Abstract
Unconventional sites are being used for pacing in patients with inaccessible right ventricle like single ventricle, atresia of tricuspid valve and in anomalous venous drainage. Here we report a case in which the right ventricle could not be accessed due to the metallic prosthesis. A 41-year-old lady required triple valve replacement for rheumatic involvement. Permanent pacemaker implantation was done with epicardial lead for bradycardia post operatively. Pulse generator change was needed within 3 years as the pacemaker reached end of life due to high lead threshold. Subsequent pacemaker implantation was done with a left ventricular lead in coronary sinus by percutaneous approach. One year after implantation, the threshold remains stable. Coronary sinus can be utilized for permanent pacing in patients with inaccessible right ventricle due to prosthetic tricuspid valve.
Keywords: Tricuspid prosthesis, Inaccessible right ventricle, Permanent pacing
1. Introduction
Trans venous right ventricular endocardial lead placement is the routine practice in clinical pacing. Inaccessibility of right ventricle mandates search for other sites in certain clinical situations. Epicardial pacemaker lead implantation is usually associated with development of high threshold and requires limited thoracotomy.1 Coronary sinus (CS) pacing was reported after Fontan operation, univentricular heart and in other conditions.2–4 There are reports of incidental placement of lead in coronary sinus due to anomalous venous drainage.5 Herre et al reported CS pacing in a patient with metallic prosthetic valve in tricuspid position.6 Organic tricuspid valve diseases requiring repair or replacement make the right ventricle inaccessible and tricuspid valve surgery often leads to heart block requiring permanent pacemaker implantation. Mechanical prosthesis in tricuspid position in our patient made the right ventricle inaccessible hence required lead placement in CS.
2. Case report
A 41-year-old lady with established rheumatic valvular heart disease had undergone percutaneous transmitral commissurotomy. Four years later she underwent aortic and mitral balloon valvuloplasty for the worsening of valve lesions. Secondary to the atrial fibrillation she had embolic occlusion of the right femoral artery in the same year which was managed by embolectomy. Elective triple valve replacement was done later on (aortic −20 mm, mitral −25 mm and tricuspid −31 mm all Medtronic valves) for the worsening of valvular lesions. Subsequent to this severe low ventricular rate in postoperative period warranted pacemaker implantation, which was done by epicardial approach. During regular follow-up evaluation she was found to have very high threshold of the ventricular lead and end of life pacemaker status at the end of three years. Pulse generator change with the same epicardial lead was not considered because of high threshold. With our experience in cardiac resynchronization therapy CS lead placement was discussed with the patient as an alternative to another thoracotomy and lead placement. After obtaining in formed consent patient was taken up for the procedure. Patient was switched over to heparin after withdrawal of oral anticoagulation in previous days. Pacemaker preparation was done as per standard hospital protocol.
Under strict aseptic precautions left subclavian pocket was made and venous access obtained by modified Seldinger technique and “J” tipped wire positioned in inferior vena cave. 9F sheath (St Jude Medical Ltd) was taken over the wire to the superior vena cave-right atrial junction. Through the sheath decapolar deflectable catheter (CR Bard Inc) was taken into CS. Then sheath was advanced over the catheter and positioned at CS ostium, using angled hydrophilic (Terumo Corp) wire distal CS was entered. Over the wire, 6F Swan–Ganz (Arrow International Inc) balloon catheter was taken and occlusive CS angiogram was done for better visualization of proximal CS and branches to select suitable vein for lead positioning. CS anatomy was distorted with proximal CS ending in a blind loop with small cardiac veins entering the proximal CS. There was a large lateral cardiac vein, which received drainage from multiple branches. Using 0.014 BMW wire (Abbott Vascular Inc) branches of CS were entered and (Medtronic) “Attain Starfix” CS lead was taken over the wire to multiple sites. As the lead position (Figs. 1 and 2) in the lateral cardiac vein had acceptable parameters and no diaphragmatic pacing at high outputs the lead was fixed with opening of “stars”. After confirming the position, the sheaths were removed and the lead was then connected to Medtronic “SIGMA” pulse generator and the same was fixed to deep fascia. Hemostasis achieved and wound was closed in three layers and sterile dressing applied. Patient was discharged on 4th postoperative day with normal pacing and sensing parameters. Pacemaker evaluation after one year revealed a 0.5 V threshold at 40 ms pulse width with normal pacing and sensing.
Fig. 1.
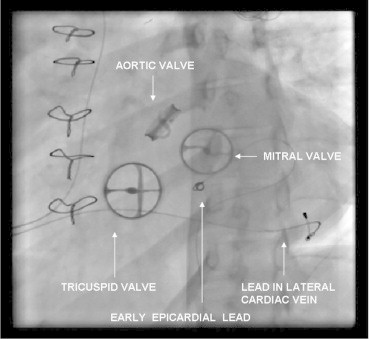
Anteroposterior view showing the valves and leads.
Fig. 2.

Lateral view illustrating the lead position and valves.
3. Discussion
Inaccessibility of right ventricle leaves behind the option for epicardial pacing lead which in stability and threshold is inferior to ventricular leads. Epicardial leads are known to develop high pacing thresholds on follow-up. Anomalous venous drainage, postoperative cardiac status, univentricular heart and prosthetic tricuspid valves are few situations in which the right ventricle entry is difficult or impossible. Rheumatic heart disease with involvement of tricuspid valve is not uncommon in our population. Since the compact AV node is closely related to the anterior superior tricuspid annulus post surgical complete heart block can occur.
Distorted CS ostium and dilated tributaries are not uncommon in patients with right sided valvular involvement which even with dedicated system for canulation may sometimes cause trouble shooting. Pacing from CS lead seems to be the feasible when there is a prosthetic valve in tricuspid position.7 Conventional ventricular leads were tried in great cardiac vein or middle cardiac vein in patients with tricuspid prosthesis in this situation. Lead length, steerability of the lead without guide wire, stability and acceptable threshold are issues with this conventional leads. Great and middle cardiac vein were utilized for permanent pacing in patients with tricuspid prosthesis.8,9 Development of dedicated leads for ventricular pacing from CS for cardiac resynchronization resolved this problem to a greater extent. Unacceptable threshold at implantation is another issue at times.10 Due to unacceptable threshold in CS at the time of implantation, right ventricular pacing was done through mechanical prosthetic valves at one occasion.11 Even though there are reports of pacing through the prosthetic valve it seems that one disc in partially opened position may lead to thrombus formation and or regurgitation. With the growing experiences and advances in cardiac resynchronization therapy CS can be utilized for permanent pacing in those with inaccessible right ventricle.
Conflicts of interest
All authors have none to declare.
References
- 1.Oldershaw P.J., Sutton M.G., Ward D., Jones S., Miller G.A. Ten-year experience of 359 epicardial pacemaker systems: complications and results. Clin Cardiol. 1982;5:515–519. doi: 10.1002/clc.4960051001. [DOI] [PubMed] [Google Scholar]
- 2.Goldstein D.J., Rabkin D., Spotnitz H.M. Unconventional approaches to cardiac pacing in patients with inaccessible cardiac chambers. Ann Thorac Surg. 1999;67:952–958. doi: 10.1016/s0003-4975(99)00150-2. [DOI] [PubMed] [Google Scholar]
- 3.Hsieh M.J., Yeh K.H., Satish O.S., Wang C.C. Permanent pacing using a coronary sinus lead in a patient with univentricular physiology: an extended application of biventricular pacing technology. Europace. 2006;8:147–150. doi: 10.1093/europace/euj023. [DOI] [PubMed] [Google Scholar]
- 4.Corbisiero R., DeVita M., Dennis C. Pacemaker implantation in a patient with persistent left superior vena cava and absent right superior vena cava. J Interv Card Electrophysiol. 2003;9:35–37. doi: 10.1023/a:1025368403990. [DOI] [PubMed] [Google Scholar]
- 5.Al-Khadra A., Al-Awami S., El-Hassan A. Permanent pacing of the heart via a coronary sinus branch. Ann Saudi Med. 1998;18:347–348. doi: 10.5144/0256-4947.1998.347. [DOI] [PubMed] [Google Scholar]
- 6.Herre J.M., Bullaboy C.A., Derkac W.M., Dow M.T. Permanent transvenous dual-chamber pacing using the coronary sinus in a patient with a mechanical prosthetic tricuspid valve. Pediatr Cardiol. 2004;25:65–66. doi: 10.1007/s00246-003-0493-4. [DOI] [PubMed] [Google Scholar]
- 7.Winter J., Gramsch-Zabel H., Fürst G., Koch J.A., Zimmermann N., Gams E. Long-term follow-up of left ventricular pacing via a posterior cardiac vein after mechanical tricuspid valve replacement. Pacing Clin Electrophysiol. 2001;24:125–126. doi: 10.1046/j.1460-9592.2001.00125.x. [DOI] [PubMed] [Google Scholar]
- 8.Bai Y., Strathmore N., Mond H., Grigg L., Hunt D. Permanent ventricular pacing via the great cardiac vein. Pacing Clin Electrophysiol. 1994;17:678–683. doi: 10.1111/j.1540-8159.1994.tb02403.x. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen L.S., Swaroop S., Prejean C.A. Pacing in middle cardiac vein in a patient with tricuspid prosthesis. Pacing Clin Electrophysiol. 2002;25:243–244. doi: 10.1046/j.1460-9592.2002.00243.x. [DOI] [PubMed] [Google Scholar]
- 10.Lee M.E. Special considerations in ventricular pacing in patients with tricuspid valve disease. Ann Thorac Surg. 1983;36:89–92. doi: 10.1016/s0003-4975(10)60657-1. [DOI] [PubMed] [Google Scholar]
- 11.Sierra J., Rubio J. Transvenous right ventricular pacing in a patient with tricuspid mechanical prosthesis. J Cardiothorac Surg. 2008;3:42. doi: 10.1186/1749-8090-3-42. [DOI] [PMC free article] [PubMed] [Google Scholar]


