Abstract
Acute myocardial infarction following snake bite is rare with few reported cases in literature. A 60-year-old male underwent uneventful stenting to a critical stenosis in left anterior descending coronary artery in June 2012. A month later, he presented to the local hospital with history of snake bite. During admission he developed chest pain with ST-segment elevation in anterior leads consistent with stent thrombosis. He was successfully thrombolysed and his coronary angiogram 5 days later revealed patent stent with TIMI III flow and no evidence of thrombus.
Keywords: Snake bite, Acute myocardial infarction, Stent thrombosis, Thrombolysis
1. Introduction
Acute myocardial infarction is a rare complication of snake envenomation with few reported cases in literature.1 Here we describe an interesting case of anterior wall ST-segment elevation myocardial infarction (STEMI) resulting from possible late stent thrombosis precipitated by snake bite.
2. Case history
A 60-year-old male farmer underwent successful percutaneous coronary intervention (PCI) to a critically narrowed left anterior descending coronary artery (LAD) with a sirolimus eluting stent in June 2012. The patient made an uneventful recovery and was asymptomatic on discharge. A month later he presented to the local hospital with a history of snake bite. The presenting symptoms were severe epigastric pain, nausea, vomiting, dryness of mouth, and inability to open the eyes. His vitals were stable and the clinical examination was unremarkable except ptosis. There were no bleeding manifestations. His baseline hemoglobin was 11 g% and the coagulation parameters were with in normal limits. He was admitted in intensive care unit and treated with anti-snake venom (AST) and other supportive measures.
Few hours later, he developed severe central chest discomfort and hypotension. His electrocardiogram (ECG) showed ST-segment elevation in anterior chest leads (Fig. 1a) and echocardiogram revealed regional wall motion abnormalities in LAD territory. He was started on inotropes and volume expansion. However, there was no improvement chest pain or hemodynamics and ECG showed persistent ST-segment elevation. With expected time delay in transfer to a higher institute and unstable hemodynamics, it was decided to continue treatment locally. After discussing the risk and benefits of thrombolysis with patient's relatives, he was treated with bolus doses of reteplase. Post thrombolysis, there was complete ST-segment resolution (Fig. 1b) and the hemodynamics stabilized. His peak troponin was 1 ng/ml. The patient was monitored for hemodynamic instability and bleeding over next three days. His hemoglobin and coagulation parameters remained stable. Patient underwent coronary angiography on day 5 which revealed patent stent with TIMI-3 distal flow (Fig. 2). He was asymptomatic and the ejection fraction was 50% on discharge.
Fig. 1.
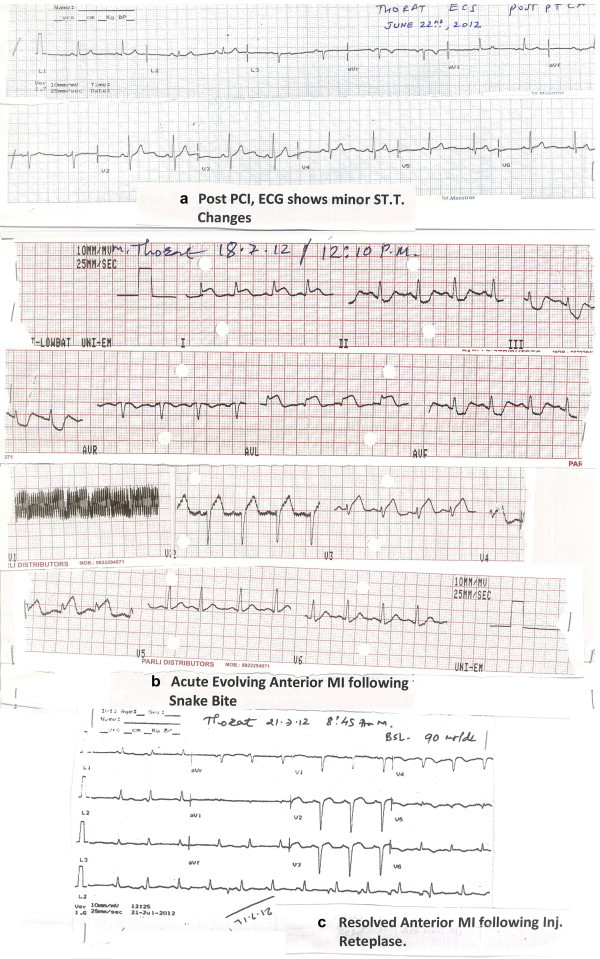
(a) Electrocardiogram (ECG) showing ST-segment elevation in leads I, aVL and V1–V4 and reciprocal changes in leads II, III, aVF. (b) Post thrombolysis ECG showing good ST-segment resolution.
Fig. 2.
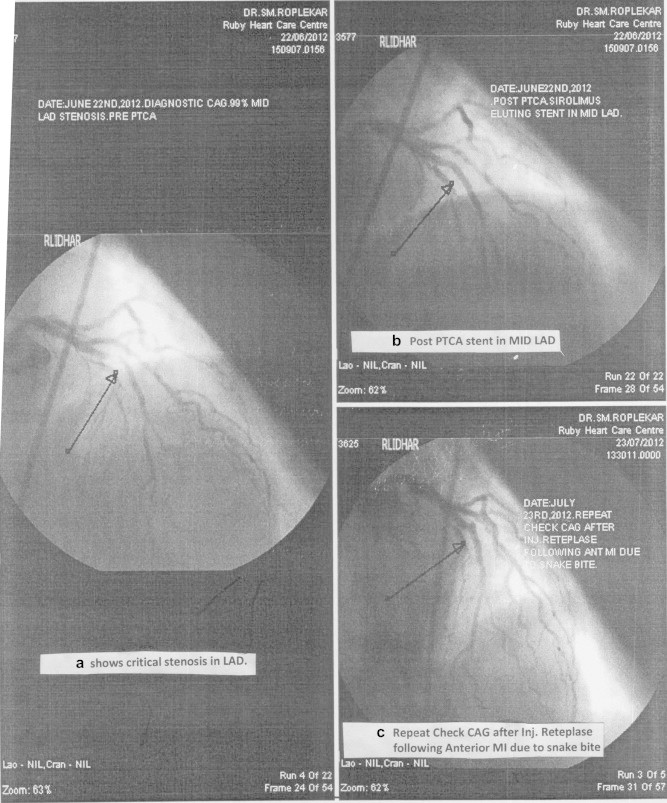
Follow up angiogram showing patent stent in left anterior descending coronary artery.
3. Discussion
Snake bites have been estimated to account for 45,900 deaths annually in India.2 Russell's vipers are widely prevalent across the country and account for nearly half of the poisonous snake bites. Viper envenomation commonly causes local tissue reaction, coagulopathy, nephrotoxicity and neurotoxicity.1
Though cardiac manifestations are common with snake bites, significant myocardial damage is very rare. In a study involving 108 patients from Nigeria, more than 60% patients had hemodynamic and electrocardiographic abnormalities; however, significant cardiac enzyme elevation occurred in only one patient.3 There have been only scattered reports of proven myocardial infarction following snake bite and the exact mechanism of myocardial damage from snake bite remains unclear.1,4–6 Aravanis et al,4 have reported a case of acute inferior wall MI in a 17-year-old girl following viper snake bite. She was treated conservatively. Later she developed stroke which recovered over next two months. The angiogram done at that time showed normal epicardial coronary arteries. They have attributed myocardial infarction to the possible direct cardio toxicity and also considered coronary thrombosis from hypercoagulability as an alternative mechanism. Blondheim et al,5 have described a case of 28-year-old male who had diffuse ST-segment elevation, increased cardiac enzymes and segmental wall motion abnormalities after viper bite. The coronaries were free of disease and they proposed myocarditis from toxic envenomation as the mechanism of cardiac injury. Tony et al,6 have reported a case of myocardial infarction on day 2 following snake bite and proposed vasospasm caused by sarafotoxin in snake venom as the possible mechanism. There have been few cases of myocardial infarction and cerebrovascular accident where there were thrombi in the involved blood vessels during angiography or at autopsy.7,8 The other presumed mechanisms are hypovolemic shock from increased vascular permeability, coronary vasospasm from panic of snake bite hypersensitivity reactions.1,9
Any of the aforementioned mechanisms alone or in combination might have contributed to myocardial infarction in this patient. With the background of recent DES implantation, ST-segment elevation consistent with the distribution of the stented coronary artery and resolution of chest pain, ECG changes and improvement of hemodynamics with thrombolysis, stent thrombosis from the coagulation abnormalities of snake bite appears to be the most probable cause here.
Immediate cardiac catheterization not only establishes the diagnosis and also provides opportunity for definitive treatment in case of stent thrombosis. As the patient was in a remote place and hemodynamically unstable for transfer, he was treated locally. The option was between conservative management with heparin and hemodynamic support with inotropes and thrombolysis. The major issue was the risk of life threatening bleeding with thrombolysis on the background of viper bite which is known to cause consumption coagulopathy. The presentation was mainly neuroparalytic and there were no bleeding manifestations. Moreover, the worsening hemodynamics necessitated urgent revascularization and hence it was decided to thrombolyse the patient.
Myocardial injury from coronary thrombosis following snake bite is a rare event and should be kept in mind when a patient develops cardiac manifestations following snake bite. Timely recognition and appropriate treatment may be lifesaving.
Conflicts of interest
All authors have none to declare.
References
- 1.Maheshwari M., Mittal S.R. Acute myocardial infarction complicating snakebite. J Assoc Physicians India. 2004;52:63–64. [PubMed] [Google Scholar]
- 2.Mohapatra B., Warrell D.A., Suraweera W. Snakebite mortality in India: a nationally representative mortality survey. PLoS Negl Trop Dis. 2011;5:e1018. doi: 10.1371/journal.pntd.0001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karaye K.M., Mijinyawa M.S., Yakasai A.M. Cardiac and hemodynamic features following snakebite in Nigeria. Int J Cardiol. 2012;156:326–328. doi: 10.1016/j.ijcard.2012.01.098. [DOI] [PubMed] [Google Scholar]
- 4.Aravanis C., Ioannidis P.J., Ktenas J. Acute myocardial infarction and cerebrovascular accident in a young girl after a viper bite. Br Heart J. 1982;47:500–503. doi: 10.1136/hrt.47.5.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blondheim D.S., Plich M., Berman M. Acute myocardial infarction complicating viper bite. Am J Cardiol. 1996;78:492–493. doi: 10.1016/s0002-9149(96)00347-5. [DOI] [PubMed] [Google Scholar]
- 6.Tony J.C., Bhat R. Acute myocardial infarction following snake bite. Trop Doct. 1995;3:137. doi: 10.1177/004947559502500322. [DOI] [PubMed] [Google Scholar]
- 7.Gaballa M., Taher T., Brodin L.A. Images in cardiovascular medicine: myocardialinfarction as a rare consequence of a snakebite: diagnosis with novelechocardiographic tissue Doppler techniques. Circulation. 2005;112:140–142. doi: 10.1161/CIRCULATIONAHA.104.492942. [DOI] [PubMed] [Google Scholar]
- 8.Bashir R., Jinkins J. Cerebral infarction in a young female following snakebite. Stroke. 1985;16:328–330. doi: 10.1161/01.str.16.2.328. [DOI] [PubMed] [Google Scholar]
- 9.Frangides C., Kouni S., Niarchos C., Koutsojannis C. Hypersensitivity and Kounis syndrome due to a viper bite. Eur J Intern Med. 2006;17:215–216. doi: 10.1016/j.ejim.2005.11.016. [DOI] [PubMed] [Google Scholar]


