Abstract
Question
Some of my pregnant patients complain about pruritus. Are there conditions in pregnancy that present with pruritus that might put the mother or fetus at risk?
Answer
Although most cases of pruritus can be attributed to itchy dry skin, there are conditions unique to pregnancy that involve pruritus as a leading symptom. These include pemphigoid gestationis, pruritic urticarial papules and plaques of pregnancy, intrahepatic cholestasis of pregnancy, and atopic eruption of pregnancy. These conditions are associated with severe pruritus and some might be associated with adverse fetal outcomes. Clinical history and physical examination are the most important diagnostic clues when evaluating pruritus in pregnancy.
Résumé
Question
Certaines de mes patientes enceintes se plaignent de démangeaisons. Y a-t-il des problèmes durant la grossesse se présentant avec un prurit qui pourraient causer des risques à la mère ou au fœtus?
Réponse
Quoique la plupart des cas de prurit puissent être attribués à une démangeaison due à la peau sèche, certains problèmes particuliers à la grossesse comportent le prurit comme principal symptôme. Parmi eux, on peut mentionner la pemphigoïde de la grossesse, les papules prurigineuses urticariennes et les plaques de la grossesse, la cholestase intrahépatique de la grossesse et l’éruption atypique de la grossesse. Ces problèmes sont associés à des formes graves de prurit et certains pourraient être reliés à des issues fœtales indésirables. Les antécédents cliniques et l’examen physique sont les indices diagnostiques les plus importants lorsqu’on évalue le prurit durant la grossesse.
Pruritus affects up to 20% of pregnant women.1,2 Pruritus can be sufficiently severe to affect sleep and quality of life, and might lead to or worsen depression.3 Although it is commonly caused by dry skin, it can also indicate an underlying condition unique to pregnancy. The dermatoses of pregnancy include pruritic urticarial papules and plaques of pregnancy (PUPPP), intrahepatic cholestasis of pregnancy (ICP), pemphigoid gestationis (PG), and atopic eruption of pregnancy.4
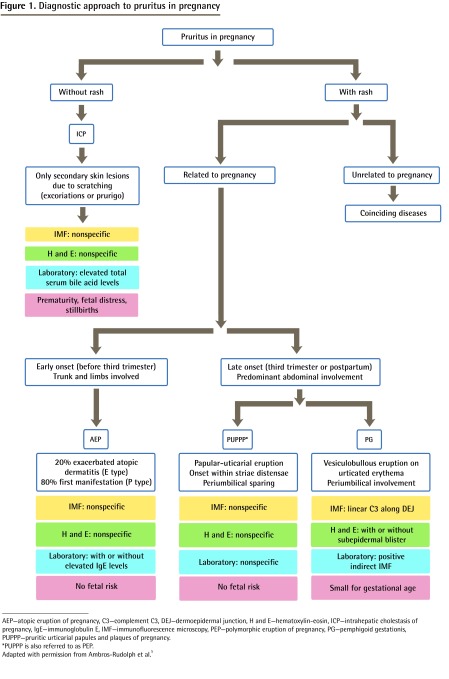
It is important for physicians to be familiar with these conditions in order to differentiate among those that can be managed symptomatically and those that require further investigation. Some of these conditions should be evaluated and managed by a multi-disciplinary team that includes an obstetrician or a maternal-fetal medicine specialist, a family physician, a dermatologist, and sometimes a gastroenterologist (Figure 1).5
Figure 1.
Diagnostic approach to pruritus in pregnancy
AEP—atopic eruption of pregnancy, C3—complement C3, DEJ—dermoepidermal junction, H and E—hematoxylin-eosin, ICP—intrahepatic cholestasis of pregnancy, IgE—immunoglobulin E, IMF—immunofluorescence microscopy, PEP—polymorphic eruption of pregnancy, PG—pemphigoid gestationis, PUPPP—pruritic urticarial papules and plaques of pregnancy.
*PUPPP is also referred to as PEP.
Adapted with permission from Ambros-Rudolph et al.5
Dermatoses unique to pregnancy
Pruritic urticarial papules and plaques of pregnancy
Pruritic urticarial papules and plaques of pregnancy is a benign, self-limited pruritic inflammatory disorder. It might also be referred to as polymorphic eruption of pregnancy, toxemia of pregnancy, or prurigo of pregnancy. The incidence of PUPPP is about 1 in 160 pregnancies (0.6%), with most cases occurring in first pregnancies in the third trimester or immediately postpartum. It also occurs more frequently in women pregnant with multiples and seldom recurs in subsequent pregnancies.4
Clinical presentation: The lesions of PUPPP are typically urticarial papules that coalesce into plaques and spread from the abdomen to the buttocks and thighs. About 50% of the time the lesions develop as microvesicles overlying the striae cutis distensae (stretch marks).5 This skin eruption starts on the abdomen, usually within the striae, and classically spares the umbilical area, palms, soles, and face. The sparing of the umbilical area helps to differentiate PUPPP from PG early on. The striae first become itchy, then erythematous, and finally urticarial. Patients are very uncomfortable and the pruritus often interferes with sleep. The lesions are rarely excoriated.
Diagnosing PUPPP: Initially, PUPPP might be confused with PG; however, sparing of the umbilicus provides the best clue to diagnosis, as PG lesions usually cluster around the umbilicus. Other disorders that might be confused with PUPPP include atopic dermatitis and contact or irritant dermatitis.
To make a diagnosis, a history and physical examination are necessary, as there are no systemic symptoms. Results of laboratory studies, including histology, serology, and immunofluorescence, are not specific.
Treatment: Pruritic urticarial papules and plaques of pregnancy is a self-limiting disorder without serious consequences to the mother and fetus. The mean duration of the eruption is 6 weeks and it remits within days of delivery. Recurrence is rare as it usually occurs in first pregnancies. Symptomatic treatment with mild to potent topical corticosteroids and antihistamines are the mainstay for treating PUPPP. Relief within 24 to 72 hours is normally seen. Oil baths and emollients are also helpful for relief of pruritus. In cases in which the diagnosis of PUPPP is not clear, referral to a dermatologist should be considered.
Intrahepatic cholestasis of pregnancy
Although ICP is a pruritic condition in pregnancy that involves only secondary skin changes, it is included in the classification of dermatoses of pregnancy because identifying this disease early is important to minimize potential adverse fetal outcomes. Intrahepatic cholestasis of pregnancy is also called idiopathic jaundice of pregnancy, obstetric cholestasis, and pruritus gravidarum. It is caused by the disruption of hepatic bile flow during pregnancy. The prevalence of ICP in North America is 0.5% to 1%, but it is particularly common in Scandinavia and South America, with the highest rates in Chile (15% to 28%).6 It runs in families and tends to recur in subsequent pregnancies.7
Clinical presentation: Intrahepatic cholestasis of pregnancy presents in the second or third trimester with the sudden onset of severe pruritus that starts on the palms and soles and quickly becomes more generalized. The pruritus persists throughout pregnancy and is worst at night. The secondary lesions involve linear excoriations and excoriated papules and develop secondary to scratching. Jaundice occurs in about 10% of patients and is due to concomitant extrahepatic cholestasis, often accompanied by dark urine and clay-coloured stools. These patients are at risk of developing steatorrhea with malabsorption of fat-soluble vitamins, including vitamin K, which might lead to bleeding complications and cholelithiasis.5
Pathophysiology: Intrahepatic cholestasis of pregnancy is a hormonally triggered cholestasis. It presents in genetically predisposed women in late pregnancy who have a defect in the excretion of bile acids resulting in elevated bile acid levels in the serum. This leads to severe pruritus in the mother and, as toxic bile acids can pass into fetal circulation, might have deleterious effects on the fetus owing to acute placental anoxia and cardiac depression. A family history of the disorder is present in half of cases, and cases with a familial component tend to be more severe.7
Diagnosis: Diagnosis is usually made based on the characteristic symptom of pruritus starting from the palms and soles that is not accompanied by a rash. The diagnosis can be confirmed by demonstrating a rise in total serum bile acid levels. In healthy pregnancies, total serum bile acid levels in the third trimester of up to 11.0 μmol/L are accepted as normal. In women with ICP, the presence of total serum bile acid levels of more than 40.0 μmol/L is associated with a higher risk of adverse fetal outcomes.4 There might also be a mild increase in liver transaminase levels including aspartate aminotransferase and alanine aminotransferase levels; this increase might only appear weeks after the onset of pruritus. Steatorrhea with subsequent vitamin K deficiency might also be noted. Close surveillance of prothrombin time might be needed. Ultrasound examination of the liver and serologic tests might be necessary to exclude other diagnoses such as cholelithiasis and viral hepatitis.
Treatment: The aim of treatment is to reduce serum bile acid levels. Ursodeoxycholic acid is the treatment of choice, as it improves maternal pruritus, decreases liver transaminase and bile acids levels, and might also reduce the rate of adverse fetal outcomes, although this latter effect is debatable.8,9 A dose of 15 mg/kg daily or 1 g daily is administered until delivery.
Before ursodeoxycholic acid treatment, cholestyramine was used to treat ICP. However, this drug can cause vitamin K deficiency, which might already occur with this disorder. Antihistamines might also improve maternal symptoms.
Elective delivery around weeks 36 to 38 has been recommended, as stillbirths tend to cluster around weeks 37 to 39. Some authors suggest that labour induction at 37 weeks is indicated only in cases of severe ICP (defined as total serum bile acid levels of more than 40 μmol/L).10
Prognosis: The prognosis for the mother is generally good. Pruritus regresses spontaneously within days to weeks after delivery but can recur with subsequent pregnancies or while using hormonal contraception.11 If jaundice and vitamin K deficiency occur, there is an increased risk of intrapartum and postpartum hemorrhage.
This condition has been associated with adverse fetal outcomes including preterm labour, meconium in the amniotic fluid, fetal distress, and fetal demise. Importantly, some have reported that fetal demise in ICP is the result of a sudden event and might occur despite a previously normal fetal heart rate tracing. Indeed, there is no evidence that close fetal monitoring in cases of ICP is effective in preventing fetal death. As a result, it has been recommended that labour be induced by 36 to 38 weeks. Prompt diagnosis, specific therapy, and close obstetric monitoring are essential.6,12 Consultation with a gastroenterologist in equivocal or severe cases is recommended.
Pemphigoid gestationis
Pemphigoid gestationis is a self-limited autoimmune bullous disorder that presents after the 20th week of gestation and might only appear in the postpartum period.
Historically, PG was referred to as herpes gestationis, a term that was coined in 1872 by Milton because of the characteristic “creeping” blister formation. However, this term might be misleading as this condition has no association with the herpes virus, and it is now referred to as pemphigoid gestationis.4 It is a relatively rare condition, with an estimated incidence of 1 in 10 000 pregnancies.13
Clinical presentation: Pemphigoid gestationis presents with intense pruritus that can precede the skin lesions. The characteristic rash begins with pruritic, urticarial, erythematous papules and plaques around the umbilicus and extremities. As the disease progresses, the lesions develop into tense blisters. The face, palms, and soles are spared and there is mucous membrane involvement about 20% of the time.4,5 Commonly, PG flares around the time of delivery but regresses spontaneously after delivery.
The pathophysiology is similar to that of bullous pemphigoid and involves immunoglobulin G directed at a 180-kDa hemidesmosome transmembrane glycoprotein.
Diagnosis: A skin biopsy is necessary to make the diagnosis. Direct immunofluorescence of perilesional skin is the criterion standard in the diagnosis of PG. It shows linear complement C3 deposition along the dermoepidermal junction, and biopsy results are characteristically negative for this in the other dermatoses of pregnancy.
The main differential diagnosis is PUPPP, especially early in the disease before the formation of the tense blisters. Thus, skin biopsy is indicated in suspected cases of PUPPP with an unusual and severe presentation that does not respond to routine therapy.
Prognosis: The natural course is characterized by exacerbations and remissions during pregnancy, with frequent improvement in late pregnancy followed by a flare-up at the time of delivery. Lesions usually resolve within weeks to months. It tends to recur in subsequent pregnancies at an earlier gestational age and with increasing severity. It might also recur with menstruation or hormonal contraception.4 There is an increased risk of other autoimmune diseases, in particular Graves disease.4
Pregnancies affected by PG are considered high risk because there is an association with an increase rate of adverse fetal outcomes, such as preterm births and low birth weight.14 Because of passive transfer of the maternal autoantibodies to the fetus, about 10% of newborns might develop mild skin lesions that resolve spontaneously within days to weeks.4
Treatment: Treatment aims to control pruritus and to prevent blister formation. In cases of mild pre-blistering state, topical corticosteroids with oral antihistamines might be sufficient. All other cases require systemic steroids—typically 20 to 60 mg of prednisone a day. The prednisone dose should be increased in time to prevent the flare that commonly occurs at delivery.
Atopic eruption of pregnancy
Atopic eruption of pregnancy is an umbrella term recently coined by Ambros-Rudolph to include prurigo of pregnancy, pruritic folliculitis of pregnancy, and eczema in pregnancy. Although in the literature they are described as separate entities, the lack of clinical distinction between these disorders led to the recently coined term.4
These are benign pruritic conditions of pregnancy that include eczematous or papular lesions in patients with a history of atopy.4
Pathogenesis: These conditions are thought to be triggered by pregnancy-specific immunologic changes— a reduced cellular immunity and reduced production of Th1 cytokines compared with the dominant humoural immunity and increased secretion of Th2 cytokines.4
Clinical presentation: Most patients (80%) experience atopic skin changes for the first time or after a long remission (since childhood).4 Most women present with widespread eczematous changes affecting typical atopic sites such as the face, neck, chest, and the flexural surfaces of the extremities, while one-third have papular lesions. These include small erythematous papules disseminated on the trunk and limbs, and typical prurigo nodules located on the shins and arms.
Diagnosis: The clinical history and physical examination are key to making the diagnosis. Histopathology is nonspecific and varies with the clinical type and stage of the disease. Direct and indirect immunofluorescence results are negative. Laboratory tests can reveal elevated serum immunoglobulin E levels. It might be helpful to culture a pustule to rule out bacterial or fungal folliculitis.
Treatment: Use of topical corticosteroids for several days will lead to improvement of the skin lesions. Severe cases might require a short course of systemic corticosteroids and antihistamines.
Prognosis: There is no associated maternal or fetal morbidity.
Conclusion
Pruritus in pregnancy requires taking a thorough history and complete physical examination. Laboratory studies such as liver transaminase levels, serum bile acid levels, and in selected cases skin biopsy might be indicated in order to determine the most likely diagnosis. The dermatoses of pregnancy should be considered in the differential diagnosis of pruritus and managed accordingly. An accurate diagnosis must be made owing to the fact that some of these conditions are associated with an increased risk of adverse fetal outcome. The treatments described for the above conditions are considered safe in pregnancy.
Motherisk
Motherisk questions are prepared by the Motherisk Team at the Hospital for Sick Children in Toronto, Ont. Dr Bergman is Clinical Pharmacology and Toxicology Fellow at the University of Toronto in Ontario. Dr Melamed is Maternal Fetal Medicine Clinical Fellow at Mount Sinai Hospital and the Hospital for Sick Children, both in Toronto. Dr Koren is Director of the Motherisk Program. Dr Koren is supported by the Research Leadership for Better Pharmacotherapy during Pregnancy and Lactation. He holds the Ivey Chair in Molecular Toxicology in the Department of Medicine at the University of Western Ontario in London.
Do you have questions about the effects of drugs, chemicals, radiation, or infections in women who are pregnant or breastfeeding? We invite you to submit them to the Motherisk Program by fax at 416 813-7562; they will be addressed in future Motherisk Updates. Published Motherisk Updates are available on the Canadian Family Physician website (www.cfp.ca) and also on the Motherisk website (www.motherisk.org).
Footnotes
Competing interests
None declared
References
- 1.Wong RC, Ellis CN. Physiologic skin changes in pregnancy. J Am Acad Dermatol. 1984;10(6):929–40. doi: 10.1016/s0190-9622(84)80305-9. [DOI] [PubMed] [Google Scholar]
- 2.Rook A, Wilkinson DS, Ebling FJ, editors. Textbook of dermatology. 3rd ed. Oxford, Engl: Blackwell Scientific Publications; 1979. p. 213. [Google Scholar]
- 3.Moses S. Pruritus. Am Fam Physician. 2003;68(6):1135–42. [PubMed] [Google Scholar]
- 4.Ambros-Rudolph CM. Dermatoses of pregnancy—clues to diagnosis, fetal risk and therapy. Ann Dermatol. 2011;23(3):265–75. doi: 10.5021/ad.2011.23.3.265. Epub 2011 Aug 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ambros-Rudolph CM, Müllegger RR, Vaughan-Jones SA, Kerl H, Black MM. The specific dermatoses of pregnancy revisited and reclassified: results of a retrospective two-center study on 505 pregnant patients. J Am Acad Dermatol. 2006;54(3):395–404. doi: 10.1016/j.jaad.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 6.Lammert F, Marschall HU, Glantz A, Matern S. Intrahepatic cholestasis of pregnancy: molecular pathogenesis, diagnosis and management. J Hepatol. 2000;33(6):1012–21. doi: 10.1016/s0168-8278(00)80139-7. [DOI] [PubMed] [Google Scholar]
- 7.Geenes V, Williamson C. Intrahepatic cholestasis of pregnancy. World J Gastroenterol. 2009;15(17):2049–66. doi: 10.3748/wjg.15.2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davies MH, da Silva RCMA, Jones SR, Weaver JB, Elias E. Fetal mortality associated with cholestasis of pregnancy and the potential benefit of therapy with ursodeoxycholic acid. Gut. 1995;37(4):580–4. doi: 10.1136/gut.37.4.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Palma J, Reyes H, Ribalta J, Hernández I, Sandoval L, Almuna R, et al. Ursodeoxycholic acid in the treatment of cholestasis of pregnancy: a randomized, double-blind study controlled with placebo. J Hepatol. 1997;27(6):1022–8. doi: 10.1016/s0168-8278(97)80146-8. [DOI] [PubMed] [Google Scholar]
- 10.Roncaglia N, Arreghini A, Locatelli A, Bellini P, Andreotti C, Ghidini A. Obstetric cholestasis: outcome with active management. Eur J Obstet Gynecol Reprod Biol. 2002;100(2):167–70. doi: 10.1016/s0301-2115(01)00463-8. [DOI] [PubMed] [Google Scholar]
- 11.Shornick JK. Dermatoses of pregnancy. Semin Cutan Med Surg. 1998;17(3):172–81. doi: 10.1016/s1085-5629(98)80011-4. [DOI] [PubMed] [Google Scholar]
- 12.Kroumpouzos G, Cohen LM. Specific dermatoses of pregnancy: an evidence-based systematic review. Am J Obstet Gynecol. 2003;188(4):1083–92. doi: 10.1067/mob.2003.129. [DOI] [PubMed] [Google Scholar]
- 13.Engineer L, Bhol K, Ahmed AR. Pemphigoid gestationis: a review. Am J Obstet Gynecol. 2000;183(2):483–91. doi: 10.1067/mob.2000.105430. [DOI] [PubMed] [Google Scholar]
- 14.Chi CC, Wang SH, Charles-Holmes R, Ambros-Rudolph C, Powell J, Jenkins R, et al. Pemphigoid gestationis: early onset and blister formation are associated with adverse pregnancy outcomes. Br J Dermatol. 2009;160(6):1222–8. doi: 10.1111/j.1365-2133.2009.09086.x. Epub 2009 Mar 9. [DOI] [PubMed] [Google Scholar]