Abstract
Objective
To determine the extent to which use of the Corsair microcatheter (CM, Asahi Intecc Co., Japan) improves procedural outcomes when an experienced operator who is not a dedicated recanalization specialist attempts retrograde chronic total occlusion (CTO) recanalization through collateral channels during percutaneous coronary intervention.
Background
The recently introduced CM has improved success rates of retrograde CTO recanalization to nearly 100% in the hands of dedicated coronary recanalization specialists; however, the impact the CM has on the results of non-specialist operators attempting retrograde CTO recanalization is not known.
Methods
A non-specialist operator attempted CM-assisted recanalization in seven consecutive CTO cases requiring retrograde recanalization. The results obtained were compared with those achieved by the same operator in eleven consecutive retrograde CTO recanalization procedures during the last 2 years before the CM became available.
Results
CM-assisted retrograde CTO recanalization was successful in 6 of 7 cases (86%), but failed in one case attempted through a tortuous epicardial collateral; there were no complications. In contrast, during the 2 years before the CM became available, retrograde CTO recanalization was successful in only 3 of 11 attempted cases (27%), and was associated with significant morbidity. Lesions in the two groups were comparable in terms of technical difficulty and procedural risk.
Conclusions
The non-specialist operator's retrograde CTO recanalization results improve significantly when using the CM. Given the effectiveness and safety of CM-assisted retrograde CTO recanalization, operators should be less aggressive with anterograde recanalization attempts, and should switch to the retrograde approach earlier and more often.
Keywords: Chronic total occlusion, Percutaneous coronary intervention, Collateral circulation, Catheter
1. Introduction
Recanalization of chronic total occlusion (CTO) of coronary arteries by percutaneous coronary intervention (PCI) has historically been associated with low success rates mainly due to failure to access the distal true lumen with the guidewire.1,2 Retrograde techniques,3–5 which use collateral channels to approach CTOs from their distal end, have improved success rates, but procedural difficulties such as the need for collateral channel dilatation (with attendant risk of channel injury) and the need for retrograde balloon access into the occlusion (that is often not possible) still remain. The recent introduction of the Corsair microcatheter (CM, Asahi Intecc Co. Ltd, Aichi, Japan, properties detailed in Table 1), that has features of both microcatheter and channel dilator,6,7 has facilitated retrograde CTO recanalization resulting in success rates close to 100% in the hands of a few dedicated CTO-specialists7; however, the impact the CM has on the results of experienced operators who occasionally perform CTO-PCI (non-specialist operators) is not known. We carried out a study to determine the extent to which use of the CM improves procedural outcomes when a non-specialist operator attempts retrograde chronic total occlusion recanalization.
Table 1.
Properties of the Corsair microcatheter.a
| Construction | Physical property conferred | Practical advantage |
|---|---|---|
| Low-profile, tapered (0.87–0.42 mm), soft, flexible (no steel wire braid) tip | Ability to smoothly enter narrow tortuous collateral channels | Eliminates need for dilatation of the collateral channel; makes use of epicardial channels safer |
| Unique spiral steel wire-braided, progressiveb polyamide elastomer-coated ≤2.8F (0.87–0.93 mm) shaft | Bidirectional torque transmission to the distal end, kink resistance and longitudinal strength of shaft | Superior pushability, trackability and back-up support; kink resistance allows easy movement of guidewires and contrast injection from the tip |
| Distal 60 cm of the 150 cm catheter has hydrophilic polymer coating | Reduces friction and enhances maneuverability and tracking | Superior ability to traverse collaterals, cross the CTO, and enter the CTO artery guiding catheter |
| Inner lumen of the shaft is lined with a fluoropolymer (PTFE) layer | Free movement of 0.014 inch guidewires within the catheter | Permits easy exchange of guidewires and full transmission of torque to the tip of the guidewire |
| Platinum marker and tungsten powder at the tip; tungsten wire braid in shaft | Enhanced fluoroscopic visibility of the catheter tip and shaft | Helps detect torque accumulation and catheter tip entrapment within the CTO; improves safety |
CTO, chronic total occlusion; PTFE, polytetrafluoroethylene.
Information sourced from Refs. 6,7 in the manuscript.
Thickness and grade of polyamide elastomer coating progressively increases towards the proximal end of the catheter.
2. Methods and results
2.1. CM-assisted retrograde CTO recanalization
2.1.1. Patients
Seven consecutive patients in whom anterograde CTO recanalization attempts failed (5 cases) or seemed unlikely to succeed due to complex coronary anatomy or lesion morphology (2 cases) were selected for retrograde CTO recanalization using the CM. Baseline patient and lesion characteristics in this group are presented in Table 2. CTO lesions were graded based on technical difficulty (A0 low, A1 intermediate, A2 high) and risk (B0 low, B1 high) associated with attempted CTO recanalization as proposed in the universal CTO classification system.8
Table 2.
Baseline patient and lesion characteristics.a
| Characteristic | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 |
|---|---|---|---|---|---|---|---|
| Age (years)/Sex | 58 M | 46 M | 54 M | 51 M | 40 M | 52 M | 49 M |
| Height (cm) | 160 | 157 | 175 | 173 | 168 | 166 | 177 |
| Weight (kg) | 57 | 70 | 73 | 70 | 84 | 59 | 68 |
| Diabetes mellitus | Yes | – | Yes | Yes | Yes | – | Yes |
| Dyslipidemia | Yes | Yes | – | Yes | – | – | Yes |
| Smoking history | Yes | – | – | – | Yes | – | Yes |
| Hypertension | – | – | – | – | Yes | Yes | – |
| Main symptom | Angina | Angina | Angina | Dyspnea | Angina | Angina | Dyspnea |
| LVEF (%) | 57 | 55 | 42 | 37 | 45 | 32 | 56 |
| CTO vessel | RCA | LAD | RCA | RCA | LCX | RCA | LAD |
| CTO segment | Prox-mid | Mid | Prox-mid | Prox-mid | Distal | Mid | Prox-mid |
| CTO length (mm) | 23 | 18 | 25 | 20 | 20 | 15 | 15 |
| CTO duration | 4 years | 9 months | 14 years | 5 years | 8 years | 1 year | >5 years |
| CTO gradeb | A2 B1 | A2 B0 | A2 B1 | A2 B1 | A2 B0 | A1 B1 | A2 B1 |
| CTO-related MI | None | Anterior | Inferior | Inferior | Inferior | None | None |
| Previous failurec | Yes | Yes | No | Yes | No | Yes | Yes |
Characteristics presented are those of patients in whom Corsair microcatheter-assisted retrograde coronary artery recanalization was attempted; M, male; LVEF, left ventricular ejection fraction; CTO, chronic total occlusion; RCA, right coronary artery; LAD, left anterior descending artery; LCX, left circumflex artery; LV, left ventricle; Prox, proximal; MI, myocardial infarction.
Grade of technical difficulty (A0 low, A1 intermediate, A2 high) and risk (B0 low, B1 high) associated with attempted CTO recanalization based on the universal CTO classification system.8
Failed previous anterograde CTO recanalization attempt.
2.1.2. Procedure
All procedures were performed by an experienced PCI operator (who was not a dedicated CTO-specialist) after obtaining written informed consent. Local anesthesia and bi-femoral percutaneous 7F access were used. Anti-platelet therapy with aspirin and clopidogrel was started several days prior to the procedure, and 7000–8000 units of heparin were administered during the procedure. Intravascular ultrasound guidance was not available, and pre-operative CT coronary angiography was not performed. Procedural details are presented in Table 3 and Figs. 1 and 2. In all cases a 0.014″ Fielder FC hydrophilic wire (Asahi) and CM were used to enter the selected collateral arising from the donor artery; navigation through the collateral to reach the distal CTO artery was done using a 0.014″ Fielder XT hydrophilic wire (Asahi). In all of six successful cases, the CM was advanced through a collateral channel to the distal cap of the CTO using forward push combined with alternating clockwise and anti-clockwise rotation. Balloon dilatation of septal collaterals was not required except in case 4 where non-availability of a new CM necessitated use of a re-sterilized CM that lacked sufficient lubricity. The distal cap of the CTO was probed using soft and then hard wires with the CM providing back-up support. In four cases balloon dilatation of a track made by a stiff guidewire advanced anterograde into the CTO (reverse controlled antegrade and retrograde tracking technique)5,9 was necessary before a retrograde stiff wire could be advanced through the lesion into the CTO artery guiding catheter; in cases 2 and 7 a retrograde soft wire successfully crossed the CTO without prior anterograde balloon dilatation (these lesions had been probed with anterograde stiff wires earlier). The CM was advanced over the retrograde wire into the CTO artery guiding catheter in most cases without the use of a balloon or snare to anchor the retrograde wire within the CTO artery guiding catheter; this allowed subsequent externalization of a 300-cm 0.014″ retrograde guidewire and creation of a femoro-femoral trans-coronary wire-loop; balloon catheters introduced anterograde over the wire-loop enabled dilatation of the entire CTO and subsequent placement of a soft 180-cm 0.014″ anterograde wire in the distal CTO artery parallel to the wire-loop. Stenting of the CTO was performed over the anterograde wire in standard fashion using sirolimus-eluting stents in all cases.
Table 3.
Procedure details.a
| Detail | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 |
|---|---|---|---|---|---|---|---|
| Donor vessel | LAD | RCA | LAD | LAD | RCA | LAD | RCA |
| Donor vessel guiding catheter | 7F XB-LAD | 6F JR3.5 | 7F XB-LAD | 6F XB-LAD | 7F AR2 | 7F XB-LAD | 7F JR3.5 |
| CTO vessel | RCA | LAD | RCA | RCA | LCX | RCA | LAD |
| CTO vessel guiding catheter | 7F JR3.5 | 7F XB-LAD | 7F AL1 | 7F JR3.5 | 7F XB-LAD | 7F JR3.5 | 7F XB-LAD |
| Collateral used | 2nd septal | 8th septal | 3rd septal | 2nd septal | Epicardial | 1st septal | Epicardial |
| Anterograde track dilatation | Yes | No | Yes | Yes | No | No | Yes |
| CTO crossing retrograde wire | CP 8-20 | Fielder FC | CP 8-20 | CP 8-20 | - | Miracle 3g | Fielder FC |
| Length of vessel stented (mm) | 66 | 32 | 38 | 90 | – | 67 | 70 |
| Concurrent PCI | Proximal LCX | First diagonal | Mid-LAD | None | LM-LAD | None | None |
| Contrast volume (ml) | 130 | 200 | 200 | 160 | 110 | 120 | 350 |
| Fluoroscopy time (min) | 54.2 | 66.5 | 120.1 | 126.0 | 52.3 | 38.5 | 122.2 |
| Procedure time (min) | 118 | 123 | 205 | 205 | 115 | 78 | 260 |
| Outcome | Successful | Successful | Successful | Successful | Failure | Successful | Successful |
| Complications | None | None | None | None | None | None | None |
Details presented are those of patients in whom Corsair microcatheter-assisted retrograde coronary artery recanalization was attempted; LAD, left anterior descending; RCA, right coronary artery; XB, extra back-up; JR, Judkins right; AR, Amplatz right; CTO, chronic total occlusion; LCX, left circumflex; AL, Amplatz left; CP, Conquest Pro; PCI, percutaneous coronary intervention; LM, left main coronary artery.
Fig. 1.
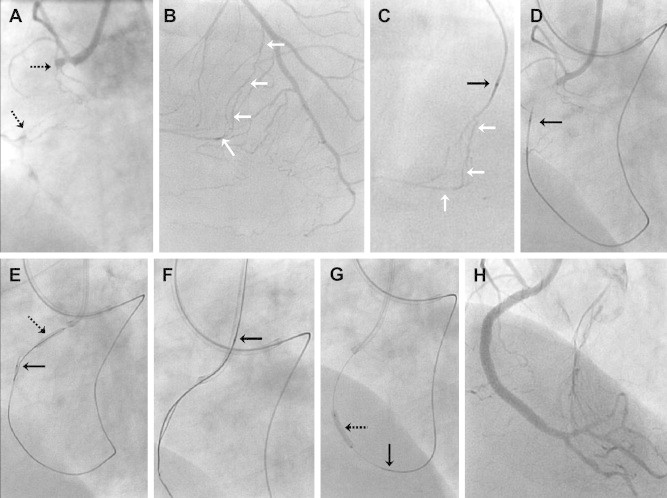
Case 1. (Solid black arrows, wherever present, indicate the tip of the Corsair microcatheter (CM), and white arrows delineate the septal collateral channel used.) A. Right coronary artery (RCA) angiogram showing proximal-mid segment chronic total occlusion (CTO, broken arrows) with obstructive disease further downstream as well. B. Left coronary angiogram and C. contrast injection through CM delineating channel selected for retrograde RCA CTO recanalization. D. The CM has been advanced into the distal end of the RCA CTO. E. Balloon dilatation of intra-CTO channel created by anterograde wire. F. The CM has been advanced into the RCA guiding catheter over the retrograde wire. G. Dilatation of RCA CTO by balloon catheter introduced anterogradely over a femoro-femoral trans-coronary wire-loop. H. Final angiogram after RCA stenting shows successful outcome.
Fig. 2.
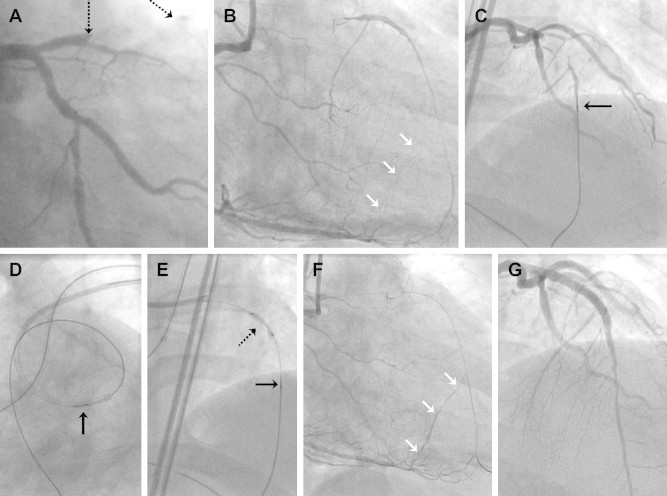
Case 2. (Solid black arrows, wherever present, indicate the tip of the Corsair microcatheter (CM), and white arrows delineate the septal collateral channel used.) A. Left coronary artery (LCA) angiogram showing mid-segment chronic total occlusion (CTO, broken arrows) of the left anterior descending (LAD) artery. B. Right coronary angiogram showing channel selected for retrograde LAD CTO recanalization. C. The CM has been advanced close to the distal end of the LAD CTO. D. The CM has been advanced into the LCA guiding catheter over the retrograde wire. E. Dilatation of LAD CTO by balloon catheter (broken arrow) introduced anterogradely over a femoro-femoral trans-coronary wire-loop. F. Right coronary angiogram, after anterograde LAD wiring and removal of CM, showing absence of injury in the septal channel used. G. Final LCA angiogram after LAD stenting showing successful outcome.
2.1.3. Results
A successful PCI result was obtained in 6 out of 7 cases. Case 5 was unsuccessful because of extreme tortuosity (that was not appreciated earlier during diagnostic angiography) in the only sizeable epicardial collateral channel present. There were no procedural complications, in-hospital deaths, emergency bypass procedures, or myocardial infarctions. Specifically, there was no collateral channel or donor artery injury, cardiac tamponade, catheter entrapment, access site complication or contrast induced nephropathy. All patients were discharged 48–72 h after the procedure in stable condition.
2.2. Retrograde CTO recanalization prior to availability of the CM
The above results were compared with those obtained in all cases (11 in number) of retrograde CTO recanalization attempted by the same operator during the last 2 years before the CM became available (Table 4). Apart from the CM, recanalization equipment available was similar during this period, as was the recanalization strategy. Technical difficulty and procedural risk grades8 of the CTO lesions in this group were comparable to those in the CM-assisted recanalization group. In contrast to the 86% success (6 out of 7 cases) with no complications obtained in CM-assisted recanalization, 27% success (3 out of 11 cases) with significant complications prevailed in the pre-CM period (chi square test 2-tailed p = 0.087); these complications were mainly related to concomitant aggressive antegrade recanalization attempts, which in turn were necessitated by failure of retrograde recanalization.
Table 4.
Retrograde CTO recanalization outcomes prior to the availability of the Corsair microcatheter (2009–2010).a
| Case No. | Age Sex | CTO vessel | Donor vessel | CTO gradeb | Crossing of CC by guidewire | Balloon dilatation of CC | Crossing of CC by microcatheterc | Retrograde CTO crossing by guidewire | Outcome | Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | 58 M | LAD | RCA | A2 B0 | Yes | Yes | Yes | Yes | Success | – |
| 2. | 67 M | LAD | LCX | A2 B0 | No | No | No | No | Failuree | – |
| 3. | 60 F | RCA | LAD | A2 B1 | Yes | No | No | No | Failure | – |
| 4. | 52 M | RCA | LAD | A1 B1 | Yes | No | No | No | Failure | Cardiac tamponaded |
| 5. | 64 M | RCA | LAD | A2 B1 | Yes | Yes | Yes | No | Failure | – |
| 6. | 60 M | LAD | RCA | A2 B1 | No | No | No | No | Failure | – |
| 7. | 62 M | LAD | LCX | A2 B0 | No | No | No | No | Failure | Cardiac tamponaded |
| 8. | 65 F | LAD | RCA | A2 B0 | Yes | Yes | No | No | Failure | Ruptured septal |
| 9. | 55 M | RCA | LAD | A2 B0 | Yes | Yes | Yes | Yes | Success | – |
| 10. | 57 M | RCA | LAD | A2 B0 | Yes | Yes | Yes | No | Failure | – |
| 11. | 59 M | RCA | LAD | A1 B0 | Yes | Yes | Yes | Yes | Success | – |
CTO, chronic total occlusion; CC, collateral channel; M, male; F, female; RCA, right coronary artery; LAD, left anterior descending artery; LCX, left circumflex artery.
Grade of technical difficulty (A0 low, A1 intermediate, A2 high) and risk (B0 low, B1 high) associated with attempted CTO recanalization based on the universal CTO classification system.8
Either microcatheter or balloon catheter.
Due to wire perforation related to anterograde recanalization attempts, treated successfully by pericardiocentesis alone.
Success was later achieved by re-attempting anterograde CTO recanalization.
3. Discussion
Availability of the CM opens up the retrograde CTO recanalization technique to the non-specialist operator like never before. This is borne out by the dramatic transformation in the success and complication rates of retrograde CTO recanalization obtained by the same operator in this study before and after the CM became available. Factors such as the small number of cases, the non-concurrent and non-randomized nature of comparison, and the operator's learning curve, may partially account for the differences seen, but they cannot entirely negate the remarkable change use of the CM has brought to retrograde CTO recanalization at our center.
In the hands of CTO-specialists, the CM produced significant improvement (from 92.5% to 98.9%) in the procedural success of retrograde CTO recanalization7; however the magnitude of improvement was not large because their success rate was already high, which is likely to be due to compensation for limitations in recanalization hardware with superior skills and strategies. Our experience suggests that the magnitude of increase in procedural success rate during retrograde CTO recanalization will be much greater among non-specialists who incorporate the CM into their CTO recanalization armamentarium. The use of intravascular ultrasound10 to guide retrograde CTO recanalization is likely to simplify the procedure and improve results further, as could incorporation of CT coronary angiography in case selection and planning; outcome differences between CTO-specialists and non-specialists may then narrow down even more. Additionally, these adjuncts and greater operator experience may reduce the long procedure and fluoroscopy times noted in the present study.
Clearly, larger experiences with the CM and results from multiple centers are needed before recommendations on changes in CTO strategy can be made. However, our results lead us to believe that with the availability of the CM, operators should spend less time on and be less aggressive with anterograde CTO recanalization attempts, and should switch to retrograde CTO recanalization with the CM earlier and more often, given the effectiveness and safety of the latter technique; this would improve the overall success rate and safety of CTO recanalization. It is likely that with wide availability of the CM in the future, the proportion of CTO cases treated percutaneously will increase significantly, and retrograde CTO recanalization will no longer remain largely within the domain of dedicated CTO-specialists.
Conflicts of interest
All authors have none to declare.
References
- 1.Stone G.W., Rutherford B.D., McConahay D.R. Procedural outcome of angioplasty for total coronary artery occlusion: an analysis of 971 lesions in 905 patients. J Am Coll Cardiol. 1990;15:849–856. doi: 10.1016/0735-1097(90)90285-w. [DOI] [PubMed] [Google Scholar]
- 2.Ivanhoe R.J., Weintraub W.S., Douglas J.S., Jr. Percutaneous transluminal coronary angioplasty of chronic total occlusions. Primary success, restenosis, and long-term clinical follow-up. Circulation. 1992;85:106–115. doi: 10.1161/01.cir.85.1.106. [DOI] [PubMed] [Google Scholar]
- 3.Kahn J.K., Hartzler G.O. Retrograde coronary angioplasty of isolated arterial segments through saphenous vein bypass grafts. Cathet Cardiovasc Diagn. 1990;20:88–93. doi: 10.1002/ccd.1810200205. [DOI] [PubMed] [Google Scholar]
- 4.Surmely J.F., Katoh O., Tsuchikane E. Coronary septal collaterals as an access for the retrograde approach in the percutaneous treatment of coronary chronic total occlusions. Catheter Cardiovasc Interv. 2007;69:826–832. doi: 10.1002/ccd.20816. [DOI] [PubMed] [Google Scholar]
- 5.Surmely J.F., Tsuchikane E., Katoh O. New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J Invasive Cardiol. 2006;18:334–338. [PubMed] [Google Scholar]
- 6.Asahi Corsair microcatheter: product information available at website <http://www.vascularperspectives.com>.
- 7.Tsuchikane E., Katoh O., Kimura M. The first clinical experience with a novel catheter for collateral channel tracking in retrograde approach for chronic coronary total occlusions. J Am Coll Cardiol Interv. 2010;3:165–171. doi: 10.1016/j.jcin.2009.10.026. [DOI] [PubMed] [Google Scholar]
- 8.Jayasinghe R., Paul V., Rajendran S. A universal classification system for chronic total occlusions. J Invasive Cardiol. 2008;20:302–304. [PubMed] [Google Scholar]
- 9.Saito S. Different strategies of retrograde approach in coronary angioplasty for chronic total occlusion. Catheter Cardiovasc Interv. 2008;71:8–19. doi: 10.1002/ccd.21316. [DOI] [PubMed] [Google Scholar]
- 10.Rathore S., Katoh O., Tuschikane E. A novel modification of the retrograde approach for the recanalization of chronic total occlusion of the coronary arteries – intravascular ultrasound-guided reverse controlled antegrade and retrograde tracking. J Am Coll Cardiol Intv. 2010;3:155–164. doi: 10.1016/j.jcin.2009.10.030. [DOI] [PubMed] [Google Scholar]


