Highlights
► Ovarian small-cell carcinoma of the hypercalcemic type is a rare neoplasm with no standard treatment. ► The chemotherapy regimen including vinblastine, cisplatin, cyclophosphamide, bleomycin, doxorubicin and etoposide (VPCBAE) has limited toxicities and was effective in the 3 patients described in this case report.
Keywords: Ovarian cancer, Small cell, Chemotherapy
Background
Ovarian small-cell carcinoma of the hypercalcemic type is a rare neoplasm that typically occurs in young females, with an average age at diagnosis of 23.9 years (Young et al., 1994, 2010). Patients typically present with advanced stage disease with a 5-year overall survival of 10% (Dykgraaf et al., 2009). There is currently no standard protocol for managing this rare type of carcinoma. However, a previous report by Senekjian et al. (1989) demonstrated response rates with a chemotherapy regimen including vinblastine, cisplatin, cyclophosphamide, bleomycin, doxorubicin and etoposide (VPCBAE). The current report presents a case series of three patients with clinical stage I ovarian small-cell carcinoma of the hypercalcemic type treated with unilateral salpingo-oophorectomy followed by six cycles of chemotherapy with VPCBAE.
Case series
Case 1
A 24 year-old nulligravid woman was noted to have a pelvic mass on physical examination. Transvaginal sonography and a computed tomography (CT) scan confirmed a solid left adnexal mass. She underwent an exploratory laparotomy and was noted to have a 16 cm left ovarian necrotic mass with no evidence of extra-ovarian disease. A left salpingo-oophorectomy (LSO) and pelvic washings were performed and the mass was removed intact. No staging was performed. Final pathology showed an ovarian small-cell carcinoma, hypercalcemic type (Fig. 1). She received 6 cycles of VPCBAE combination chemotherapy at the following doses: vinblastine (6 mg/m2 intravenous (IV) over 30 minutes on Day 1), cisplatin (90 mg/m2 IV over 4 hours on Day 1), cyclophosphamide (1000 mg/m2 IV over 60 minutes on Day 2), bleomycin (15 units/m2 IV over 24 hours on Day 2), doxorubicin (45 mg/m2 IV over 30 minutes on Day 3), and etoposide (200 mg/m2 IV over 2 hours on Day 3). All chemotherapy was given on an inpatient basis, and pegfilgrastim 6 mg was administered following each cycle for the prevention of chemotherapy-induced neutropenia. Prior to initiating treatment, an echocardiogram and pulmonary function tests (PFTs) were obtained and found to be normal.
Fig. 1.
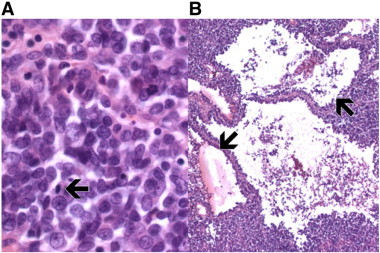
Small cell carcinoma of the ovary, hypercalcemic type. Panel A: 20× magnification; small cell carcinoma of the ovary, hypercalcemic type, is characterized by relatively monomorphic cells with scant cytoplasm arranged in sheets with frequent mitoses (arrows). Panel B: 4× magnification; follicle-like spaces that interrupt a sheet-like arrangement of cells (arrows) are noted in up to 80% of cases.
She tolerated the first five cycles of VPCBAE without difficulty. However, she experienced pancytopenia, cellulitis, and significant mucositis following her sixth cycle of treatment. She received blood and platelet transfusions and was treated with broad-spectrum antibiotics. She recovered from these complications without long-term sequelae. Of note, she resumed normal menses following completion of chemotherapy. The patient is currently without evidence of disease 33 months after completing treatment.
Case 2
A 28 year-old woman (gravida 1, para 1) presented with abdominal pain. CT scan revealed a 17 x 22 cm ovarian mass. She underwent an exploratory laparotomy and was noted to have a ruptured left adnexal mass and an inflamed retrocecal appendix. There was no evidence of metastatic disease. She underwent a LSO and appendectomy. Final pathology revealed a small cell carcinoma of the ovary, hypercalcemic type. The appendix showed no evidence of disease. She was dispositioned to 6 cycles of VPCBAE chemotherapy with the same dosing as noted in Case 1. Pegfilgrastim 6 mg was administered following each cycle.
Following her third cycle of chemotherapy, the patient was hospitalized for severe nausea, vomiting, pancytopenia and neutropenic fever. Blood cultures revealed group A beta-hemolytic streptococcocal bacteremia. During her hospitalization, she also developed acute renal insufficiency with a peak creatinine of 3.3 mg/dL that normalized with hydration. She was treated with antibiotics and underwent blood and platelet transfusions. The following dose reductions were performed for subsequent cycles of chemotherapy: cisplatin was reduced by 50% (45 mg/m2), cyclophosphamide by 25% (750 mg/m2), doxorubicin by 33% (30 mg/m2), and etoposide by 50% (100 mg/m2). Following cycle #4 of chemotherapy, the patient's PFTs showed a decrease in DLCO and her bleomycin was therefore held for cycles #5 and #6. She tolerated the remaining cycles of chemotherapy without side effect or incident.
After completion of chemotherapy, imaging showed no evidence of disease. Given that the patient was no longer interested in future fertility and the potential risk for recurrence, the patient subsequently underwent a robotic hysterectomy, RSO, and omental and peritoneal biopsies. Final pathology showed no evidence of disease. Of note, the patient had resumed ovarian function following chemotherapy prior to undergoing surgery. The patient is currently without evidence of disease 16 months following completion of therapy. However, she did experience residual neurologic sequelae after concluding treatment, with peripheral sensory and motor neuropathy with numbness and tingling in her upper and lower extremities with loss of coordination in her hands and difficulty with ambulation. Gabapentin has been initiated; she has since had significant improvement in her symptoms.
Case 3
A 26 year-old nulligravid woman presented with abdominal pain and was found to have a 15 cm right adnexal mass on CT scan. She underwent exploratory laparotomy and right salpingo-oophorectomy. Final pathology showed a small cell carcinoma of the ovary, hypercalcemic type. She received 6 cycles of VPCBAE chemotherapy with the same dosing as described in the first two cases. Pegfilgrastim 6 mg was administered following each cycle. The patient was admitted to the hospital following cycle #1 and cycle #5 with neutropenic fever. She was treated with broad-spectrum antibiotics and recovered quickly. All cultures were negative. No chemotherapy dose adjustments were made. Imaging performed 1 month after the completion of chemotherapy showed no evidence of disease.
Discussion
We report three cases of ovarian small-cell carcinoma of the hypercalcemic type treated with unilateral salpingo-oophorectomy followed by six cycles of VPCBAE chemotherapy. All patients are without evidence of disease 33, 16 and 1 month following completion of therapy.
The VPCBAE regimen has been shown by Senekjian et al. (1989) to be effective in prolonging survival in patients with early-stage disease. In that series, five cases were described, with patient ages ranging from 17 to 31 years. Four patients died 11–18 months following initial laparotomy, and one patient was alive and disease-free at 29 months. The two longest-surviving patients had stage IA disease. Major reported toxicities included severe myelosuppression, neutropenic fever, and polyneuropathy. A subsequent report by Tewari et al. (1997) used the same regimen for a woman with stage IIIC disease diagnosed during pregnancy and demonstrated a 5.5-year disease-free interval. Toxicities included severe myelosuppression, moderate-to-severe nausea and vomiting, and one episode of neutropenic sepsis. However, she completed all six courses of chemotherapy and fully recovered from all aforementioned toxicities.
The regimen administered for the three patients in our series is the same as that previously reported in the literature. However, in prior reports, chemotherapeutic agents were omitted secondary to dose-limiting myelosuppression (Senekjian et al., 1989; Tewari et al., 1997). In our series, all three patients sustained severe myelosuppression, but all were treated with colony stimulating growth factors and supportive measures such as transfusion of blood products. In Case 2, after the myelosuppressive episode following the third cycle of VPCBAE, dosages of cisplatin, cyclophosphamide, doxorubicin, and etoposide were reduced, permitting the patient to continue therapy without severe bone marrow toxicity. This dose modification strategy was effective as an alternative to discontinuing VPCBAE due to significant hematologic toxicity. In addition, the known myelosuppressive burden of this regimen merits primary prophylaxis with a colony-stimulating growth factor after each cycle of VPCBAE to prevent neutropenic fever.
The Gynecologic Cancer Intergroup recently reported a case series of 17 patients with this disease (Harrison et al., 2006). Although no consistent chemo- or radiotherapeutic regimens were reported, the authors concluded that both radiation therapy and cisplatin-based combination chemotherapy were shown to improve disease-free survival. Of the patients with stage I tumors, median survival had not yet been reached, with 7 of 10 still alive at the time of publication. In contrast, the median survival of patients with advanced disease was only 6 months.
Of note, the two patients in this series with extended follow-up resumed ovarian function following chemotherapy. Previous studies have shown post-treatment pregnancy rates of 75% to 100% among women attempting conception after receiving bleomycin, etoposide and cisplatin (BEP) in conjunction with fertility-sparing surgery for ovarian cancer (Weinberg et al., 2011). However, cyclophosphamide and doxorubicin may have significant effects and the long-term outcomes of VPBCAE on future fertility remain unknown.
There is currently no standard approach to managing ovarian small-cell carcinoma of the hypercalcemic type. The rarity of this disease has precluded the development of an established first-line chemotherapeutic regimen for this condition. To facilitate progression toward a more consistent standard of care for this rare gynecologic tumor, additional cases and case series should continue to be reported. In addition, an accessible and frequently updated case registry may serve patients and their providers with the best hope in developing the most optimal treatment for ovarian small-cell carcinoma of the hypercalcemic type.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Informed consent
Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent forms is available for review by the Editor-in-Chief of this journal upon request.
References
- Dykgraaf R.H., de Jong D., van Veen M., Ewing-Graham P.C., Helmerhorst T.J., van der Burg M.E. Clinical management of ovarian small-cell carcinoma of the hypercalcemic type: a proposal for conservative surgery in an advanced stage of disease. Int. J. Gynecol. Cancer. 2009;19:348–353. doi: 10.1111/IGC.0b013e3181a1a116. [DOI] [PubMed] [Google Scholar]
- Harrison M.L., Hoskins P., du Bois A., Quinn M., Rustin G.J., Ledermann J.A., Baron-Hay S., Friedlander M.L. Small cell of the ovary, hypercalcemic type—analysis of combined experience and recommendation for management. A GCIG study. Gynecol. Oncol. 2006;100:233–238. doi: 10.1016/j.ygyno.2005.10.024. [DOI] [PubMed] [Google Scholar]
- Senekjian E.K., Weiser P.A., Talerman A., Herbst A.L. Vinblastine, cisplatin, cyclophosphamide, bleomycin, doxorubicin, and etoposide in the treatment of small cell carcinoma of the ovary. Cancer. 1989;64:1183–1187. doi: 10.1002/1097-0142(19890915)64:6<1183::aid-cncr2820640603>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Tewari K., Brewer C., Cappuccini F., Macri C., Rogers L.W., Berman M.L. Advanced-stage small cell carcinoma of the ovary in pregnancy: long-term survival after surgical debulking and multiagent chemotherapy. Gynecol. Oncol. 1997;66:531–534. doi: 10.1006/gyno.1997.4801. [DOI] [PubMed] [Google Scholar]
- Weinberg L.E., Lurain J.R., Singh D.K., Schink J.C. Survival and reproductive outcomes in women treated for malignant ovarian germ cell tumors. Gynecol. Oncol. 2011;121(2):285–289. doi: 10.1016/j.ygyno.2011.01.003. [DOI] [PubMed] [Google Scholar]
- Young R.H., Oliva E., Scully R.E. Small cell carcinoma of the ovary, hypercalcemic type. A clinicopathological analysis of 150 cases. Am. J. Surg. Pathol. 1994;18(11):1102–1116. doi: 10.1097/00000478-199411000-00004. [DOI] [PubMed] [Google Scholar]
- Young R.H., Goodman A., Penson R.T., Russell A.H., Uppot R.N., Tambouret R.H. Case records of the Massachusetts General Hospital. Case 8–2010. A 22-year-old woman with hypercalcemia and a pelvic mass. N. Engl. J. Med. 2010;362:1031–1040. doi: 10.1056/NEJMcpc1000272. [DOI] [PubMed] [Google Scholar]


