Abstract
Background & objectives
There is poor knowledge and behaviors regarding chronic diseases related nutritional and lifestyle factors among women in low income countries. To evaluate efficacy of a multilevel population-based intervention in improving knowledge and practices for related factors we performed a study in India.
Methods
Population based study among women 35–70 years was performed in four urban and five rural locations. Stratified sampling was performed and we enrolled 4624 (rural 2616, urban 2008) of eligible 8000 women (58%). Demographic details, medical history, diet, physical activity and anthropometry were recorded and blood hemoglobin, glucose and total cholesterol determined. Knowledge and behaviors regarding diet in chronic diseases were inquired in a randomly selected 100 women at each site (n = 900). A systematic multilevel population based intervention (using posters, handouts, street plays, public lectures, group lectures and focused group discussions) was administered over 6 months at each site. The questionnaire was re-administered at the end in random 100 women (n = 900) and differences determined. Descriptive statistics are reported. Comparison of parameters before and after intervention was assessed using Mann Whitney test.
Results
Prevalence (%) of chronic disease related lifestyles and risk factors in rural/urban women, respectively, was illiteracy in 63.6/29.4, smoking/tobacco use 39.3/18.9, high fat intake 93.6/93.4, high salt intake 18.2/12.6, low physical activity 59.5/70.2, overweight/obesity 22.5/45.6, truncal obesity 13.0/44.3, hypertension 31.6/48.2, hypercholesterolemia 13.5/27.7, and diabetes in 4.3/15.1 percent. Composite chronic diseases knowledge at baseline vs after intervention increased significantly in overall (32.0 vs 62.0), rural (29.0 vs 63.5) and urban (39.5 vs 60.5) groups (p < 0.001). Significant increase in knowledge regarding diet in hypertension, diabetes, heart disease and anemia as well as importance of dietary proteins, fats, fibres and fruits was observed (p < 0.001). There was insignificant change in most of the practices regarding intake of low fat, high protein, high fibre diet except sieving the flour which declined significantly (80.1 vs 53.6, p < 0.001).
Conclusions
A short-term multilevel population-wide intervention among women in rural and urban locations in India increased chronic disease knowledge but failed to influence practices.
Keywords: Noncommunicable diseases, Cardiovascular disease, Dietary intervention, Lifestyle intervention, Hypertension
1. Introduction
Chronic non-communicable diseases are major cause of morbidity and mortality worldwide including in low and low-middle income countries.1 Chronic diseases such as cardiovascular diseases, cancers, chronic obstructive respiratory disease and diabetes are widely prevalent in these countries.1–3 World Health Organization (WHO) has defined that four lifestyle risk factors – smoking and tobacco use, sedentary lifestyle, poor diet and alcohol abuse are important precursors of all these conditions.4 These risk factors can be prevented by lifestyle changes and risk factor control.4
Two preventive strategies are useful in practice – population based intervention and high risk individual based intervention.5 Population based prevention strategies for chronic diseases have mainly focused on cardiovascular diseases and their risk factors. Multiple studies have been performed over the years.6–11 Reviews have reported variable outcomes of these interventions. Most of the interventions improved knowledge, some improved practices, while almost all failed to influence risk factors or disease outcomes, especially cardiovascular disease outcomes.12,13 Almost all the studies that have been reviewed in the past have emerged from high and high-middle income countries. In these countries, the level of general literacy as well as health literacy are high and it is likely that interventions have not influenced lifestyles and risk factors due to changes in social determinants of health.13 These social and economic changes are important drivers of change in lifestyles and risk factors.14
Health related poor lifestyles are widely prevalent in low and low-middle income countries such as India.1,15,16 Prevalence of smoking and tobacco use is high, intake of dietary saturated fats, trans-fats and salt are high while fruits and vegetables intake low. There have not been significant population wide efforts to influence abnormal lifestyles. Only a small number of studies are available from low and low-middle income countries.17 Studies among urban populations in Iran, Pakistan and a small study in India reported increased awareness of cardiovascular diseases risk factors.18–20 These studies did not focus on multiple chronic diseases risk factors, which are more likely to influence practices and be of long-term benefit, neither the efficacy of population-wide intervention using a multilevel approach used. We performed a nationwide study in urban and rural women in India to assess influence of a structured multilevel population wide intervention on knowledge and dietary behaviors related to widely prevalent chronic diseases such as cardiovascular diseases, obesity, diabetes, chronic obstructive lung disease and anemia. Interventions among women are important21 as better knowledge of dietary factors involved in chronic diseases can lead to transformational influence on diet and other lifestyle behaviors and can have direct impact on these diseases in the society22 and also be economically justifiable.23
2. Methods
A multisite study was initiated by investigators from different regions of the country and funding obtained from Science and Society Division, Department of Science and Technology, Government of India, New Delhi. A central institutional review board approved the study and ethical clearance was obtained from each study site. Sites participating in the study included institutions in northern (Haryana), central (Jaipur), western (Pune), eastern (Kolkata), and southern (Kochi, Gandhigram) India. Study was performed at four urban and five rural locations in the years 2004–2007. Details of the study methodology have been published earlier.24,25
In brief, a proforma was prepared which obtained information regarding social, demographic, diet, physical activity, anthropometric and biochemical variables. This questionnaire has been used in previous epidemiological studies in women in urban slums in Delhi and has been validated for diet, physical activity and other assessments.26 Investigators from each site were centrally trained to ensure uniformity in sampling methodology, questionnaire administration, physical examination and measurements, and biochemical estimations. Written informed consent was obtained from each participant. Sampling involved a systematic stratified strategy at each study site. To ensure uniformity in data collection each site was instructed to identify low and low-middle social status locations in the urban and rural areas. Urban locations were in Jaipur (central), Kolkata (east), Kochi and Pondicherry (south) and rural locations were in Haryana (north), Jaipur (central), Pune (west), Pondicherry (south), and Gandhigram (south). Low middle socioeconomic status locations were identified at each study site. The population at each study location varied from 20 to 30,000 adults and, therefore, the total population at all eight sites was 180,000 to 250,000 adults. At the study site a central point was identified and the study investigators moved house-to-house in a clockwise direction from there till the sampling target (n = 500 at each location) was completed. We evaluated middle-aged women 35–70 years at all locations. This strategy has been used in previous studies and recommended by the WHO.27 The response rate at each site varied from 50 to 70% and was similar in rural and urban locations.
The baseline questionnaire was designed to collect information on demographic data, family income, educational level, history of chronic illnesses such as coronary heart disease, hypertension, diabetes or high cholesterol, and smoking or tobacco intake. Dietary history was inquired using 2-day 24 hour recalls. A set of standardized cups, glasses and spoons were used to assess the intake of each food item. Food intake data was converted into raw ingredients and its nutritive was calculated using food composition tables in self designed computer software.26 Physical activity was inquired using a previously validated instrument that provides details of all the day long activity.28 In Indian women, the prevalence of leisure time physical activity is low but household chores and work-related physical activity could be substantial. This questionnaire captures all these physical activity domains and is more useful for low-income countries such as India. Physical examination was performed to assess height, weight, waist and hip size, mid-upper arm circumference (MUAC), calf circumference, and blood pressure using techniques recommended by the WHO.29 All the study investigators were centrally trained in measurement techniques for uniformity. Standardised tape-measures and weighing machines that were periodically calibrated were used. Body mass index (BMI) was calculated as weight (kg) divided by squared height (m). Waist-to-hip ratio (WHR) was calculated. Sitting blood pressure was measured using a calibrated digital sphygmomanometer supplied centrally (Omron model SDX, Healthcare Omron Inc, Illinois 60015, USA). Fasting blood sample was obtained in all the study participants. Glucose was determined at the site-based central laboratory using glucose peroxidase method and external quality control and periodical validation from the central laboratory at New Delhi. Blood levels of hemoglobin, fasting glucose and total cholesterol were measured using heme oxidase, glucose oxidase peroxidise and cholesterol oxidase-phenol 4-aminophenazone peroxidase methods, respectively, with quality control.26
The diagnostic criteria have been reported earlier.24,25 Educational status was classified according to number of years of formal education into four categories: illiterate, 1–5, 6–10 and >10 years of formal education. Women who smoked tobacco as bidis or cigarettes or used tobacco in non-smoked form were classified as smokers/tobacco use. Former tobacco users were also identified. Physical activity levels (PALs) were calculated for each woman and PAL <1.4 units taken as sedentary activity as defined in an Indian study.28 Overweight and obesity defined as body mass index (BMI) ≥25 kg/m2. Truncal obesity was defined by waist:hip ratio of >0.9 for stage II and >0.8 for stage I and waist circumference >90 cm for stage II and >80 cm for stage I.24 Hypertension was diagnosed when the systolic or diastolic BP was ≥140 and/or ≥90 mm Hg on multiple single day measurements or the subject was known hypertensive on medications.25 Hypercholesterolemia was defined by the presence of high total cholesterol (≥200 mg/dl). Diabetes was diagnosed in women with previously diagnosed diabetes or fasting blood glucose ≥126 mg/dl.24
2.1. Intervention
One hundred women at each study location were randomly selected after the initial screening for chronic diseases knowledge, awareness and practices as well as dietary knowledge and behaviors. A total of 900 were evaluated at different study sites before the start of intervention. This questionnaire focussed on health issues among middle-aged women, mainly non-communicable diseases such as cardiovascular disease and their risk factors obesity, hypertension, diabetes and cholesterol; chronic lung disease, osteoarthritis and anemia. Individual study workers were trained by the central team in questionnaire delivery to achieve uniformity.
For multilevel intervention a planned strategy was implemented. We used a population-wide intervention using posters, leaflets and handouts that were designed specifically for the study. These posters were in local languages at every study site and were context specific developed at each of the sites after assessment of abnormal lifestyles and risk factors. For local population we organized street plays focussing on problem of chronic diseases and ways and means to stop tobacco and alcohol use, improve diet and physical activity (Annexure 2, video attachment). Public lectures were organized in the locality of intervention. Population-group based intervention included small group lectures and focussed group discussions. The total duration of intervention was six months.
2.2. Statistical analyses
All the case report forms were transferred to the study management office in Delhi. The data were entered in a customised database using SPSS program (SPSS Inc, Chicago, USA). In a random 10% double entry was made to check for errors. All the analyses have been performed using SPSS version 10.0. All analyses have been performed after age-adjustment within the SPSS statistical package using ANCOVA. The prevalence rates for risk factors are reported as percentage. Age-adjustment was performed using the direct method and 2001 Indian census female population was used as standard. Descriptive statistics are reported for knowledge, attitudes, practices and behaviors questions. Comparison of variables before and after intervention was performed by the non-parametric Mann–Whitney test and U-values were calculated. p values < 0.05 were considered significant.
3. Results
A total of 4624 women aged 35–70 years were evaluated at different sites, more from rural areas (n = 2616) than urban (n = 2008) of the targeted 8000 (response 57.8%). The age-adjusted prevalence of various sociodemographic, dietary, anthropometric and biochemical variables in urban and rural women and the overall population are shown in Table 1. There was a high prevalence (%) of chronic disease and cardiovascular diseases related risk factors in both rural and urban women. Prevalence of risk factors in overall, rural and urban women were: illiteracy in 48.7% (rural 63.6%, urban 29.4%); smoking/tobacco use in 30.4% (rural 39.3%, urban 18.9%); high fat intake >30% energy/day in 93.6% (rural 93.6%, urban 93.4%); high salt intake >2500 mg sodium/day in 15.8%, (rural 18.2%, urban 12.6%); low physical activity <1.4 PALs/day in 63.2% (rural 59.5%, urban 70.2%); overweight or obesity BMI ≥25 kg/m2 in 33.2% (rural 22.5%, urban 45.6%); truncal obesity in 26.8% (rural 13.0%, urban 44.3%); hypertension in 38.9% (rural 31.6%, urban 48.2%); hypercholesterolemia in 20.0% (rural 13.5%, urban 27.7%); and diabetes in 9.3% (rural 4.3%, urban 15.1%).
Table 1.
Demographic and clinical characteristics of study subjects and prevalence of chronic disease risk factors.
| Variables | Urban (n = 2005) | Rural (n = 2613) | Total (n = 4618) |
|---|---|---|---|
| Age groups | |||
| 35–39 | 476 (23.7) | 777 (29.7) | 1253 (27.1) |
| 40–49 | 704 (35.1) | 820 (31.4) | 1524 (33.0) |
| 50–59 | 478 (23.8) | 608 (23.3) | 1086 (23.5) |
| 60–69 | 233 (11.6) | 328 (12.6) | 561 (12.1) |
| ≥70 | 114 (5.7) | 80 (3.1) | 194 (4.2) |
| Educational status | |||
| Illiterate | 590 (29.4) | 1662 (63.6) | 2250 (48.7) |
| 1–5 years | 415 (20.7) | 468 (17.9) | 883 (19.1) |
| 6–10 years | 674 (33.6) | 410 (15.7) | 1084 (23.5) |
| >10 years | 326 (16.3) | 74 (2.8) | 400 (8.7) |
| Smoking/tobacco use (n = 3937) | |||
| Current users | 326 (19.6) | 1197 (31.7) | 871 (41.6) |
| Smoking | 14 (0.7) | 290 (6.3) | 276 (10.6) |
| Non-smoked tobacco use | 325 (16.2) | 932 (20.2) | 607 (23.2) |
| Former users (stopped > 6 months) | 17 9 (1.07) | 57 (1.7) | 40 (2.14) |
| Fat intake | |||
| >30 en% | 1876 (93.4) | 2447 (93.6) | 4323 (93.6) |
| Desirable < 30 en% | 132 (6.6) | 166 (6.4) | 298 (6.4) |
| Sodium intake | |||
| <2500 mg/day | 1754 (87.4) | 2137 (81.8) | 3891 (84.2) |
| >2500 mg/day | 254 (12.6) | 476 (18.2) | 730 (15.8) |
| Total fibre intake | |||
| Low < 25 g/day | 674 (33.6) | 1688 (64.6) | 2362 (51.1) |
| Desirable > 25 g/day | 1334 (66.4) | 925 (35.4) | 2259 (48.9) |
| Regular physical activity | |||
| Low < 1.4 PAL/day | 1387 (70.1) | 1535 (59.5) | 2922 (63.2) |
| Moderate 1.4–1.6 PAL/day | 337 (17.0) | 495 (19.2) | 832 (18.2) |
| High > 1.6 PAL/day | 256 (12.9) | 549 (21.3) | 805 (17.7) |
| Sedentary lifestyle (n = 4604) Physical activity levels < 1.55 PALs |
1406 (71.0) | 2964 (65.0) | 1558 (60.1) |
| Overweight/obesity (n = 4601) | |||
| BMI < 23.0 kg/m2 | 715 (36.8) | 2385 (52.7) | 1670 (64.9) |
| BMI 23.0–24.9 kg/m2 | 355 (11.6) | 679 (14.8) | 324 (12.5) |
| BMI 25.0–29.9 kg/m2 | 640 (31.7) | 1091 (23.3) | 451 (16.8) |
| BMI ≥ 30.0 kg/m2 | 288 (13.9) | 440 (9.6) | 152 (5.7) |
| Truncal obesity (n = 4611) | |||
| WHR > 0.8 | 1812 (90.7) | 3359 (73.6) | 1547 (60.4) |
| WHR > 0.9 | 880 (44.3) | 1198 (26.8) | 318 (13.03) |
| Waist circumference > 80 cm (n = 4614) | 1274 (63.3) | 1999 (43.4) | 725 (28.3) |
| Waist circumference > 90 cm | 638 (31.4) | 864 (18.5) | 226 (8.4) |
| Hypertension | 925 (48.2) | 1671 (38.9) | 746 (31.6) |
| Hypercholesterolemia (n = 4435) | |||
| Cholesterol < 150 mg/dl | 359 (18.3) | 1198 (27.1) | 839 (34.4) |
| 150–199.9 mg/dl | 1088 (54.0) | 2363 (52.9) | 1275 (52.1) |
| ≥200 mg/dl | 552 (27.7) | 874 (20.0) | 322 (13.5) |
| Impaired fasting glycemia (n = 4438) | |||
| <100 gm/dl | 1418 (70.4) | 3556 (68.8) | 2138 (87.9) |
| 100–125 gm/dl | 404 (20.3) | 647 (13.6) | 243 (10.1) |
| ≥126 gm/dl | 181 (9.3) | 235 (6.9) | 54 (2.2) |
| Diabetes (fasting glucose ≥ 126 gm/dl or history) (n = 4408) | 292 (15.1) | 390 (9.3) | 98 (4.3) |
| Anemia < 12 gm/dl (n = 4429) | 702 (35.7) | 2551 (58.2) | 1849 (76.8) |
Knowledge of risk factors of chronic diseases, viz., tobacco use, physical inactivity, alcohol abuse as well as types of chronic diseases viz. obesity, hypertension, diabetes, cholesterol, heart disease and stroke, before and after the 6-month intervention period are shown in Table 2. Individual and composite chronic disease knowledge scores at baseline and after the intervention period are shown. Knowledge and awareness increased in both rural and urban women. There was a significant increase in median and inter-quartile (IQR) intervals scores in overall, rural as well as urban women. The composite knowledge score in the overall group increased from 32.0 (IQR 19.0–54.0) to 62.0 (IQR 46.0–79.0) (U = 21.30, p < 0.001). In rural women it increased from 29.0 (IQR 20.0–46.0) to 63.5 (IQR 48.0–81.7) (=20.31, p < 0.001) and in urban women it increased from 39.5 (IQR 18.0–64.0) to 60.5 (IQR 43.0–76.0) (U = 9.16, p < 0.001). The increase was more in rural as compared to urban women (Fig. 1).
Table 2.
Composite scores for chronic disease risk factors knowledge and attitudes in study women at baseline and 6-month follow-up (median and interquartile range, IQR).
| Variables | Urban |
Rural |
Total |
|||
|---|---|---|---|---|---|---|
| Baseline (n = 400) | Follow-up (n = 400) | Baseline (n = 500) | Follow-up (n = 500) | Baseline (n = 900) | Follow-up (n = 900) | |
| Tobacco use | 3.0 (1.0–4.0) | 3.0 (3.0–4.0) | 2.0 (1.0–3.0) | 3.0 (3.0–4.0) | 2.0 (1.0–3.0) | 3.0 (3.0–4.0) |
| Physical activity | 3.0 (3.0–5.0) | 4.0 (3.0–6.0) | 3.0 (2.0–5.0) | 5.0 (4.0–6.0) | 3.0 (2.0–5.0) | 5.0 (4.0–6.0) |
| Anaemia | 2.0 (0.0–5.0) | 4.0 (3.0–5.0) | 2.0 (0.0–3.0) | 5.0 (3.25–6.0) | 2.0 (0.0–4.0) | 5.0 (3.0–6.0) |
| Obesity | 7.0 (7.0–11.0) | 9.0 (6.0–12.0) | 7.0 (5.0–10.0) | 12.0 (10.0–13.0) | 7.0 (5.0–10.0) | 11.0 (8.0–13.0) |
| Hypertension | 5.0 (0.0–9.0) | 9.0 (5.0–11.0) | 3.0 (0.0–7.0) | 9 (5.0–12.0) | 4.0 (0.0–8.0) | 9.0 (5.0–12.0) |
| Diabetes | 7.0 (1.0–15.0) | 13.0 (5.0–18.0) | 2.0 (1.0–8.0) | 12.0 (7.0–18.0) | 3.0 (1.0–12.0) | 12.0 (6.0–18.0) |
| Cholesterol and lipids | 4.0 (2.0–5.0) | 5.0 (4.0–6.0) | 4.0 (4.0–5.0) | 6.0 (5.0–6.0) | 4.0 (3.0–5.0) | 6.0 (4.0–6.0) |
| Heart disease | 7.5 (2.0–13.75) | 12.0 (8.0–15.0) | 5.0 (2.0–8.0) | 13.0 (9.0–16.0) | 6.0 (2.0–11.0) | 13.0 (9.0–16.0) |
| Stroke | 0.0 (0.0–3.0) | 2.0 (0.0–4.0) | 0.0 (0.0–0.0) | 2.0 (0.0–5.0) | 0.0 (0.0–2.0) | 2.0 (0.0–4.0) |
| Total score | 39.5 (18.0–64.0) | 60.5 (43.0–76.0) | 29.0 (20.0–46.0) | 63.5 (48.0–81.75) | 32.0 (19.0–54.0) | 62 (46.0–79.0) |
| Inter-group comparisons (Mann Whitney U-test, p value) | 9.158 (<0.001) | 20.314 (<0.001) | 21.299 (<0.001) | |||
Fig. 1.
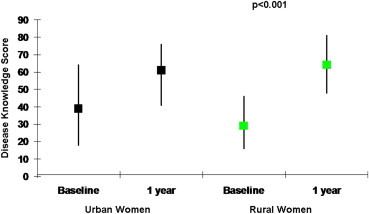
Change in composite scores for chronic disease and risk factors knowledge in study women (overall, urban and rural) at baseline and 6-month follow-up (median and interquartile range).
We evaluated changes in dietary knowledge as well as behaviours related to chronic diseases (Tables 3 and 4). Significant increase in knowledge regarding diet in hypertension, diabetes, heart disease and anemia as well as knowledge of importance of dietary proteins, fats, fibres and fruits was observed (Table 3, p < 0.001). Dietary behaviors and practices before and after the intervention are shown in Table 4. There was significant decline in practice of sieving the flour and in intake of milk, curds and butter milk and increase in intake of gram. There were no significant changes in practices regarding intake of low fat, high protein or high fibre diet.
Table 3.
Comparison of chronic disease related dietary knowledge at baseline and 6-month follow-up (number, %).
| Variables | Urban |
Intergroup comparison |
Rural |
Intergroup comparison |
Total |
Intergroup comparison |
|||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (n = 400) | Follow-up (n = 400) | Mann–Whitney U test (p value) | Baseline (n = 500) | Follow-up (n = 500) | Mann–Whitney U test (p value) | Baseline (n = 900) | Follow-up (n = 900) | Mann–Whitney U test (p value) | |
| Importance of diet in disease | |||||||||
| Hypertension | 250 (62.7) | 317 (79.2) | −5.284 (0.000) | 235 (47.0) | 432 (86.4) | −13.819 (0.000) | 485 (53.9) | 749 (83.2) | −13.872 (0.000) |
| Diabetes | 240 (60.0) | 315 (78.8) | −6.004 (0.000) | 213 (42.6) | 429 (85.8) | −15.598 (0.000) | 453 (50.3) | 744 (82.7) | −15.665 (0.000) |
| Heart disease | 224 (56.0) | 300 (75.0) | −6.021 (0.000) | 202 (40.4) | 455 (91.0) | −17.290 (0.000) | 426 (47.3) | 755 (83.9) | −16.963 (0.000) |
| Anaemia | 209 (52.2) | 231 (57.8) | −3.401 (0.001) | 197 (39.4) | 351 (70.2) | −11.696 (0.000) | 406 (45.1) | 582 (64.7) | −11.132 (0.000) |
| Dietary protein | |||||||||
| Sprouts are good | 221 (55.4) | 249 (62.6) | −2.781 (0.005) | 190 (38.0) | 386 (77.4) | −11.421 (0.000) | 411 (45.7) | 635 (70.8) | −10.513 (0.000) |
| Soya bean is good | 211 (52.8) | 270 (67.7) | −5.112 (0.000) | 115 (23.0) | 362 (72.5) | −14.915 (0.000) | 326 (36.2) | 632 (70.4) | −14.716 (0.000) |
| Dietary fats | |||||||||
| Type of fat is important | 123 (30.8) | 99 (24.8) | −1.513 (0.130) | 71 (14.2) | 112 (22.4) | −5.890 (0.000) | 194 (21.6) | 176 (23.8) | −5.352 (0.000) |
| Reheated oil/fat is bad | 178 (44.5) | 303 (76.3) | −1.470 (0.141) | 103 (20.6) | 18 (3.6) | 1.292 (0.196) | 335 (37.2) | 573 (64.0) | −0.086 (0.931) |
| High fibre diet | |||||||||
| Green leafy vegetables important | 351 (87.8) | 361 (90.5) | −1.159 (0.247) | 441 (88.4) | 465 (93.4) | −2.704 (0.007) | 792 (88.1) | 826 (92.1) | −2.744 (0.006) |
| Salads in every meal essential | 299 (74.8) | 315 (79.3) | −1.899 (0.058) | 341 (68.2) | 401 (80.2) | −3.271 (0.001) | 640 (71.1) | 716 (79.8) | −3.752 (0.000) |
| Unpeeled fruits are good | 193 (48.4) | 274 (69.2) | −6.457 (0.000) | 207 (41.1) | 378 (75.8) | −10.228 (0.000) | 400 (44.5) | 652 (72.8) | −12.003 (0.000) |
| Natural vitamins | |||||||||
| Fruits in diet important | 341 (85.2) | 349 (87.9) | −1.295 (0.195) | 428 (85.6) | 468 (93.8) | −4.149 (0.000) | 769 (85.4) | 817 (91.2) | −3.824 (0.000) |
Table 4.
Comparison of chronic disease related dietary behaviors at baseline and 6-month follow-up (number, %).
| Variables | Urban |
Intergroup comparison |
Rural |
Intergroup comparison |
Total |
Intergroup comparison |
|||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (n = 400) | Follow-up (n = 400) | Mann–Whitney U test (p value) | Baseline (n = 500) | Follow-up (n = 500) | Mann–Whitney U test (p value) | Baseline (n = 400) | Follow-up (n = 400) | Mann–Whitney U test (p value) | |
| High protein diet | |||||||||
| Seive the flour for chapatis | 230 (66.1) | 174 (47.9) | −4.883 (0.000) | 380 (91.8) | 262 (58.1) | −11.311 (0.000) | 610 (80.1) | 436 (53.6) | −11.120 (0.000) |
| Regular whole gram intake (>15 times/mt) | 9 (3.0) | 7 (2.2) | −0.676 (0.499) | 15 (3.9) | 69 (15.4) | −5.496 (0.000) | 24 (3.5) | 76 (9.8) | −4.763 (0.000) |
| Regular sprouts intake (>15 times/mt) | 5 (3.8) | 4 (2.7) | −0.526 (0.599) | 3 (1.8) | 3 (1.1) | −0.557 (0.578) | 8 (2.7) | 7 (1.7) | −0.891 (0.373) |
| Regular milk consumption (>20 times/mt) | 77 (50.0) | 42 (36.8) | −2.139 (0.032) | 144 (61.8) | 83 (40.7) | −4.403 (0.000) | 221 (57.1) | 125 (39.3) | −4.700 (0.000) |
| Regular curds consumption (>20 times/mt) | 44 (16.1) | 18 (10.1) | −1.808 (0.071) | 51 (19.3) | 21 (8.8) | −3.383 (0.001) | 95 (17.7) | 39 (9.3) | −3.689 (0.000) |
| Regular paneer intake (10–15 times/mt) | 11 (10.4) | 4 (6.9) | −0.737 (0.461) | 3 (12.5) | 2 (2.3) | −2.106 (0.035) | 14 (10.8) | 6 (4.2) | −2.094 (0.036) |
| Low fat diet | |||||||||
| Use of ghee on chapatis | 39 (52.7) | 35 (43.8) | −0.505 (0.613) | 155 (61.0) | 185 (69.8) | −0.790 (0.430) | 194 (59.1) | 220 (63.8) | −0.075 (0.940) |
| Regular butter milk consumption | 27 (17.9) | 11 (8.9) | −2150 (0.032) | 124 (57.4) | 71 (39.4) | −3.556 (0.000) | 151 (41.1) | 82 (27.0) | −3.835 (0.000) |
| High fibre diet | |||||||||
| Regular consumption of salads | 39 (17.6) | 22 (8.0) | −3.228 (0.001) | 45 (16.6) | 35 (9.7) | −2.570 (0.010) | 84 (17.0) | 57 (9.0) | −4.059 (0.000) |
| Natural vitamins | |||||||||
| Addition of lemon juice to foods | 86 (22.3) | 96 (25.9) | −1.157 (0.247) | 116 (23.3) | 123 (24.8) | −0.497 (0.619) | 202 (22.9) | 219 (25.3) | −1.134 (0.257) |
4. Discussion
This study shows that a six-month multicomponent population based intervention increases knowledge and awareness of chronic diseases and risk factors in urban and rural low and middle socioeconomic status middle aged women in India. The intervention is not effective on changing dietary behaviors and practices. The study did not evaluate change in risk factors.
The efficacy of population based intervention on improving knowledge of chronic diseases, change in nutrition-related behaviours, changes in risk factors and disease outcomes has been studied in multiple studies in high income countries. Pennant et al systematically reviewed the effectiveness of community based programs in high-income countries for prevention of cardiovascular disease and evaluated studies published from years 1970 to mid-2008.11 Controlled studies of community programs for primary prevention of CVD were included. There were 36 relevant community programs and most of these programs used combination of media, screening and counselling activities and most were before-after studies similar to the present study. In 22 studies investigators reported improvement in physiological risk factors such as obesity, blood pressure or lipids while in other 14 there were no significant changes in risk factors. Brunner et al performed a meta-analysis of 17 randomized controlled trials and studied influence of intensive dietary behavioral interventions of at least 3-months duration for change in cardiovascular risk factors.9 After 3–6 months, there was decrease in dietary fat intake and decrease in serum cholesterol, urinary sodium and blood pressure. In this meta-analysis, the average duration of intervention was similar to the present study. We could demonstrate only a knowledge increase while there was no change in behaviors and practices. As the present study did not assess risk factors after the intervention, the studies are not comparable.
There are limited number of studies in low and low-middle income countries that evaluated influence of population based public health interventions for increasing awareness and practices of chronic diseases such as cardiovascular diseases, or influence of these interventions of cardiovascular and chronic disease risk factors, or on all-cause and cardiovascular mortality.30 Sarrafzadegan et al17 performed a comprehensive integrated community based randomized lifestyle intervention study in Isfahan, Iran and evaluated changes in diet, smoking and physical activity in urban and rural areas. After 4 years, at intervention sites there was more uptake of healthy diet, reduced smoking and lesser decline in physical activity. Mean lifestyle score was better in intervention as compared to control populations. Aziz et al18 evaluated effects of a household based intervention delivered by a social worker focussing on fat and salt in lower middle class community in Karachi, Pakistan. At two years there was 48% lower fat intake and 41% lower salt intake in intervention households as compared to control households. Prabhakaran et al31 studied influence of a multilevel comprehensive worksite risk reduction program in influencing cardiovascular risk in industrial workers in India. The interventions focused on behaviors at individual level, interpersonal level and environmental-population level. In the intervention sites there was a significant reduction in smoking-tobacco use, more physical activity, more consumption of fruits and lower consumption of salt at 4-year follow-up. There was significant decline in weight, waist size, blood pressure, fasting glucose and cholesterol at intervention sites. The benefits were confirmed in cross-sectional populations as well as cohort populations. Shah et al,32 evaluated influence of a school-based multilevel risk reduction program in increasing awareness for chronic diseases in different regions of India. Singhal et al,33 reported benefits of this school intervention program in reducing obesity and truncal obesity among school children in Delhi, India. Small studies in Nigeria34 and Cameroon35 failed to demonstrate benefits of a population-wide intervention program on cardiovascular and chronic disease risk factors. The present study is unique as it has been performed all over the country, has large number of illiterate rural subjects, has focus on women, has a multilevel population wide easily replicable intervention and has demonstrated benefits in terms of better disease and dietary awareness. There are subtle changes in behavior (Table 4) but the study duration is too short to assess change in risk factors.
This study has other limitations also. The study has been performed at limited centers in India and may not represent the whole country. However, this is the largest study in the country (Fig. 1) and has representation from rural as well as urban regions. Secondly, focus on study on women only may be considered a limitation but we consider this a study strength because influencing behavior of women has transformative benefits on the society as suggested by WHO.22 Thirdly, short duration of follow-up and assessment of knowledge and behaviors in a small sub-sample of the study cohort is an important limitation. The study was initially designed with a larger sample with greater assessment of knowledge and behaviors, 12 month intervention, and reassessment of knowledge and practices with risk factor assessment at the end. However, shortage of funding led to curtailing of the follow-up duration and risk factor assessment at follow-up. The six-month duration for risk factor assessment was considered too short a period and therefore the study was re-designed as assessment of knowledge and behaviors only. Fourthly, sampling for knowledge and behaviors in a random 900 of the more than 4600 women evaluated could lead to sampling bias. Proper randomization techniques were used and such a strategy is considered methodologically and statistically adequate according to the WHO guidelines.29 And finally, use of non-parametric statistics in a small sample may not be appropriate for assessment of knowledge and behaviors. We, therefore, combined the questions into a comprehensive risk score (Table 3) as has been performed in previous studies and advised in a meta-analysis.11
The cardiovascular epidemic is evolving in low and low-middle income countries. Risk factors are widespread and there are limited efforts at prevention and control of these diseases.30 Policy initiatives are few.36 The United Nations Organization General Assembly guidelines have recently recommended national policy changes to focus on the epidemic of chronic diseases, especially in low and middle income countries.37 These guidelines recommend national focus on promotion of healthy diet, more physical activity, moderation of alcohol intake and smoking-tobacco cessation. Increasing awareness and practices are critical components of these guidelines and important in each of these fields. The present study shows that a short-term multilevel intervention can increase chronic disease awareness and risk factor knowledge among largely illiterate and low educational status Asian Indian women. Changes in behaviors and practices are not apparent and influence of risk factors conjectural. Larger studies with a longer follow-up with assessment of risk factors and disease outcomes are required before the present strategies are translated into practice.
Author contributions
RMP, AM, NKV and VS designed the study, wrote the protocols and obtained funding. AA, VS and RG analyzed the data and RG wrote the first and subsequent drafts of the manuscript. VS, PM, SD, NK, VUM, KR, KPV and KV were involved in data collection and study management at individual centers. They also critically reviewed the drafts and contributed to manuscript. All authors have read the manuscript and agree to its contents. This article has not been submitted elsewhere for publication.
Conflicts of interest
All authors have none to declare.
Acknowledgement
This work was supported by ad-hoc research grants from Science and Society Division, Department of Science and Technology, Government of India, New Delhi to all the participating centers. The contribution of study coordinators and research workers in data collection and management is gratefully acknowledged.
References
- 1.World Health Organization . World Health Organization; Geneva: 2011. Global Status Report of Non Communi-cable Diseases 2010. [Google Scholar]
- 2.Fuster V., Kelly B.B., Board for Global Health . Institute of Medicine; Washington: 2010. Promoting Cardiovascular Health in Developing World: A Critical Challenge to Achieve Global Health. [PubMed] [Google Scholar]
- 3.Anand S.S., Yusuf S. Stemming the global tsunami of cardiovascular disease. Lancet. 2011;377:529–532. doi: 10.1016/S0140-6736(10)62346-X. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . World Health Organization; Geneva: 2005. Chronic Diseases: A Vital Investment. [Google Scholar]
- 5.Rose G. Oxford University Press; Oxford: 1992. The Strategy of Preventive Medicine. [Google Scholar]
- 6.Farquhar J.W., Maccoby N., Wood P.D. Community education for cardiovascular health. Lancet. 1977;1(8023):1192–1195. doi: 10.1016/s0140-6736(77)92727-1. [DOI] [PubMed] [Google Scholar]
- 7.Blackburn H. Population strategies of cardiovascular disease prevention: scientific base, rationale and public health implications. Ann Med. 1989;21:157–162. doi: 10.3109/07853898909149926. [DOI] [PubMed] [Google Scholar]
- 8.Elder J.P., Schmid T.L., Dower P., Hedlund S. Community heart health programs: components, rationale, and strategies for effective interventions. J Public Health Policy. 1993;14:463–479. [PubMed] [Google Scholar]
- 9.Brunner E., White I., Thorogood M. Can dietary interventions change diet and cardiovascular risk factors? A meta-analysis of randomized controlled trials. Am J Public Health. 1997;87:1415–1422. doi: 10.2105/ajph.87.9.1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parker D.R., Assaf A.R. Community interventions for cardiovascular disease. Prim Care. 2005;32:865–881. doi: 10.1016/j.pop.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 11.Pennant M., Davenport C., Bayliss S., Greenheld W., Marshall T., Hyde C. Community programs for the prevention of cardiovascular disease: a systematic review. Am J Epidemiol. 2010;172:501–516. doi: 10.1093/aje/kwq171. [DOI] [PubMed] [Google Scholar]
- 12.Thompson B.T., Coronado G., Snipes S.A., Puschel K. Methodological advances and ongoing challenges in designing community based health promotion programs. Annu Rev Public Health. 2003;24:315–340. doi: 10.1146/annurev.publhealth.24.100901.140819. [DOI] [PubMed] [Google Scholar]
- 13.Sellers D.E., Crawford S.L., Bullock K., McKinlay J.B. Understanding the variability in the effectiveness of community heart health programs: a meta-analysis. Soc Sci Med. 1997;44:1325–1339. doi: 10.1016/s0277-9536(96)00263-8. [DOI] [PubMed] [Google Scholar]
- 14.Marmot M.G. Social determinants of health inequities. Lancet. 2005;365:1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 15.Gupta R., Joshi P., Mohan V., Reddy K.S., Yusuf S. Epidemiology and causation of coronary heart disease and stroke in India. Heart. 2008;94:16–26. doi: 10.1136/hrt.2007.132951. [DOI] [PubMed] [Google Scholar]
- 16.Reddy K.S., Shah B., Varghese C., Ramadoss A. Responding to the threat of chronic diseases in India. Lancet. 2005;336:1744–1749. doi: 10.1016/S0140-6736(05)67343-6. [DOI] [PubMed] [Google Scholar]
- 17.Sarrafzadegan N., Kelishadi R., Esmaillzadeh A. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bull World Health Organ. 2009;87:39–50. doi: 10.2471/BLT.07.049841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aziz K.U., Dennis B., Davis C.E. Efficacy of CVD risk factor modification in a lower middle class community in Pakistan: the Metroville Health Study. Asia Pac J Public Health. 2003;15:30–36. doi: 10.1177/101053950301500106. [DOI] [PubMed] [Google Scholar]
- 19.Mohammadifard N., Kelishadi R., Safavi M. Effect of a community-based intervention on nutritional behaviour in a developing country setting: the Isfahan Healthy Heart Programme. Public Health Nutr. 2009;12:1422–1430. doi: 10.1017/S1368980008004230. [DOI] [PubMed] [Google Scholar]
- 20.Saptharishi L., Soudarssanane M., Thiruselvakumar D. Community based randomized controlled trial of non-pharmacological interventions in prevention and control of hypertension among young adults. Indian J Community Med. 2009;34:329–334. doi: 10.4103/0970-0218.58393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Villablanca A.C., Arline S., Lewis J., Raju S., Sanders S., Carrow S. Outcomes of national community organization cardiovascular prevention programs for high-risk women. J Cardiovasc Transl Res. 2009;2:306–320. doi: 10.1007/s12265-009-9118-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization . World Health Organization; Geneva: 2003. Diet, Nutrition and the Prevention of Chronic Diseases. Report of a Joint WHO-FAO Consultation. [PubMed] [Google Scholar]
- 23.Zhuo X., Zhang P., Gregg E.W. A nationwide community-based lifestyle program could delay or prevent type 2 diabetes cases and save $5.7 billion in 25 years. Health Aff (Millwood) 2012;31:50–60. doi: 10.1377/hlthaff.2011.1115. [DOI] [PubMed] [Google Scholar]
- 24.Pandey R.M., Gupta R., Misra A. Determinants of urban-rural differences in cardiovascular risk factors in middle-aged women in India: a cross-sectional study. Int J Cardiol. August 2011 doi: 10.1016/j.ijcard.2011.06.008. Early online. [DOI] [PubMed] [Google Scholar]
- 25.Gupta R., Pandey R.M., Misra A. High prevalence and low hypertension awareness, treatment and control in Asian Indian women. J Hum Hypertens. September 2011 doi: 10.1038/jhh.2011.79. Early online. [DOI] [PubMed] [Google Scholar]
- 26.Misra A., Pandey R.M., Devi J.R., Sharma R., Vikram N.K., Khanna N. High prevalence of diabetes, obesity and dyslipidemia in urban slum population in northern India. Int J Obes. 2001;25:1722–1729. doi: 10.1038/sj.ijo.0801748. [DOI] [PubMed] [Google Scholar]
- 27.Luepkar R.V., Evans A., McKeigue P., Reddy K.S. 3rd ed. World Health Organization; Geneva: 2004. Cardiovascular Survey Methods. [Google Scholar]
- 28.Bharathi A.V., Sandhya N., Vaz M. The development and characteristics of a physical activity questionnaire for epidemiological studies in urban middle class Indians. Indian J Med Res. 2000;11:95–102. [PubMed] [Google Scholar]
- 29.WHO Expert Committee . World Health Organization; Geneva: 1995. Physical Status: The Use and Interpretation of Anthropometery. [Google Scholar]
- 30.Beaglehole R., Bonita R., Horton R., Lancet NCD Action Group Priority actions for the non-communicable disease crisis. Lancet. 2011;377:1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 31.Prabhakaran D., Jeemon P., Goenka S. Impact of a worksite intervention program on cardiovascular risk factors: a demonstration project in an Indian industrial population. J Am Coll Cardiol. 2009;53:1718–1728. doi: 10.1016/j.jacc.2008.12.062. [DOI] [PubMed] [Google Scholar]
- 32.Shah P., Misra A., Gupta N. Improvement in nutrition related knowledge and behaviour of urban Asian Indian school children: findings from the “medical education for children/adolescents for realistic prevention of obesity and diabetes and for healthy aging “ (MARG) intervention study. Br J Nutr. 2010;104:427–436. doi: 10.1017/S0007114510000681. [DOI] [PubMed] [Google Scholar]
- 33.Singhal N., Misra A., Shah P., Gulati S. Effects of controlled school-based multi-component model of nutrition and lifestyle interventions on behaviour modification, anthropometery and metabolic risk profile of urban Asian Indian adolescents in North India. Eur J Clin Nutr. 2010;64:364–373. doi: 10.1038/ejcn.2009.150. [DOI] [PubMed] [Google Scholar]
- 34.Hendriks M., Brewster L., Wit F. Cardiovascular disease prevention in rural Nigeria in the context of a community based health insurance scheme: quality improvement cardiovascular care Kwara-I (QUICK-I) BMC Public Health. 2011;11:186. doi: 10.1186/1471-2458-11-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De-Graft A.A., Boynton P., Atanga L.L. Developing effective chronic disease interventions in Africa: insights from Ghana and Cameroon. Glob Health. 2010;19(6):6. doi: 10.1186/1744-8603-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gupta R., Guptha S., Joshi R., Xavier D. Translating evidence into policy for cardiovascular disease control in India. Health Res Policy Syst. 2011;9:8. doi: 10.1186/1478-4505-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mamudu H.M., Yang J.S., Novotny T.E. UN resolution on the prevention and control of non-communicable diseases: an opportunity for global action. Glob Public Health. 2011;6:347–353. doi: 10.1080/17441692.2011.574230. [DOI] [PubMed] [Google Scholar]


