Abstract
There are a handful of studies that have been done investigating the effect of music on various vital signs, namely systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR). Many studies have also assessed effects of music on self-reported anxiety level, attributing some degree of music-induced anxiety relief to the beneficial impacts of music on vital signs. Several randomised studies have shown varying effects of music on these vital parameters and so a metaanalysis was done to compare the effect of music on them. The fixed effects model was used as studies were homogenous. A two-sided alpha error < 0.05 was considered to be statistically significant. Compared to those who did not receive music therapy, those who did receive music therapy had a significantly greater decrease in SBP before and after (difference in means, −2.629, confidence interval (CI), −3.914 to −1.344, P < 0.001), a significantly greater decrease in DBP (difference in means, −1.112, CI, −1.692 to −0.532, P < 0.001), and a significantly greater decrease in HR (difference in means, −3.422, CI, −5.032 to −1.812, P < 0.001).
Keywords: Blood pressure, Diastolic, Heart rate, Music, Systolic
Introduction
The relaxing effects of music have been culturally accepted for centuries. Despite this, music has not given much attention in formal medical settings, where patients experience heightened levels of anxiety. While anxiety does not cause chronic hypertension (HTN), it can lead to acute elevations in blood pressure (BP) as may be noted with patients in a variety of medical settings; thus, BP and heart rate (HR) may be a result of anxiety in these settings. Studies have been conducted to assess the effect music therapy has on self-reported anxiety, BP, and HR. This meta-analysis was conducted to analyse results of conducted studies on systolic BP (SBP), diastolic BP (DBP), and HR, reductions in which seem to provide physical and mental relaxation in patients in a diverse range of healthcare settings.1
Methods
Literature sources, search terms, and study selection
A systematic review of medical literature was performed to obtain studies that assessed the effects of music on SBP, DBP, and HR. Studies were collected by two authors (Parinda H. Shah and Suraj Chandrasekar), independently, by searching MEDLINE and the Cochrane Library using web-based search engines such as OVID and PubMed. Search terms used include music, SBP, DBP, and HR. References of collected studies were used to conduct a hand search for additional trials, abstracts, and reviews. Inclusion and exclusion criteria were defined and agreed upon by all authors of the manuscript, with the authors collecting manuscripts using these criteria to determine inclusion potential. Study selection methodology is outlined in Figure 1.
Figure 1.
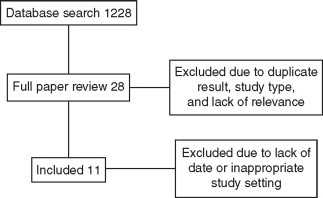
Study selection methodology.
End points and definitions
A total of three end points were extracted from 11 studies. Data from each end point was successfully obtained from each included study. End points extracted were SBP, DBP, and HR. End point definitions were matched, and data for end points was reported in similar fashion, among all included studies.
Data extraction and quality assessment
Manuscripts that were screened and thought to fulfill inclusion criteria were then collected in their entirety and scored against the developed criteria. Data was independently extracted and the methodology of each study was carefully reviewed and analysed in order to gauge whether or not it should be included. Conflicts between the two authors evaluating studies were addressed by all the authors.
Statistical analysis
Summary statistics from each study were used for the meta-analysis as individual patient data was not available. The difference between end points, before and after music therapy, was used with standard deviation (SD) for analysis. Statistical analysis was performed using the MedCalc Software Package (Version 11.3, Mariakerke, Belgium). Cochrane's Q statistics were calculated and used to determine the heterogeneity of the studies for each end point. All studies were homogenous for all end points and, thus, the fixed effects model was used for analysis (Table 1). A two-sided alpha error > 0.05 was considered to be statistically significant.
Table 1.
Test for heterogeneity results.
| Q value | df (Q) | P value | I-squared | ||
|---|---|---|---|---|---|
| Heart rate | 31.08 | 10 | 0.001 | 67.8 | Heterogenic |
| Systolic BP | 27.79 | 10 | 0.002 | 64.0 | Heterogenic |
| Diastolic BP | 11.13 | 10 | 0.348 | 10.1 | Homogenous |
BP: blood pressure.
Results
Baseline characteristics
The characteristics of each included trial are included in Table 2.2–12 Results of the meta-analysis are shown in Figures 2–4. It should be noted that some of the studies included only mechanically ventilated patients while others did not include any.
Table 2.
Baseline patient characteristics for included studies.
| Augustin et al. |
Buffum et al. |
Bun et al. |
Chan et al. 2010 |
Chan et al. 2007 |
Dijkstra et al. |
Han et al. |
Haun et al. |
Lai et al. |
Lee et al. |
Mok et al. |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| Type of study | Randomised | Randomised | Randomised | Randomised | Randomised | Randomised | Randomised | Randomised | Randomised | ||
| Age | |||||||||||
| Music | 47 | 67.01 ± 10.29 | 65.20 ± 10.15 | − | − | 47.2 ± 15.2 | 46.43 ± 15.45 | − | − | 70.6 + 15.1 | − |
| No Music | 47 | 66.65 ± 9.61 | 70.90 ± 6.49 | − | − | 57.2 ± 56.5 | 47.61 ± 13.47 | − | − | 68.3 ± 15.6 | − |
| Patient (n) | |||||||||||
| Music | 21 | 89 | 10 | 21 | 31 | 8 | 44 | 10 | 22 | 32 | 40 |
| No Music | 21 | 81 | 10 | 21 | 35 | 10 | 49 | 10 | 22 | 32 | 40 |
| Setting | Ambulatory surgery clinic | Before vascular angiography | Before transuretheral prostate resection | Community centre | ICU | ICU, mechanical vent | ICU, mechanical vent | Women before breast biopsy | During root canal | ICU, mechanical vent | Minor surgery with local anaesthesia |
| Average baseline HR | |||||||||||
| Music | 72.2 ± 12.00 | 67.04 ± 11.11 | 71.90 ± 12.92 | 78.2 ± 13.6 | 72.6 ± 14.3 | 107 ± 22.6 | 96.98 ± 15.93 | 78.4 ± 17.9 | 77.23 ± 6.65 | 98.5 + 18.2 | 82.50 ± 10.05 |
| No music | 71.1 ± 10.70 | 69.01 ± 12.49 | 77.70 ± 10.30 | 71.0 ± 8.5 | 77.0 ± 10.8 | 90 ± 14.0 | 93.20 ± 15.49 | 81.2 ± 10.5 | 81.41 ± 7.45 | 97.8 + 21.9 | 80.83 ± 4.95 |
| Average baseline SBP | |||||||||||
| Music | 129.6 ± 16.09 | 142.53 ± 26.52 | 135.80 ± 19.55 | 143.6 ± 18.5 | 143.6 ± 23.9 | 117 ± 16.8 | 119.77 ± 18.39 | 123.7 + 16.3 | 135.73 ± 11.83 | 133.6 ± 26.6 | 125.35 + 15.33 |
| No music | 135.4 ± 13.33 | 137.81 ± 22.02 | 132.30 ± 17.79 | 137.7 ± 15.2 | 143.6 ± 23.4 | 107 ± 23.9 | 116.78 + 16.25 | 122.3 + 12.8 | 136.00 ± 12.78 | 129.0 ± 22.2 | 127.53 ± 10.27 |
| Average baseline DBP | |||||||||||
| Music | 83.1 ± 13.12 | 76.71 ± 14.17 | 79.40 ± 11.63 | 82.1 ± 11.0 | 71.7 ± 11.8 | 62 ± 11.1 | 70.61 ± 12.39 | 69.1 ± 10.5 | 84.14 ± 7.86 | 61.3 ± 12.8 | 74.82 ± 12.80 |
| No music | 84.1 ± 11.47 | 75.30 ± 9.94 | 81.00 ± 10.71 | 80.4 ± 8.3 | 73.1 ± 11.6 | 54 ± 7.6 | 68.02 ± 12.74 | 72.3 ± 12.1 | 84.91 ± 9.54 | 61.2 ± 12.5 | 76.05 ± 8.27 |
| Length of intervention (min) | 15–30 | 15 | 20 | 30 | 45 | 30 | 30 | 20 | − | 30 | − |
DBP: diastolic blood pressure, HR: heart rate, ICU: intensive care unit, SBP: systolic blood pressure.
Figure 2.
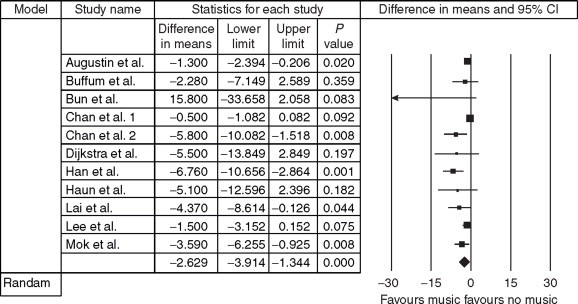
Forest plot for effect of music on systolic blood pressure. CI: confidence interval.
Figure 3.
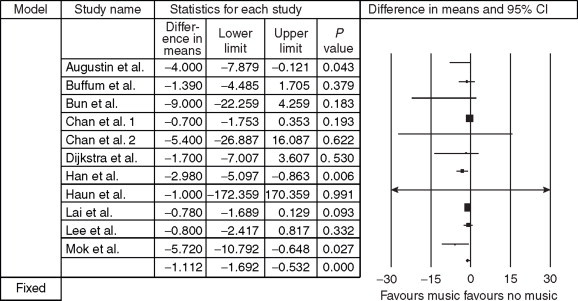
Forest plot for effect of music on diastolic blood pressure. CI: confidence interval.
Figure 4.
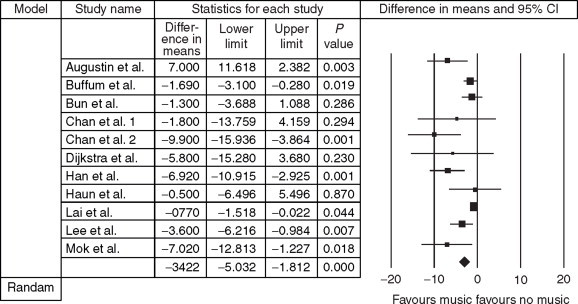
Forest plot for effect of music on heart rate. CI: confidence interval.
Systolic blood pressure
The difference in means for SBP showed a greater decrease in the group receiving music therapy (difference in means, –2.629; confidence interval (CI), –3.914 to –1.344; P > 0.001).
Diastolic blood pressure
The difference in means for DBP also showed a greater decrease in the group receiving music therapy (difference in means, –2.629; CI, –3.914 to –1.344; P > 0.001).
Heart rate
Greater decrease in difference of means was also noted for HR in the group receiving music therapy (difference in means, –2.629; CI, –3.914 to –1.344; P > 0.001).
Discussion
This meta-analysis demonstrates that music therapy leads to a significantly greater reduction in SBP, DBP, and HR in a variety of clinical settings. These findings were different from findings by Evans in an earlier analysis of 102 pooled patients.13 Our meta-analysis consisted of 331 patients not receiving music therapy and 328 patients who did. Three of the studies included in this analysis were in a pre-operative setting, four were in an intensive care unit (ICU) setting, two were in an intra-operative setting, one before vascular angiography, and one in a community centre care facility. Of the four studies done in ICUs, three studied the effects of music on mechanically ventilated patients. Similar findings were noted in all these settings although it should be noted that the reduction in BP and HR was greater in patients that were mechanically ventilated. Reduction in BP and HR serves to relax patients both physiologically and mentally, leading to, or representing, a reduction in anxiety.1
The pre-operative setting is one often filled with anxiety. With 53.5 million surgical procedures performed during 34.7 million ambulatory surgery visits in the United States in 2006,14 the ambulatory surgery setting must be given proper attention along with the inpatient surgical setting. Patients awaiting even minor surgical procedures can experience significant levels of anxiety which can affect postoperative recovery and increase risk of physiological complications.15 Patients may spend a significant amount of time in a surgical holding area before their procedure, a potentially overwhelming experience due to unfamiliar sights and sounds.16 Reduction in a patient's pre-operative anxiety can lead to decreased postoperative vomiting, pain, and recovery time.17 For inpatient surgeries, proper reduction of pre-operative anxiety can also lead to lower hospital length of stay, postoperative fever, and need for analgesia and sedation.18 Additionally, anxiety can have intra-operative effects as an anxious patient may not be as co-operative in the operating room, leading to the need for increased sedation as well as technical difficulties.19
The ICU is another setting of particular interest for the utility of music therapy. Patients in the ICU receiving mechanical ventilation have been studied. Inability to verbally communicate, difficulty breathing, frequent suctioning, and concern for their current condition, are all causes of increased anxiety in ventilated patients.20 This, along with increased in morbidity and mortality in critically ill patients with higher anxiety levels, makes studying the effects of music in these patients of potentially more value than in other subgroups.21 Analysis of included studies seems to indicate that music may have increased effects on reduction of SBP, DBP, and HR in those who are mechanically ventilated.
There is a need for larger randomised controlled trials exploring music as an intervention to reduce physiological parameters such as BP and HR, and subsequently anxiety. Future studies, ideally, should have large patient number and focus on an individual healthcare setting. Different kinds of music should be studied, including patient-selected music.22 Optimal length of music therapy as well as timing relative to procedures also still remains to be established. Larger patient numbers will also allow for subgroup analysis by factors such as age, gender, ethnicity, and diagnosis.
Limitations of included studies include small sample sizes, lack of analysis of effect of ethnicity on results, and lack of analysis of other factors that can alter anxiety levels such as presence of family.
Limitations of the study include those of all meta-analyses such as the pooling of data from studies with different designs. Pooled patient characteristics are similar but not exactly the same, introducing obstacles to interpretation of results.
Conclusion
There remains a need for larger randomised studies that allow for analysis of specific factors but it appears that music has beneficial effects in the reduction of SBP, DBP, and HR in a variety of clinical settings such as the pre-operative setting and the ICU. These physiological changes may be the result of and/or aid in the relief of patient anxiety.
References
- 1.Wiklund I, Halling K, Ryden-Bergsten T. Does lowering the blood pressure improve the mood? Quality of life results from the hypertension optimal treatment study. Informa Healthcare. 1997;6:357–364. doi: 10.3109/08037059709062095. [DOI] [PubMed] [Google Scholar]
- 2.Augustin P, Hains A. Effect of music on ambulatory surgery patients' preoperative anxiety. AORN. 1996;63:750–758. doi: 10.1016/s0001-2092(06)63126-8. [DOI] [PubMed] [Google Scholar]
- 3.Buffum M, Sasso C, Sands L. A music intervention to reduce anxiety before vascular angiography procedures. J Vasc Nurs. 2006;24:68–73. doi: 10.1016/j.jvn.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Yung P, Chui-Kam S, Chan T. A controlled trial of music and preoperative anxiety in Chinese men undergoing transurethral resection of the prostate. J Adv Nurs. 2002;39:352–359. doi: 10.1046/j.1365-2648.2002.02296.x. [DOI] [PubMed] [Google Scholar]
- 5.Chan MF. Effects of music on patients undergoing a C-clamp procedure after percutaneous coronary interventions: a randomized controlled trial. Heart Lung. 2007;36:431–439. doi: 10.1016/j.hrtlng.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Chan MF, Chan E, Mok E. Effects of music on depression and sleep quality in elderly people: a randomised controlled trial. Complement Ther Med. 2010;18:150–159. doi: 10.1016/j.ctim.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 7.Dijkstra B, Gamel C, Bijil J. The effects of music on physiological responses and sedation scores in sedated, mechanically ventilated patients. JCN. 2010;19:1030–1039. doi: 10.1111/j.1365-2702.2009.02968.x. [DOI] [PubMed] [Google Scholar]
- 8.Han L, Li J, Sit J. Effects of music intervention on physiological stress response and anxiety level of mechanically ventilated patients in China: a randomised controlled trial. JCN. 2008;19:978–987. doi: 10.1111/j.1365-2702.2009.02845.x. [DOI] [PubMed] [Google Scholar]
- 9.Haun M, Mainous R, Looney S. Effect of music on anxiety of women awaiting breast biopsy. Music Anxiety. 2001;27:127–132. doi: 10.1080/08964280109595779. [DOI] [PubMed] [Google Scholar]
- 10.Lai H, Hwang M, Chen C. Randomized controlled trial of music on state anziety and physiological indices in patients undergoing root canal treatment. JCN. 2008;17:2654–2660. doi: 10.1111/j.1365-2702.2008.02350.x. [DOI] [PubMed] [Google Scholar]
- 11.Lee O, Chung Y, Chan M. Music and its effect on the physiological responses and anxiety levels of patients receiving mechanical ventilation: a pilot study. JCN. 2004;14:609–620. doi: 10.1111/j.1365-2702.2004.01103.x. [DOI] [PubMed] [Google Scholar]
- 12.Mok E, Wong KY. Effects of music on patient anxiety. AORN J. 2003;77:396–410. doi: 10.1016/s0001-2092(06)61207-6. [DOI] [PubMed] [Google Scholar]
- 13.Evans D. The effectiveness of music as an intervention for hospital patients: a systematic review. J Adv Nurs. 2002;337:8–18. doi: 10.1046/j.1365-2648.2002.02052.x. [DOI] [PubMed] [Google Scholar]
- 14.Cullen K, Hall M, Golosinskiy A. Ambulatory surgery in the United States, 2006. National Health Statistics Reports 2009;11. [PubMed]
- 15.Swindale JE. The nurse's role in giving preoperative information to reduce anxiety in patients admitted to hospitals for elective minor surgery. J Adv Nurs. 1989;14:899–905. doi: 10.1111/j.1365-2648.1989.tb01478.x. [DOI] [PubMed] [Google Scholar]
- 16.Cirina C. Effects of sedative music on patient preoperative anxiety. Today's OR Nurse. 1994;16:15–18. [PubMed] [Google Scholar]
- 17.Orr D. Preoperative teaching: reducing presurgial anxiety. Can Oper Room Nurs J. 1986;4:29–31. [PubMed] [Google Scholar]
- 18.Hathway D. Effect of preoperative instruction on postoperative outcomes: a meta-analysis. Nurs Res. 1986;35:269–275. [PubMed] [Google Scholar]
- 19.Warner C, Peebles B, Miller J. The effectiveness of teaching a relaxation technique to patients undergoing elective cardiac catheterization. J Cardiovasc Nurs. 1992;6:66–75. [PubMed] [Google Scholar]
- 20.Wong HL, Lopez-Nahas V, Malassiotis A. Effects of music therapy on anxiety in ventilator dependent patients. Heart Lung. 2001;30:376–387. doi: 10.1067/mhl.2001.118302. [DOI] [PubMed] [Google Scholar]
- 21.Moser DK, Dracup K. Is anxiety early after myocardial infarction associated with subsequent ischemic and arrhythmic events? Psychosom Med. 1996;58:395–401. doi: 10.1097/00006842-199609000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Stevens K. Patients' perceptions of music during pregnancy. J Adv Nurs. 1990;15:1045–1051. doi: 10.1111/j.1365-2648.1990.tb01985.x. [DOI] [PubMed] [Google Scholar]


