Abstract
Background
Injuries with sharps are common occupational hazards for healthcare workers. Such injuries predispose the staff to dangerous infections such as hepatitis B, C and HIV.
Objectives
The present study was conducted to investigate the behaviors of healthcare workers in Kashan healthcare centers after needle sticks and injuries with sharps in 2012.
Materials and Methods
A cross-sectional study was conducted on 298 healthcare workers of medical centers governed by Kashan University of Medical Sciences. A questionnaire was used in this study. The first part included questions about demographic characteristics. The second part of the questionnaire consisted of 16 items related to the sharp instrument injuries. For data analysis, descriptive and analytical statistics (chi-square, ANOVA and Pearson correlation coefficient) SPSS version 16.0 software was used.
Results
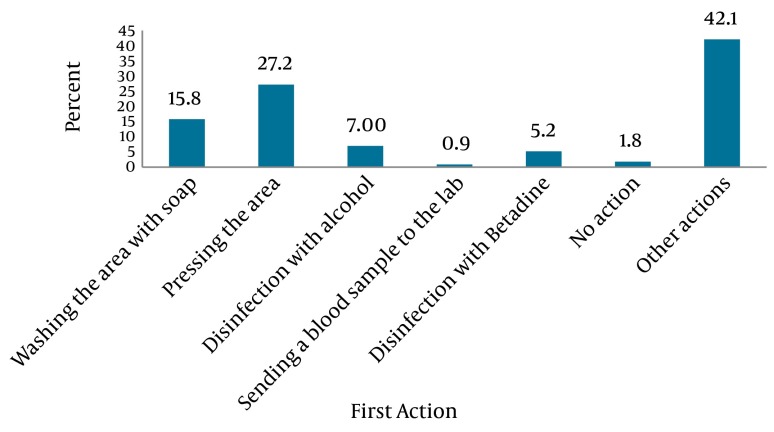
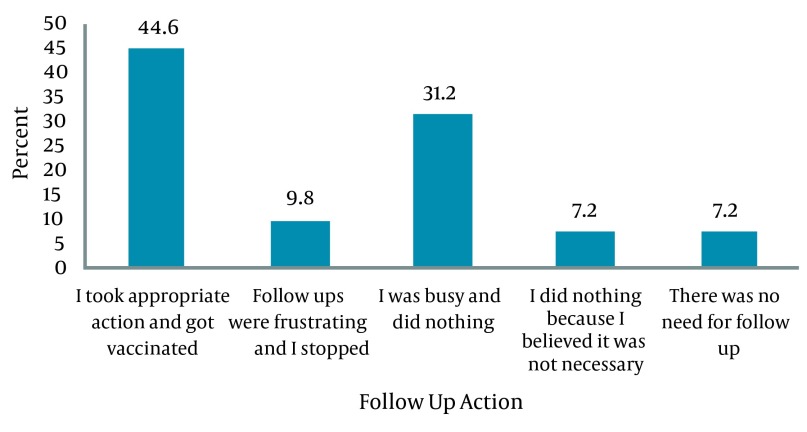
From a total of 298 healthcare workers, 114 (38.3%) had a history of injury from needles and sharp instruments in the last six months. Most needle stick and sharp instrument injuries had occurred among the operating room nurses and midwifes; 32.5% of injuries from sharp instruments occurred in the morning shift. Needles were responsible for 46.5% of injuries. The most common actions taken after needle stick injuries were compression (27.2%) and washing the area with soap and water (15.8%). Only 44.6% of the injured personnel pursued follow-up measures after a needle stick or sharp instrument injury.
Conclusions
More than a half of the healthcare workers with needle stick or sharp instrument injury had refused follow-up for various reasons. The authorities should implement education programs along with protocols to be implemented after needle stick injuries or sharps.
Keywords: Needle stick Injuries, Behaviors, Knowledge, Health Personnel
1. Background
Needle stick injury has been defined as a percutaneous piercing wound by a needle point or other sharp instrument contaminated with blood or body fluids (1). Needle stick injuries are of the most common occupational hazards healthcare workers are faced with (2, 3). These injuries usually occur during activities such as transfusion, blood sampling, needle disposal, waste collection, transferring body fluids and transferring blood from a syringe into another vessel (3). Injuries due to contact with contaminated needles may have serious physical and psychological consequences (4-6). These injuries may be dangerous and predispose healthcare workers to more than 20 different types of pathogens (7) including HIV and hepatitis B and C viruses (8-10). The risk of catching HIV through needle stick is 0.3%; while, such risk is 3% for hepatitis C, and 30% for hepatitis B (8). The risk of exposure is also increases with the increasing number of patients (11). According to the World Health Organization, 16,000 cases of hepatitis C, 66,000 cases of hepatitis B and 1,000 cases of AIDS have occurred through occupational exposure in the year 2000 (12). The costs of injuries related to sharp contaminated instruments in the US has been estimated to be around 118 to 591 million dollars in 2010 (4, 7-13). These injuries also induce considerable psychological aftermaths such as phobia, anxiety and stress in affected individuals (14, 15). It is difficult to provide accurate statistics on the incidence of needle stick or sharps injuries because even in developed countries all cases are not reported (16, 17). Several factors such as time constraint, underestimating the risk, and lack of knowledge may prevent injuries from being reported (18). The incidence of needle sticks among health-care workers varies in different countries. For instance, its prevalence has been reported to be about 66% in Egypt, 45% in Pakistan, 31.4 % in Germany, 46.8% in Saudi Arabia, 45% in Turkey, 50% in Australia and Taiwan and 79.5% in India (19-26). It seems that these injuries are more prevalent in developing countries. In a recent study, 57% of African nurses and midwives had experienced at least one needle stick injury in the past year. Only 18% had not experienced any such injury in their entire career and the rate of needle stick injury was 4.2 per person per year (27); however, the rates of such injuries are lower in healthcare workers of some developed countries (19, 20, 22, 24, 26). The most common causes of needle sticks in various studies were high workload, working hastily, fatigue and a crowded work environment. Also, the highest rates of needle sticks occur during activities such as blood sampling, injections, IV catheter insertion, disposal of contaminated needles, needle recapping and washing contaminated instruments (28, 29). Behaviors and actions of employees after a needle stick are of great importance in preventing the consequences. Healthcare workers should take appropriate actions after needle stick injuries. Also employers are responsible for implementing protocols to reduce such injuries (30). Despite the publication of the guidelines for prevention of sharp percutaneous injuries, such injuries continue to occur. Studies have also shown that compliance with these precautions is less than optimal worldwide (31). Baghcheghi et al., have studied the prevalence of needle sticks and sharps injuries among nursing students and reported that the most important measures taken after needle sticks were washing the area with soap and sending a blood sample to the lab; but in 10% of cases no specific action was taken (28). In another study, Rakhshani et al. studied the prevalence of needle stick injuries among the healthcare professionals in Zahedan hospitals and reported that compression, washing the injured area with povidone iodide and washing with soap were the most prevalent actions respectively. However, in 0.09% of cases nothing was done (29).
2. Objectives
Due to the lack of precise information on the rate of needle sticks and sharps injuries and related factors and the differences among previous studies, the present study was conducted to investigate the behaviors of healthcare workers in Kashan’s healthcare centers after needle sticks and sharps injuries.
3. Materials and Methods
This cross-sectional study was conducted in the last three months of 2012 on healthcare workers of medical centers affiliated with Kashan University of Medical Sciences. Sample size was calculated based on a previous report of the prevalence of needle sticks and sharps injuries which was 24.1% (32); Three hundred and sixty samples were selected considering a possible attrition rate of 25%. Stratified random sampling was performed. First, the number of staff at each center was assessed. Then, the quota for each center was calculated and selected randomly among the staff at each center. A two-part, researcher-made questionnaire was used. The first part included questions on demographic characteristics (i.e. age, gender, marital status, work experience, job, the highest qualification, working unit and the employment status). The second part of the questionnaire consisted of 16 items including: the knowledge related to sharps injuries, complications and actions needed to be taken after an injury occurred (4 items), the history of exposure to a sharp injury and its causes if occurred (7 items), and the actions they have taken after a sharp injury occurred (5 items). The participants were asked to fill-out the questionnaire and put it in a special box which was placed for this purpose at each center. The data was collected 24 hours later. To evaluate the reliability, the test-retest method was used. The correlation coefficient was 0.93.
3.1. Ethical Considerations
All participants in the study signed a written informed consent to participate and were assured about the confidentiality of their personal information. Ethical issues of the study were approved in the research ethics committee in the Faculty of Nursing and Midwifery, Kashan University of Medical Sciences. Also permission was obtained from the university authorities and hospitals.
3.2. Data Analysis
For data analysis, descriptive and analytical statistics (chi-square, ANOVA and Pearson’s correlation coefficient) SPSS 16.0 software was used.
4. Results
From a total of 360 questionnaires, 298 were fully answered and were used in analysis; 68.1% (203 subjects) were female. The age ranged from 20 to 54 years, and their mean age and mean working experience were 32.25 ± 7.06 and 8.10 ± 6.63 years, respectively. No significant differences were observed between the mean age and mean working experience of men and women. Also 38.3% of the subjects (n = 114) had a history of injury from needles and sharps in the last six months. In addition, 19.8% (n = 59) subjects were injured from sharp instruments for at-least 2 times during the last six months. The mean of sharp instrument injuries was 2.74±1.56 times in the last 6 months. Most needle sticks and sharp instrument injuries have occurred among the operative nurses and midwifes and 44.8% of this group had experienced such injuries in the past six months before the study (Table 1).
Table 1. Demographic Characteristics of the Participants and History of Needle Sticks and Sharps Injury in the Last Six Months.
| Variable | Total, No. (%) | History of Injury, No. (%) | P value |
|---|---|---|---|
| Gender | 0.46 | ||
| Female | 203 (68.1) | 81 (39.9) | |
| Male | 95 (31.9) | 33 (34.7) | |
| Marital status | 0.80 | ||
| Single | 63 (22.1) | 24 (38.1) | |
| Married | 235 (78.9) | 90 (38.3) | |
| Job | 0.77 | ||
| Nurse | 155 (52) | 60 (38.7) | |
| Lab staff | 34 (11.4) | 15 (44.1) | |
| Operating room nurse and midwife | 29 (9.7) | 13 (44.8) | |
| Nursing assistant | 80 (26.8) | 26 (32.5) | |
| Education level | 0.20 | ||
| Diploma & lower | 89 (29.9) | 26 (29.2) | |
| Associate degree | 14 (6) | 9 (50) | |
| Bachelor or higher | 191 (64.1) | 79 (41.4) | |
| Employment status | 0.35 | ||
| Permanent | 66 (22.1) | 29 (43.9) | |
| By contract | 232 (77.9) | 85 (36.6) |
No significant association was found between age and the history of needle stick; however, a significant correlation was observed between being exposed to needle stick and work experience. Those with more work experience had less frequent needle sticks in the past 6 months (P ≤ 0.05). In total, 32.5% of injuries from sharp instruments occurred in morning shifts. Also, 89.3% of reported that they have received hepatitis B vaccination. More than half of the participants reported that they have high levels of knowledge about the needle stick injury, its side effects and actions required when a sharp instrument injury occurs. However, no significant association was found between the level of knowledge and the history of needle stick injury (Table 2). Also, 78.7% of nurses evaluated their knowledge as high in this regard.
Table 2. The History of Sharp Injury in the Last Six Month and Knowledge about Needle Stick Injuries.
| History of Sharps Injury in the Last Six Month | Knowledge About Needle Stick Injuries, No. (%) | P value | ||
|---|---|---|---|---|
| High Knowledge | Low Knowledge | No Knowledge | ||
| Yes | 75 (65.8) | 30 (26.3) | 9 (7.9) | 0.80 |
| No | 111 (71.4) | 35 (22.7) | 9 (5.8) | |
Needles were responsible for 46.5% of injuries (Table 3). Also blood sampling from a restless patient and needle recapping were the most common situations in which injuries occurred (Table 3). Also, careless interventions (in 28.25% of cases) and crowded environment in the unit (in 20.34% of cases) were cited as the two common factors predisposing to injuries (Table 3).
Table 3. Frequency, Type of Instrument, Behavior Leading to Injury and Predisposing Factors.
| Variable | No. (%) |
|---|---|
| Type of instrument | |
| Needle | 53 (46.5) |
| Angiocatheter | 11 (9.6) |
| Lancet | 7 (6.1) |
| Surgical blade | 5 (4.4) |
| Suture needle | 4 (3.5) |
| Vials of drugs | 3 (2.6) |
| Others | 31 (27.2) |
| Behavior leading to injury | |
| Injection and taking a blood sample | 22 (22.2) |
| Needle recapping | 18 (18.2) |
| Inappropriate disposal of needles | 11 (11.1) |
| Preparing drugs | 7 (7.1) |
| Transporting sharps | 7 (7.1) |
| Others | 34 (34.3) |
| Predisposing factor for injury | |
| Imprudence of the subject | 25 (28.25) |
| Crowded ward | 18 (20.34) |
| Imprudence of colleagues | 10 (11.30) |
| Lack of facilities | 5 (5.65) |
| Fatigue | 2 (2.26) |
| Inappropriate education | 2 (2.26) |
| Drowsiness | 2 (2.26) |
| Putting needles in waste basket | 5 (5.65) |
The most common actions taken after needle stick injuries were compression (27.2%) and washing the area with soap (15.8%) respectively (Figure 1). Only 44.6% of the injured people took follow up actions after a needle stick or sharp instrument injury while no specific action was performed in 53.4% of cases (Figure 2). A significant association was found between the staff’s knowledge about sharp instrument injuries and the follow-up actions implemented after the occurrence of an injury (P = 0.01) (Table 4).
Figure 1. The First Action After the Injury.
Figure 2. Follow Up Action After the Injury.
Table 4. Frequency of Follow-Up Measures in Different Levels of Knowledge About Needle Stick Injuries.
| Type of Follow-Up Action After the Injury | Knowledge About Needle Stick Injuries, No. (%) | P value | ||
|---|---|---|---|---|
| High | Low | No | ||
| Yes | 40 (58.0) | 7 (25.9) | 3 (37.5) | 0.01 |
| No | 29 (42.0) | 20 (74.1) | 6 (62.5) | |
Overall, 9.6% of the staff who experienced a sharp instrument injury did not report the occurrence of the injury to the ward’s authorities; 38.6% reported the injury to the ward’s authorities and received some guidance; 24.6% of the wards authorities implemented special supportive and follow up actions. However, according to the participants, in 21.1% of cases the wards authorities were indifferent towards the staff’s injuries. Most participants (62.8%) stated that experiencing a needle stick or sharp instrument injury made them more cautious and careful.
5. Discussion
More than one third of the participants in this study had experienced injury to sharp instruments in the last six months. This rate was lower than that reported in other studies in Iran. The incidence of needle stick ranged from 47.05% to more than 76% in different studies previously conducted in Iran (33, 34). This rate ranged from 61% to 80% in studies conducted in Britain, Uganda and India (35, 36). Although the rate of sharp injuries in this study may be influenced by the response rate; however, the lower rate of injuries may also be attributed to the low rate of reporting (16, 17) and this may be an alarm for the need to establish a reliable reporting system for these injuries. Although the participants evaluated their level of knowledge about such injuries to be high; however, this self-rated evaluation may be inaccurate and their level of knowledge needs to be evaluated through more appropriate methods. Most operating room staff, midwives and lab staff had a history of needle stick or sharps injury in the last six months before the study. A previous study reported that such injuries are more prevalent among nurses (29). It seems that operating room staff, midwives and lab staff are at a higher risk. Hospital authorities should establish special education programs to decrease the risk in these high risk groups. Most of the participants in the present study had been vaccinated against HBV. This finding was consistent with previous studies in Hamadan Iran (37) and in Pakistan (38). Although the immunization rates in our study were acceptable, vaccination alone does not guarantee immunity against diseases. Therefore, it is necessary for high risk staff to be checked periodically for the levels of antibody of dangerous pathogens (28). In the present study, most sharp instrument injuries occurred in the morning shifts. However, no significant difference was found between working shift and occurrence of sharp instrument injury. This finding was consistent with the results of Ghasemi, who studied the frequency of needle stick injuries among healthcare workers of Ardebil hospitals (33). Also the same results were reported by Aghadoost et al., in Kashan (39), and some of the studies from other countries (40, 41). Nevertheless, Ayas et al., studied the risk of self-reported percutaneous injuries in interns and reported that most injuries occurred during the night shifts (42). In the current study, injecting and taking a blood sample from a restless patient and recapping the needles were the most dangerous interventions resulting in needle stick injury. This finding was consistent with several previous studies (17, 29, 37), but are inconsistent with Jayanth et al., (17). Also as reported in several studies (29, 42) the most common damaging instrument in the current study were needles and intravenous catheters. However using safe syringes, needles and intravenous catheters can significantly reduce the rate of needle stick injuries. Modern safety syringes, needles and intravenous catheters may decrease injury. In the present study, the most common causes of injury were imprudence and crowded ward environment. Several previous studies also reported that imprudence of the healthcare staff, high workload, and rushing were common predisposing factors for needle stick injuries among nurses and other healthcare workers. Also disposal of needles with other rubbish is an important risk factor for needle stick injury among the custodian and ward cleaners (29, 42-44). In the present study, the most common actions performed after a needle stick injury were applying pressure and washing the area with soap and water. These findings are consistent with the results of Rakhshani et al., and Baghcheghi et al. (28, 29). But, Hashemi et al., reported that most needle stick injured staff immediately referred to the hospital’s center for infection control to receive proper treatment (37). It seems that executing proper in-service education programs along with establishing protocols for implementing them following needle stick injuries may help healthcare workers receive proper treatment.
More than a half of the healthcare workers with needle stick or sharps injury refused follow-up for various reasons. Also, facilities for treatment and follow up was available in less than a quarter of the cases, The exact rate of injury may be underestimated.
Acknowledgments
The authors would like to thank the faculty of nursing and midwifery for their help in this study.
Footnotes
Implication for health policy/practice/research/medical education:
This study showed that more than half of the healthcare staff with sharp instrument injuries refused follow-up care. The authorities and policy makers should implement proper in-service education programs and protocols to help healthcare staff to take appropriate actions after a needle stick or injuries with sharps.
Authors’ Contribution:
Draft was performed by Mohsen Adib-Hajbaghery; Data analysis: Mohammad Sajjad Lotfi.
Financial Disclosure:
The authors declare that they have no competing interests.
Funding/Support:
None.
References
- 1.Rele M, Mathur M, Turbadkar D. Risk of needle stick injuries in health care workers - a report. Indian J Med Microbiol. 2002;20(4):206–7. [PubMed] [Google Scholar]
- 2.Gabriel J. Reducing needlestick and sharps injuries among healthcare workers. Nurs Stand. 2009;23(22):41–4. doi: 10.7748/ns2009.02.23.22.41.c6777. [DOI] [PubMed] [Google Scholar]
- 3.Norsayani MY, Noor Hassim I. Study on incidence of needle stick injury and factors associated with this problem among medical students. J Occup Health. 2003;45(3):172–8. doi: 10.1539/joh.45.172. [DOI] [PubMed] [Google Scholar]
- 4.Fisman DN, Mittleman MA, Sorock GS, Harris AD. Willingness to pay to avoid sharps-related injuries: a study in injured health care workers. Am J Infect Control. 2002;30(5):283–7. doi: 10.1067/mic.2002.124586. [DOI] [PubMed] [Google Scholar]
- 5.Lee JM, Botteman MF, Xanthakos N, Nicklasson L. Needlestick injuries in the United States. Epidemiologic, economic, and quality of life issues. AAOHN J. 2005;53(3):117–33. [PubMed] [Google Scholar]
- 6.Patel D, Gawthrop M, Snashall D, Madan I. Out of hours management of occupational exposures to blood and body fluids in healthcare staff. Occup Environ Med. 2002;59(6):415–8. doi: 10.1136/oem.59.6.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ertem M, Dalar Y, Cevik U, Sahin H. Injury or body fluid splash incidence rate during three months period in elective surgery procedures, at Dicle University Hospital, Diyarbakir, Turkey. Ulus Travma Acil Cerrahi Derg. 2008;14(1):40–5. [PubMed] [Google Scholar]
- 8.Health Protection Agency. Guidelines of United Kingdom surveillance of significant occupational exposures to blood borne viruses in healthcare workers. Eye of the Needle. 2008. [Google Scholar]
- 9.Pruss-Ustun A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005;48(6):482–90. doi: 10.1002/ajim.20230. [DOI] [PubMed] [Google Scholar]
- 10.Schmid K, Schwager C, Drexler H. Needlestick injuries and other occupational exposures to body fluids amongst employees and medical students of a German university: incidence and follow-up. J Hosp Infect. 2007;65(2):124–30. doi: 10.1016/j.jhin.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Michielsen PP, Francque SM, van Dongen JL. Viral hepatitis and hepatocellular carcinoma. World J Surg Oncol. 2005;3:27. doi: 10.1186/1477-7819-3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atenstaedt RL, Payne S, Roberts RJ, Russell IT, Russell D, Edwards RT. Needle-stick injuries in primary care in Wales. J Public Health (Oxf). 2007;29(4):434–40. doi: 10.1093/pubmed/fdm048. [DOI] [PubMed] [Google Scholar]
- 13.Leigh JP, Gillen M, Franks P, Sutherland S, Nguyen HH, Steenland K, et al. Costs of needlestick injuries and subsequent hepatitis and HIV infection. Curr Med Res Opin. 2007;23(9):2093–105. doi: 10.1185/030079907X219517. [DOI] [PubMed] [Google Scholar]
- 14.Lee J, Botteman M, Nicklasson L. A Systematic Review of the Economic and Humanistic Burden of Needlestick Injury in the United States. Am J Infect Control. 2004;32(3):E43. doi: 10.1016/j.ajic.2004.04.064. [DOI] [Google Scholar]
- 15.Smith DR, Choe MA, Jeong JS, Jeon MY, Chae YR, An GJ. Epidemiology of needlestick and sharps injuries among professional Korean nurses. J Prof Nurs. 2006;22(6):359–66. doi: 10.1016/j.profnurs.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Au E, Gossage JA, Bailey SR. The reporting of needlestick injuries sustained in theatre by surgeons: are we under-reporting? J Hosp Infect. 2008;70(1):66–70. doi: 10.1016/j.jhin.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 17.Jayanth ST, Kirupakaran H, Brahmadathan KN, Gnanaraj L, Kang G. Needle stick injuries in a tertiary care hospital. Indian J Med Microbiol. 2009;27(1):44–7. [PubMed] [Google Scholar]
- 18.Haiduven DJ, Simpkins SM, Phillips ES, Stevens DA. A survey of percutaneous/mucocutaneous injury reporting in a public teaching hospital. J Hosp Infect. 1999;41(2):151–4. doi: 10.1016/s0195-6701(99)90053-1. [DOI] [PubMed] [Google Scholar]
- 19.Abu-Gad HA, Al-Turki KA. Some epidemiological aspects of needle stick injuries among the hospital health care workers: Eastern Province, Saudi Arabia. Eur J Epidemiol. 2001;17(5):401–7. doi: 10.1023/a:1013793301772. [DOI] [PubMed] [Google Scholar]
- 20.Azap A, Ergonul O, Memikoglu KO, Yesilkaya A, Altunsoy A, Bozkurt GY, et al. Occupational exposure to blood and body fluids among health care workers in Ankara, Turkey. Am J Infect Control. 2005;33(1):48–52. doi: 10.1016/j.ajic.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Bi P, Tully PJ, Pearce S, Hiller JE. Occupational blood and body fluid exposure in an Australian teaching hospital. Epidemiol Infect. 2006;134(3):465–71. doi: 10.1017/S0950268805005212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ismail NA, Aboul Ftouh AM, El-Shoubary WH, Mahaba H. Safe injection practice among health-care workers in Gharbiya Governorate, Egypt. East Mediterr Health J. 2007;13(4):893–906. [PubMed] [Google Scholar]
- 23.Sharma R, Rasania S, Verma A, Singh S. Study of Prevalence and Response to Needle Stick Injuries among Health Care Workers in a Tertiary Care Hospital in Delhi, India. Indian J Community Med. 2010;35(1):74–7. doi: 10.4103/0970-0218.62565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wicker S, Jung J, Allwinn R, Gottschalk R, Rabenau HF. Prevalence and prevention of needlestick injuries among health care workers in a German university hospital. Int Arch Occup Environ Health. 2008;81(3):347–54. doi: 10.1007/s00420-007-0219-7. [DOI] [PubMed] [Google Scholar]
- 25.Yang YH, Wu MT, Ho CK, Chuang HY, Chen L, Yang CY, et al. Needlestick/sharps injuries among vocational school nursing students in southern Taiwan. Am J Infect Control. 2004;32(8):431–5. doi: 10.1016/S0196655304004523. [DOI] [PubMed] [Google Scholar]
- 26.Zafar A, Aslam N, Nasir N, Meraj R, Mehraj V. Knowledge, attitudes and practices of health care workers regarding needle stick injuries at a tertiary care hospital in Pakistan. J Pak Med Assoc. 2008;58(2):57–60. [PubMed] [Google Scholar]
- 27.Nsubuga FM, Jaakkola MS. Needle stick injuries among nurses in sub-Saharan Africa. Trop Med Int Health. 2005;10(8):773–81. doi: 10.1111/j.1365-3156.2005.01453.x. [DOI] [PubMed] [Google Scholar]
- 28.Baghcheghi N, Koohestani HR, Rezaei K, Seraji A, Abedi AR. Prevalence needlestick/sharps injuries among nursing student and related factor. Iran Occup Health J. 2011;7(4):32–9. [Google Scholar]
- 29.Rakhshani F, Heydari MT, Barati Bani S. Prevalence of needlestick injuries among the healthcare professionals in Zahedan medical Sciences university. Iran J Epidem. 2008;4(3-4):87–91. [Google Scholar]
- 30.Yang L, Mullan B. Reducing needle stick injuries in healthcare occupations: an integrative review of the literature. ISRN Nurs. 2011;2011:315432. doi: 10.5402/2011/315432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beltrami EM, Williams IT, Shapiro CN, Chamberland ME. Risk and management of blood-borne infections in health care workers. Clin Microbiol Rev. 2000;13(3):385–407. doi: 10.1128/cmr.13.3.385-407.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bakaeen F, Awad S, Albo D, Bellows CF, Huh J, Kistner C, et al. Epidemiology of exposure to blood borne pathogens on a surgical service. Am J Surg. 2006;192(5):e18–21. doi: 10.1016/j.amjsurg.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 33.Ghasemi A, Etemad E, Pourmohammadjan N, Rashiri J, Habibzadeh SH. Needle stick injuries among health care workers of ardebil university of medical science. Iran J Infect Dis Trop Med. 2009;27:32–4. [Google Scholar]
- 34.Nasiri E, Mortazavi Y, Siamian H, Shabankhani B. The prevalence and study of the rate of needlestick injuries infected by blood in staff of special departments of teaching and non teaching hospital of Mazandaran province in 2003-2004. Iran J Infect Dis Trop Med. 2005;10:41–4. [Google Scholar]
- 35.Muralidhar S, Singh PK, Jain RK, Malhotra M, Bala M. Needle stick injuries among health care workers in a tertiary care hospital of India. Indian J Med Res. 2010;131:405–10. [PubMed] [Google Scholar]
- 36.Ziraba AK, Bwogi J, Namale A, Wainaina CW, Mayanja-Kizza H. Sero-prevalence and risk factors for hepatitis B virus infection among health care workers in a tertiary hospital in Uganda. BMC Infect Dis. 2010;10:191. doi: 10.1186/1471-2334-10-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hashemi SH, Torabian S, Mamani M. Moazen Dehkordi Sh. The Prevalence of Needlestick and Sharps Injuries among Health Care Workers in Hamadan, Iran. Hamadan Univ Med Sci. 2012;18(4):41–6. [Google Scholar]
- 38.Siddique K, Mirza S, Tauqir SF, Anwar I, Zafar Malik A. Knowledge attitude and practices regarding Needle stick injuries amongst health care providers. Pak J Surg. 2008;24(4):243–8. [Google Scholar]
- 39.Aghadoost D, Hajijafari M, Tabatabaei B, hossein Ziloochi M, Dalirian A. Occupational exposure to blood in the stuff of educational-medical centers of Kashan University of Medical Sciences in 2005. Feyz J Kashan Univ Med Sci. 2007;10(4):59–64. [Google Scholar]
- 40.Habib H, Khan EA, Aziz A. Prevalence and Factors Associated with Needle Stick Injuries among Registered Nurses in Public Sector Tertiary Care Hospitals of Pakistan. Int J Coll Res Int Med Public Health. 2011;3(2):124–30. [Google Scholar]
- 41.Mbaisi EM, Ng'ang'a Z, Wanzala P, Omolo J. Prevalence and factors associated with percutaneous injuries and splash exposures among health-care workers in a provincial hospital, Kenya, 2010. Pan Afr Med J. 2013;14:10. doi: 10.11604/pamj.2013.14.10.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ayas NT, Barger LK, Cade BE, Hashimoto DM, Rosner B, Cronin JW, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006;296(9):1055–62. doi: 10.1001/jama.296.9.1055. [DOI] [PubMed] [Google Scholar]
- 43.Parks DK, Yetman RJ, McNeese MC, Burau K, Smolensky MH. Day-night pattern in accidental exposures to blood-borne pathogens among medical students and residents. Chronobiol Int. 2000;17(1):61–70. doi: 10.1081/cbi-100101032. [DOI] [PubMed] [Google Scholar]
- 44.Stewardson DA, Palenik CJ, McHugh ES, Burke FJ. Occupational exposures occurring in students in a UK dental school. Eur J Dent Educ. 2002;6(3):104–13. doi: 10.1034/j.1600-0579.2002.00253.x. [DOI] [PubMed] [Google Scholar]