Abstract
We report on emergency percutaneous renal artery stenting in two children who developed acute anuria due to bilateral renal artery stenosis and near-total occlusion. In both children, urine output could be reestablished following the procedure. One patient died from persistent severe cardiac failure. Emergency stenting is feasible, and may buy time for future procedures.
Keywords: Takayasu arteritis, Anuria, Renal artery stenting
1. Introduction
Nonspecific aortoarteritis is an uncommon inflammatory disease of the aorta and other major vessels, and involvement of the abdominal vessels is particularly more frequent in the Indian population.1 It results in stenosis, occlusion or dilation and aneurysm formation of the involved arteries.2 Therapeutic options include surgical revascularization, balloon angioplasty or stent implantation, all of which have been performed electively.3–7 There are very limited data regarding emergency transcatheter therapy in the setting of active inflammatory disease. We report on two children with anuric renal failure who underwent emergency renal artery stenting.
2. Cases
2.1. Case 1
A 13-year-old boy presented with fever, dyspnea, oliguria and hypertension. Initial investigations showed a high erythrocyte sedimentation rate (75 mm in the first hour), and serum creatinine of 2.5 mg/deciliter. Abdominal ultrasound and magnetic resonance angiography demonstrated an irregular abdominal aorta with severe bilateral renal artery stenosis. Systemic steroid therapy with prednisolone was commenced. Within 24 h of hospital admission, his clinical condition deteriorated with onset of anuria and the serum creatinine increasing to 4.5 mg/deciliter. Emergency angiography showed total occlusion of the right, and subtotal obstruction of the left renal artery (Fig. 1a). The left renal artery was cannulated with a 6 French guiding catheter (Cordis, Johnson & Johnson, USA) and crossed with a 0.014 inch Galeo guide wire (Biotronik, Germany). A 4 × 13 mm Zeta stent (Abbott Vascular, USA) was deployed covering the renal artery ostium and entire diseased segment (Fig. 1b). The right renal artery could not be salvaged. There were no procedure related complications. Urine output was reestablished within 4 h of the procedure, and the serum creatinine normalized on the fifth day. He was started on aspirin 3 mg/kg daily and multiple antihypertensive drugs. The follow-up evaluation after 12 months revealed persistent hypertension. At this time, a right renal auto-transplantation was performed together with a left spleno-renal shunt due to in-stent restenosis. He could be weaned off all his antihypertensive medications within 12 months of these surgical procedures.
Fig. 1.
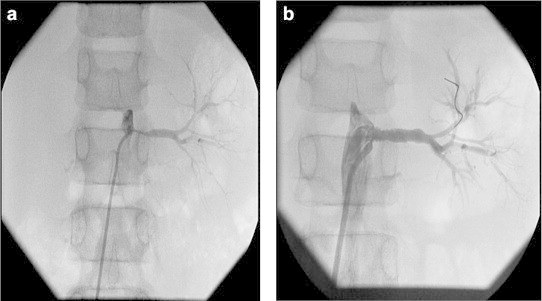
a) Left panel: Selective left renal artery injection showing severe proximal segment stenosis with filling of distal branches. The right renal artery was occluded. b) Right panel: Angiogram post-stent implantation in patient 1.
2.2. Case 2
This 11-year-old boy presented with generalized edema, dyspnea and decreased urine output of 5 days' duration prior to admission. Initial evaluation demonstrated absence of lower limb pulses, severe hypertension, and dilated cardiomyopathy with left ventricular dysfunction on echocardiography. Abdominal ultrasound revealed obstruction of both renal arteries. The erythrocyte sedimentation rate in the first hour was 40 mm, and serum creatinine was 4.3 mg/deciliter. Within a few hours of admission, he developed metabolic acidosis with increasing serum lactate levels, and anuria. Emergency catheterization with the intention of renal revascularization was attempted. Under intravenous sedation, percutaneous right femoral artery access was obtained. Descending aortic angiography revealed a severely diseased thoracic and abdominal aorta with multiple areas of constriction (Fig. 2a). The right renal artery and nephrogram were not visualized; the left renal artery was seen faintly filling through a long segment stenosis (Fig. 2b). A 2.5 × 15 mm Cobalt C stent (Relisys, India) was deployed in the left renal artery after pre-dilatation with a 2 × 10 mm balloon. Urine output was established 2 h after the procedure. Despite this, peritoneal dialysis was done and therapy commenced with intravenous heparin and oral prednisolone. He continued to be in cardiac failure with severe left ventricular dysfunction, which did not improve despite appropriate inotropic support. Five days later he developed ventricular arrhythmias, requiring several attempts at cardiopulmonary resuscitation and antiarrhythmic therapy. An emergency balloon dilation of the thoracic and abdominal aorta was performed and partially relieved the multiple obstructions. However, his clinical condition continued to deteriorate, and he died the next day.
Fig. 2.
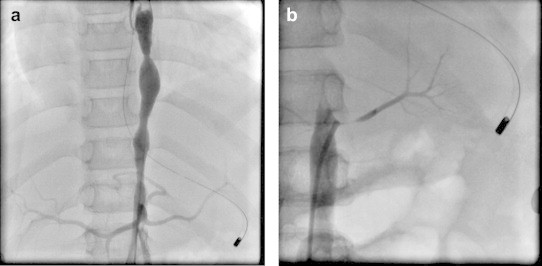
a) Left panel: Descending aortogram in patient 2, demonstrating multiple stenosis-typical for aortoarteritis. b) Right panel: Selective left renal artery angiogram showing a long segment stenosis in patient 2. The right renal artery was totally occluded.
3. Discussion
Nonspecific aortoarteritis, also known as Takayasu disease, is of unknown etiology. In contrast to patients in Japan and Europe, in whom the aortic arch and its branches are mainly involved, involvement of the abdominal aorta and the renal arteries is more common in Indian patients.1,8 Long-term steroid therapy together with aggressive pharmacologic therapy of hypertension are indicated. Surgical revascularization and balloon dilation of the affected renal artery segment have both been employed to improve renal perfusion in patients with poor control of hypertension, or with associated cardiac dysfunction. There are few long-term data for surgical revascularization in children.3 Balloon angioplasty is associated with higher recurrence rates for children, due both to the smaller diameter of the affected artery and the persistence of active inflammatory disease.5 In a large multicenter retrospective study of surgical and endovascular interventions in young adults, clinical or laboratory evidence of biological inflammation at the time of revascularization was independently associated with the risk of arterial complications (including restenosis or thrombosis) after the procedure.9 There are few data on stent therapy in children. In a small series of children with non-inflammatory renal arterial stenosis, elective stent therapy was associated with a higher rate of restenosis when compared to balloon angioplasty.6 Bilateral renal artery stenosis with anuria as a manifestation of aortoarteritis, in the absence of a previous clinical history of disease, is very rare. Emergency renal artery stenting was technically feasible and acutely successful in both children, and resulted in immediate improvement of renal function. Patient 2 succumbed to left ventricular failure due to multiple obstructions in the aorta. Despite the chronic nature of the disease, and the relatively high recurrence rate for restenosis following surgery or transcatheter therapy, emergency revascularization and salvage of the kidney by stent implantation may play a useful role in the management of children presenting with anuria. In particular, it enhances the prospects of patient survival, so that further measures may be instituted in a stable clinical setting.
Conflicts of interest
All authors have none to declare.
References
- 1.Moriwaki R., Noda M., Yajima M., Sharma B.K., Numano F. Clinical manifestations of Takayasu arteritis in India and Japan – new classification of angiographic findings. Angiology. 1997;48:369–379. doi: 10.1177/000331979704800501. [DOI] [PubMed] [Google Scholar]
- 2.Yamato M., Lecky J.W., Hiramatsu K., Kohda E. Takayasu's arteritis: radiographic and angiographic findings in 59 patients. Radiology. 1986;161:329–334. doi: 10.1148/radiology.161.2.2876459. [DOI] [PubMed] [Google Scholar]
- 3.Stanley J.C. Surgical intervention in pediatric renovascular hypertension. Child Nephrol Urol. 1992;12:167–174. [PubMed] [Google Scholar]
- 4.Sharma S., Saxena A., Talwar K.K., Kaul U., Mehta S.N., Rajani M. Renal artery stenosis caused by nonspecific arteritis (Takayasu disease): results of treatment with percutaneous transluminal angioplasty. AJR. 1992;158:417–422. doi: 10.2214/ajr.158.2.1346073. [DOI] [PubMed] [Google Scholar]
- 5.Tyagi S., Kaul U.A., Satsangi D.K., Arora R. Percutaneous transluminal angioplasty for renovascular hypertension in children: initial and long-term results. Pediatrics. 1997;99:44–49. doi: 10.1542/peds.99.1.44. [DOI] [PubMed] [Google Scholar]
- 6.Shroff R., Roebuck D.J., Gordon I. Angioplasty for renovascular hypertension in children: 20-year experience. Pediatrics. 2006;118:268–275. doi: 10.1542/peds.2005-2642. [DOI] [PubMed] [Google Scholar]
- 7.Liang P., Tan-Ong M., Hoffman G.S. Takayasu's arteritis: vascular interventions and outcomes. J Rheumatol. 2004;31:102–106. [PubMed] [Google Scholar]
- 8.Arend W.P., Michel B.A., Bloch D.A. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990;33:1129–1134. doi: 10.1002/art.1780330811. [DOI] [PubMed] [Google Scholar]
- 9.Saadoun D., Lambert M., Mirault T. Retrospective analysis of surgery versus endovascular intervention in Takayasu arteritis: a multicenter experience. Circulation. 2012;125:813–819. doi: 10.1161/CIRCULATIONAHA.111.058032. [DOI] [PubMed] [Google Scholar]


