Highlights
► Intravenous leiomyomatosis is histologically benign, but biologically aggressive. ► No diagnostic tools reliably distinguish it from leiomyosarcoma prior to surgery. ► Complete resection is curative, but antiestrogens can stabilize disease.
Keywords: Intracardiac tumor, Intravascular leiomyomatosis, Pelvic mass, Venous thrombi
Introduction
Intravenous leiomyomatosis (IVL) is a rare, histologically benign but biologically aggressive tumor. It should be considered in patients with a history of uterine fibroids or a pelvic mass accompanied by right atrial tumor, right heart dysfunction, Budd–Chiari syndrome, or deep vein thrombosis (Anselmi et al., 2010). Surgical resection is curative if complete resection is achieved. Unique features of our case include the gonadal vein origin of the leiomyomas, the extensive nature of tumor related venous thrombi, and severe intraoperative coagulopathy resulting in the use of a staged procedure for tumor resection.
Case report
The patient is a 44 year-old gravida 5, para 5 who presented with a history of dyspnea and lower extremity edema. Physical exam findings included sinus tachycardia, an oxygen saturation of 93% on room air, and severe lower extremity edema. Chest X-ray showed pulmonary edema. Lower extremity Doppler showed left sided deep venous thrombi. Computed tomography (CT) demonstrated a solid, 10 cm mass involving the right uterine cornua and extending into the right gonadal vein, inferior vena cava (IVC), and right atrium (see Fig. 1). No peritoneal nodularity or retroperitoneal adenopathy was noted. CT angiogram detected extensive thrombus in the left common femoral, renal, and hepatic veins, inferior vena cava, and right atrium, also a large pulmonary artery thrombus. Magnetic resonance imaging (MRI) confirmed these findings (see Figs. 2 and 3). Echocardiogram demonstrated an ejection fraction of 66% and a 3 cm mass in the right atrium extending from the IVC.
Fig. 1.
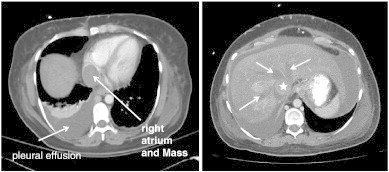
Left: Large right pleural effusion, solid mass in the right atrium. Right: Thrombosis of the hepatic veins, signs of liver congestion, and enhancing solid mass is shown in the intrahepatic inferior vena cava.
Fig. 2.
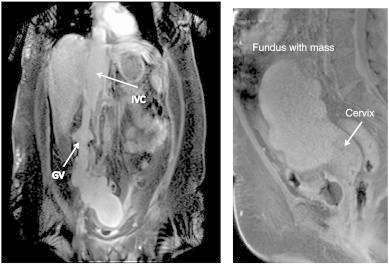
Left: Large exophytic mass arising from superior, lateral aspect of the uterus growing superiorly into the right gonadal vein and IVC. Right: Large enhancing exophytic mass arising from superior aspect of uterus.
Fig. 3.
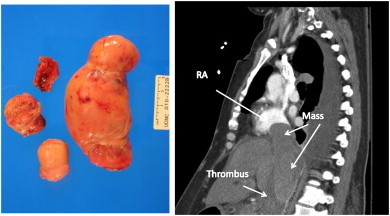
Portions of inferior vena cava tumor correspond to area of the inferior vena cava mass on pre-operative CT scan. Gross specimen on left measures 6 × 3 × 4 cm.
Initial treatment included percutaneous thrombectomy and streptokinase thrombolysis, followed by intravenous heparin for treatment of the extensive thrombi. Subsequently this was converted to lepirudin after the patient developed heparin induced thrombocytopenia.
A CT guided core needle biopsy demonstrated whorled fascicles of uniform smooth muscle cells without cellular atypia, mitosis, or necrosis. There was no evidence of malignancy, yet the sample was not sufficient to allow for a definitive pathologic diagnosis. Given the extent of the disease and the uncertain pathology, the ability to achieve surgical cure was unclear. However during the course of our workup, the patient's hemodynamic status began to deteriorate, resulting in symptoms of severe pulmonary edema and hypotension due to cardiogenic shock. Therefore the decision was made by gynecologic oncology, vascular, and cardiothoracic surgery, to attempt complete resection of the mass and venous thrombi which was accomplished in a two-staged procedure.
First intra-atrial and perihepatic IVC tumor extraction was performed via a median sternotomy and midline laparotomy. After complete dissection of the infrahepatic IVC tumor, including the bilateral gonadal veins, right heart bypass was initiated and the intra-atrial portion of the tumor was removed. Adherence of the tumor to the cardiac and caval walls resulted in a prolonged and difficult resection with significant blood loss. The combination of prolonged operating time, hemorrhage, hypovolemia and hepatic dysfunction subsequently lead to significant coagulopathy. This was managed with massive transfusion of blood products and packing of the abdominal and retroperitoneal cavity. Given the patient's hemodynamic instability, total abdominal hysterectomy and bilateral salpingooophorectomy was delayed for 48 h, during which time final pathology of the intracardiac mass revealed benign leiomyoma (see Fig. 3). At the second operation, findings included multiple uterine leiomyoma with extension into the right cornua and right gonadal vein. The patient recovered well from her surgery and given the benign final pathology and the completeness of her resection, no further adjuvant therapy was indicated.
Comment
Intravascular leiomyomatosis is a rare tumor characterized by nodular masses of histologically benign smooth muscle growing within veins. It may arise from the uterus, ovaries, or kidneys (Anselmi et al., 2010). It usually spreads through the uterine or ovarian veins, and can progress into the caval vein and right heart (Nam et al., 2003). There are two main theories about the etiology of these tumors (Norris and Parmley, 1975). The first is that the tumor arises from the vein walls. The second is that the primary uterine leiomyoma spreads into adjacent venous structures by direct extension.
The most common presenting symptom among reported cases is shortness of breath and dyspnea on exertion, though pelvic pain and abnormal uterine bleeding was also sometimes noted. Other common symptoms include pleuritic chest pain, pedal edema, abdominal distension, or syncope (Nam et al., 2003). The tumor can be misdiagnosed as thrombus or primary cardiac tumor such as a myxoma. Imaging such as echocardiography, chest and abdominal CT and MRI should be performed pre-operatively to determine the extent of the disease (Nam et al., 2003).
Distinguishing between intravascular leiomyoma and leiomyosarcoma can be challenging. There have been three reports of leiomyosarcoma in the literature with a similar clinical presentation (Coard and Fletcher, 2002; McDonald et al., 2007; Moorjani et al., 2005). All three cases were also associated with tumor emboli and venous thromboembolism. No signs or symptoms, tumor markers, or imaging could reliably differentiate between the two entities. The diagnosis of each is based on histological findings. Leiomyosarcoma is defined by coagulative tumor necrosis, severe cytological atypia, and greater than 10 mitotic figures per 10 high power fields. However, even with these clear definitions, sampling error can confound the results of any histological analysis. Therefore only a large tissue sample can conclusively exclude the diagnosis of malignancy. While the accuracy of CT guided biopsy for the diagnosis of abdominal masses is on the order of 90% (Steil et al., 2009), in the case of leiomyosarcoma, sampling error and the rarity of the disease decrease this test's negative predictive value substantially. In our case, CT guided biopsy was requested by a co-consulting service. Though the biopsy and final surgical pathology proved to be concordant, as a general rule, differentiating leiomyoma from leiomyosarcoma must be done using a large specimen to overcome the problem of sampling error. Therefore core needle biopsy plays little role in establishing a pre-operative diagnosis.
Complete resection is curative, therefore every effort should be made to achieve this. Complete resection can be accomplished via a two stage procedure involving resection of the abdominal/pelvic and intrathoracic components in two separate operations, or in a single-stage operation using cardiopulmonary or right heart bypass. Our case was done in two stages due to the complications of coagulopathy and hemorrhage during the intrathoracic portion of the procedure. Our patient's presentation with extensive venous thrombi requiring anticoagulation prior to surgery further complicated her care and to our knowledge has not been reported elsewhere.
In cases of incomplete resection or tumor recurrence, use of antiestrogens such as tamoxifen has been considered but their efficacy remains controversial (Nam et al., 2003). Animal models for uterine leiomyoma have provided valuable preclinical evidence for the usefulness of SERMs. Palomba et al. investigated the effects of raloxifene in postmenopausal women with uterine leiomyoma and found that tumor size was significantly reduced after 12 months of treatment, with relatively few side effects (Palomba et al., 2001; Palomba et al., 2002). Recurrence rates as high as 30% have been reported following incomplete resection (Ahmed et al., 2004), and can occur as early as 6 months and as late as 15 years after initial presentation (Anselmi et al., 2010). A standard follow up regimen has yet to be established.
In summary, intravenous leiomyomatosis is a rare, histologically benign, but biologically aggressive tumor. There are no diagnostic tools that can reliably distinguish it from leiomyosarcoma prior to surgery. Complete resection is curative, but antiestrogens have also been shown to stabilize and decrease tumor burden when surgical resection cannot be achieved.
Conflict of interest statement
None of the authors have a conflict of interest.
References
- Ahmed M., Zangos S., Bechstein W.O. Intravenous leiomyomatosis. Eur. Radiol. 2004;14:1316–1317. doi: 10.1007/s00330-003-2186-z. [DOI] [PubMed] [Google Scholar]
- Anselmi A., Tsiopoulos V., Perri G. Case series of resection of pelvic leiomyoma extending into the right heart: surgical safeguards and clinical follow-up. J. Cardiovasc. Med. 2010;11:583–586. doi: 10.2459/JCM.0b013e328337d856. [DOI] [PubMed] [Google Scholar]
- Coard K.C.M., Fletcher H.M. Leiomyosarcoma of the uterus with a florid intravascular component. Int. Soc. Gynecol. Pathol. 2002;21:182–185. doi: 10.1097/00004347-200204000-00012. [DOI] [PubMed] [Google Scholar]
- McDonald D.K., Kalva S.P., Fan C.M. Leiomyosarcoma of the uterus with intravascular tumor extension and pulmonary tumor embolism. Cardiovasc. Intervent. Radiol. 2007;30:140–142. doi: 10.1007/s00270-006-0118-4. [DOI] [PubMed] [Google Scholar]
- Moorjani N., Kuo J., Ashley S. Intravenous uterine leiomyosarcomatosis with intracardial extension. J. Card. Surg. 2005;20:382–385. doi: 10.1111/j.1540-8191.2005.200476.x. [DOI] [PubMed] [Google Scholar]
- Nam M.S., Jeon M.J., Kim Y.T. Pelvic leiomyomatosis with intracaval and intracardiac extension: a case report and review of the literature. Gynecol. Oncol. 2003;89:175–180. doi: 10.1016/s0090-8258(02)00138-5. [DOI] [PubMed] [Google Scholar]
- Norris H.J., Parmley T. Mesenchymal tumors of the uterus v intravenous leiomyomatosis: a clinical and pathological study of 14 cases. Cancer. 1975;36:2164–2178. doi: 10.1002/cncr.2820360935. [DOI] [PubMed] [Google Scholar]
- Palomba S., Sammartino A., Di Carlo C. Effects of raloxifene treatment on uterine leiomyomas in postmenopausal women. Fertil. Steril. 2001;76:38–43. doi: 10.1016/s0015-0282(01)01849-0. [DOI] [PubMed] [Google Scholar]
- Palomba S., Russo T., Orio F. Effectiveness of combined GnRH analogue plus raloxifene administration in the treatment of uterine leiomyomas: a prospective, randomized, single-blind, placebo-controlled clinical trial. Hum. Reprod. 2002;17:3213–3219. doi: 10.1093/humrep/17.12.3213. [DOI] [PubMed] [Google Scholar]
- Steil S., Zerwas S., Moos G. CT-guided percutaneous core needle biopsy in oncology outpatients: sensitivity, specificity, complications. Onkologie. 2009;32:254–258. doi: 10.1159/000209966. [DOI] [PubMed] [Google Scholar]


