Abstract
Background
Balloon mitral valvotomy (BMV) is a safe and an effective treatment in patients with symptomatic rheumatic mitral stenosis. This study was conducted to validate the importance of assessing the morphology of mitral valve commissures by transoesophageal echocardiography and thereby predicting the outcome after balloon mitral valvotomy [BMV].
Materials and methods
Study consisted of 100 patients with symptomatic mitral stenosis undergoing BMV. The Commissural Morphology and Wilkins score were assessed by transoesophageal echocardiography. Both the commissures (anterolateral and posteromedial) were scored individually according to whether non-calcified fusion was absent (0), partial (1), or extensive (2) and calcification (score 0) and combined giving an overall commissural score of 0–4. Outcome of BMV was correlated with commissural score and Wilkins score.
Results
The commissural score and outcome after BMV correlated significantly. 66 of 70 patients (94%) with a commissural score of 3–4 obtained a good outcome compared with only six (20%) patients of 30 with a commissural score of 0–2 (positive and negative predictive accuracy 94% and 80%, respectively, p < 0.001). Increase in 2DMVA post BMV was more in patients with higher commissural score (score of 3–4). Wilkins score <8 usually predicts a good outcome but even in patients with Wilkins score >8 a commissural score >2 predicts a 50% chance of a good result.
Conclusions
A higher commissural score predicts a good outcome after BMV hence it can be concluded that along with Wilkins score, commissural morphology and score should be assessed with TOE in patients undergoing BMV.
Keywords: Balloon mitral valvotomy, Transoesophageal echocardiography, Wilkins score, Commissural score
1. Introduction
After the first description in 1984 by Inoue et al,1 balloon mitral valvotomy (BMV) has become a safe and effective treatment for severe rheumatic mitral stenosis with results equivalent to surgical valvotomy.2–4 Commissural splitting is the dominant mechanism by which mitral valve area is increased during BMV.5–7
Mitral valve morphology is assessed by two dimensional transthoracic echocardiographic score based on the criteria of Wilkins et al.8 The Wilkins score is based on a semi quantitative assessment of leaflet thickening, mobility, calcification, and subvalvar thickening each graded on a scale of 1–4. Higher Wilkins scores (>8) indicates more severe degenerative disease and studies have shown this to be a significant, though relatively weak, predictor of success from BMV.9 However, the Wilkins score does not include commissural assessment.
Earlier studies have shown that assessment of commissural morphology by transthoracic echocardiography (TTE) is useful in predicting outcome after BMV. In 149 patients investigated by Cannan et al,10 the mitral commissures were assessed in the short axis parasternal view. Commissural calcification was associated with a lower survival rate and a higher incidence of mitral valve replacement after BMV. Fatkin et al7 studied 30 patients by a similar transthoracic approach and showed that assessment of commissural disease before BMV is useful for the prediction of commissural splitting and the final increase in valve area. Sutaria et al11 studied 300 patients, and found that commissural calcification was an independent predictor of outcome with only 40% of those with commissural calcification achieving a final MVA > 1.5 cm2 compared with 64% of those without commissural calcification.
Transoesophageal echocardiography (TOE) is performed routinely at our center before BMV to exclude left atrial thrombus. In comparison with TTE, TOE offers superior resolution of the mitral valve apparatus and overcomes problems caused by anterior leaflet shadowing, thereby providing a systemic scan of the whole length of mitral commissure and mitral valve calcification. This study was conducted to assess commissural morphology and score in mitral stenosis patients using Transoesophageal Echocardiography (TOE) and correlate it with outcomes after balloon valvotomy.
2. Material and methods
Hundred patients of mitral stenosis who underwent BMV in Department of Cardiology, Sri Venkateswara Institute of Medical sciences, Tirupati between May 2007 and Dec 2008 were included in this study. This study was approved by the Institutional Ethical Committee of Sri Venkateswara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India.
Patients with symptomatic mitral stenosis undergoing BMV for the first time and patients with history of previous valvotomy (BMV/Surgical valvotomy) undergoing BMV for symptomatic mitral restenosis were included in this study.
Patients with left atrial or left atrial appendage thrombus, mitral regurgitation greater than 2/4 on echocardiography, those with calcific mitral stenosis, severe aortic valve disease, severe tricuspid valve disease and critically ill patients were excluded.
After informed consent all patients underwent a detailed clinical evaluation as per proforma which included clinical features, baseline blood investigations, electrocardiogram, chest roentgenogram and echocardiography.
2.1. Transthoracic echocardiography (TTE)
All patients underwent two dimensional and Doppler TTE immediately before BMV with Philips Sonos 7500, ultrasound scanners. After recording LA size, LVEF, Wilkins score was assessed. Mitral stenosis severity was assessed by transmitral gradients, valve area and pulmonary artery systolic pressure. Initial mitral valve area (MVA) was measured by Doppler pressure half time and planimetry taking the mean of five recordings. Final MVA was measured by planimetry of the mitral orifice in the parasternal short axis view within 24 h after BMV. The severity of mitral regurgitation (MR) after BMV was assessed by color Doppler.
Good outcome was defined as
-
1.
final MVA>1.5 cm2
-
2.
increase in the valve area>25% of baseline
-
3.
absence of severe MR
2.2. Transoesophageal echocardiography (TOE)
All patients underwent TOE immediately before BMV with a 7 MHz multiplane transoesophageal probe and Philips 7500 ultrasound scanner. The mitral valve leaflets and subvalvar apparatus were examined at mid-oesophageal and transgastric levels. Mitral valve anatomy was scored according to the criteria of Wilkins et al8 (Table 1). The mitral commissures were scanned systematically at the mid-oesophageal level. The anterolateral commissure was visualized in the transverse plane by advancing and retracting the probe, thereby scanning the length of the commissure from the leaflet tip to the annulus. The posteromedial commissure was scanned in the longitudinal plane by rotating the probe clockwise and anticlockwise (Fig. 1). Commissural calcification was identified by high intensity echoes casting an acoustic shadow (Fig. 2).
Table 1.
Anatomic classification of the mitral valve echocardiographic examination. (Wilkins score, Massachusetts General Hospital, Boston).
Leaflet mobility
|
Valvular thickening
|
Subvalvular thickening
|
Valvular calcification
|
Note: The final score is found by adding the scores for each of the components.
From Wilkins GT, Gillam LD, Weyman AE, et al Percutaneous balloon dilatation of the mitral valve: an analysis of echocardiographic variables related to outcome and the mechanism of dilatation. Br Heart J 1988; 60: 299–308.
Fig. 1.
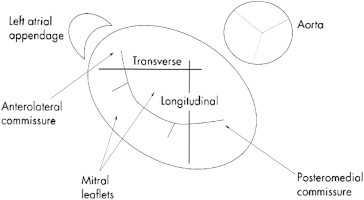
Mitral valve anatomy viewed from the left atrium with orientation of the transverse and longitudinal transoesophageal planes.
Fig. 2.
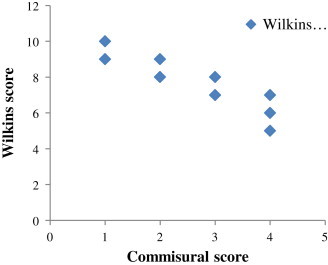
The distribution of Wilkins score across commissural scores.
Each commissure was assigned a score to reflect the likelihood of splitting (Table 2). Anterolateral and posteromedial commissures were scored individually according to whether non-calcified fusion was absent (0), partial (1), or extensive (2). Calcified commissures usually resist splitting and scored 0. Scores for each commissure were combined giving an overall commissure score for each valve of 0–4, higher scores reflecting increased likelihood of commissural splitting. A high score indicated extensively fused, non-calcified commissures that were therefore more likely to split. A low score indicated either minimal fusion or the presence of resistant commissural calcification. Valve anatomy graded by the method of Wilkins et al, does not include commissural assessment.
Table 2.
Commissural score.
| Commissure score | Commissure morphology |
|---|---|
| 0 | Neither commissure fused or calcification of both commissures or absent fusion of one commissure and calcification of other |
| 1 | Partial fusion of one commissure and absent fusion or calcification of the other |
| 2 | Extensive fusion of one commissure and absent fusion or calcification of the other or partial fusion of both commissures |
| 3 | Extensive fusion of one commissure, partial fusion of the other, and no commissural calcification |
| 4 | Extensive fusion of both commissures and no commissural calcification |
From – N Sutaria, TRD Shaw, D Northridge et al. Commissural morphology predicts outcome after balloon mitral valvotomy. Heart 2006; 92: 52–57.
2.3. Statistical analysis
Mean and standard deviation were calculated for continuous variables and Percentages were used for describing the categorical variables. An unpaired students ‘t’ test was used to assess the significance of difference between means of two independent groups (A&B). Pearson correlation co-efficient (r) was calculated for studying the relationship between two continuous variables, the significance of which was tested with a ‘t’ test. p value < 0.05 was considered as statistically significant. All computation and statistical analysis were done using SPSS version 13.0, SPSS Inc. Chicago, USA.
3. Results
We studied 100 patients, the baseline characteristics of these patients are described in Table 3.The patients age ranged from 9 to 59 years with mean (SD) of 33.51 ± 10.42 years. Majority of patients were in the age group of 21–40 years. Out of the 100 patients included 72% were females and 28% were males.
Table 3.
Baseline patient characteristics (No. of patients n = 100).
| Characteristic | Patients |
|---|---|
| Age | 33.51 ± 10.42 yrs |
| Sex | |
| Male | 28 |
| Female | 72 |
| Duration of symptoms | 22 ± 18.2 months |
| Functional class (NYHA) | |
| Class-I | 0 |
| Class-II | 64 |
| Class-III | 28 |
| Class-IV | 8 |
| Rheumatic fever history | |
| Present | 43% |
| Absent | 57% |
| CVA history | 4% |
| AF present | 12% |
| AV block present | 1% |
| Restenosis cases | |
| Post BMV | 7 |
| OMV/CMV | 8 |
| Height | 156.6 ± 9.47 cm |
NYHA – New York Heart Association, CVA – cerebrovascular accident, AF – atrial fibrillation, AV block – atrio-ventricular conduction block, BMV- balloon mitral valvuloplasty, CMV – closed mitral valvuloplasty.
The mean (SD) duration of symptoms was 22 ± 18.2 months (range 10–40 months). Most common symptom was dyspnea and 64% of patients were in NYHA Class-II, 28% were in NYHA Class-III, 8% were in NYHA Class-IV.
Rheumatic fever history was present in 43% of cases and 76% were receiving benzethine penicillin prophylaxis.
Atrial fibrillation was noted in 12% of cases. Cerebrovascular accident history was noted in 4 cases and all were in atrial fibrillation.
Of the 100 cases included, 15% were mitral restenosis, 7 cases were post BMV and 8 cases were post surgical valvotomy [both open mitral valvotomy (OMV) and close mitral valvotomy (CMV).
On TTE, 87% of cases had dilated left atrium (LA) >40 mm and LA size ranged from 33 to 58 mm with mean (SD) LA size being 46.77 ± 5.96 mm, 7% of patients had left ventricular (LV) systolic dysfunction, one patient had moderate dysfunction with an ejection fraction (EF) of 35%, and remaining 6 patients had mild dysfunction (EF >40%). Mean (SD) EF was 58.8 ± 6.52%.
On TOE, Wilkins score ranged from 5 to 10 with a mean (SD) score of 7.25 ± 0.98. Commissural score ranged from 0 to 4. 2 patients had score of 1, 28 patients had score 2, 45 patients had score 3 and 25 patients had score 4. Majority of patients (70%) had commissural score more than 2. The Echocardiographic parameters are summarized in Table 4. The hemodynamic parameters were recorded during the BMV procedure and are presented in Table 5.
Table 4.
Echocardiographic parameters in the entire study population (n = 100).
| Parameter | Values |
|---|---|
| LA size (mm) | 46.77 + 5.96 |
| LV dysfunction | 7 cases (7%) |
| LVEF (%) | 58.8 + 6.5 |
| Wilkins score | |
| Average score distribution | 7.25 + 0.98 |
| 5 | 3 (3%) |
| 6 | 15 (15%) |
| 7 | 49 (49%) |
| 8 | 20 (20%) |
| 9 | 12 (12%) |
| 10 | 1 (1%) |
| Mean commissural score | 2.91 + 1.2 |
| Mean Wilkins score in patients with commissural calcification | 8.67 + 0.7 |
All values are mean ± standard deviation or actual numbers with percentages in parentheses. LA – left atrium, LV –left ventricular, LVEF – left ventricular ejection fraction.
Table 5.
Hemodynamic parameters.
| Parameter | Pre |
Post |
p value |
|---|---|---|---|
| BMV | |||
| MVA cm2 | 0.83 ± 0.16 | 1.82 ± 0.24 | <0.01 |
| MVIg mmHg | 18.57 ± 5 | 4.74 ± 2.89 | <0.001 |
| RVSP mmHg | 62.27 ± 21.9 | 45.4 ± 18.8 | <0.001 |
| LAm – LVEDP gradient | 13.14 ± 5.69 | 2.1 ± 1.6 | <0.001 |
BMV – balloon mitral valvuloplasty, MVA – mitral valve area, MVIg – mitral inflow gradient, RVSP – right ventricular systolic pressure, LAm – left atrial mean, LVEDP – left ventricular end diastolic pressure.
3.1. Outcomes from BMV
Balloon dilatation of the mitral valve was achieved in all patients and mean MVA assessed by echocardiography increased from 0.83 ± 0.16 cm2 to 1.82 ± 0.24 cm2 (p < 0.01). Eight patients (8%) developed significant MR on echocardiography. Patients were divided according to outcomes into 2 groups, Group A included those with good outcome (as defined by our prespecified criteria), which was seen in 72% and Group B which included those with suboptimal outcome, seen in 28%.
3.2. Commissural score
The commissure score and outcome after BMV correlated significantly, higher scores predicted a more favorable result (Table 6, Fig. 3). 66 of 70 patients (94%) with a commissure score of 3–4 obtained a good outcome compared with only six (20%) patients of 30 with a commissure score of 0–2 (positive and negative predictive accuracy 94% and 80%, p < 0.001 (Table 6)). Increase in MVA post BMV was more in patients with higher commissural score (score of 3–4) (Table 7).
Table 6.
Relation between commissural score and valvular outcome after balloon mitral valvotomy.
| Commissural score | No. of patients | Good outcome | |
|---|---|---|---|
| 0 | 0 | – | 6/30 (20%)* |
| 1 | 2 | 0 (0%) | |
| 2 | 28 | 6 (22%) | |
| 3 | 45 | 42 (93%) | 66/70 (94.3%)* |
| 4 | 25 | 24 (96%) | |
*p Value < 0.001 for comparison between favorable commissural score (3–4) and unfavorable score (0–2). The commissural score of 3–4 had positive and negative predictive values of 94% and 80%, respectively for good outcome after balloon mitral valvotomy.
Fig. 3.
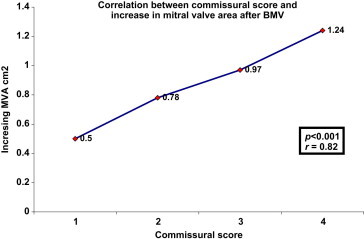
Depicting an increase in post BMV MVA with an increase in commissural score. BMV – balloon mitral valvuloplasty, MVA – mitral valve area.
Table 7.
Correlation between commissural score and increase in MVA after BMV.
| Commissural score | No. of patients | Pre BMV cm2 | Post BMV cm2 | Increase in MVA (cm2) |
|---|---|---|---|---|
| 1 | 2 | 0.75 | 1.25 | 0.5 |
| 2 | 28 | 0.81 | 1.59 | 0.78 |
| 3 | 45 | 0.85 | 1.82 | 0.97 |
| 4 | 25 | 0.86 | 2.10 | 1.24 |
MVA – mitral valve area, BMV – balloon mitral valvuloplasty.
Nine patients (9%) had calcification localized to either the anterolateral or posteromedial commissure by TOE. No patients had bicommissural calcification. Commissural calcification predicted a suboptimal result, being present in 2.8% (2/72) of Group A patients compared with 25% (7/28) in Group B (p < 0.01). Commissural calcification increased significantly with advancing age (p < 0.001). Mean (SD) age of patients with commissural calcification was 49 ± 8 yrs verses mean (SD) age of total patients of 33.5 ± 10.4 yrs. Patients with higher Wilkins scores were more likely to have commissural calcification (p = 0.013). Mean Wilkins score of commissural calcification patients was 8.67 ± 0.7 verses mean Wilkins score of total patients of 7.25 ± 0.9.
3.3. Wilkins score
The Wilkins score significantly predicted outcome (mean Wilkins score 6.5 ± 0.8 v 8 ± 1.05 in groups A and B, respectively, p < 0.01). Patients achieving a greater increase in valve area tended to have lower Wilkins scores. Wilkins score distribution in the study population is summarized in Table 4. In this study 87 patients had Wilkins score ≤ 8 and 13 patients had Wilkins score > 8 predicting an unfavorable outcome from BMV. Of the 13 patients, 6 (46%) patients had good outcome in comparison to 66 (76%) of 87 patients with score ≤ 8 had good outcome. At the conventional cut off of 8, the Wilkins score was less helpful in predicting good outcome compared with the commissure score (positive and negative accuracy of 76% and 54%, respectively, p < 0.04). The Wilkins score and commissure score did not significantly correlate.
3.4. Combined assessment of Wilkins criteria and commissural morphology
In patients with good Wilkins valves (Wilkins score ≤ 8), leaflet and subvalvar changes are minimal and severe stenosis is predominantly due to commissural fusion. In such cases, the commissural score (assessing non-calcified, splittable commissural fusion) was more accurate in predicting outcome.
Out of 65 patients with Wilkins score < 8 and commissural score > 2, 57 (88%) patients had good outcome. In this group of patients, a commissure score > 2 predicted a good result with positive and negative predictive value of 88% and 70%, respectively (p < 0.01). In those with Wilkins score > 8 and a commissure score > 2 only 50% obtained a good result (total 12 patients).
3.5. Mitral regurgitation
In this study, 8 (8%) patients developed significant MR. Two patients with severe MR had anterior leaflet tear and underwent mitral valve replacement and the remaining 6 patients had commissural MR (mean MR jet area – 6.5 cm2).
We did not observe a significant correlation between commissure score and the development of severe echocardiographic MR. Mean commissural score was 2.5 ± 0.9 v 2.9 ± 1.2.
The eight patients developing severe MR had a significantly higher Wilkins score (8.8 ± 0.84 v 7.25 ± 0.9, p < 0.04). We observed that four of these eight patients had commissural calcification and in these cases TTE done in the short axis plane showed the mechanism of MR to be a leaflet tear adjacent to the area of calcification.
3.6. Result of restenosis cases
Out of 100 patients, 15% were restenosis cases. Among them, 7 were post BMV patients and 8 were post surgical valvotomy (OMV/CMV). Only 7 patients (47%) had good outcome, compared to 72% in the total patients.
Mean MVA increased from 0.88 ± 0.18 cm2 to 1.65 ± 0.19 cm2, compared to MVA of total patients of 0.83 ± 0.16 cm2–1.82 ± 0.24 cm2. Wilkins score, commissural score and mean mitral gradients difference was statistically insignificant (p = 0.08).
In this study no deaths are reported.
4. Discussion
Mitral valve anatomy has been shown to be the strongest independent predictor of success after BMV.4,8,9 The Wilkins echocardiographic score8 which is used widely to guide patient selection for BMV is based on an assessment of leaflet thickness, mobility, and calcification and of the extent of subvalvar disease, but commissural morphology is not considered. In a study evaluating the relation between Wilkins score and change in MVA, Abascal et al9 observed a substantial scatter in the data; although 84% of those with scores < 8 had a good outcome, so did 42% of those with scores > 8. More recent studies have found this scoring system to be inadequate7,10 indicating the need for a better echocardiographic assessment.
TTE is the most commonly used technique for the assessment of mitral valve morphology and for screening patients for BMV. Left atrial thrombus cannot be reliably excluded by TTE because of its inability to visualize the left atrial appendage fully in all patients,12–14 and many centers now routinely perform TOE before BMV for this reason. The longitudinal transgastric plane, when available, also allows more detailed visualization of the chordae and papillary muscles than does TTE.15 TOE also has a role after BMV, since it is more accurate in determining the severity and mechanism of MR and in evaluating the degree of any residual left to right shunting across the interatrial septum.12,15
A further advantage of TOE over TTE is that acoustic shadowing from leaflet calcification is cast behind the valve into the left ventricle and is less likely to obscure the orifice, thereby allowing more accurate localization of calcification. So our study insists the advantages of TOE over conventional TTE for the assessment of commissural calcification and fusion and thereby shows the value of TOE in predicting procedural outcome after BMV.
In vivo and in vitro studies5–7 have confirmed that the mechanism underlying the increase in valve area associated with BMV involves splitting of one or both fused mitral commissures in a manner similar to surgical commissurotomy. BMV is therefore unlikely to increase the MVA if commissural fusion is absent or minimal, or if the commissures resist splitting because of the presence of calcium. In the present study, commissural calcification was identified in nine patients and predicted a suboptimal immediate outcome. The significance of commissural calcification has recently been reported by other investigators. In 149 patients investigated by Cannan et al,10 the mitral commissures were examined for the presence or absence of calcification by TTE alone in the parasternal short axis view. Calcification localized to a commissure was associated with a lower survival rate and a higher incidence of mitral valve replacement. Fatkin et al7 used a similar transthoracic approach in 30 patients undergoing BMV. Commissural splitting resulted in a greater increase in valve area and this occurred if at least one commissure was not heavily fibrosed or calcified. The assessment of commissural morphology allowed an accurate prediction of immediate outcome. Sutaria et al11 reported the relation between commissural calcification and immediate outcome after BMV in 300 patients, mean age 61 years, studied by TTE. Only 40% of those with commissural calcification visualized in the parasternal short axis view achieved a final MVA > 1.5 cm2 compared with 64% of those without. A quantitative grading of the extent of commissural calcification was an independent predictor of outcome. This grading was most useful for patients with low Wilkins scores and therefore of little use for other degenerative disease of the leaflets and chordae.
Although the Wilkins score does not specifically assess the commissures, the Wilkins score and commissural calcification were significantly correlated. Degenerative disease of the commissures probably progresses in parallel with leaflet and subvalvar disease. Heavy generalized leaflet calcification is likely to involve the commissures.
The Wilkins score therefore is a useful screening tool for patients referred for BMV and in our study was a significant independent predictor of outcome. However, our results and those of Fatkin et al7 and Cannan et al10 have shown that echocardiographic assessment of commissural morphology has important additional predictive value. In our patients, the commissure score was a more accurate predictor of outcome than the Wilkins score.
The extent of non-calcified commissural fusion can also be semiquantitatively assessed. Calcified commissures were shown to be strongly associated with adverse outcome. In patients where one commissure was calcified, absent, or minimal, fusion of the opposite commissure (commissure score 0 or 1) resulted in a suboptimal outcome. In the absence of commissural calcium, a low commissure score of 0 or 1 may also be given when mitral stenosis is mild or when stenosis is caused by disease localized to the mitral leaflets or subvalvar apparatus rather than the commissures, a situation not infrequent after a previous surgical valvotomy. In both cases, balloon dilatation is unlikely to achieve a satisfactory increase in valve area. Evaluation of commissural fusion as well as calcification should therefore provide a scoring system that more accurately reflects valve splittability. We found a strong correlation between commissure score and increase in valve area (p < 0.001; Fig. 3), consistent with this hypothesis.
Our scoring system did not differentiate between non-fusion and calcification; in both instances a score of 0 would be assigned to the commissure, since we assume the commissure will not split at this site. 28 patients had a commissure score of 2, 9 cases were caused by severe fusion of one commissure and calcification of the other and among them four (22%) had a good result. Commissural score of 3–4 was present in 70 patients, and among them 94% had good outcome. Although patient numbers are small, the findings suggest that patients with one severely fused and splittable commissure and partial-fusion/total fusion at the other will gain a favorable immediate result from balloon dilatation, whereas any commissural calcification confers an adverse prognosis. In accordance, the positive predictive value of the commissure score was improved in those patients with good Wilkins valves in whom commissural fusion is the dominant cause of stenosis.
Mitral regurgitation is a relatively common complication of BMV but is difficult to predict from pre procedure valve morphology and clinical variables alone.16 MR often increases mildly after BMV at the sites of successful commissural splitting.7,15,16 Surgical data from patients undergoing early mitral valve replacement for severe MR after BMV have shown that the mechanism of severe MR usually involves a leaflet tear associated with commissural calcification.12 Hernandez et al16 noted that, besides commissural calcification, severe subvalvar disease was often found at surgery in patients with severe MR after BMV. Padial et al17 showed that a combined echocardiographic assessment of leaflet thickening, subvalvar disease, and commissural calcification was a powerful independent predictor of severe MR with BMV. In the present study, development of severe MR was associated with a significantly higher Wilkins score and the role of commissural morphology is not clear although it could have a contributing role.
5. Limitations
TOE is a safe, though semi invasive procedure. TOE may not be indicated in all the patients, especially the younger population with good TTE images but is routinely performed at our center at no extra cost to the patients. TOE was not repeated routinely after BMV. We did not follow up patients in the longer term and previous studies have shown long term outcome to be strongly related to initial improvement in valve area.
The commissural score was derived from TOE only, and actual comparison of this semi quantitative and objective score was not done with TTE, as TOE images were clearly superior for commissural assessment and this prevented a real time comparison between the two echo modalities.
6. Conclusions
TOE is simple and semi invasive investigation in assessing mitral commissural fusion and calcification in patients undergoing BMV.
The present study validates a novel echocardiographic assessment score.
The commissure score, is reproducible and a useful predictor of immediate outcomes.
Patients with unfavorable commissural morphology (indicated by a commissure score of 0–2) are less likely to obtain a good result Patients with low Wilkins score < 8 and favorable commissural morphology (commissural score 3–4) are likely to get good results with BMV.
Majority of restenosis cases would get suboptimal results with BMV.
Along with Wilkins score, application of this scoring system during routine TOE examination before BMV may improve patient selection and in those with poor commissural morphology, modification of BMV technique (suboptimal inflations) or mitral valve replacement would need to be considered.
Conflicts of interest
All authors have none to declare.
References
- 1.Inoue K., Owaki T., Nakamura T. Clinical application of transvenous mitral Inoue commissurotomy by a new balloon catheter. J Thorac Cardiovasc Surg. 1984;87:394–402. [PubMed] [Google Scholar]
- 2.Farhat M.B., Ayari M., Maatouk F. Percutaneous balloon versus surgical closed and open mitral commissurotomy: short and long term results. Circulation. 1998;97:245–250. doi: 10.1161/01.cir.97.3.245. [DOI] [PubMed] [Google Scholar]
- 3.Vahanian A., Michel P.L., Cormier B. Results of percutaneous mitral commissurotomy in 200 patients. Am J Cardiol. 1989;63:847–852. doi: 10.1016/0002-9149(89)90055-6. [DOI] [PubMed] [Google Scholar]
- 4.Bassand J., Schiele F., Bernard Y. Double balloon and Inoue techniques in percutaneous mitral valvotomy: comparative results in a series of 232 cases. J Am Coll Cardiol. 1991;18:982–989. doi: 10.1016/0735-1097(91)90757-z. [DOI] [PubMed] [Google Scholar]
- 5.Reid C.L., McKay C.R., Chandraratna P.A.N. Mechanisms of increase in mitral valve area and the influence of anatomic features in double-balloon catheter balloon valvotomy in adults with rheumatic mitral stenosis: a Doppler and two dimensional echocardiographic study. Circulation. 1987;76:628–636. doi: 10.1161/01.cir.76.3.628. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan J.D., Isner J.M., Karas R.H. In vitro analysis of balloon valvuloplasty of stenotic mitral valves. Am J Cardiol. 1987;59:318–323. doi: 10.1016/0002-9149(87)90806-x. [DOI] [PubMed] [Google Scholar]
- 7.Fatkin D., Roy P., Morgan J. Percutaneous balloon mitral valvotomy with the Inoue single balloon catheter: commissural morphology as a determinant of outcome. J Am Coll Cardiol. 1993;21:390–397. doi: 10.1016/0735-1097(93)90680-y. [DOI] [PubMed] [Google Scholar]
- 8.Wilkins G.T., Weyman A.E., Abascal V.M. Percutaneous dilatation of the mitral valve: an analysis of echocardiographic variables related to outcome and the mechanism of dilatation. Br Heart J. 1988;60:299–308. doi: 10.1136/hrt.60.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abascal V.M., Wilkins G.T., Choong C.Y. Echocardiographic evaluation of mitral valve structure and function in patients followed for at least six months after percutaneous mitral balloon valvuloplasty. J Am Coll Cardiol. 1988;12:606–615. doi: 10.1016/s0735-1097(88)80045-7. [DOI] [PubMed] [Google Scholar]
- 10.Cannan C., Nishimura R., Reeder G.S. Echocardiographic assessment of commissural calcium: a simple predictor of outcome after percutaneous mitral balloon valvotomy. J Am Coll Cardiol. 1997;29:175–180. doi: 10.1016/s0735-1097(96)00422-6. [DOI] [PubMed] [Google Scholar]
- 11.Sutaria N., Northridge D., Shaw T.R.D. The significance of commissural calcification on outcome of mitral balloon valvotomy. Heart. 2000;84:398–402. doi: 10.1136/heart.84.4.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cormier B., Vahanian A., Michel P.L. Transoesophageal echocardiography in the assessment of percutaneous mitral commissurotomy. Eur Heart J. 1991;12(suppl B):61–65. doi: 10.1093/eurheartj/12.suppl_b.61. [DOI] [PubMed] [Google Scholar]
- 13.Kronzon I., Tunick O.A., Glassman E. Transoesophageal echocardiography to detect atrial clots in candidates for percutaneous transseptal mitral balloon valvuloplasty. J Am Coll Cardiol. 1990;16:1320–1322. doi: 10.1016/0735-1097(90)90572-7. [DOI] [PubMed] [Google Scholar]
- 14.Thomas M.R., Monaghan M.J., Smyth D.W. Comparative value of transthoracic and transoesophageal echocardiography before balloon dilatation of the mitral valve. Br Heart J. 1992;68:493–497. doi: 10.1136/hrt.68.11.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rittoo D., Sutherland G.R., Currie P. The comparative value of transoesophageal and transthoracic echocardiography before and after percutaneous mitral balloon valvotomy: a prospective study. Am Heart J. 1993;125:1094–1105. doi: 10.1016/0002-8703(93)90119-t. [DOI] [PubMed] [Google Scholar]
- 16.Hernandez R., Macaya C., Benuelos C. Predictors, mechanisms and outcome of severe mitral regurgitation complicating percutaneous mitral valvotomy with the Inoue balloon. Am J Cardiol. 1993;70:1169–1174. doi: 10.1016/0002-9149(92)90050-9. [DOI] [PubMed] [Google Scholar]
- 17.Padial L.R., Abascal V.M., Moreno P.R. Echocardiography can predict the development of severe mitral regurgitation after percutaneous mitral valvuloplasty by the Inoue technique. Am J Cardiol. 1999;83:1210–1213. doi: 10.1016/s0002-9149(99)00061-2. [DOI] [PubMed] [Google Scholar]


