Abstract
Background
Fractional Flow Reserve (FFR), a measure of coronary stenosis severity is based on the achievement of maximal hyperemia of coronary microcirculation. The most widely used pharmacological agent is adenosine which is administered either by intra coronary or intra venous routes. IV route is time consuming, has more side effects and expensive. This study is undertaken to compare the two routes of administration.
Methods
FFR was assessed in 50 patients with 56 intermediate focal lesions using both IV and intracoronary (IC) adenosine. FFR was calculated as the ratio of the distal coronary pressure to the aortic pressure at maximal hyperemia.
Results
A total of 25 left anterior descending, 8 right, 21 circumflex, and 2 left main coronary arteries were evaluated. The mean percent stenosis was 63.91 ± 13.13 SD and, the mean FFR was 0.831 ± 0.0738 SD for IV and 0.832 ± 0.0707 SD for IC adenosine. There was a strong and linear correlation between 2 sets of observations with IV dose and IC adenosine dose (R = 0.964, y = 0.065 + 0.923x; p < 0.001) (y = IV dose, x = IC dose). The agreement between the two sets of measurements was also high, with a mean difference of: 0.001 ± 0.0197. The changes in heart rate and blood pressure were significantly higher in IV adenosine group. Different incremental doses were well tolerated, with fewer systemic adverse events with IC adenosine. Transient AV blocks were observed with both IV and IC adenosine.
Conclusions
This study suggests that IC adenosine is equivalent to IV infusion for the determination of FFR. The administration of IC adenosine is easy to use, cost effective, safe and associated with fewer systemic events.
Keywords: Fractional Flow Reserve, Adenosine, Maximal hyperemia
1. Introduction
The temporal and spatial resolution of coronary angiography (CAG) have meant that despite major advances in noninvasive cardiac imaging, CAG continues to remain the gold standard for the diagnosis and management of coronary artery disease. However, the 2-dimensional silhouette image provided by CAG has well recognized limitations; it does not accurately represent the true complexity of the coronary luminal morphology, and gives no indication of the functional influence of luminal changes on coronary blood flow. These limitations are more pronounced in angiographically intermediate stenosis (50–90%) and in patients in whom there is a clear discrepancy between the clinical picture and angiographic findings.1–4
The measurement of Fractional Flow Reserve (FFR) is used to determine the hemodynamic significance of epicardial coronary stenosis detected at CAG.3 For an accurate calculation of FFR, the principle is to achieve a maximal hyperemia to minimize the contribution of microvascular resistance.5 With suboptimal levels of coronary hyperemia, FFR will be artificially high, resulting in a potentially significant underestimation of the functional severity of the coronary stenosis. This physiologic method of assessing the severity of coronary lesions has become a very acceptable simple method utilized in a large numbers of cardiac catheterization laboratories world over after the results of FAME study were published.4,5 The method is being utilized in our country also increasingly. We have previously demonstrated its utility and cost saving advantage in our set.6
Although adenosine invariably intravenously (IV), has been recommended for FFR measurements, intracoronary (IC) administration of adenosine constitutes a valuable alternative in everyday practice.4–9 Compared with the IC route, IV adenosine administration requires relatively large doses, and it is associated with more systemic adverse effects and costs.10,11 However, several observations cast some doubts about the ability of the IC adenosine boluses to achieve maximal hyperemia in all patients.11,12
The aim of this study was to compare IV versus IC adenosine for calculating an accurate FFR at maximal hyperemia by two methods. The FFR was calculated by both methods in our setting at maximum hyperemia.
2. Methods
2.1. Study population
FFR was assessed in a total of 50 patients enrolled prospectively. The study population consisted of 36 males and 14 females with a mean age of 62 ± 8 years. Most patients had normal left ventricular function, and only focal or short segment of coronary artery stenosis ranging from 50–90%, as assessed by QCA, were analyzed. In all patients, FFR was determined for a target coronary lesion by both IV and IC adenosine. All patients were symptomatic with angina or angina equivalent and had been referred for a diagnostic or interventional cardiac catheterization. Exclusion criteria included culprit vessel in acute coronary syndrome, acute myocardial infarction, and atrioventricular conduction abnormalities in the electrocardiogram. All patients gave informed consent to participate in the study.
2.2. Study protocol
Coronary angiography (CAG) was performed from femoral or radial approach. Heparin was administered at the beginning of the procedure (5000 units). The heart rate and arterial pressure were continuously monitored throughout the procedure. After CAG, a 0.014-inch pressure-recording guidewire (PressureWire Certus, St. Jude Medical, USA) was introduced through a guiding catheter into the coronary artery. Arterial pressure wave damping or variation of the measured coronary guide pressure was avoided. The guidewire was externally calibrated and then advanced to the distal tip of the catheter.14 At this position, it was verified that both the catheter and the pressure wire recorded equal pressures. The pressure wire was subsequently advanced into the coronary artery with the pressure sensor placed beyond the lesion site. Distal coronary and aortic pressures were measured at baseline and at maximal hyperemia. Pressure signals were continuously recorded and a beat-to-beat analysis of mean pressure was performed automatically (RadiAnalyzer Xpress, St. Jude Medical, USA).
2.3. Pharmacologic protocol
All patients first received multiple IC adenosine boluses, which were then followed by IV adenosine. Incremental doses of IC adenosine (60, 100, and 120 μg for both coronary arteries) were administered. Each bolus was followed by a flush with 5 ml saline. Subsequent doses were given after pressure curves returned to baseline values. Thereafter, adenosine infusion via a large systemic vein at incremental doses of 140, 160, 180 μg/kg/min was administered until a steady-state hyperemia was achieved for a minimal duration of 1 min15 The electrocardiogram was simultaneously recorded.
2.4. Calculations of pressure-derived FFR
FFR is defined as the ratio of the hyperemic flow in a stenotic artery to the hyperemic flow in the same artery in the hypothetical case when there is no stenosis present.16 FFR expresses maximum hyperemic blood flow in a stenotic vessel as a fraction of normal maximal blood flow in that vessel. FFR is calculated from intracoronary and aortic pressure measurements obtained during maximal hyperemia by the following equation: FFR = Pd−Pv/Pa−Pv, or FFR≅Pd/Pa (if Pv is negligible), where Pa is the mean proximal coronary pressure, Pd is the mean distal coronary pressure, and Pv is the mean central venous pressure. FFR measurement was done with IC adenosine at incremental doses. The values were taken at maximum hyperemia. This was compared with IV adenosine at sequentially increasing doses till maximum hyperemia was produced.
2.5. Statistical analysis
Data are presented as mean ± SD. Student paired t test was used to compare FFR values after different hyperemic responses for IV and IC adenosine. Linear regression was calculated for FFR data derived from both hyperemic stimuli, and nonlinear regression was used for the relation of percent stenosis to the FFR. The mean ± SD of the signed differences between measurements of FFR with intravenous and intracoronary adenosine was used as an index of agreement between measurements. Results were considered statistically significant at p ≤ 0.05.
3. Results
3.1. Patient characteristics
A total of 50 patients with 56 lesions were included in the analysis. Baseline demographic data is provided in Table 1. Procedural success was 100% for crossing the target lesion with pressure wire and there was no procedure related complication. Mean percent stenosis was 63.9 ± 13.1%.
Table 1.
Baseline demographic data of the study population.
| Study cohort (50 patients, 56 lesions) | |
|---|---|
| Age (yr.) | 62 ± 8 |
| Male/Female | 36/14 |
| Risk factors | |
| Hypertension | 18 (36%) |
| Diabetes | 21 (42%) |
| Smoking | 10 (20%) |
| Dyslipidemia | 15 (30%) |
| Old MI | 5 (10%) |
| Angiographic parameters | |
| Single vessel disease | 13 (26%) |
| Double vessel disease | 26 (52%) |
| Triple vessel disease | 11 (22%) |
| Percent stenosis (%) | 63.9 ± 13.1 |
| Target vessel | |
| LAD | 25 (44.6%) |
| LCX | 21 (37.5%) |
| RCA | 8 (14.3%) |
| LM | 2 (3.6%) |
| Ejection fraction (%) | 55 ± 5% |
LAD, Left anterior descending artery; RCA, right coronary artery; LCx, left circumflex artery; LM, left main coronary artery.
3.2. IC versus IV adenosine for FFR measurements
The mean FFR was 0.832 ± 0.0707 SD with IC adenosine and it was 0.831 ± 0.738 SD with IV adenosine. No statistically significant difference was detected between the 2 routes of administration. There was a strong and linear correlation between IC administered adenosine (as the dependent variable) and IV adenosine (as the independent variable) R = 0.964, y = 0.065 + 0.923x; p < 0.001 (Fig. 1). The agreement between the 2 sets of measurements was similarly good, with a mean difference of 0.001 and an SD of 0.0197 (Fig. 2). A random scatter in both directions of FFR measurements was, however, noted with 2 (3.6%) lesions FFR with IC adenosine was ≥0.05 as compared to IV adenosine employing a suboptimal response in these patients.
Fig. 1.
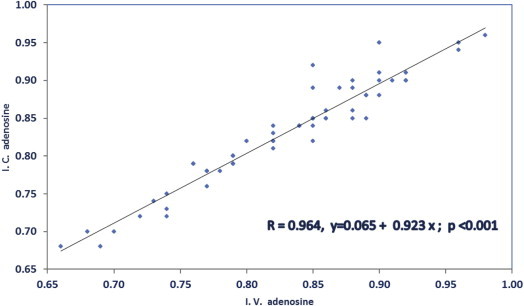
Linear regression analysis of FFR measurements performed with intracoronary (IC) (dependent variable) and intravenous (IV) 9 independent variable adenosine.
Fig. 2.
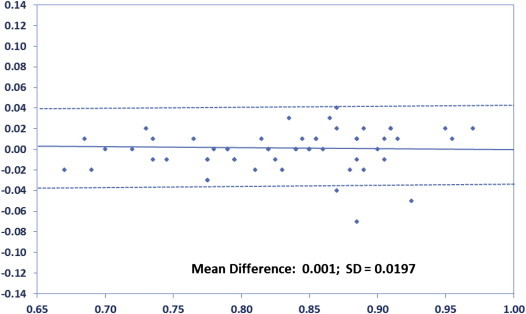
Bland–Altman agreement between 2 sets of measurements. Difference between measurements with intracoronary (IC) and intravenous (IV) adenosine plotted against mean.
Changes in heart rate and blood pressure during IC and IV adenosine administration are presented in Table 2. IV adenosine administration caused a significantly higher increase in heart rate and decrease in arterial pressure than did IC adenosine. Several systemic adverse effects (Table 3) were observed during IV adenosine administration, whereas IC boluses elicited an asymptomatic transient atrioventricular block in as many as 11% of patients.
Table 2.
Hemodynamic data for intravenous and intracoronary adenosine.
| IC adenosine (mean ± SD) | IV adenosine (mean ± SD) | p value | |
|---|---|---|---|
| ΔHR (beats/min) | 0.8 ± 3.4 | 5 ± 5.6 | <0.001 |
| ΔBP systolic (mmHg) | −3.8 ± 7.9 | −15.6 ± 16.3 | <0.001 |
| ΔBP diastolic (mmHg) | −3.4 ± 7.0 | −9.6 ± 6.8 | <0.001 |
| ΔBP mean (mmHg) | −3.2 ± 5.1 | −10 ± 12.8 | <0.001 |
IV, Intravenous; IC, intracoronary; ΔHR, difference in heart rate; ΔBP, difference in arterial blood pressure.
Table 3.
Adverse effects of different dosages and routes of administration of adenosine of determination of FFR.
| 60 μg, IC | 100 μg, IC | 120 μg, IC | IV | |
|---|---|---|---|---|
| Chest tightness | 0 | 0 | 0 | 12 (21%) |
| Dyspnea | 0 | 0 | 0 | 3 (5%) |
| Nausea | 0 | 0 | 0 | 4 (7%) |
| A-V blocks | 5 (9%) | 6 (11%) | 6 (11%) | 4 (7%) |
IC, intracoronary adenosine; IV, intravenous adenosine.
4. Discussion
Physiologic lesion assessment is a reliable method for assessing stenosis severity and a better indicator for the necessity of interventions than angiography alone.1 FFR has several advantages in clinical practice, this measure is independent of hemodynamic variation, has an unequivocal normal value of 1.0 for each vessel, and has an ischemic threshold value of 0.80 tightly related to non-invasive indexes of inducible ischemia.4,13,14 However, even for FFR calculation, it is critical to achieve a maximal decrease in myocardial resistance for an accurate estimate of its value. With submaximal hyperemia, FFR will be artificially high, and therefore, it underestimates the functional severity of the lesion. The utility of this method in clinical decision making for selecting the vessel needing PCI in borderline lesions has been clearly demonstrated in the recently published FAME and FAME 2 studies.4,5 FAME and FAME 2 used fixed dose IV adenosine, 140 μg/kg/min dose. In our study of comparison between IC and IV adenosine, we have used incremental doses in both methods to achieve hyperemia. The aim of our study was to see if maximum hyperemia can be achieved by both methods and to see its effects on FFR as measured during PCI procedures.
Adenosine, mainly IV, has been validated for FFR measurements. Several observations have raised doubts about the ability of the IC adenosine boluses to achieve maximal hyperemia in all patients and a recent study by Leone et al has demonstrated comparable hyperemia with IC adenosine to IV adenosine at higher doses (600 μg) currently suggested.9,11,12 In this study, IC bolus administration of adenosine in a dose of 60–120 μg produced equivalent maximal hyperemia to an IV infusion with incremental doses. The calculation of FFR in the majority of patients, a random scatter was observed in both directions of FFR measurements. However, in 2 (3.6%) lesions FFR with IC adenosine was ≥0.05 as compared to IV adenosine employing a suboptimal response in these patients which was statistically nonsignificant. The explanation for this comparable hyperemic response between two groups could be, adequate dosing of the drug, or meticulous delivery technique of the IC drug, or may be superior hyperemic response in the Indian ethnic population.
Administration of IV adenosine in the catheterization laboratory has several disadvantages compared with IC boluses. The latter is much easier to administer, has an extremely rapid onset of action, and has a short half-life, which makes it ideal for repetitive measurements. Furthermore, IC adenosine is associated with fewer systemic adverse effects and since, only a small fraction of the IV dosage is needed for the IC bolus it is significantly more cost effective. No major adverse events related to the IC drug administration have been reported from multiple trials measuring FFR.17 However, IV adenosine achieves a more complete and stable vasodilatation and is more convenient for the assessment of tandem lesions, diffuse coronary artery disease and ostial lesions where a pull back of the pressure wire is needed.
5. Conclusions
This study suggests that IC adenosine is equivalent to IV infusion for achievement of maximal hyperemia and the determination of FFR in short segment or focal lesions. The administration of IC adenosine is easy to use, cost effective, safe and associated with fewer systemic events.
Conflicts of interest
All authors have none to declare.
References
- 1.Kern J.M., De Bruyne B. From research to clinical practice: current role of intracoronary physiologically based decision making in the cardiac catheterization laboratory. JACC. 1997;30:613–620. doi: 10.1016/s0735-1097(97)00224-6. [DOI] [PubMed] [Google Scholar]
- 2.Kern J.M. Coronary physiology revisited. Practical insights from the cardiac catheterization laboratory. Circulation. 2000;101:1344–1351. doi: 10.1161/01.cir.101.11.1344. [DOI] [PubMed] [Google Scholar]
- 3.Topol E.J., Nissen S.E. Our preoccupation with coronary luminology: the dissociation between clinical and angiographic findings in ischemic heart disease. Circulation. 1995;92:2333–2342. doi: 10.1161/01.cir.92.8.2333. [DOI] [PubMed] [Google Scholar]
- 4.Tonino P.A., De Bruyne B., Pijls N.H. FFR versus angiography for guiding PCI. NEJM. 2009;360:213–224. doi: 10.1056/NEJMoa0807611. [DOI] [PubMed] [Google Scholar]
- 5.De Bruyne B., Pijls N.H., Kalesan B. FFR-guided PCI versus medical therapy in stable coronary disease. NEJM. 2012;367:991–1001. doi: 10.1056/NEJMoa1205361. [DOI] [PubMed] [Google Scholar]
- 6.Kaul U., Rastogi V., Seth A. Role of fractional flow reserve (FFR) in decision making during multivessel PCI and the cost effectiveness. Our experience. IHJ. 2011;63:6. [Google Scholar]
- 7.Jeremias A., Whitbourn R.J., Filardo S.D. Adequacy of IC vs IV adenosine-induced maximal coronary hyperemia for FFR measurements. AHJ. 2000;140:651–667. doi: 10.1067/mhj.2000.109920. [DOI] [PubMed] [Google Scholar]
- 8.Casella G., Leibig M., Schiele T.M. Are high doses of IC adenosine an alternative to standard intravenous adenosine for the assessment of FFR? AHJ. 2004;148:590–595. doi: 10.1016/j.ahj.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 9.Leone A.M., Porto I., de Caterina A.R. IC vs IC sodium nitroprusside vs IV adenosine: the NASCI study. JACC Intv. 2012;5:402–408. doi: 10.1016/j.jcin.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 10.Wilson R.F., Wyche K., Christensen B.V. Effects of adenosine on human coronary circulation. Circulation. 1990;82:1595–1606. doi: 10.1161/01.cir.82.5.1595. [DOI] [PubMed] [Google Scholar]
- 11.Kern M.J., Deligonul U., Tatineni S. IV adenosine: continuous infusion and low dose bolus administration for determination of coronary vasodilator reserve in patients with and without coronary artery disease. JACC. 1991;18:718–729. doi: 10.1016/0735-1097(91)90795-b. [DOI] [PubMed] [Google Scholar]
- 12.Jeremias A., Filardo S.D., Whitbourn R.J. Effect of IV and IC adenosine 5’- triphosphate as compared with adenosine on coronary flow and pressure dynamics. Circulation. 2000;101:318–323. doi: 10.1161/01.cir.101.3.318. [DOI] [PubMed] [Google Scholar]
- 13.de Bruyne B., Bartunek J., Sys S.U. Simultaneous coronary pressure and flow velocity measurements in humans: feasibility, reproducibility, and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index, and FFR. Circulation. 1996;94:1842–1849. doi: 10.1161/01.cir.94.8.1842. [DOI] [PubMed] [Google Scholar]
- 14.Pijls N.H., van Gelder B., van der Voort P. FFR: a useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation. 1995;92:3183–3193. doi: 10.1161/01.cir.92.11.3183. [DOI] [PubMed] [Google Scholar]
- 15.Wilson R.F., Wyche K., Christensen B.V. Effects of adenosine on human coronary arterial circulation. Circulation. 1990;82:1595–1606. doi: 10.1161/01.cir.82.5.1595. [DOI] [PubMed] [Google Scholar]
- 16.Pijls N.H., van Son J.A., Kirkeeide R.L. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation. 1993;87:1354–1367. doi: 10.1161/01.cir.87.4.1354. [DOI] [PubMed] [Google Scholar]
- 17.Pijls N.H.J., Klauss V., Siebert U. Coronary pressure measurements after stenting predicts adverse events at follow-up: a multicenter registry. Circulation. 2002;105:2950–2954. doi: 10.1161/01.cir.0000020547.92091.76. [DOI] [PubMed] [Google Scholar]


