Abstract
Aims
In India, larger proportions of patients with ACS present with STEMI. We sought to study the recent trends of reperfusion in patients of acute STEMI.
Methods and Results
1905 patients presenting with acute STEMI enrolled. 1636 (86%) received some form of reperfusion therapy. Streptokinase, 1235 (65%) patients, was the most common mode of reperfusion therapy used followed by primary PCI (205, 10.7%) and tenecteplase (196, 10%). 269 (14%) did not receive any form of reperfusion therapy, the most common reason being late presentation in 230 (85.7%). Patients presenting with STEMI increased from 297 to 446 comparing first and last half-year of study period. The PCI and tenecteplase numbers increased from 19 to 68 and 27 to 97 respectively.
Conclusion
There was 20% increase in STEMI every year. Younger patients are least likely to receive primary PCI or tenecteplase. 1 in 8 patients of STEMI did not receive any form of reperfusion therapy.
Keywords: ST elevation myocardial infarction (STEMI), Percutaneous Coronary intervention (PCI), Reperfusion therapy, Thrombolytic agents, Acute coronary syndrome (ACS)
1. Introduction
Coronary artery disease (CAD) is the most common cause of death in both developing and developed countries.1 By 2020 CAD is expected to increase by more than 120% in the developing countries as compared to 30–40% in the developed countries.2 60% of the world's heart disease is expected to occur in India.3 This will place a huge strain on healthcare resources which are already inadequate and overstretched. Providing optimal care to patients of CAD in the Indian setting requires specific and relevant data applicable to the general population.
The spectrum of CAD in the developed countries appears to be different from that in the Indian population. Less than 40% of the patients with acute coronary syndrome present with ST-Segment Elevation Myocardial Infarction (STEMI) in the developed countries4,5 and this is also showing a decreasing trend with time. On the other hand 60% of patients with ACS present with ST segment elevation myocardial infarction in India. In patients with ST elevation myocardial infarction, the main consideration in treatment is reperfusion which is influenced by duration from onset of symptoms. The best treatment for patients presenting with STEMI is reperfusion either in the form of primary Percutaneous coronary intervention (PCI) or by means of thrombolytic agents. Primary PCI re-establishes blood flow in the culprit coronary artery by mechanically dislodging the thrombus obstructing the vessel and has been shown consistently in most studies to be superior to thrombolytics. Primary PCI is not available in most tertiary care centres in India. So in most centres treatment of STEMI is based on pharmacological thrombolysis by using streptokinase or tenecteplase.
Most data on patients with acute coronary syndromes are derived from several large registries from developed countries.6–13 Data regarding revascularization in STEMI from India came from study by Jose and Gupta (2004) and CREATE study.15 The study by Jose et al was a single-centre study done in pre PCI era of CMC Vellore. It enrolled 1320 patients with STEMI with mean age of 56 ± 13. Males comprised of 83.6% of patients and 82.8% of patients underwent reperfusion only by means of thrombolytic. CREATE registry which was a prospective registry done in 89 centres from 10 regions and 50 cities in India. It enrolled 20,937 patients out of which 12,405 (60.6%) had STEMI. The mean age of these patients was 57.5 (SD 12.1) years. 6226 (30.4%) patients had diabetes; 7720 (37.7%) had hypertension; and 8242 (40.2%) were smokers. Percutaneous coronary interventions were used in 8% in STEMI. Thrombolytic (96.3% streptokinase) were used for 58.5% of patients with STEMI.
We present data from a registry of 1905 patients with STEMI who presented to CMC Vellore looking at the treatment modalities used for reperfusion.
In this study, we aim to study the current trends in revascularization in STEMI in a tertiary care centre in South India. We also assessed the number and proportion of patients receiving pharmacological or invasive reperfusion treatment of STEMI. The number of patients not receiving any form of reperfusion therapy and the reasons for the same were also evaluated.
2. Materials and methods
This was a retrospective observational study done in Vellore, which is a tier 3 South Indian city. It is a single-centre study done in the Cardiology department of Christian Medical College, a tertiary care centre. The Department of Cardiology CMC Vellore is equipped with all the required facilities for tackling cardiac emergencies and primary PCI. The cardiac catheterization laboratory was established almost 45 years back. The cardiac catheterization laboratory and interventional cardiologists are available round the clock. The department caters around 700–800 patients of acute ST elevation myocardial infarction per year.
2.1. Subjects
All patients irrespective of age who presented with acute STEMI were included in the study. Patients coming with STEMI are usually local with poor socioeconomic status. Affordability of interventional procedures is always a problem. As Vellore district covers a large rural population, awareness among people about coronary artery disease and the recent advances in treatment are deficient.
2.2. Data collection and analysis
The number of patients thrombolysed with streptokinase, tenecteplase or undergoing primary PCI was determined. Their percentages, mean and standard deviations were calculated. The data was scrutinized for the trends in revascularization. Data were collected from the in-patient and out-patient records as well as the records in the Coronary Care Unit (CCU)/Chest Pain Unit (CPU). Patients were divided into age groups of 20–39, 40–59, 60–79 and >80 years. Other variables that were taken into account included age, gender and risk factors for coronary artery disease. The number of patients not revascularized and the reasons for the same were also studied. Sample size was calculated using the formula 4PQ/D2, using data from CREATE study. P is percentage of patient revascularized in the previous study. Q is 100−P.
3. Results
Between 1st August 2008 and 28th Feb 2011, a total of 1905 patients with ST-segment elevation myocardial infarction (STEMI) were enrolled into this study. The demographic characteristics of the patients are presented in Tables 1 and 2. The largest number of patients was in the age group of 40–59 years (949, 49.8%). Younger age group included 153 (8%) patients. 49 (2.6%) patients were >80 years. 1636 (86%) of patients received some form of reperfusion therapy either by thrombolytic agent or PCI. Thrombolytic with streptokinase was the most common mode of reperfusion. 1235 (75.5%) of the total STEMI patients were reperfused with it. It was also the most common mode of reperfusion in all age group categories.
Table 1.
Demographic characteristics of patients.
| STK lysis (%) | TNK lysis (%) | Primary PCI (%) | Nil (%) | Total (%) | |
|---|---|---|---|---|---|
| Total | 1235 (65) | 196 (10) | 205 (10.7) | 269 (14) | 1905 |
| Age 20–39 | 114 (9.2) | 8 (4) | 21 (10.0) | 11 (4) | 153 (8) |
| Age 40–59 | 627 (50.7) | 88 (44.9) | 103 (50) | 123 (45.7) | 949 (49.8) |
| Age 60–79 | 468 (37.9) | 96 (49) | 76 (37) | 116 (43) | 754 (39.5) |
| Age >80 | 26 (2.1) | 4 (2) | 5 (2.4) | 19 (7.6) | 49 (2.6) |
| Age mean + SD | 58.8 + 13 | 61 + 9.4 | 55.6 + 12 | 58 + 12 | 56.3 + 11.8 |
| Male | 1024 (83) | 172 (88) | 184 (90) | 197 (73) | 1577 (83) |
| Female | 211 (17) | 24 (12) | 21 (10) | 72 (27) | 328 (17) |
| AWMI | 719 (58) | 117 (59) | 125 (61) | 189 (70) | 1150 (60) |
| IMI | 497 (40) | 76 (39) | 79 (38.5) | 75 (28) | 727 (38) |
| Others | 19 (2) | 3 (1.5) | 1 (0.5) | 5 (1.8) | 28 (1.5) |
| DM | 617 (50) | 94 (48) | 110 (54) | 123 (46.6) | 944 (49.5) |
| HTN | 407 (32.9) | 80 (42) | 74 (36) | 96 (36.6) | 657 (34) |
| Dyslip | 864 (73) | 111 (57) | 171 (84) | 199 (74.4) | 1345 (70) |
| Smoking* | 370 (30.7) | 82 (42) | 70 (34) | 67 (25.5) | 589 (31) |
Data are number (%) or ± standard deviation.
IMI includes inferior and all other combinations (right ventricular, posterior and lateral).
AWMI includes anterior, antero-sepal, anterolateral and extensive anterior wall STEMI.
Others include high lateral, isolated lateral or posterior wall STEMI.
Includes both current and ex-smoker (*).
Table 2.
Comparison of baseline characteristics and management strategy outcomes of patients enrolled in earlier study by Jose et al14 from the same centre vs present study.
| Characteristics | Earlier study |
Present study |
|---|---|---|
| N = 1320 (%) | N = 1905 (%) | |
| Age | 56 ± 13 | 56.3 ± 11.8 |
| Males | 1106 (83.8) | 1577 (83) |
| Females | 214 (16.2) | 328 (17) |
| Smoking | 569 (43.1) | 589 (31) |
| Diabetes mellitus | 531 (40.2) | 944 (49.5) |
| Hypertension | 504 (38.2) | 657 (34) |
| Location of MI | ||
| Anterior wall MI | 752 (57) | 1150 (60) |
| Inferior wall MI | 517 (39) | 727 (38) |
| Reperfusion therapy | ||
| STK | 1093 (82.8) | 1235 (65) |
| TNK | Nil (0) | 196 (10) |
| PCI | Nil (0) | 205 (10.7) |
This was followed by primary PCI which was used in total of 205 patients (11%). The age group in which this modality was most utilized was 40–59 years (103, 50%). Patients with age >80 years were least benefited by PCI (2.4%) followed by age group 20–39 years (10.2%). Tenecteplase was used in 196 (10%) patients. 269 (14%) did not receive any form of reperfusion for various reasons. The most common reason for not receiving reperfusion therapy was late presentation in 230 (85.5%) patients followed by cardiogenic shock or death in 32 (12%) (Fig. 1). There were 7 patients who were denied thrombolytic agents because of contraindications for thrombolysis. Out of which 5 patients had either recent or associated cerebrovascular accident and 2 had an associated pericardial effusion.
Fig. 1.
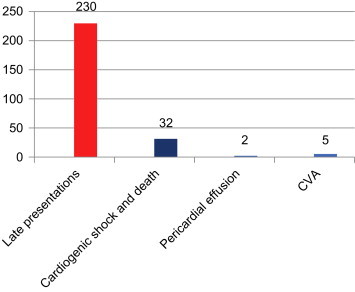
Reasons for not utilizing reperfusion therapy.
Mean age of patients in the whole study population was 56.3 + 11.8 years. Maximum patients were in the age groups of 40–59 years with least in >80 years.
Patients with STEMI increased progressively in every 6 months assessment. It was 297 patients to start with in 1st half-year which became 465 and 446 in the last two half-years. Number of patients utilizing STK as thrombolytic agent remained same in first half-year and the last half-year (Fig. 4), even though the proportion decreased from 75.5% in first half-year to 48% in last half-year. Patient who did not receive any form of revascularization too increased from 35 (11.8%) in the first half-year to 65 (14.6%) in the last half-year. The use of tenecteplase was almost the same in the first four half-years, however there was an exponential rise in the last half-year duration.
Fig. 4.
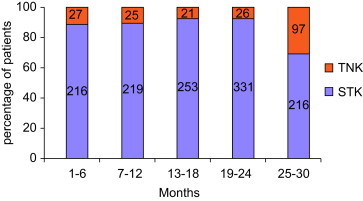
Changes in lysis strategy over study period.
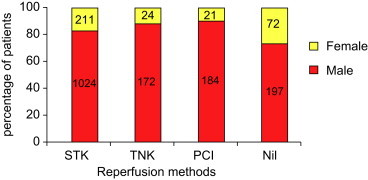
In all treatment groups the proportion of males was more than females. Overall 83% of total STEMI patients were male and 17% were females. In the group of patients not reperfused, females were 72 (26.7%), for tenecteplase (24, 12%), PCI (21, 10%) and streptokinase 211 (14.4%).
Most common territory involved was anterior wall which constituted 1150 (61%) patients. Inferior wall STEMI in various combinations was 727 (38%). Other territories included high lateral, isolated posterior wall etc were 28 (1.%). 49.7% of the patients has type 2 diabetes mellitus. 73% of patients had dyslipidemia. 34% of the patients had hypertension. 31% of the patients were either current or ex-smoker. 60% of the patients have at least ≥2 risk factors.
4. Discussion
Mean age of presentation of STEMI in present study was 56.3 ± 11.8 years with majority of them being males (83%). In the study done by Jose and Gupta (2004), which included patients from 1999 to 2003 in the same centre and the CREATE15 registry which enrolled patients from 2001 to 2005, the mean age been 56 ± 13 years and 57.5 ± 12 years. This is suggesting that mean age of patients has not change over a decade even when comparing data from the same centre. Patients enrolled in this study presented a decade earlier in comparison to the western data where the mean age of presentation has increased from 64.1 years to 66.4 years. Early age of STEMI could lead to tremendous loss of productive years and can have an adverse outcome on the economy as well as national health.
It is noteworthy that only a small percentage of patients in younger age group of 20–39 years received PCI (10.7%) and tenecteplase (4%) as compared to the 40–59 years age group (PCI 50%, tenecteplase 44.9%). This relates to the social status and financial means of the patients enrolled in the study. Younger patients who would be benefited the most in terms of productive life-years saved remain the least benefited by recent advances in reperfusion therapy.
In the present study, women comprised 17% of all patients, which was comparable to the proportion of women patients in the CREATE study (18%) and the study by Jose et al (16.2%). The data also highlighted the inferior treatment received by women in comparison to men, as of the patients who received PCI only 10% were women. Similarly, women comprised only 12% of all STEMI patients who received tenecteplase as a thrombolytic agent.
4.1. Trends in STEMI
There was steady increase in admissions of patients with STEMI over a period of 2½ years which was divided into five half-years for analysis. There was almost 20% increase in the number of STEMI, if we compare the first two half-years with the last two (Fig. 3). This increment raises serious concern that the incidence of STEMI is likely to be doubled in less than 4 years in the local population. There was increase of approximately 30% of STEMI patients from the first half-year to the last two. In the first half-year, streptokinase was used in 72% of patients of all STEMI. This percentage remained almost the same till the first four half-years; however in the last half-year only 48.4% of STEMI patient's utilized streptokinase. So even though the numbers of patients of STEMI have increased, the role of streptokinase as the main thrombolytic agent remained the same over the first 2 years period of study, but newer modalities in the form of PCI and TNK together constituted 37% of STEMI patients in the last half-year reflecting a very significant change in reperfusion strategy. Streptokinase constituted 86% of all thrombolysed cases. This is in comparison to data from CREATE study in which thrombolytic (96% streptokinase) were used for 58.5% of patients with STEMI and study of Jose and Gupta, 2004 in which 82.8% of patients received thrombolytic (all with streptokinase).
Fig. 3.
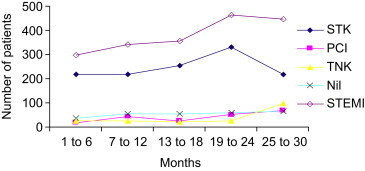
Trends of reperfusion in STEMI. *Numbers represent months in serial order from July 08 to Feb 11.
A very important result of this study was the analysis of patients who did not receive any reperfusion therapy because of various reasons. 14% patients of STEMI did not receive reperfusion therapy over the period of two and a half-years; there was 46% increase in the number of such patients between the 1st and the last half-years, which is very alarming considering that this number should ideally be expected to fall. In comparison, in the study by Jose and Gupta (2004) 17.2% patient did not receive reperfusion therapy. So even a decade after the study by Jose and Gupta, 2004, the reperfusion therapy usage in STEMI has only marginally increased. The most important reasons for no reperfusion therapy usage was late presentation (85.5%) (Fig. 2). There were many reasons for this, such as late diagnosis and referral, poor transport facilities and lack of awareness in the general population. Even though, females formed only 17% of all STEMI patients, they constituted 27% of patients not receiving reperfusion therapy (Fig. 5). So reperfusion therapy usage rates were lower in female patients as compared to males.
Fig. 2.
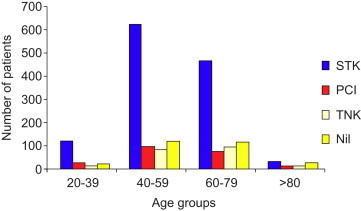
Age distribution for reperfusion therapy.
Fig. 5.
Gender percentage for reperfusion strategy.
Cardiogenic shock and death prior to instituting reperfusion therapy (12%) was the second most common cause for not receiving reperfusion therapy. These patients could have been treated with primary PCI, if they could have afforded it. High cost of PCI procedures and its non-availability even in some tertiary care centres remains one of the important drawbacks in the management of STEMI in India.
There were 7 patients who had an absolute contraindication to thrombolytic therapy. Five of them had a recent cerebrovascular accident and one had a concurrent large ischaemic stroke. Two patients were not offered thrombolytic in view of large associated pericardial effusion. PCI would have been the best option in these patients, if they could have afforded it. Tenecteplase was used in 10% of patients, where as in the study by Jose et al study the only thrombolytic used was streptokinase. The number of patients who were thrombolysed with tenecteplase remained almost same till the first four half-years studied following which it has an exponential rise in last half-year. Tenecteplase was used in 9% of all STEMI patients in the first half-year compared to only 21.7% in the last (Fig. 4). The cost of tenecteplase still was the reason for fewer patients being thrombolysed with it. The cost of tenecteplase in our centre is 7–8 times that of streptokinase. Interestingly, it was found that most of the patients who could afford tenecteplase, could afford PCI as well and so opted for the latter. So even though TNK is replacing STK as thrombolytic agent in our centre, to do it completely, its price has to come down significantly.
Primary PCI was used in 10.7% of patients as a reperfusion modality. There was 20% increase in primary PCI between first and 2nd year of study. In the 1st half-year PCI was used only in 6.3% of all STEMI patients and this percentage increased to 15.2% in the last half-year. So even though the percentage of primary PCI between 1st and the last half-year has almost doubled, this may not be adequate considering 30–35% increase in the rates of STEMI hospitalizations during this period.
This study also analyzed the main risk factors for CAD prevalent in the Indian population. Diabetes mellitus was found in 49.7% of patients; systemic hypertension was found in 34; 31% of patients were either current or ex-smokers and 73% of patients had some form of dyslipidemia. This data is different from data from CREATE study where 34% patients had diabetes; 37.7% had hypertension; and 40.2% were smokers. Study from Jose et al from the same centre as the present study a decade back showed 40.2% prevalence of diabetes in STEMI patients. So data from present study demonstrates an increase in the proportion of patients with diabetes as compared to the past studies and suggest a strong correlation of diabetes mellitus with coronary artery disease.
There may be other non-conventional risk factors for e.g. Mediterranean diet, stress, depression, playing an important role in pathogenesis of coronary artery disease (Singh et al, 2010; Tee and Hassan, 2011; Corona et al, 2011). These factors may play an important role in young patients especially those who lack conventional risk factors.
There were many differences between the present study and the study by Jose and Gupta (2004) and the CREATE registry. The study by Jose and Gupta (2004) was done a decade ago in the same centre as the present study. Thrombolytic with streptokinase was the only mode of reperfusion in patients of STEMI, where as in the present study STK is considered as a last option for reperfusion therapy after PCI and tenecteplase. Data on gender and territory of MI has remained almost the same in the two studies. Prevalence of diabetes mellitus has increased 10% in STEMI patients over a decade which may be the reason for increased number of patients presenting with STEMI in the present study. The present study differed from the CREATE registry as it is a single-centre study as compared to the multi-centre CREATE registry.
The present study highlights the current scenario of STEMI and its management in a tier 3 South Indian city. Even with a tertiary care centre with cardiac catheterization laboratories and experienced cardiologists available 24 h a day, the rates of primary PCI have been low. Many reasons are responsible for this. The most important being the financial constraints of the patients; most patients in India pay for emergency medical expenses themselves and lack insurance cover. Tenecteplase is in process of replacing STK as a main thrombolytic agent but it has a long way to go.
Lack of awareness in general population and poor referral and transport have an important role to play. Increasing the numbers of tertiary cardiac centres alone is unlikely to be sufficient to improve the management of STEMI; the efforts have to be made in all directions.
5. Conclusion
Patients with STEMI in this study are decade younger than western population. There was 20% increase in STEMI every year in the studied population. The younger patients are least likely to get primary PCI or tenecteplase as reperfusion therapy. 86% of patients received some form of reperfusion therapy in this study. Streptokinase was the most common type of reperfusion therapy used. Primary PCI rates showed increasing trend but still only 10% STEMI patients receive it. Use of tenecteplase, which is a better replacement for streptokinase showed exponential rise in the last half-year but much more needs to be done especially in terms of cost reduction so that it can completely replace streptokinase in centres where PCI is not available. In present study, 1 in 8 patients of STEMI didn't receive any form of reperfusion therapy. Most common reason for this was late presentation. Almost 50% of STEMI patients had diabetes mellitus signifying the role of diabetes mellitus as a major risk factor for coronary artery disease in Indian population. Out of all STEMI, 3/5th of them were involving anterior wall indicating high risk STEMI.
Conflicts of interest
All authors have none to declare.
Acknowledgements
Researchers would like to acknowledge Christian Medical College (CMC) Vellore in for providing the equipment and facilities for this research.
References
- 1.Lopaze A.D., Mathers C.D., Ezzati M., Jamison D.T., Murray C.J. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 2.Yusuf S., Reddy S., Ounpuu S., Anand S. Global burden of cardiovascular diseases: Part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104:2855–2865. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- 3.Gaffar A., Reddy K.S., Singhi M. Burden of non-communicable diseases in South Asia. BMJ. 2004;328:807–810. doi: 10.1136/bmj.328.7443.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fox K.A., Goodman S.G., Klein W. Management of acute coronary syndromes. Variations in practice and outcome; findings from the Global registry of Acute Coronary Events (GRACE) Eur Heart J. 2002;23:1177–1189. doi: 10.1053/euhj.2001.3081. [DOI] [PubMed] [Google Scholar]
- 5.Mandelzweig L., Battler A., Boyko V. The second Euro Heart Survey on acute coronary syndrome: characteristics, treatment, and outcome of patients with ACS in Europe and Mediterranean Basin in 2004. Eur Heart J. 2006;27:2285–2293. doi: 10.1093/eurheartj/ehl196. [DOI] [PubMed] [Google Scholar]
- 6.Budaj A., Brieger D., Steg P.G. Global patterns of use of antithrombotic and antiplatelet therapies in patients with acute coronary syndromes: insights from the Global Registry of Acute Coronary Events (GRACE) Am Heart J. 2003;146:999–1006. doi: 10.1016/S0002-8703(03)00509-X. [DOI] [PubMed] [Google Scholar]
- 7.Steg P.G., Goldberg R.J., Gore J.M. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (GRACE) Am J Cardiol. 2002;90:358–363. doi: 10.1016/s0002-9149(02)02489-x. [DOI] [PubMed] [Google Scholar]
- 8.Gibson C.M. NRMI and current treatment patterns for ST-elevation myocardial infarction. Am Heart J. 2004;148:29–33. doi: 10.1016/j.ahj.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Rogers W.J., Canto J.G., Barron H.V., Boscarino J.A., Shoultz D.A., Every N.R. Treatment and outcome of myocardial infarction in hospitals with and without invasive capability. Investigators in the National Registry of Myocardial Infarction. J Am Coll Cardiol. 2000;35:371–379. doi: 10.1016/s0735-1097(99)00505-7. [DOI] [PubMed] [Google Scholar]
- 10.Rogers W.J., Canto J.G., Lambrew C.T. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: the National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000;236:2056–2063. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 11.Yusuf S., Flather M., Pogue J. Variations between countries in invasive cardiac procedures and outcomes in patients with suspected unstable angina or myocardial infarction without initial ST elevation. OASIS (Organisation to Assess Strategies for Ischaemic Syndromes) Registry Investigators. Lancet. 1998;352:507–514. doi: 10.1016/s0140-6736(97)11162-x. [DOI] [PubMed] [Google Scholar]
- 12.Hasdai D., Behar S., Wallentin L. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin; the Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS) Eur Heart J. 2002;23:1190–1201. doi: 10.1053/euhj.2002.3193. [DOI] [PubMed] [Google Scholar]
- 13.Mandelzweig L., Battler A., Boyko V. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006;27:2285–2293. doi: 10.1093/eurheartj/ehl196. [DOI] [PubMed] [Google Scholar]
- 14.Jose V.J., Gupta S.N. Mortality and morbidity of acute ST segment elevation myocardial infarction in the current era. Indian Heart J. 2004;56:210–214. [PubMed] [Google Scholar]
- 15.Xavier D., Pais P., Devereaux P.J. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;361:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]


