Highlights
► Malignant struma ovarii can result in cerebral ischemic stroke and Trousseau's syndrome. ► The combination of anti-neoplastic and anti-coagulant therapy should be undertaken to treat and correct the malignancy-associated coagulopathy.
Keywords: Trousseau's syndrome, Malignant struma ovarii, Stroke, Thrombosis
1. Introduction
Trousseau's syndrome, unexplained thrombotic events that precede the diagnosis of an occult visceral malignancy or appear concomitantly with a tumor, was first recognized by Trousseau in 1865 (Trousseau, 1865). Historically, pancreatic carcinoma has been associated with the greatest risk of thrombo-embolic events with a 57% incidence rate (Viselli et al., 1993). Aside from pancreatic malignancy, tumors in other organs such as breast, lung, and colon carcinomas may also have increased risks (Sack et al., 1977). In a review of literature, Sack et al. showed seven reported cases of Trousseau's syndrome related to ovarian carcinoma, which represented 3.8% of all reported cases of thrombo-embolic events associated with malignancies (Sack et al., 1977).
Coagulopathy usually occurs in patients with advanced or recurrent ovarian carcinomas, which may result in deep venous thrombosis (DVT) of the lower extremities in most ovarian cancer patients and subsequently, pulmonary emboli in some cases (Viselli et al., 1993). In addition to the lower extremities and lung, there are reports of ovarian malignancy causing thrombo-embolism in other tissues or organs, including the brain, heart, kidneys, and spleen (Nakayama et al., 2002).
Here is a rare case of malignant struma ovarii with cerebral ischemic stroke in the middle cerebral artery (MCA). The patient underwent anti-thrombotic therapy followed by surgical intervention. However, repeated episodes of ischemic strokes and DVTs occurred and she died of respiratory failure due to brainstem infarction one month after surgery.
2. Case report
A 66-year-old woman with hypertension under good medical control complained of lower abdominal distention for several days. During consultation with a general physician, a fetal-head sized pelvic tumor was palpated on physical examination. The mass originated from ovary and was highly suspected on ultrasonography; therefore, the patient was referred for further work-up. A series of studies including blood testing, imaging studies, and endoscopy for gastro-intestinal examinations was conducted. Except for elevated serum carcinoma antigen 125 (CA-125, 3786.0 U/ml), all of the blood test results were within normal limits. Abdominal and pelvic magnetic resonance imaging (MRI) exhibited a 10 cm left adnexal tumor with heterogeneous components, which was suspected to be ovarian malignancy (Fig. 1). No other abnormalities of the gastro-intestinal tract were noted by endoscopic examination.
Fig. 1.
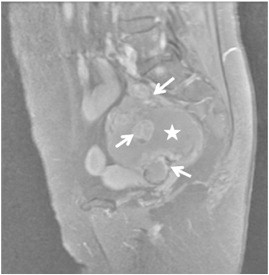
Pre-operative magnetic resonance imaging study of the pelvis revealed a pelvic mass approximately 10 cm in diameter, with cystic (star) and solid (arrows) components.
After completing the diagnostic studies, the patient suddenly suffered from right hemianopia, rightward gaze palsy, and right hemiplegia with global aphasia. The perfusion evaluation of emergency brain computed tomography (CT) revealed occlusion of the left MCA with large territory of cerebral damage (Fig. 2). Studies of coagulation factors, including fibrinogen (159.3 mg/dl; normal ranges 163.5–362.7 mg/dl), fibrinogen and fibrin degradation product (42.5 μg/ml; normal range < 4.1 μg/ml), and fibrinogen and fibrin degradation product-D dimer (27.05 μg/ml; normal range < 2.09 μg/ml) showed hyper-coagulation status. However, ultrasonographic duplex study of the carotid vessels and trans-thoracic echocardiography did not identify any definite thrombus formation.
Fig. 2.
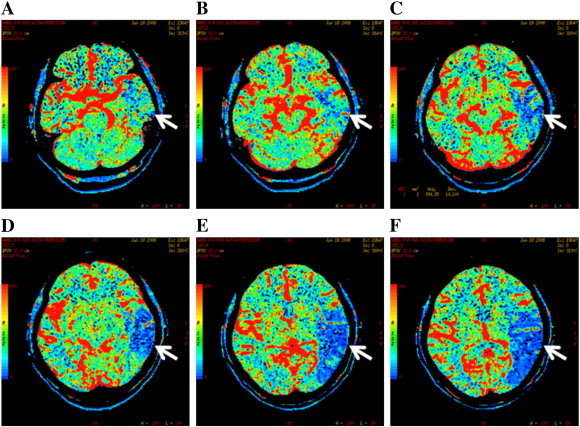
(A–C) Perfusion CT scan of the patient after the first episode of ischemic stroke revealed occlusion of the left MCA. (D–F) The large involved territory (arrows) extended to the left temporal and parietal lobes.
After two weeks of medical control in intensive care unit to balance her vascular and intracranial pressure, the aphasia and right lower limb weakness improved by rehabilitation. However, the tenderness of the left leg became more severe. Venous Doppler ultrasonography revealed thrombi formation over the bilateral lower limbs, especially in left leg. Follow-up brain CT scan showed sub-acute infarctions in the territory of the left MCA but without progression when referenced with previous CT studies. Thus, anti-coagulation therapy as suggested by the hematologist was started with low molecular weight heparin by subcutaneous injection.
After the leg tenderness subsided, staging surgery, including peritoneal washing cytology, total abdominal hysterectomy, bilateral salpingo-oophorectomy, left pelvic lymphadenectomy, and infra-colic omentectomy was performed. Peritoneal tumor seeding or tumor metastasis to adjacent organs was not noted. Optimal debulking surgery without gross residual tumor was performed. Microscopic examination of the left ovary showed predominant thyroid tissue. Tumor cells forming fused glands or irregular nests adjacent to the benign thyroid tissue in a small area demonstrated hyper-chromatic and pleomorphic nuclei, eosinophilic cytoplasm, and evident mitoses. Furthermore, there was lymph node metastasis (Fig. 3). Based on the FIGO criteria of ovarian carcinoma, her tumor was diagnosed as malignant struma ovarii with FIGO stage IIIC disease (Johnson et al., 1999). Results of the thyroid function tests, including T3, free T4, and TSH, were all within normal ranges.
Fig. 3.
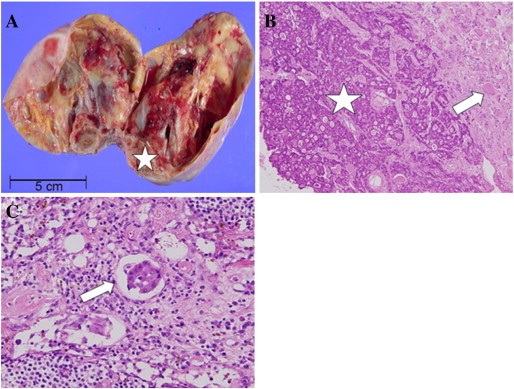
(A) The gross picture of the left ovarian tumor, which was composed of a predominantly cystic lesion with diffuse calcification on the cystic wall. A small, tan-to-brown, gelatinous and solid area (star) was also noted on the cystic wall. (B) Microscopic findings of the solid area revealed an area of malignant neoplastic cells (star) forming fused glands or irregular nests intimately mixed with the adjacent benign thyroid tissue (arrow) (hematoxylin and eosin, original magnification × 200). (C) Microscopic findings of the metastatic cancer cells in the lymph node showed identifiable cancer cells (arrow) in the lymph node (hematoxylin and eosin, original magnification × 400).
The patient's consciousness and right-sided weakness deteriorated two weeks after surgery. Brain CT scan showed ischemic stroke of the left MCA with enlarging territory and infarction of the right occipital lobe, from which the patient never recovered. Two weeks later, a third episode of ischemic stroke occurred. She died of respiratory failure due to brainstem infarction one month after surgery.
3. Discussion
Thrombo-embolic manifestation is a very rare event associated with malignant struma ovarii. To date, there is no thrombo-embolic manifestation associated with malignant struma ovarii reported in literature (http://www.ncbi.nlm.nih.gov/pubmed with the keyword of malignant struma ovarii). This patient may be the first case of Trousseau's syndrome developed in association with malignant struma ovarii. Struma ovarii is a variant of dermoid tumors of the ovary in which the component of thyroid tissues is the major constituent (Kempers et al., 1970). Struma ovarii comprises 2.7% of all ovarian dermoid tumors and very rarely presents in a malignant form, occurring in 0.3–5% of all struma ovarii tumors (Gould et al., 1983). Previous reports have shown that patients with struma ovarii are largely asymptomatic or are accompanied by non-specific symptoms similar to other ovarian neoplasms. Despite disorders of blood coagulation in untreated neoplastic diseases, overt clinically significant thrombo-embolic events remain relatively uncommon. Of the cases associated with malignancy, 3.8% are ovarian in origin (Sack et al., 1977).
Coagulopathy usually occurs in patients with advanced or recurrent ovarian carcinomas, which may result in DVT of the lower extremities and subsequently, pulmonary emboli (Gould et al., 1983; Dvorak, 1987). There are very few reports of ovarian malignancy causing thrombo-embolism in organs other than the lower extremities and lungs, as in the current case report (Nakayama et al., 2002). Several mechanisms for malignancy-coagulopathy have been proposed, including release of thromboplastin-like substances, fibrin deposition, direct factor X activation by tumor proteases, and destruction of endothelial cells with subsequent activation by sub-endothelial tissue or tissue factors (Dvorak, 1987). Furthermore, thrombo-embolic disease like the one in this patient can be due to embolization of free clusters of metastatic malignant cells. Such a hypothesis has been demonstrated in the report of Begin and Raptis, which involved fatal diffuse pulmonary carcinomatous embolization in an ovarian cancer patient (Begin and Raptis, 1991). As such, the thrombo-embolic events of the current patient may be the result of embolization of malignant cell clusters rather than her well-controlled hypertension, because her tumor cells metastasized to the lymph node via lympho-vascular route that can also cause thrombi formation.
A hyper-coagulation state is a frequent complication in advanced cancer, ranging from asymptomatic abnormal coagulation tests to massive clinical thrombo-embolism (Johnson et al., 1999). Malignancy-associated hyper-viscosity is characterized by normal or low hematocrit and hemoglobin concentrations, elevated platelet count, prolonged prothrombin or thrombin time, and increased clotting factor turnover (Sack et al., 1977). However, blood cell counts, hemoglobin, hematocrit, and platelet count were all within normal ranges in this patient when the ischemic stroke occurred. Neither the prothrombin time nor the thrombin time was prolonged and only abnormally increased fibrinogen and fibrin degradation product, and fibrinogen and fibrin degradation product-D dimer were noted.
The primary approach for treating malignancy-related Trousseau's syndrome is the elimination of the causative tumor regardless of underlying mechanisms. Treatment directed to the underlying malignancy can also significantly improve the hyper-coagulable state. If the disease still progresses despite treatment, adequate anti-coagulant therapies are necessary for these patients (Sack et al., 1977). However, a hallmark of Trousseau's syndrome is that breakthrough thrombo-embolic events may occur despite satisfactory levels of anti-coagulation, especially when these patients have persistent, progressive, or recurrent ovarian cancer (Viselli et al., 1993). In the present patient, even though anti-coagulant therapies and complete removal of the tumor were performed, the thrombo-embolic process could not be adequately controlled and eventually led to death.
For advanced malignant struma ovarii, DeSimone et al. reported that surgical resection accompanied by radioiodine therapy could improve clinical outcome (DeSimone et al., 2003). However, the optimal treatment modality remains to be established. For advanced malignant struma ovarii patients with Trousseau's syndrome, as in this case, adjuvant treatment can be started more immediately post-surgery to aggressively correct the coagulopathy, if possible.
In summary, ischemic stroke as the presenting symptom of advanced ovarian cancer is rare. Physicians should take into consideration the possibility that stroke can sometimes be the manifestation of underlying malignancy. Patients with cerebral infarct of unknown etiology should be investigated for a malignant process. When the diagnosis of malignancy is confirmed, a combination of anti-neoplastic and anti-coagulant therapy should be undertaken as soon as possible to treat and correct the malignancy-associated coagulopathy.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
References
- Begin L.R., Raptis S. Diffuse pulmonary carcinomatous embolization: a rare and fatal manifestation of ovarian cancer. Gynecol. Oncol. 1991;41:250–254. doi: 10.1016/0090-8258(91)90318-y. [DOI] [PubMed] [Google Scholar]
- DeSimone C.P., Lele S.M., Modesitt S.C. Malignant struma ovarii: a case report and analysis of cases reported in the literature with focus on survival and I131 therapy. Gynecol. Oncol. 2003;89:543–548. doi: 10.1016/s0090-8258(03)00141-0. [DOI] [PubMed] [Google Scholar]
- Dvorak F.W. Thrombosis and cancer. Hum. Pathol. 1987;18:275–284. doi: 10.1016/s0046-8177(87)80010-2. [DOI] [PubMed] [Google Scholar]
- Gould S.F., Lopez R.L., Speers W.C. Malignant struma ovarii. A case report and literature review. J. Reprod. Med. 1983;28:415–419. [PubMed] [Google Scholar]
- Johnson M.J., Sproule M.W., Paul J. The prevalence and associated variables of deep venous thrombosis in advanced cancer. Clin. Oncol. (R Coll Radiol) 1999;11:105–110. doi: 10.1053/clon.1999.9023. [DOI] [PubMed] [Google Scholar]
- Kempers R.D., Dockerty M.B., Hoffmann D.L., Bartholomew L.G. Struma ovarii: ascitic, hyperthyroid and asymptomatic syndromes. Ann. Intern. Med. 1970;72:883–893. doi: 10.7326/0003-4819-72-6-883. [DOI] [PubMed] [Google Scholar]
- Nakayama M., Iha T., Kanazawa K. Unusual Trousseau's syndrome in ovarian carcinosarcoma: multiple systemic thrombo-embolic events. J. Obstet. Gynaecol. 2002;22:699–700. doi: 10.1080/014436102762062475. [DOI] [PubMed] [Google Scholar]
- Sack G.H., Jr., Levin J., Bell W. Trousseau's syndrome and other manifestations of chronic disseminated coagulopathy in patients with neoplasms: clinical, pathologic and therapeutic features. Medicine (Baltimore) 1977;56:1–37. [PubMed] [Google Scholar]
- Trousseau A. Vol. 3. 1865. Phlegmasia alba dolens: clinique Medicale de l'Hotel-Dieu de Paris, London; p. 94. (New Sydenham Society). [Google Scholar]
- Viselli A.L., Freuer G.A., Granai C.O. Lower limb ischemic venous thrombosis in patients with advanced ovarian carcinoma. Gynecol. Oncol. 1993;49:262–265. doi: 10.1006/gyno.1993.1120. [DOI] [PubMed] [Google Scholar]


