Abstract
Malignant disease with pericardial metastasis is one of the most common causes of recurrent pericardial effusion (PE) with tamponade. While surgical pericardiotomy in these patients is very morbid and may not be a viable option, a palliative treatment percutaneously with percutaneous balloon pericardiotomy (PBP) can be a preferred treatment. We report herewith a case of PBP technique done using our day-to-day catheterisation laboratory equipment.
Keywords: Pericardial effusion, Pericardiotomy
Introduction
Malignant disease with pericardial metastasis is one of the most common causes of pericardial effusion (PE) with tamponade. Recurrence rates are high after pericardiocentesis and in critically ill patients it is desirable to avoid the risk of general anaesthesia and the discomfort of surgical pericardiotomy. We report a case of malignant angiocarcinoma of lung presented with malignant PE with tamponade with recurrent filling, which was successfully treated percutaneously with percutaneous balloon pericardiotomy (PBP).
Case summary
A 45-year-old female was referred to our department for recurrent PE with tamponade. The patient was a known case of malignant adenocarcinoma of the right lung with recurrent PE. Her pericardial fluid cytology was positive for malignant cells and she was planned for chemotherapy. The patient underwent emergency percutaneous pericardiocentesis at our centre via sub-xiphoid approach to relieve the tamponade and a 6 French pigtail catheter was left in the pericardial cavity for drainage. She was having repeated refilling of the pericardial cavity during the hospital stay and thus, PBP was planned for her after discussions with her family.
The procedure was done under local anaesthesia. We used a percutaneously sub-xiphoid approach to access the pericardial cavity. A 0.035” angiography guide wire was passed into the pericardial cavity. A TYSHAK II® (NuMED, New York, USA) percutaneous transluminal angioplasty (PTA) balloon catheter of 18 mm size was tried over the wire, but could not be negotiated due to lack of support. The angiography guide wire was then exchanged with stiff coiled-tip 0.25”–175 cm stainless steel Inuoe balloon guide wire with coil tip (Toray Medical, Tokyo) (Figure 1) and local site was dilated with 10 French dilator. The balloon catheter was then manipulated over the coiled-tip guide wire into the pericardial cavity. The balloon was partially inflated and withdrawn slowly until a waist appeared over the balloon which confirmed the position of the parietal pericardium (Figure 2). After optimal position, the balloon was inflated with 20cc contrast for 1 minute until the waisting disappeared (Figure 3). The absence of the waist was confirmed again, by second inflation and the balloon and coiled-tip catheter were removed subsequently. The patient remained haemodynamically stable throughout the procedure. Echocardiogram done immediately and 24 hours after the procedure, revealed no PE. Patient remained effusion-free in the 1 month follow-up.
Figure 1.

Balloon catheter in pericardial cavity over coiled-tip guide wire.
Figure 2.
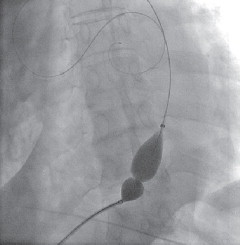
Inflated balloon showing waist at pericardial junction.
Figure 3.
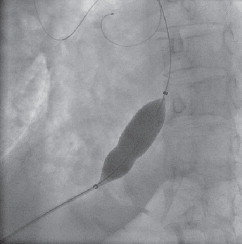
Near loss of waist and full inflation of balloon.
Discussion
Patients with large malignant PEs are often in a symptomatic, preterminal stage. The survival of this subgroup is most closely related to the extent of disease and the tumour type. In cancerous patients with symptomatic large PE, the standard treatment consisted of pericardiocentesis and drainage. Palacios et al. reported on the effectiveness of PBP,1 and in a multicentre study of 50 patients by Ziskind et al. the success rate of PBP was 95%.2 The recurrence rate after pericardiocentesis may be as high as 62%.3 Recurrence suggests the need for repeated hospitalisation, with its attendant cost, morbidity, and mortality. More recently Swanson et al. showed that balloon pericardiotomy as the initial management of symptomatic malignant PEs, allows a definitive procedure to be performed at presentation and that reaccumulation rates between balloon pericardiotomy and simple aspiration (7.4% vs 14.3%) and complication rates (7.4% vs 7.1%) were not statistically different.4 Therefore, primary therapy with a pericardial window creation should be considered.
Many individual studies and case reports across the world have reported successful percutaneous pericardiotomy; however, the use of coiled-tip balance middle weight (BMW) guide wire with springe tip in performing percutaneous pericardiotomy successfully is reported for the first time. The technique is relatively simple, safe, and can be performed with local anaesthesia and with minimal discomfort even in critically ill patients.
References
- 1.Palacios I, Tuzcu E, Sizkind A. Percutaneous balloon pericardial window for patients with malignant pericardial effusion and tamponade. Cathet Cardiovasc Diagn. 1991;22:244–249. doi: 10.1002/ccd.1810220403. [DOI] [PubMed] [Google Scholar]
- 2.Ziskind AA, Pearce AC, Lemon C. Percutaneous balloon pericardiotomy for the treatment of cardiac tamponade and large pericardial effusion: description of technique and report of the first 50 cases. J Am Coll Cardiol. 1993;21:1–5. doi: 10.1016/0735-1097(93)90710-i. [DOI] [PubMed] [Google Scholar]
- 3.Laham RJ, Cohen DJ, Kuntz RE. Pericardial effusion in patients with cancer: outcome with contemporary management strategies. Heart. 1996;75:67–71. doi: 10.1136/hrt.75.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swanson N, Mirza I, Wijesinghe N, Devlin G. Primary percutaneous balloon pericardiotomy for malignant pericardial effusion. Catheter Cardiovasc Interv. 2008;71:504–507. doi: 10.1002/ccd.21431. [DOI] [PubMed] [Google Scholar]


