)c | 3.58 (2.69) | |
| Five or more depressive symptoms | 3122 | (38.8) |
Mexican Health and Aging Study, 2001
Percentages>100 due to rounding error
Ns are unweighted and percentages are weighted to reflect unequal probability of inclusion in the sample
Urban residence defined as≥100, 000 residents
Based on 1990–1995 out-migration data (Durango, Guanajuato, Michoacan, Nayarit, Jalisco and Zacatecas)
Mean is weighted
Finally, for the dependent variable, respondents on average reported between three and four depressive symptoms feelings for the majority of the prior week, out of nine possible depressive symptoms on the adapted CES-D scale (mean=3.6, SD=2.7). A weighted estimate indicates that 38.8 % of respondents reported five or more past-week depressive symptoms. This is higher than the estimated 32 % of older Mexican adults classified as having clinically significant depression in the past-month by Guerra et al. (2009), albeit using different measures, time frame, and geographic coverage compared to the MHAS.
Table 2 presents results for variables related to socio-economic status across the life-course. Overall, current older adults in Mexico had relatively low SES in childhood. Over two-thirds of respondents did not have sanitation facilities in their home before age 10. The majority of respondents had less than a primary school education, with 30 % reporting no formal education and another 65 % reporting between 1 and 5 years of schooling. Fewer than 5 % completed primary school or went further with their education. Nearly forty-percent labored in lower-status occupations during their working life, which include the agricultural and domestic sectors. Quintiles of monthly household income, constructed based on unweighted data, suggest that those in the lowest quintile had either no monthly income or negative monthly income due to debts or expenditures exceeding income, while those in the highest quintile reported monthly incomes of $421 US dollars or more. Those in the lowest wealth quintiles reported net assets of $3500 US dollars or less. Those in the highest wealth quintile reported net assets of $52,256 US dollars or more, with most of that coming from home ownership (Wong and Palloni 2009).
Table 2.
Descriptive statistics for indicators of childhood and adult socio-economic status (SES), Mexican adults born before 1951 (n=8696)
| n | % | |
|---|---|---|
| No household sanitation facilities before age 10 | 5740 | 71.9 |
| Education | ||
| No formal education | 2180 | 30.3 |
| Some primary school (1–5 years) | 5990 | 65.0 |
| Primary school or more (6+ years) | 526 | 4.7 |
| Domestic or agriculture occupation | 2783 | 38.3 |
| Monthly household incomea | ||
| 1st quintile (≥ USD $420.8) | 1759 | 18.2 |
| 2nd quintile (≥ USD $178.3 to<$420.8) | 1739 | 18.7 |
| 3rd quintile (≥ USD $70.8 to<$178.3) | 1745 | 19.7 |
| 4th quintile (≥ USD $0 to<USD $ 70.8) | 1461 | 19.2 |
| 5th quintile (Negative or no income) | 1992 | 24.2 |
| Net assets | ||
| 1st quintile (≥ USD $52256) | 1753 | 18.4 |
| 2nd quintile (≥ USD $26900 to<$52256) | 1743 | 18.8 |
| 3rd quintile (≥ USD $12900 to<$26900) | 1735 | 18.8 |
| 4th quintile (> USD $3500 to<$12900) | 1728 | 20.2 |
| 5th quintile (≤ USD $3500) | 1737 | 23.9 |
Mexican Health and Aging Study, 2001. Ns are unweighted and percentages are weighted to reflect unequal probability of inclusion in the sample
Income and wealth measures include net income and assets of the respondent and spouse or partner, if applicable. Income and wealth are provided in US dollars (US$1=10 pesos in 2000)
Results from multiple regression models and mediation analyses
Table 3 first presents the bivariate relationship between household sanitation facilities as a child and depressive symptoms at 50 years or older (Model 1). The resulting coefficient suggests that unadjusted for other factors, reporting no sanitation facilities in one’s household before age 10 was associated with a 0.71 point higher score on the 9-item scale of past week depressive symptoms (p<0.001). Given a response range of 0–9 points, this coefficient represents about 8 % of the distance between no depressive symptoms in the past-week and the extreme case of nine such symptoms, suggesting a modest, but non-trivial effect of childhood poverty on later-life depressive symptoms without any controls.
Table 3.
Regression coefficients and standard errors for Ordinary Least Squares regression models of past-week depressive symptoms (9-item CES-D, range 0–9) on an indicator of childhood poverty, adult socio-economic status and covariates for a national sample of Mexican adults born before 1951 (n=8696)
| Model 1 (Bivariate)
|
Model 2 (Add Covariates)
|
Model 3 (Add Education)
|
Model 4 (Add Other SES)
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | b | SE | b | SE | b | SE | |||||
| No household sanitation facilities before age 10 | 0.71 | *** | (0.06) | 0.47 | *** | (0.06) | 0.35 | *** | (0.06) | 0.27 | *** | (0.06) |
| Socio-demographic characteristics | ||||||||||||
| 50 to 59 years old (Ref: Age 60 and older) | −0.19 | ** | (0.06) | −0.14 | * | (0.06) | −0.13 | * | (0.06) | |||
| Female | 0.75 | *** | (0.06) | 0.70 | *** | (0.06) | 0.72 | *** | (0.06) | |||
| Marital status (Ref: Married) | ||||||||||||
| Never married | 0.15 | (0.12) | 0.19 | (0.12) | 0.15 | (0.12) | ||||||
| Divorced/separated | 0.53 | *** | (0.08) | 0.52 | *** | (0.08) | 0.47 | *** | (0.09) | |||
| Widowed | 0.62 | *** | (0.07) | 0.59 | *** | (0.07) | 0.56 | *** | (0.07) | |||
| Urban residencea (Ref: Rural residence) | −0.19 | ** | (0.06) | −0.13 | * | (0.06) | −0.06 | (0.06) | ||||
| Residence in high out-migration state (Ref: Other state)b | 0.37 | *** | (0.06) | 0.37 | *** | (0.06) | 0.39 | *** | (0.06) | |||
| Migration history (Ref: No migration history) | ||||||||||||
| Domestic migration | 0.06 | (0.06) | 0.07 | (0.06) | 0.07 | (0.06) | ||||||
| US migration | −0.04 | (0.10) | −0.03 | (0.10) | −0.02 | (0.10) | ||||||
| Health status | ||||||||||||
| Adverse childhood health event before age 10 | 0.55 | *** | (0.08) | 0.55 | *** | (0.08) | 0.56 | *** | (0.08) | |||
| Any chronic health condition, current | 0.45 | *** | (0.05) | 0.44 | *** | (0.05) | 0.44 | *** | (0.05) | |||
| Relative health status (Ref: Better than 2 years ago) | ||||||||||||
| Same as two years ago | −0.27 | ** | (0.08) | −0.25 | ** | (0.08) | −0.23 | ** | (0.08) | |||
| Worse than 2 years ago | 1.41 | *** | (0.09) | 1.38 | *** | (0.09) | 1.37 | *** | (0.09) | |||
| Socio-economic status | ||||||||||||
| Education (Ref: No formal education) | ||||||||||||
| Some primary school | −0.31 | *** | (0.06) | −0.21 | ** | (0.07) | ||||||
| Primary school or more | −1.00 | *** | (0.13) | −0.71 | *** | (0.13) | ||||||
| Domestic or agricultural occupationc | 0.18 | ** | (0.06) | |||||||||
| Monthly Income (Ref: 5th quintile, negative or no income)d | ||||||||||||
| 1st quintile (≥ USD $420.8) | −0.25 | ** | (0.08) | |||||||||
| 2nd quintile (≥ USD $178.3 to<$420.8) | −0.17 | * | (0.08) | |||||||||
| 3rd quintile (≥ USD $70.8 to<$178.3) | 0.05 | (0.08) | ||||||||||
| 4th quintile (≥ USD $0 to<USD $ 70.8) | 0.06 | (0.08) | ||||||||||
| Net Assets (Ref: 5th quintile, $3500 or less) | ||||||||||||
| 1st quintile (≥ USD $52256) | −0.34 | *** | (0.09) | |||||||||
| 2nd quintile (≥ USD $26900 to<$52256) | −0.26 | ** | (0.08) | |||||||||
| 3rd quintile (≥ USD $12900 to<$26900) | −0.07 | (0.08) | ||||||||||
| 4th quintile (> USD $3500 to<$12900) | −0.01 | (0.08) | ||||||||||
| Constant | 3.11 | *** | 2.09 | *** | 2.41 | *** | 2.46 | *** | ||||
| R-squared | 0.02 | 0.19 | 0.19 | 0.20 | ||||||||
| Adjusted Wald Test | 135.9 | *** | 142.3 | *** | 129.4 | *** | 86.0 | *** | ||||
Mexican Health and Aging Study, 2001
Urban residence defined as≥100, 000 residents
Based on 1990–1995 out-migration data (Durango, Guanajuato, Michoacan, Nayarit, Jalisco and Zacatecas)
Occupational categories included in the reference group are construction, service, professional, other, and no formal work history
Income and wealth data include net income and/or assets of the respondent and spouse or partner, if applicable. Income and wealth are provided in US dollars (US$1=10 pesos in 2000)
p<0.05,
p<0.01,
p<0.001
Model 2 adjusts for a set of covariates that may confound the relationship between childhood poverty and later-life depression in addition to migration and health-related mediating variables. Adding socio-demographic and health-related covariates to the regression analysis resulted in a 34 % decrease in the coefficient for the measure of no household sanitation facilities – from b=0.71 to b=0.47 points, although still significant (p<0.001). Additional three-variable analyses of the relationships between each of these variables (not shown) suggest that respondent age partially confounded the relationship between childhood poverty and later-life depression, given that younger respondents as a whole would have benefitted from more widespread economic and social development than older respondents, and are more likely to have had basic infrastructure like household sanitation facilities on average. However, the indicator of childhood poverty remained significant, even when controlling for age and possible intervening factors like childhood and adult health status.
Several other covariates appear important in this model, including gender, marital status and health status. Female gender was associated with an additional 0.75 points in the scale of past-week depressive symptoms compared to men, all else equal (p<0.001). Being divorced/separated or widowed were each associated with 0.5 and 0.6 additional past-week depressive symptoms compared to those married or in a consensual union at the time of the survey, respectively (both, p<0.001). Personal migration history was not significantly associated with depressive symptoms in this multivariate model despite its significance in bivariate analysis, suggesting that there are no significant differences in depression across individuals with different migration histories, or that this effect is confounded by other variables like gender. Residence in a high out-migration state was associated with 0.4 points higher on the adapted CES-D scale, perhaps attributed to more tenuous social networks in these states due to international migration (Massey et al. 1990). All health measures were significantly associated with past-week depressive symptoms – adverse childhood health events and any chronic health condition were associated with 0.55 and 0.45 points higher on the scale of past-week depressive symptoms, respectively (p<0.001). Finally, having worse health status than 2 years prior was associated with 1.4 points higher on the adapted CES-D scale compared to better health status (p<0.001).
Model 3 includes the education variable, which resulted in a 26 % reduction in the regression coefficient for the indicator of childhood poverty, from b=0.47 to b=0.35. There was no observable reduction in the significance level for the measure of household sanitation facilities during childhood. A Sobel-Goodman test of mediation (results not shown) partitioned the total effect of the childhood poverty measure into direct and indirect effects. The coefficient for the indirect effect (b=0.12) suggests that reporting no household sanitation facilities as a child, a proxy for childhood poverty, was associated with a 0.12 point increase in past-week depressive symptoms for MHAS respondents through its effect on educational attainment. The coefficient that remained when controlling for education (b=0.35) indicates the direct effect of childhood poverty on later-life depression, or that mediated by as-yet unmeasured factors.
In addition, the coefficients for the education measure suggest that having some formal education was associated with lower past-week depressive symptoms in older adulthood compared with having no formal education. Specifically, reporting at least some primary schooling (1–5 years of education) was associated with a 0.31 points lower on the scale of past-week depressive symptoms compared with those who had no formal education, all else equal (p<0.001). Those who had a full primary education or more (6 or more years of education) were associated with one full point lower on the adapted CES-D scale (b=−1.00, p<0.001) compared with those who had no formal education net of other variables in the model. The magnitude of the association for those with primary education or more was greater than for all other demographic and health covariates, with the exception of the measure indicating a significant health decline in the past 2 years.
The subsequent model adds the three additional measures of adult SES: domestic or agricultural occupation, and quintiles of wealth and income. Reporting domestic or agricultural lifetime occupations was significantly associated with higher scores on the measure of past-week depressive symptoms (b=0.18, p<0.01) compared with having higher-status occupations, including professional occupations and homemaking for female respondents. There was also a significant association between being in the highest quintiles of income and wealth, respectively, and lower scores on the past-week depressive symptoms measure when compared to those in the lowest income and wealth quintiles. For example those in the highest household income quintile, making $421 US dollars or more per month, were associated with an adapted CES-D score that was 0.25 points lower than for those with either no or negative monthly income, all else equal (p<0.01). However, there were no significant differences in past-week depressive symptoms for those in the other income quintiles relative to those with no or a negative household income. Those in the two highest wealth quintiles were associated with significantly lower scores on the past-week depressive symptoms scale compared to those in the lowest wealth quintile, with $3500 US dollars or less in net assets.
The measure of household sanitation facilities as a child remained significant at p<0.001 even when adding the adult socio-economic status (SES) measures. However, the addition of these adult SES variables resulted in a 23 % decrease (from b=0.35 to b=0.27) in the coefficient for the measure of childhood socio-economic status, or having household sanitation facilities as a child, suggesting additional indirect effects of childhood poverty on later-life depressive symptoms through its effect on adult socio-economic attainment. A decomposition analysis of the mediating effects of each of the socioeconomic status variables using the −khb- function confirms the importance of education relative to the other measures in mediating the relationship between childhood poverty and past-week depressive symptoms later in life (Table 4). Specifically, about 47 % of the indirect effect of childhood poverty on past-week depressive symptoms was accounted for by the education measure. The remaining indirect effect was split somewhat evenly between the additional adult socio-economic status measures although wealth appeared to be a slightly more important mediator than lifetime occupation or monthly income. Some of the effect of education was itself mediated by the other measures of adult socio-economic status, suggesting that the effect of educational attainment on past-week depressive symptoms later in life is in part due to the influence of education on occupational choice, income and wealth acquisition.
Table 4.
Decomposition of mediation effects of four measures of adult socio-economic status in the OLS regression of depressive symptoms on childhood poverty for Mexican adults born before 1951 (n=8696)
| Decomposition of total effects of childhood poverty on depressive symptoms | |||
|---|---|---|---|
| b | SE | ||
| Direct effectsa | 0.27 | ** | (0.06) |
| Indirect effects | 0.19 | *** | (0.03) |
| Total effects | 0.47 | *** | (0.06) |
| Components of indirect effectsb | |||
| b | SE | % indirect effects | |
| Education, y | 0.09 | (0.02) | 47.4 |
| Domestic or agricultural occupation | 0.03 | (0.01) | 15.8 |
| Net income, per month | 0.03 | (0.01) | 15.8 |
| Net assets, total | 0.04 | (0.01) | 21.0 |
Mexican Health and Aging Study, 2001
Decomposition effects estimated from a regression model including controls for socio-demographic and other health status indicators (see Model 4, Table 3), although education, income and net assets indicators are continuous
In Table 5 we present the results of the full multivariate model using a logistic regression analysis assessing the odds of reporting five or more past-week depressive symptoms. We found that even when controlling for the complete set of adult health and socio-economic status indicators and other covariates, there was a significant association between having no household sanitation facilities as a child and the odds of reporting five or more past-week depressive symptoms, a proxy for clinical depression. Specifically, those who reported having no sanitation facilities as a child had 19 % greater odds of reporting five or more past-week depressive symptoms compared with those who reported having household sanitation facilities, all else equal (OR: 1.19; 95 % CI: 1.06, 1.34).
Table 5.
Odds ratios and 95 % confidence intervals for logistic regression of 5 or more past-week depressive symptoms on an indicator of childhood poverty, adult socio-economic status and covariates for Mexican adults born before 1951 (n=8696)
| OR | 95 % CI | |
|---|---|---|
| No household sanitation facilities before age 10 | 1.19** | (1.06, 1.34) |
| Socio-demographic characteristics | ||
| 50 to 59 (Ref=60 year or older) | 0.95 | (0.85, 1.05) |
| Female | 1.82*** | (1.63, 2.03) |
| Marital status (Ref=Married) | ||
| Never married | 1.23 | (0.99, 1.53) |
| Divorced/separated | 1.56*** | (1.34, 1.83) |
| Widowed | 1.56*** | (1.38, 1.77) |
| Urban residencea | 0.89 | (0.80, 0.99) |
| Residence in high out-migration stateb | 1.39*** | (1.25, 1.55) |
| Migration history (Ref=No Migration) | ||
| Domestic migration | 1.11* | (1.00, 1.24) |
| US migration | 1.14 | (0.95, 1.37) |
| Health status | ||
| Adverse childhood health event before age 10 | 1.57*** | (1.35, 1.82) |
| Any chronic health condition, current | 1.65*** | (1.50, 1.82) |
| Relative health status (Ref=Better than 2 years ago) | ||
| Same as 2 years ago | 0.85* | (0.72, 0.99) |
| Worse than 2 years ago | 2.60*** | (2.22, 3.05) |
| Socio-economic status | ||
| Education (Ref=No formal education) | ||
| Some primary school | 0.82** | (0.73, 0.93) |
| Primary school or more | 0.58*** | (0.43, 0.77) |
| Domestic or agricultural occupation | 1.11 | (0.99, 1.24) |
| Monthly Income (Ref=5th quintile, negative/no income)c | ||
| 1st quintile (≥ USD $420.8) | 0.78** | (0.66, 0.91) |
| 2nd quintile (≥ USD $178.3 to<$420.8) | 0.83* | (0.72, 0.97) |
| 3rd quintile (≥ USD $70.8 to<$178.3) | 0.96 | (0.83, 1.11) |
| 4th quintile (≥ USD $0 to<USD $ 70.8) | 1.03 | (0.88, 1.19) |
| Net assets (Ref=5th quintile, <$3500) | ||
| 1st quintile (≥ USD $52256) | 0.73*** | (0.62, 0.86) |
| 2nd quintile (≥ USD $26900 to<$52256) | 0.76** | (0.66, 0.89) |
| 3rd quintile (≥ USD $12900 to<$26900) | 0.89 | (0.76, 1.03) |
| 4th quintile (> USD $3500 to<$12900) | 0.90 | (0.78, 1.05) |
Mexican Health and Aging Study, 2001
Urban residence defined as>100, 000 residents
Based on 1990–1995 out-migration data (Durango, Guanajuato, Michoacan, Nayarit, Jalisco and Zacatecas)
Income and wealth data include net income and/or assets of the respondent and spouse or partner, if applicable. Income and wealth are provided in US dollars (US$1=10 pesos in 2000)
p<0.05,
p<0.01,
p<0.001
We additionally found no significant interaction effects between the measure of childhood household sanitation facilities and any of the additional life-course socio-economic status measures of education, occupation, income or wealth in the linear or logistic regression models (results not shown). That is, there were no differences in the association between having sanitation facilities as a child and past-week depressive symptoms by level of education attained, occupation or quintile of income or wealth. This runs counter to our hypothesis that the adverse effects of material deprivation in childhood on later-life depressive symptoms might be buffered or, conversely, exacerbated, by the socio-economic status achieved in mid-life. Finally, there were no significant differences in the association between the measure of household sanitation facilities and past-week depressive symptoms by respondents’ age, given non-significant interaction terms between the sanitation facilities measure and both continuous and categorical specifications of age.
Discussion
Overall, these results provide support for the hypothesis that childhood poverty, as measured by whether or not respondents had household sanitation facilities as a child, is significantly associated with past-week depressive symptoms for Mexican adults 50 years and older. In particular, the findings lend support for both the latent and pathway mechanisms hypothesized by the life-course perspective. The latent, lasting effect of childhood conditions is suggested by the persistence of a significant association between the indicator of household sanitation facilities as a child and past-week depressive symptoms later in life, even when controlling for measures of adult socio-economic status, health, and family circumstances. We observed this significant association in both linear and logistic regression models.
Although this significant association may be explained by other unobserved measures related to contemporary circumstances, the results are suggestive of the notion that adverse conditions during critical periods in early life may become ‘embedded’, with lasting consequences for health outcomes in middle-age and older adulthood despite intervening conditions over the life course (Hertzman and Boyce 2010). This finding of a significant direct association between childhood conditions and past-week depressive symptoms for middle-aged and older adults, consistent with the latent effects hypothesis, underscores the potential importance of childhood context in shaping adult health in Mexico, even as material conditions and epidemiological trends have shifted drastically during the lifetimes of MHAS respondents.
At the same time, we found support for an association between childhood household sanitation facilities and past-week depressive symptoms that is partially mediated by adult socio-economic status attainment. This finding is consistent with the hypothesis that early life conditions influence later-life health through pathway mechanisms, or through their influence on socio-economic status and health outcomes in young and mid-adulthood. A decomposition of the mediation effects confirms that educational achievement accounts for the majority of the mediated effect of the childhood poverty proxy measure on later-life depressive symptoms, underscoring the importance of earlier life socio-economic status attainment, including educational achievement, on later-life health.
We found no support for the conditional effects of childhood poverty and education on past-week depressive symptoms. The conditional effects hypothesis proposed that educational attainment might buffer the adverse effects of adverse childhood socio-economic and health context on depression outcomes in older adulthood. Alternatively, lower educational attainment may have exacerbated the effects of childhood circumstances given downward or stagnant socio-economic mobility. The lack of support for the conditional effects, indicated by a non-significant interaction term between the measure of household sanitation facilities as a child and educational attainment, instead suggests that material deprivation during childhood has a consistently adverse impact on depressive symptoms later on regardless of education, even though we find that education is related to fewer depressive symptoms independently. We additionally found non-significant interaction effects between childhood poverty and all other adult socio-economic status indicators, including current monthly income, household assets, and working in a domestic or agricultural occupation versus other lifetime occupations. These findings again point to the urgency of reducing exposure to material deprivation during childhood in particular, given the potential for effects on later-life mental health that may not be completely counter balanced by mid-life socio-economic attainment.
Limitations
Several limitations should be acknowledged as part of this analysis. First, this study was limited to cross-sectional analysis using only the baseline MHAS wave. The potential for concluding causal relationships between variables is consequently highly limited. Given the extensive time between early childhood and later-life, measures used in this analysis may be subject to recall bias, where respondents have difficulty recalling conditions before age 10. Currently, no data is available for Mexico analogous to longitudinal birth cohort studies elsewhere; such a study would allow for improved causal analysis from early childhood onward and limit problems of recall bias. However, Haas’ (2007) analysis of US surveys of older adults suggests that retrospective measures of childhood health appear to be reliable, given generally consistent reports of the same retrospective measures across two different study waves. In the same study, Haas (2007) found little evidence of ‘anchoring’, whereby retrospective reports of child health by older adults are influenced by current health status.
Another important consideration is that this analysis assumes social causation, that social factors such as early childhood economic conditions leads to depressive symptoms. However, it may be that the relationship between adult SES and depressive symptoms is reverse, whereby those with increased depressive symptoms have reduced socio-economic status due to more limited occupational opportunities or an inability to work, and a subsequent decline in financial assets (Krause 1999). The process of health selection may certainly be at work, although it is not clear that health selection would account entirely for the disparity in depressive symptoms by SES measures. For example, in a longitudinal study of British adults, Stansfeld et al. (2011) found support for both social causation and health selection hypotheses in the link between childhood socio-economic position and depressive or anxiety disorder in mid-life.
An additional concern is that the measure of household sanitation facilities, which we use to approximate childhood poverty, may be confounded by respondents’ urban or rural residence during childhood. If the measure of household sanitation facilities is conflated with rural childhood residence, then it may be that rural residence generally, rather than family-level conditions of material deprivation, are driving the direct and indirect association with later-life depressive symptoms. However, it is difficult to infer whether or not respondents were raised in rural areas in the absence of detailed data on their geographical location during childhood. Even those areas currently classified as “urban” were likely rural during respondents’ childhood in Mexico at the beginning of the 20th century. In sensitivity analyses, we tested an interaction effect between the measure of household sanitation facilities during childhood and current urban or rural residence on past-week depressive symptoms and found no significant differences by area of residence. We additionally report no apparent cohort effects in the relationship between household sanitation facilities during childhood and later-life depressive symptoms based on respondents’ age, even if the older cohorts were more likely to report having no household sanitation facilities before age 10.
Finally, we note a limitation with our outcome measure. The measure of past-week depressive symptoms, even when using a validated cut-off score, is not able to indicate major depressive disorder. Major depressive disorder is indicative of depression that is severe enough to interfere with work or other normal activities, and we are unable to assess this level of severity with the CES-D scale (Aguilar-Navarro et al. 2007). Given the lack of a severity criterion as part of the CES-D scale, a relatively large portion of the sample was categorized above our cut-off indicating clinically significant depression. Nevertheless, cases of ‘sub-clinical’ or ‘clinically significant’ depression might be important targets for community-level interventions that may help prevent the onset of major depressive disorder, particularly in developing country settings where clinical mental health services are limited (Reynolds III et al. 2012).
Conclusion
These findings suggest that adverse socio-economic and health-related conditions in childhood may negatively impact the mental health of older adults in Mexico. These results are relevant for two simultaneous concerns for public policy in Mexico. For one, the proportion of the elderly population in Mexico is rapidly increasing, as with the rest of Latin America (Wong and Palloni 2009). The current state of depressive symptoms among this growing older adult population appears to be both directly and indirectly affected by historical conditions of material deprivation combined with little investment in public health infrastructure that characterized the first half of the 20th century in Mexico. The effects of these conditions do not appear in this analysis to be ameliorated by divergent socio-economic patterns in adulthood, an important finding given the growing concerns related to mental health among older adults in Mexico (Wagner et al. 1999). The life-course experiences of these older adults should be further understood as they continue to expand in their share of the Mexican population in the context of limited institutional supports and family care networks weakened by declining fertility rates, high out-migration to the United States, and changing norms about family caregiving (Wong and Palloni 2009).
The second concern raised by these finding relates to the persistence of childhood poverty and deep economic inequality in Mexico despite national economic development. The issue of limited access to so-called “improved” sanitation facilities, which in part refers to sanitation facilities that are in family households rather than in collective or public settings, was particularly acute in rural Mexico through 1990, when only 32 % of the population had access to household sanitation facilities (UNICEF/WHO 2012). This is notable in particular given the lasting effects of these conditions of material deprivation during childhood on past-week depressive symptoms later in life.
However, there have been significant efforts to reduce childhood poverty in Mexico. The most prominent example is Oportunidades, Mexico’s cash-assistance program for families that incentivizes school attendance and preventative health care utilization (Lomelí 2008). In addition, educational spending in Mexico is on par with developed nations in terms of percentage of GDP (World Bank 2011). As a result, Mexicans have made huge gains in educational attainment; primary school attendance rivals that of the US and the UK, although disparities are still felt in low secondary and tertiary school enrollment (World Bank 2011). The question that remains is whether programs like Oportunidades will sufficiently address low standards of living for children in a country where economic development has led to widening income inequality—namely, the expanded wealth of the already rich and the continued push towards out-migration for the poor (Wong and Palloni 2009). Recent findings suggest that at a national level, income inequality is significantly associated with lower educational attainment regardless of spending on education (Siddiqi et al. 2012). The present analysis provides greater urgency to public policy efforts in Mexico that seek to improve childhood conditions and also address social determinants of mental health across the life-course given their relationship to health outcomes in middle-age and older adulthood.
Contributor Information
Jacqueline M. Torres, Email: jacquemtorres@gmail.com, Department of Community Health Sciences, UCLA Fielding School of Public Health, P.O. Box 951772, Los Angeles, CA 90095-1772, USA.
Rebeca Wong, University of Texas Medical Branch, Galveston, TX, USA.
References
- Aguilar-Navarro SM, Fuentes-Cantú A, Ávila-Funes JA, García-Mayo EJ. Validez y confiabilidad del cuestionario del ENASEM para la depresión en adultos mayores. Salud Pública de México. 2007;49(4):256–262. doi: 10.1590/s0036-36342007000400005. [DOI] [PubMed] [Google Scholar]
- Alvarado BE, Zunzunegui MV, Béland F, Sicotte M, Tellechea L. Social and gender inequalities in depressive symptoms among urban older adults of Latin America and the Caribbean. Journals of Gerontology Series b-Social Sciences. 2007;62B(4):S226–S237. doi: 10.1093/geronb/62.4.s226. [DOI] [PubMed] [Google Scholar]
- Barker DJP. The intrauterine origins of cardiovascular disease. Acta Paediatrica. 1993;82(s392):93–99. doi: 10.1111/j.1651-2227.1993.tb12938.x. [DOI] [PubMed] [Google Scholar]
- Beltrán-Sanchez H, Crimmins E, Teruel G, Thomas D. Links Between Childhood and Adult Social Circumstances and Obesity and Hypertension in the Mexican Population. Journal of Aging and Health. 2011;23(7):1141–1165. doi: 10.1177/0898264311422255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenzon S, Lara MA, Robles R, Medina-Mora ME. Depresión: Estado del Conocimiento y la Necesidad de Políticas Públicas y Planes de Acción en México. Salud Pública de México. 2013;55(1):74–80. doi: 10.1590/s0036-36342013000100011. [DOI] [PubMed] [Google Scholar]
- Bojorquez-Chapela I, Manrique-Espinoza B, Mejía-Arango S, Solis MMT-R, Salinas-Rodriguez A. Effect of Social Capital and Personal Autonomy on the Incidence of Depressive Symptoms in the Elderly: Evidence from a Longitidinal Study in Mexico. Aging & Mental Health. 2012;16(4):462–471. doi: 10.1080/13607863.2011.651432. [DOI] [PubMed] [Google Scholar]
- Elo IT, Preston SH. Effects of early-life condtions on adult mortality – a review. Population Index. 1992;58(2):186–212. [PubMed] [Google Scholar]
- Goodman LA. On the exact variance of products. Journal of the American Statistical Association. 1960;55(292):708–713. [Google Scholar]
- Guerra M, Ferri CP, Sosa AL, Salas A, Gaona C, Gonzales V, et al. Late-life depression in Peru, Mexico and Venezuela: the 10/66 population-based study. The British Journal of Psychiatry. 2009;195:510–515. doi: 10.1192/bjp.bp.109.064055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas SA. The long-term effects of poor childhood health: an assessment and application of retrospective reports. Demography. 2007;44(1):113–135. doi: 10.1353/dem.2007.0003. [DOI] [PubMed] [Google Scholar]
- Haas SA. Trajectories of functional health: the ‘long arm’ of childhood health and socioeconomic factors. Social Science & Medicine. 2008;66(4):849–861. doi: 10.1016/j.socscimed.2007.11.004. [DOI] [PubMed] [Google Scholar]
- Haas SA, Krueger PM, Rohlfsen L. Race/ethnic and nativity disparities in later life physical performance: the role of health and socioeconomic status over the life course. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2012;67B(2):238–248. doi: 10.1093/geronb/gbr155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertzman C, Boyce T. How experience gets under the skin to create gradients in developmental health. Annual Review of Public Health. 2010;31:329–347. doi: 10.1146/annurev.publhealth.012809.103538. [DOI] [PubMed] [Google Scholar]
- Hertzman C, Power C, Matthews S, Manor O. Using an interactive framework of society and lifecourse to explain self-rated health in early adulthood. Social Science & Medicine. 2001;53(12):1575–1585. doi: 10.1016/s0277-9536(00)00437-8. [DOI] [PubMed] [Google Scholar]
- Huang C, Soldo BJ, Elo IT. Do early-life conditions predict functional health status in adulthood? The case of Mexico. Social Science & Medicine. 2011;72(1):100–107. doi: 10.1016/j.socscimed.2010.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Archives of Internal Medicine. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Kohler IV, Soldo BJ. Childhood predictors of late-life diabetes: the case of Mexico. Social Biology. 2005;52(3–4):112–131. [PubMed] [Google Scholar]
- Kohler U, Karlson KB, Holm A. Comparing coefficients of nested nonlinear probability models. The Stata Journal. 2011;11:420–439. [Google Scholar]
- Krause N. Mental disorder in late life. In: Aneshensel CS, Phelan JC, editors. Handbook of the sociology of mental Health. New York: Springer; 1999. pp. 183–208. [Google Scholar]
- Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life course epidemiology. Journal of Epidemiology and Community Health. 2003;57(10):778–783. doi: 10.1136/jech.57.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lomelí EV. Conditional cash transfers as social policy in Latin America: an assessment of their contributions and limitations. Annual Review of Sociology. 2008;34:475–499. [Google Scholar]
- Luo Y, Waite L. The impact of childhood and adult SES on physical, mental and cognitive well-being in later-life. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2005;60B:S93–S101. doi: 10.1093/geronb/60.2.s93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey DS, Alarcon R, Durand J, González H. Return to Aztlan: the social processes of international migration from Western Mexico. Berkeley, CA: UC Press; 1990. [Google Scholar]
- Maurer J. Height, education and later-life cognition in Latin America and the Caribbean. Economics and Human Biology. 2010;8(2):168–176. doi: 10.1016/j.ehb.2010.05.013. Article. [DOI] [PubMed] [Google Scholar]
- Maurer J. Education and Male–female Differences in Later-Life Cognition: International Evidence From Latin America and the Caribbean. Demography. 2011;48(3):915–930. doi: 10.1007/s13524-011-0048-x. [DOI] [PubMed] [Google Scholar]
- Medina-Mora ME, Borges G, Benjet C, Lara C, Berglund P. Psychiatric Disorders in Mexico: Lifetime Prevalence in a Nationally Representative Sample. The British Journal of Psychiatry. 2007;190:521–528. doi: 10.1192/bjp.bp.106.025841. [DOI] [PubMed] [Google Scholar]
- Monteverde M, Noronha K, Palloni A. Effect of early conditions on disability among the elderly in Latin America and the Caribbean. Population Studies-a Journal of Demography. 2009;63(1):21–35. doi: 10.1080/00324720802621583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD. Disability-Adjusted Life Years (DALYs) for 291 Diseases and Injuries in 21 Regions, 1990–2010: A Systematic Analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- Nguyen C, Couture M, Alvarado B, Zunzunegui M. Life course socioeconomic disadvantage and cognitive function among the elderly population of seven capitals in Latin America and the Caribbean. Journal of Aging and Health. 2008;20(3):347–362. doi: 10.1177/0898264308315430. [DOI] [PubMed] [Google Scholar]
- O’Rand AM. The precious and the precocious: understanding cumulative disadvantage and cumulative advantage over the life course. Gerontologist. 1996;36(2):230–238. doi: 10.1093/geront/36.2.230. [DOI] [PubMed] [Google Scholar]
- Pearlin L, Schieman S, Fazio E, Meersman S. Stress, health, and the life course: some conceptual perspectives. Journal of Health and Social Behavior. 2005;46(2):205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Poulton R, Caspi A, Milne BJ, Thompson WM, Taylor A, Sears MR, et al. Association between children’s experience of socioeconomic disadvantage and adult health: a life-course study. Lancet. 2002;360(9346):1640–1645. doi: 10.1016/S0140-6736(02)11602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LC. The CES-D scale, a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Reynolds CF, III, Cuijpers P, Patel V, Cohen A, Dias A, Chowdhary N, et al. Early intervention to reduce the global health and economic burden of major depression in older adults. Annual Review of Public Health. 2012;33:123–135. doi: 10.1146/annurev-publhealth-031811-124544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross CE, Wu CL. The links between education and health. American Sociological Review. 1995;60(5):719–745. [Google Scholar]
- Sánchez-García S, Juárez-Cedillo T, García-González JJ, Espinel-Bermúdez C, Gallo JJ, Wagner FA, et al. Usefulness of two instruments in assessing depression among elderly Mexicans in population studies and for primary care. Salud Pública de México. 2008;50(6):447–456. doi: 10.1590/s0036-36342008000600005. [DOI] [PubMed] [Google Scholar]
- Siddiqi A, Kawachi I, Berkman LF, Hertzman C, Subramanian SV. Education determines a nation’s health, but what determines educational outcomes? A cross-national comparative analysis. Journal of Public Health Policy. 2012;33(1):1–15. doi: 10.1057/jphp.2011.52. [DOI] [PubMed] [Google Scholar]
- Smith KV, Goldman N. Socioeconomic differences in health among older adults in Mexico. Social Science & Medicine. 2007;65(7):1372–1385. doi: 10.1016/j.socscimed.2007.05.023. [DOI] [PubMed] [Google Scholar]
- Stansfeld SA, Clark C, Rodgers B, Caldwell T, Power C. Repeated exposure to socioeconomic disadvantage and health selection as life course pathways to mid-life depressive and anxiety disorders. Social Psychiatry and Psychiatric Epidemiology. 2011;46(7):549–558. doi: 10.1007/s00127-010-0221-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens G, Dias RH, Thomas KJA, Rivera JA, Carvalho N, Barquera S, et al. Characterizing the epidemiological transition in Mexico: National and subnational burden of diseases, injuries, and risk factors. PLoS Medicine. 2008;5(6):e125. doi: 10.1371/journal.pmed.0050125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF. A multidimensional approach to childhood poverty. New York: UNICEF; 2011. [Google Scholar]
- UNICEF/WHO. Progress on drinking water and sanitation: 2012 update. New York, NY: UNICEF; 2012. [Google Scholar]
- Wagner FA, Gallo JJ, Delva J. Depression in late life: a hidden public health problem for Mexico? Salud Pública de México. 1999;41(3):189–202. doi: 10.1590/s0036-36341999000300007. [DOI] [PubMed] [Google Scholar]
- Wong R, Espinoza M. Mexican Health and Aging Study (ENASEM), 2001: Methodological Document and Project Report, Version 2. 2004 Retrieved from: http://www.mhas.pop.upenn.edu/english/documents/Methodological/Doc_metodologico-v2.pdf.
- Wong R, Palloni A. Aging in Mexico and Latin America. In: Uhlenberg P, editor. International handbook of population aging. Springer Science; US: 2009. [Google Scholar]
- Wong R, Pelaez M, Palloni A, Markides K. Survey data for the study of aging in Latin America and the Caribbean - Selected studies. Journal of Aging and Health. 2006;18(2):157–179. doi: 10.1177/0898264305285655. [DOI] [PubMed] [Google Scholar]
- World Bank. Educational statistics database. 2011 from http://go.worldbank.org/85XM5TBQA0.


