Abstract
In Indian settings pulmonary tuberculosis remains the most common diagnosis in a patient presenting with constitutional symptoms, hemoptysis and lung opacities. We describe a case report of a fifty-year-old woman who was receiving empirical anti-tubercular drugs for a metastatic illness to lungs arising from a primary angiosarcoma in the right atrium. This rare entity was misdiagnosed and typical echocardiographic findings suggested this diagnosis.
Keywords: Cardiac angiosarcoma, Right atrium, Tuberculosis, Lung metastases
1. Introduction
Malignant primary cardiac tumors contribute to 25% of the cardiac tumors with one third of these being angiosarcoma.1 The angiosarcoma arises from the right atrial wall in two third of the cases and has a poor outlook with survival ranging from 3 to 9 months irrespective of the treatment. It is seen more commonly in males between the third and fifth decade of life.2 The diagnosis is difficult and usually late as there are no specific symptoms. We present a case of primary cardiac angiosarcoma causing right atrial rupture in which echocardiography suggested the diagnosis.
2. Case report
The patient was a fifty-year-old female who presented to the satellite hospital with complaints of hemoptysis and low-grade fever for the past 1 month. The patient also gave history of significant weight loss and decreased appetite over the previous few months. Chest X-ray showed nodular opacities in both lung fields with right-sided pleural effusion while sputum examination was negative for acid fast bacilli (Fig. 1). The patient treatment was started empirically on four drug Anti-tubercular drug regimen, category 1 treatment. However over the next 2 months her condition deteriorated and she developed progressive breathlessness and pedal edema with further episodes of hemoptysis. A cardiac referral was sought from our centre for the above complaints.
Fig. 1.

Chest X-ray reveals right-sided pleural effusion with multiple nodular opacities in both lung fields. Consolidation of right middle lobe also noted silhouetting right heart border.
On general physical examination, the patient was anemic with engorged jugular vein and bilateral pedal edema. Her heart rate was 100/min, blood pressure 94/60 mmHg, with cold and clammy extremities. Cardiovascular examination revealed soft heart sounds without any audible murmur. Her hemoglobin was low (9.0 g/dL), white cell count was 10,400/mm3 and platelet count was 98,000/mm3. Other biochemical investigations were within normal limits. The echocardiogram showed a large mobile, non pedunculated mass arising from the right atrial free wall, not involving the septum, with loculated pericardial effusion against the right atrium and right ventricle Fig. 2(A). An atrio-pericardial fistula was suspected and subsequent contrast echo with saline bubbles confirmed the finding with a blood flow between right atrium and effusion Fig. 2(B). Hepatic sinusoids and inferior vena cava was dilated. Liver, Inferior vena cava, Right ventricle, Pulmonary artery and left chambers were tumor free. CT-chest done on the same day revealed multiple secondary metastases in both lungs besides showing the atrio-pericardial fistula and papillary like tumor mass projecting from the right atrial wall Fig. 3(A) and (B). Due to her poor general condition and metastatic pulmonary illness any surgical intervention was refused and the patient was kept on conservative treatment. The patient received two units of blood transfusion but she continued to have hemoptysis. Her condition deteriorated over the next 2 days and she was put on ventilatory support and vasoactive drugs but eventually the patient expired on third day.
Fig. 2.
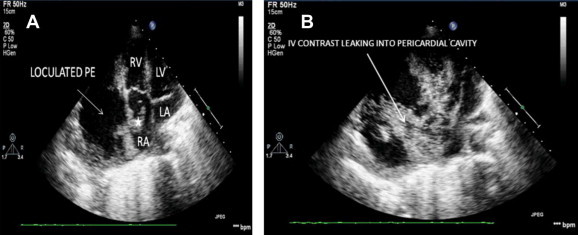
(A) Apical 4c view showing friable looking sessile, mobile mass (✰) arising from right atrial wall and a large loculated effusion around right atria and ventricle. (B) Apical 4c view showing leakage of saline bubble contrast (white arrow) from right atrial free wall to surrounding pericardial effusion thus confirming atrio-pericardial fistula.
Fig. 3.
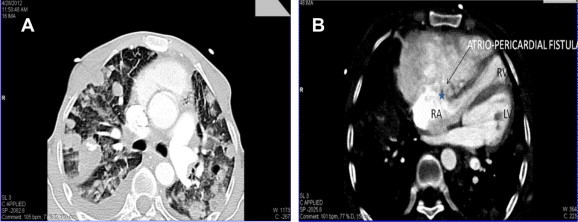
(A) Axial CT reveals multiple non cavitating nodular lesions of varying sizes scattered in bilateral lung parenchyma in angiocentric distribution suggesting metastatic deposits. Bilateral pleural effusion (R > L) is also seen. (B) Contrast enhanced axial CT reveals pericardial collection communicating with right atria and causing attenuation of the right ventricle. Associated papillary like projection (*) noted in the free wall of the right atria.
On autopsy 850 ml of haemorrhagic pericardial fluid was removed. There was Bilateral pleural effusion (right > left) with 200 ml of pleural fluid that was hemorrhagic in its gross appearance. There were no were no malignant or atypical cells in pleural/pericardial fluid. There was a friable, vascular tumor on the lateral surface of the right atrium. Both lungs were diffusely studded by multiple nodular metastases. No metastasis was found to any other organ. Histological examination of the mass and tumor metastases showed multiple anastomosing vascular channels lined with malignant endothelial cells, indicative of angiosarcoma.
3. Discussion
Angiosarcoma is the most common malignant tumor of the heart that shows rapid growth, local invasion, and distant metastasis. Its clinical presentation is variable and metastases are present in 66–89% at the time of diagnosis with Lung metastasis being the most common site.3 Cardiac rupture due to angiosarcoma is extremely rare; few cases all involving the right atrium, have been reported in the literature.4–6 Other multivaried presentations of cardiac angiosarcoma that have been reported include presentation as recurrent pulmonary embolism,7 difficult to treat bilateral pleural effusion,8 collapse of the lung,9 and as coronary artery pseudo aneurysm.10
In our patient bilateral nodular lung infiltration with right-sided pleural effusion and constitutional symptoms led to the initiation of empirical treatment with anti-tubercular treatment (a common diagnosis in our country) and a cardiac referral suggested the rare diagnosis. Recently Fiorelli et al11 also reported similar scenario when the patient scheduled for thorascopic lung biopsy for nodular lung lesion was incidentally detected as having cardiac angiosarcoma on echocardiography during pre operative work up.
Echocardiography is a readily available non-diagnostic tool to detect these tumors and a screening test in patients with varied presentations can aid to make a proper diagnosis. Meng et al12 reported that the sensitivities of transthoracic echocardiogram (TTE) and transesophageal echocardiogram to detect these primary masses are 93% and 97%, respectively. On the other hand, magnetic resonance imaging (MRI) currently appears to be the imaging modality of choice in the assessment of a patient with known cardiac mass.13
Treatment of angiosarcoma is controversial due to the poor prognosis. Surgical resection is indicated when no evidence of metastasis exists and when myocardial resection is reparative. Chemotherapy and radiation therapy may be indicated as adjuvant or preferential therapies, but their use is usually limited due to the poor physical condition of the patient.14 Orthotopic Heart transplantation can allow complete resection of cardiac tumors but has high risk of tumor recurrence or metastasis and the possible enhancement of tumor growth by immunosuppressive drugs.15
4. Conclusion
This case highlights the need for awareness among the clinicians and avoiding misdiagnosis with tuberculosis especially in the Indian setting. Characteristics that favor a malignant cardiac tumor on echocardiography include lack of a pedicle, right atrial location and invasive growth pattern. A haemorrhagic effusion, invasive tumor mass in right atrium and non-cavitatory lung infiltrates should alert about the possibility of this rare condition.
Conflicts of interest
All authors have none to declare.
References
- 1.Burke A.P., Cowan D., Virmani R. Primary sarcomas of the heart. Cancer. 1992;69:387–395. doi: 10.1002/1097-0142(19920115)69:2<387::aid-cncr2820690219>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 2.Herrmann M.A., Shankerman R.A., Edwards W.D. Primary cardiac angiosarcoma: a clinicopathologic study of six cases. J. Thorac Cardiovasc Surg. 1992;103(4):655–664. [PubMed] [Google Scholar]
- 3.Chul H.K., Jane Y.D., Donna C. Clinicopathologic study of 24 patients with primary cardiac sarcomas: a 10-year single institution experience. Hum Pathol. 2008;39:933–938. doi: 10.1016/j.humpath.2007.12.018. [DOI] [PubMed] [Google Scholar]
- 4.Corso R.B., Kraychete N., Nardeli S. Spontaneous rupture of a right atrial angiosarcoma and cardiac tamponade. Arq Bras Cardiol. 2003;81:611–613. doi: 10.1590/s0066-782x2003001400008. [DOI] [PubMed] [Google Scholar]
- 5.Sakaguchi M., Minato N., Katayama Y. Cardiac angiosarcoma with right atrial perforation and cardiac tamponade. Ann Thorac Cardiovasc Surg. 2006 Apr;12(2):145–148. [PubMed] [Google Scholar]
- 6.Satou Y., Nakagawa Y., Miki H. Cardiac angiosarcoma with ruptured right atrium diagnosed by echocardiography. Chest. 1991;100:274–275. doi: 10.1378/chest.100.1.274. [DOI] [PubMed] [Google Scholar]
- 7.O'Callaghan D.S., Breen D.P., Young V. Angiosarcoma of the right atrium masquerading as recurrent pulmonary embolism. Thorac Cardiovasc Surg. 2008 Dec;56(8):488–490. doi: 10.1055/s-2007-989292. [DOI] [PubMed] [Google Scholar]
- 8.Uto T., Bando M., Yamauchi H. Primary cardiac angiosarcoma of the right auricle with difficult-to-treat bilateral pleural effusion. Intern Med. 2011;50(20):2371–2374. doi: 10.2169/internalmedicine.50.5751. [DOI] [PubMed] [Google Scholar]
- 9.Van der Lee C., Klootwijk P.J., van Geuns R.J. Angiosarcoma of the right atrium presenting as collapse. Int J Cardiol. 2009 Feb 6;132(1):e17–e19. doi: 10.1016/j.ijcard.2007.07.100. [DOI] [PubMed] [Google Scholar]
- 10.Chaturvedi A., Vummidi D., Shuman W.P. Cardiac angiosarcoma: an unusual cause of coronary artery pseudoaneurysm. J Thorac Imaging. 2012 Jan;27(1):W8–W9. doi: 10.1097/RTI.0b013e3182078187. [DOI] [PubMed] [Google Scholar]
- 11.Fiorelli A., Vicidomini G., Palladino A. Bilateral lung lesions: when the eyes deceive the brain! Ann Ital Chir. 2012 Mar–Apr;83(2):87–89. [PubMed] [Google Scholar]
- 12.Meng Q., Lai H., Lima J. Echocardiographic and pathologic characteristics of primary cardiac tumor; a study of 149 patients. Int J Cardiol. 2002;84:69–75. doi: 10.1016/s0167-5273(02)00136-5. [DOI] [PubMed] [Google Scholar]
- 13.Mader M.T., Poulton T.B., White R.D. Malignant tumors of the heart and great vessels: MR imaging appearance. Radiographics. 1997;17:145–153. doi: 10.1148/radiographics.17.1.9017805. [DOI] [PubMed] [Google Scholar]
- 14.Simpson L., Kumar S.K., Okuno S.H. Malignant primary cardiac tumors: review of a single institution experience. Cancer. 2008;112:2440–2446. doi: 10.1002/cncr.23459. [DOI] [PubMed] [Google Scholar]
- 15.Michler R.E., Goldstein D.J. Treatment of cardiac tumors by orthotopic cardiac transplantation. Semin Oncol. 1997;24(5):534–539. [PubMed] [Google Scholar]


